Histo-Logic December 1999 · their slides. It is important to note that the pathologist is looking...
Transcript of Histo-Logic December 1999 · their slides. It is important to note that the pathologist is looking...

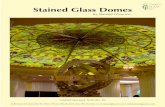
HISTOLOGIC ®
T e c h n i c a l B u l l e t i n f o r H i s t o t e c h n o l o g y
®
Vol. XXXI, No. 2, December 1999
Years before the first person evercoined the phrase “Y2K,” I used towonder where I would be when theclock struck 12:01 AM on January 1,2000. After all, changing centuriesseems like a pretty big deal.My thoughts always strayed toimaginings of what life was like atthe last turn of the century, andabout the incredible technologicalchanges that my grandparents hadwitnessed in their lifetime. Theautomobile, the airplane, computers,and all of the rest (see Countdownto the 21st Century, Histo-Logic,Spring, 1999) have left theirindelible marks on society so thattoday, none of us can imagine livingwithout such modern conveniences.
While everyone else is fretting overY2K and the millennium bug thatthreatens to cripple civilized societyas we know it, we at Histo-Logichave decided instead to celebratethe arrival of 2000 with a whole newlook for our publication that we areexcited about! This is in keepingwith our rich tradition since 1971 ofserving you and the discipline ofhistotechnology with up-to-date,relevant and useful technicalinformation that so often findsapplication in your work.
Over those many years, Histo-Logichas had a tremendous impact on thehistotechnology profession, servingfor many years as the sole technical
bulletin in the discipline. Manyauthors have, in fact, enjoyed seeingtheir very first attempts at author-ship published here. Believe it ornot, it is you, our readers, who havecontributed to much of our successbecause it is not uncommon forindividuals to pass along their copiesto friends or colleagues. Our mix oftechnical, news, and feature articlesprovide the variety that keeps thispublication fresh and interesting.
I am particularly excited about thechanges that we have in store forHisto-Logic, for as the discipline andits practitioners change in the yearsahead, we will continue to workbehind the scenes to provide youwith a resource that you will want toretain for frequent reference. I inviteyou to consider participating in thepreparation of this publication bycontributing your ideas andknowledge in order that they may be
IN THIS ISSUEAs the Century Draws to a Close ………… 21Atypical Cytokeratin Staining of SentinelNode Biopsies for Breast Cancer Due toMicrowave Pretreatment …………………… 22Adapting a Modified Gram Stainfor Use in Resin Embedded Tissues ……… 23Retiring at the Top of His Game…………… 26Description and Preliminary Resultsof a Novel Cassette System (Tissue-Tek® Paraform® Cassette System) … 28All in a Day’s Work! ………………………… 30Using Frozen Sections for HighThroughput Tissue Analysis in the Ageof Molecular Pathology ……………………… 33How to Perform an ElectronicLiterature Search, or Answer the Question “Has Anyone Ever Done This Stain Before?” ………………………… 35Histonet: The List Server forHistotechnology ……………………………… 36What is Cytology Anyway? ………………… 38NSHers Party Like It’s 1999 ……………… 40Mark Your Calendar! ……………………… 42
As the Century Draws to a Close…Vinnie Della Speranza, Scientific Editor
21
Managing Editor, Gilles LefebvreScientific Editor, Vinnie Della Speranza,
MS, HTL (ASCP) HT, MT
1984
19721974
1981
1986 1988
April 1999

Fig.1. CK22 staining of lymph node dendritic cells usingcitrate buffer/microwave antigen retrieval method
Fig. 2. Proteolytic enzyme antigen retrieval methodeliminates dendritic cell staining with CK22
22
shared with others in the discipline.Perhaps you have a tip, or use amethod in your lab that others couldbenefit from. I would be happy tooffer you assistance in preparing anarticle to get your ideas into print.
Rest assured that no matter what theoutcome on January 1, 2000, we atHisto-Logic are poised to continueto serve you. While others arestockpiling foods and other goods, Ihave assembled a large collection ofpads and pencils (remember thoseneat inventions?) so that nothing willprevent our future issues fromgetting to you. Oh, and yes, I nolonger wonder where I will be onNew Year’s Eve. I’m required to beat work with many of my coworkers,prepared to intervene shouldanything go awry at 12:01 AM. Manythanks to whoever is responsible forthis little blunder. Where will you bewhen the lights go out?
Atypical CytokeratinStaining of SentinelNode Biopsies for
Breast CancerDue to Microwave
PretreatmentMichele Margiotta MA,MT(ASCP)HTL,QIHC
Immunohistology SupervisorUniversity Hospital
Stony Brook, New York
The standard procedure for theassessment of nodal staging in breastcancer has been the axillary lymphnode dissection. This is a necessaryprocedure for patients with earlybreast cancer in order to predictrecurrence and survival.1,2 The statusof the lymph nodes also determinesthe mode of treatment the patientwill receive. Unfortunately, there arecomplications from this procedure,which include lymphedema, pain,infection and a limitation ofshoulder motion.1 Consequently, aless invasive procedure such as thesentinel lymph node biopsy isbecoming the preferred procedure.
The sentinel node is the first lymphnode that receives lymphaticdrainage from the tumor. This isusually determined by the injectionof a blue dye or radioisotope aroundthe primary tumor, which thentravels to that first draining orsentinel lymph node.3,4 The node isthen excised and sent to the hos-pital’s surgical pathology laboratorywhere the pathologist examines thespecimen, and the tissue is thenparaffin processed for microtomecutting.The pathologist will thenassess the cut sections to determineif micrometastases are present.3
At this hospital, there is a specialcutting procedure for sentinel lymphnode biopsies. First, level one is cutand a stained H&E is made on oneslide, and unstained slides are cut forimmunohistochemical testing, suchas the cytokeratin antibody stain.Next, the paraffin block is trimmed40 microns and level two is cut.Again, an H&E is stained and un-stained slides are cut for cytokeratinstaining. In our lab, we use the pan-cytokeratin antibody called CK22(Biomeda, Foster City, CA). A pre-treatment step is necessary in orderto expose epitopes on the cells, whichare masked by formalin fixation. Forthe CK22 antibody, we have alwaysperformed a microwave citratebuffer treatment.
When we first started testing thesentinel node biopsies, we noticedthat other cells besides the tumorcells were staining, such as dendritic
cells. This atypical staining was verydisturbing to the pathologists. Theinitial thought was that somethingwent wrong in the staining process,so we repeated the CK22 test andagain the dendritic cells stained. Wethen contacted another lab forcomparison and found that theslides they stained for CK22 had noatypical staining. After discussionwith the other lab, it was determinedthat the only difference in ourstaining methods was the pre-treatment step. They were using anenzyme pretreatment instead of themicrowave citrate buffer method.We then tried a trypsin enzyme pre-treatment and the atypical staininghad disappeared. We theorized thatthe microwave pretreatment exposedepitopes on these other cells thatsomehow reacted with the CK22antibody. This phenomenon did notoccur with enzyme pretreatment.
The pathologists were satisfied thatthey no longer had to disregard theatypical staining while examiningtheir slides. It is important to notethat the pathologist is looking forone or two positively stained tumorcells on the CK22-stained sentinellymph node. So, if they have to weedthrough atypical-staining cells, itmakes their job much harder. Astechnologists, we must ensure thatthe final product is the best it can befor the pathologist. Sometimes it isbeneficial to compare notes withother labs doing similar testing.Ultimately, the patient’s treatment isdependent upon our analysis.

References:1. McMasters K. Sentinel-lymph-node biopsy for
breast cancer. Breast Treatment Associates. Availableat: http:\\www.lymphedemainfo.com\surgeryinfo.html
2. Winchester DJ, et al. Sentinel lymphadenectomy forbreast cancer. J Am Coll Surg. 1999;188(6):597-603.
3. Zavotsky J, Hansen N, Brennan M, Turner R, GiulianoA. Lymph node metastasis from ductal carcinoma insitu with microinvasion. Cancer. 1999;85(11):2439-2443.
4. Liberman L, et al. Sentinel lymph node biopsy afterpercutaneous diagnosis of nonpalpable breast cancer.Radiology. 1999;211(3):835-844.
Adapting a ModifiedGram Stain
for Use in ResinEmbedded Tissues
Robert A. Skinner, HTL(ASCP)Orthopaedic ResearchUniversity of Arkansas
for Medical Sciences4301 West Markham St. Slot 644
Little Rock, AR 72205
Sandra G. McLarenDept. of Orthopaedic Surgery
University of Arkansasfor Medical Sciences
4301 West Markham St. Slot 644Little Rock, AR 72205
AbstractOur laboratory has been engaged inongoing studies to evaluate thepresence or absence of knownGram-positive bacteria in decal-cified paraffin sections of bone.Interest in assessing the impact ofinfection on bone mineralizationor implant materials required usto focus on developing a methodto demonstrate bacteria inundecalcified sections. This is areport on our experience withefforts to adapt our routine Gram-positive stain for use in the study ofundecalcified bone.
IntroductionOur laboratory has several ongoingstudies of osteomyelitis (bone infec-tion) in various models. Theprimary focus of these studies is thepresence or absence of bacteriaafter treatment. Over the pastdecade, an increasing number ofcure modalities have includedgrowth enhancement constituents,bioerodeable delivery systems, orin some cases, both. Studies of the
effect of these cure regimensgenerally include not onlypresence/absence of bacteria butalso the effect of the materials onthe structure and rate of formationof the resulting new or remodeledbone. Additional questions withinthe orthopedic community centeraround the influence of bio-materials (most notably metal andpolyethylene —those typicallyassociated with joint replacements)on bone formation and infectiondynamics. Our lab set out to investi-gate the feasibility of demonstratingthe presence/absence of bacteriaafter antibiotic treatment in non-decalcified samples of bone. Thesestudies would require processing thespecimens into some polymerembedding system. A literaturesearch revealed no significantstaining technique being performedin the types of media available inour facility, to demonstrate Gram-positive bacteria in undecalcifiedbone specimens.
Our earlier investigations ofosteomyelitis involved studyingparaffin-embedded decalcifiedsamples as per establishedprotocol.1 A 5% formicdecalcification regimen allows us toperform procedures from routineH&E to immunohistochemistry. Weuse an established modified Gramstain for the particular strains ofGram-positive Staphylococcusaureus that are used to induce thedisease process.2 We have foundthat Gill’s II hematoxylin incombination with eosin Y/phloxinecounterstain gives the nucleardetail and osteoid seam definitionnecessary to evaluate bone growthand overall architectural formation.Prior to dissection, the infectedrabbit limb is radiographed and theresulting X-ray is evaluated as partof the overall score to categorizethe extent of the disease process.The performance of the modifiedGram stain across a variety ofembedding media became aprimary concern. Our intent was tocompare the performance of thisstain in a decalcified paraffinpreparation with a preparation in
the resin we use for the study ofmetallic implants in undecalcifiedsamples.
Materials & MethodsIn a standard decalcified paraffinstudy, osteomyelitic rabbit fore-limbs, which were infected with aknown strain and quantity ofS aureus, were harvested, cleanedof nonessential soft tissue, fixed in10% neutral buffered formalin,and decalcified in 5% formic aciduntil negative end pointdetermination by the ammoniumoxalate test.1 Decalcified limbswere then split using a disposablemicrotome blade and processedthrough graded ethanols, cleared inmethyl salicylate, and infiltratedinto paraffin as per establishedprotocol.
Five-micron paraffin sections ofdecalcified bone were hydrated andflooded with 2% crystal violet for2 minutes followed by decanting theexcess crystal violet and floodingwith Lugol’s iodine for 2 minutes.The slide was then washed in a 50:50acetone:ethanol mixture until thesection was clear. After a five-minutewater rinse, the slide was immersedin Van Gieson solution for 3 minutesfollowed by a water rinse, a dip insaturated picric acid, ethanoldehydration, clearing and mounting.2
Routine results are depicted inFigure 1.
23
Fig. 1 – Five-micron paraffin section of decalcified rabbitradius stained with routine modified Gram stainincluding Van Gieson counterstain.2 Gram-positive staphaureus cocci appear dark blue. Bone is red. Connectivetissue and purulence (pus) is yellow. 100�

In order to make it possible forus to demonstrate the presence ofbacteria in undecalcified bonecontaining metal implants, our firstapproach was to investigate if thestain would be successful on cut andground sections of bone embedded inKulzer/Exakt 7200 embeddingmedium.This medium was chosenbecause of our prior success withhistologic studies of undecalcifiedbone containing titanium and stain-less steel implants using the ExaktMacro Cut & Grind System. Thelack of staining in earlier specimenswith metallic implants that wereculture positive for Gram-positivebacteria and embedded in the 7200medium suggested that the crystalviolet stain was not getting into thetissue. We designed a parallel pilotstudy to examine the utility ofstaining the infected sample by botha conventional slide staining methodas well as a block impregnationmethod in a manner similar toBielschowsky’s work in 1904.3
A 3.5-cm segment of radius washarvested from two operatedforelimbs of rabbits infected withS aureus (ATCC 49230). The fore-limbs were split longitudinally withthe Exakt Macro Band System andfixed in 10% buffered formalin.One-half of each specimen wassubmitted for decalcification, as acontrol. The remaining halves ofthese specimens were brieflywashed in water and moved to 70%EtOH for storage until processinginto the Kulzer/Exakt resin. Thetwo decalcified control specimenswere processed into paraffin andstained, as per above, and werefound to be positive for bacteria.These tissue blocks were thendeparaffinized in xylene andrehydrated through graded ethanolsto 70% for storage.
One each of the decalcified andundecalcified specimens werewashed in running tap water for2 hours followed by distilled water.These specimens were then pre-stained by immersion into filteredcrystal violet for 30 minutesfollowed by a thirty-minute
immersion in Lugol’s iodine. Theywere decolorized through fivechanges of 50:50 acetone:alcoholwith a final immersion in 100%EtOH over a period of 30 hours,then processed into Kulzer/Exakt7200. The two remaining decalcifiedand undecalcified specimens werenot prestained but processedthrough into the 7200 resin.
For Kulzer/Exakt 7200 processing,the specimens were dehydratedthrough a series of graded acetone/ethanol mixtures starting at 50:50,and infiltrated through gradedethanol/Kulzer 7200 starting at 50:50,to pure Kulzer 7200. After infiltra-tion under 15 psi vacuum at 4°C, allsamples were polymerized overnightby the Exakt Histolux System.Polymerized specimen blocks werethen affixed to plastic slides, sawed toa nominal thickness of 100 microns,and then ground and polished on theExakt Macro Grinder as per manu-facturers protocol to a thickness ofapproximately 45 microns.4 Theslides from previously unstainedspecimens were then stained withcrystal violet for 30 minutes (tocompensate for section thickness),Lugol’s iodine for 30 minutes, anddecolorized with acetone:alcohol.
Microscopic examination revealedGram-positive cocci in bothpurulence and bone in the tissuesprestained prior to processing intoplastic resin. In the sections that
were stained after polymerization,the Gram stain did not penetrate theExakt/Kulzer-infiltrated tissue andno bacteria were seen. Furthermore,decolorization with acetone:alcoholcaused visual deformation of thepolymerized resin.5 The results aredepicted in Figure 2.
A co-investigator on the sameproject later inquired about doingundecalcified processing of bonewithout metallic implants on asmaller and more cost-effectivescale. The primary focus of thisstudy was to assess the effect ofinfection on mineralization andbone remodeling. The earlierKulzer 7200-metal pilotinvestigation was to involve large,if not whole, rabbit radii. This newproject would study small, specificsegments of the radius at theinfection site. Because our lab wasnot equipped at that time with theinstrumentation necessary toprocess and sledge sectionmethylmethacrylate (MMA)samples, we decided to investigatethe use of glycol methacrylate(GMA) for this application.
An extensive literature search onGram stains in GMA sections wasconducted. A keyword search ofMedline from 1966 through thepresent was performed. The keywordsearch pattern looks for the specificword (as it is spelled in the query) inthe Title, Abstract, Registry number,word, and MeSH subject headings.Keyword searches were combinedusing Boolean logic operators “and”and “or.” Using the keywords “gramstain,” “glycol methacrylate,”“plastic,” and “histology” in allcombinations of Boolean logic, therewere no citations (0/52683) thatdescribed Gram stain in GMA forthe period of 1966 to the present.
Glycol methacrylate was at onetime considered a potential water-soluble embedding medium forelectron microscopy. The work ofRuddell in 1967 suggested the useof GMA for routine lightmicroscopy.6 GMA gained favor inthe late 1970s as a more rapid
Fig. 2 – Forty-five micron ground section of Kulzer/Exakt 7200 embedded undecalcified rabbit radiusGram stained and decolorized prior to processing.Gram positive staph aureus cocci appear dark blue.Multiple layers of bacteria can be seen. 100�
24

methodology for the clinical studyof osteoporosis and osteomalacia iniliac crest biopsies. It became theembedding medium of choice forclinical bone marrow core biopsiesat the pathology lab at SUNYStony Brook during the early 1980sbecause of the superior cellulardetail afforded by the standard2-micron section. Our prior exper-ience with converting paraffinefficient stains to glycol meth-acrylate-embedded sections con-vinced us that such a conversion forthis pilot study was very possible.7,8
Since bacteria colonize surroundingsoft tissue as well as bone, we wereable to evaluate staining perfor-mance in soft tissue embedded inGMA.
In order to answer the basicquestion of whether the stain wouldwork in GMA, we collectedelliptical skin samples containing acentral outwardly draining sinustract located immediately above theinfected bone. This tract shouldcontain the Gram-positive bacteriafrom the infected site within thebone. The sample could then bebisected through the tract to beparallel processed through paraffinas well as GMA. In this way, wecould experiment with thealternative processing and stainingprocedure without compromisingany N value for the infected bonegenerated for the actual project,and not add significantly to thecost.
The paraffin skin sample wasprocessed, as per routine, with theexception that no decalcification wasperformed. The GMA sample wasfixed in formalin, dehydratedthrough graded ethanols to absolute,and infiltrated in three changes ofcatalyzed GMA (JB4 kit), beforebeing polymerized via an 8:1 ratio ofcatalyzed GMA: accelerator, as perkit recommendations.9 The poly-merized samples were sectioned at2 microns on a JB4 microtome usingglass knives.
An initial staining run included boththe 5-micron deparaffinized slide
and a 2-micron GMA slide from thesame skin sample, in parallel, usingthe times established for paraffinsection staining. The results aredepicted in Figure 3.
ResultsFigure 2 shows that staining anddecolorizing of the fixed tissue priorto processing and embeddingsuccessfully demonstrates thepresence of Gram-positive bacteria.Note that the section in Fig. 2 isphotographed with no counterstain.This was done to afford the inves-tigator maximum visualization ofthe bacteria with no other distrac-tion. While the staining outcomewith this technique was successful,the results were less optimal thanthe staining of slide-mountedsections.
A comparison between Fig. 3a andFig. 3b illustrates that the stain
successfully demonstrates thepresence of bacteria in each sectionwithout the need for modifying theparaffin staining procedure. Thebacteria are clearly visualized inparaffin decalcified bone (Fig. 1),paraffin skin (Fig. 3a), and GMAskin sections (Fig. 3b). There is asignificant difference in the stainingintensity of the red component ofthe Van Gieson counterstainbetween the paraffin skin and theGMA skin sections. This can beovercome by staining longer in theVan Gieson stain and shorteningthe dehydration time in order toachieve paraffin-like stainingresults.
DiscussionOur experience illustrates thathistotechs have opportunities tocontribute their expertise in theplanning and implementation ofprojects such as the study describedhere. Principal investigators have anidea of what they would like toachieve but oftentimes have onlyvague ideas of how to reach theirgoal. When we proposed performingthe Gram stain in the Kulzer/Exaktresin, the reaction was “who’s doingthat?” A similar reaction wasexpressed when the GMA approachwas suggested. The answer in bothcases was “nobody, that we candetermine, so why not be the first?”The original expectation of ourinvestigator to see crisp, clearstaining in a cut and ground section(45 microns) while achieving thequality one expects from 5-micronparaffin sections was unrealistic eventhough the bacteria were clearlydemonstrated in both. Whether thetotal expectations are realistic or not,in circumstances such as these it isgenerally in the histotech’s bestinterest to work more closely withthe PI to establish new method-ologies through adaptation of thosefrom other applications.
Acknowledgments:The authors wish to thank Carl L. Nelson, MD,Chairman, UAMS Orthopaedics, and Mark S. Smeltzer,PhD, Associate Professor, UAMS Microbiology, forconceptual and financial support, Charles L. Stewart,UAMS Orthopaedic Research, for technical assistance,Donna Montague, UAMS Orthopaedic Research, for theliterature search, and Nasrin Rahman for help with themanuscript.
25
Fig. 3b – 2-micron GMA section of rabbit skin stained asper Fig. 1. Note the similarity of the color quality ofthe bacteria, the clarity of the 2-micron section, and thefaintness of the counterstain compared to 3a. 250�
Fig. 3a – 5-micron paraffin section of rabbit skin stainedas per Fig. 1. 250�

References:1. Skinner RA, Hickmon SG, Lumpkin CK Jr, Aronson
JA, Nicholas RW. Decalcified bone: twenty years ofsuccessful specimen management. J Histotech.1997;20(3):267-277.
2. Skinner RA, Hickmon SG, Nelson CL, Germer RA.Modified stain for identification of Staphylococcusaureus in osteomyelitis. J Histotech. 1992;15:303-306.
3. Bancroft JD, Cook HC. Manual of HistologicalTechniques and Their Diagnostic Application. NewYork, NY: Churchill Livingstone; 1994:345-347.
4. Exakt Technologies Inc., Oklahoma City, OK.5. Hickmon SG, Skinner RA, Stewart CL, Nelson CL.
Modified gram stain for undecalcified tissue processedinto Kulzer 7200 Resin. The Musculoskeletal InfectionSociety. Snowmass, Col: August 1995.
6. Ruddell CL. Hydroxyethyl methacrylate combinedwith polyethylene glycol 400 and water; an embeddingmedia for routine 1-2 Micron sectioning. Stain Technol.1967;42:119-123.
7. Skinner R. Modified Osheroff and Ruffing: animproved trichrome procedure for glycol methacrylateembedded tissue. J Histotech. 1987;10:249-250.
8. Skinner R, Boylston E.An improved method of alizarinRed-S stain for calcium in glycol methacrylateembedded sections of bone. J Histotech. 1987;10:177-178.
9. JB4 Embedding Kit data Sheet #123. Warrington Penn:Polysciences Inc;1982.
Retiring at theTop of His Game
Vinnie Della Speranza,Scientific Editor
Earlier this year, Dr. Jules Eliasinformed the NSH Board ofDirectors of his plan to retire aseditor of the Journal ofHistotechnology by year’s end.This would end a fifteen yearstewardship of what has becomerecognized worldwide as thepremier journal for Histo-technology, the culmination of adream that Jules set for himselfwhen he accepted the role of editorin 1985. It is my privilege to sharewith our readers some insights intothis remarkable man who has beenone of the thought leaders of our
discipline, and who has madeimmeasurable contributions to thescience of histotechnology.
One of my goals in writing thispiece is to say “thank you” to Jules,my former teacher, mentor, coun-selor, boss and friend, not only formyself but for the many who maynot even be aware of his impact onthe profession. I recall all too wellhow, as a neophyte histotech manyyears ago, I had occasion to hear thenames of some of the pioneers ofthe NSH spoken with reverence,including Lee Luna, DominicEuropa, and Dezna Sheehan, and Iregret to admit that I didn’t have anappreciation back then for who theywere and the significance of theircontributions until they were gone.
I had occasion to meet Jules Elias in1974 as an undergraduate medicaltechnology student at the StateUniversity of New York at StonyBrook, when I took the histo-pathology course he taught in thecurriculum. I remember being struckby his energy and passion forsharing his knowledge, which stim-ulated my interest in histologydespite my having devoted twoyears to train to become a med tech.I casually inquired of him one dayafter class where I could takeadditional histology courses after mygraduation that summer. His enthu-siasm and encouragement set me ona course that would allow me toenjoy a rewarding career of my own.
Like most of us, Dr. Elias began hiscareer at the bench in both researchand clinical environments. Armedwith a bachelor’s degree in Biology,he began he first job at the JewishCenter for Chronic Disease inBrooklyn, N.Y. just a few hours afterhis first child was born in 1959,where he was involved in diabetesresearch, performing blood sugarson dogs and rabbits. A maternityleave in the histology lab at thesame facility prompted him to learnto cut sections. As he aptly pointsout, there were no disposablemicrotome blades back then soone’s success was directly linked toone’s ability to skillfully sharpen a
knife, an art that has all but becomelost today. He worked as a histotechfor four years before taking aposition in electron microscopy.During this time, he began hismaster’s study in hematopathologyat Long Island University, and uponcompletion of his degree in theearly 1960s, he set up a histology labat the federal government’sBrookhaven National Laboratorywhere he prepared animal tissuespreviously injected with tritiatedthymidine to study cell turnover. Heworked with an English researcherwho brought some of his processedblocks back with her to England.The techs there were startled todiscover how easily Jules’s blockscut, and they were eager to learnhow he had prepared his tissues. Helater went on to study leukemiausing both animal and human bonemarrow and spleen. His firstpublished paper appeared in StainTechnology in 1969.
In 1970, Jules joined the StateUniversity of New York at StonyBrook where he establishedlaboratories to work up renal andskeletal muscle biopsies. By the mid-1970s he had established the ThomasA. Edison program for the NSH topermit histotechs in the field to earncredits toward an associate degree bystudying at home and taking examsat the NSH symposium, believingwith conviction that developingtechnologies would require at leastentry level college study forhistotechs. I had the privilege ofrejoining him and his talented staff atthe university in 1979 to prepare thepathology laboratories for the soon-to-open University Hospital &Medical Center at Stony Brook.He earned his doctorate degree in1982, the same year that he wrote hisfirst textbook. In the years thatfollowed, he has written over90 publications, including severaltextbooks and workbooks.
In 1985, Dr. Elias accepted theeditorship of the JOH and sethimself on a course to elevate thecredibility and esteem of this, “our”journal, working hard to attract theinterest and participation of noted
26
Dr. Jules Elias

27
Tissue-Tek®
®
Sakura Finetek U.S.A., Inc.1750 West 214th Street
Torrance, CA 90501 U.S.A.Phone: (800) 725-8723
Tissue-Tek® VIP™ Tissue ProcessorTissue-Tek® DRS 2000™ Slide StainerTissue-Tek® SCA™ CoverslipperTissue-Tek® TEC™ Tissue Embedding ConsoleTissue-Tek® Cryo 2000™ Microtome/Cryostat
Tissue-Tek® Uni-Cassette® SystemTissue-Tek® Mesh Biopsy Cassette SystemTissue-Tek® Accu-Edge® Blade SystemNeutra-Guard™ Aldehyde Control SystemCyto-Tek® CentrifugeAnd more…
The most trusted name in histology.
Instrument by instrument. Specimen by specimen. Cassette after cassette.
Blade after blade. Proven reliability.
Consistent, dependable, long-life performance. Greater value. Sakura Tissue-Tek.
A tradition of quality for over 125 years.
Proven Reliability
Visit our web site atwww.sakuraus.com©1998 Sakura Finetek U.S.A., Inc.
One name found on more products,in more histology labs—worldwide.

28
physicians, researchers, and scholarsin medicine around the world.Today, the journal is recognized asa major vehicle for the reportingof significant technological advancesin histopathology, and has achievedinternational repute as evidencedby the number of agencies indexingits articles. Most would agree thatDr. Elias’s vision, energy and hardwork have put the discipline andthe National Society for Histo-technology on the map. Some haveexpressed that the journal under histutelage lost sight of its readership,and that its contents were toosophisticated for the needs of thetech at the bench. One has only toexamine the journal’s editorialboard to appreciate that it was neverhis intention to abandon the tech atthe bench, but rather to bring themto the level of knowledge theywould need in the decades to come.
Those who have frequented theNSH Symposium/Convention eachyear can attest that Dr. Elias oftenpresents numerous workshops, and isalways eager to share his expertise,despite a rather grueling schedule.By his own admission, one reasonthat he has been such a valuableresource to the profession is that hehas never stopped learning. For all ofthe years that I have known him, hehas always encouraged those aroundhim to read and absorb everythingthat they could get their hands onand to never stop imagining howmethods might be improved.
Since retiring from Stony Brook andmoving to the west coast, Jules hasbeen making time to pursue hisloves; his music and dancing, teach-ing and, of course, his family. His lifeat the moment can hardly be called“retirement.” He presently consultsonce a week at Oregon HealthSciences University, Dept. ofSurgery, instructing residents andothers about research projects. Healso consults for manufacturers ofhistology instrumentation and sup-plies, and he is busy writing a well-ness book. In his free time, he isprincipal clarinetist for his com-munity orchestra. He also plays with
the Gresham Senior Band, and hisown wind quintet, which meetsevery Saturday morning at his homefor rehearsal. It seems clear that hedoesn’t plan to slow down anytimesoon. He tells me that his daughtercomplains that it is a struggle to fitinto his and Renee’s busy schedule.
In a year that has left sports fansstunned and reeling from the voidsleft by the unwelcomed retirementsof greats like Michael Jordan andJohn Elway, it isn’t a reach to saythat like them, Dr. Jules Elias isretiring at the top of his game. Onbehalf of all of us who have reapedthe benefits of your labors and yourcontagious love of the profession,Jules, thank you and Godspeed.
Description andPreliminary Results of a Novel Cassette
System (Tissue-Tek®
Paraform® CassetteSystem)
Chris Diederichsen, HT (ASCP)Stephen Whitlatch, M.D.Department of PathologyGood Samaritan Hospital
Cincinnati, Ohio
AbstractA new and unique sectionablecassette system (Tissue-Tek®
Paraform® Cassette) and preliminaryresults of its use are described. TheParaform® system includes an outerframe similar to a traditional cassettewith an inner soft material insertwith lid. The insert is composed of amaterial possessing two key charac-teristics: It is essentially unaltered byfixation and processing, and it can besectioned in a manner similar to atraditional paraffin block.The softmaterial is compatible with allcommonly used fixatives and solvents.
The tissue is placed in the cassette,oriented, and the lid is closed. The lidfirmly holds the tissue against thebottom of the cassette by a series of
ratchets. By this mechanism, propertissue placement and orientationdetermined at the time of grossing-inis preserved through processing andembedding. At the time ofembedding, the inner material insertwith lid is displaced downward intoan embedding mold. Embedding isachieved without opening the lid ordirectly manipulating the tissue.
A large tissue cassette has beenprototyped and tested. The paraffinblocks produced using the Paraform®
system look similar to traditionalblocks except for the presence of thesoft portion of the cassette within theblock. The paraffin block is faced,removing the bottom portion ofthe cassette. The block is thenmicrotomed in the usual manner.The resulting histologic sectionsare indistinguishable from thoseproduced from a traditional block.Special stains and immuno-histochemical stains are not affectedby the Paraform® system.
The Paraform® system offers severaladvantages compared to the tradi-tional cassette/embedding system.Proper tissue placement andorientation, as determined at thetime of grossing-in, are maintainedthrough processing and embedding.Manipulation of cassette lids andthe tissue itself is no longerperformed, saving time and wearand tear on technologists’ hands.Mechanical manipulation of thehard outer frame is possible offeringthe potential for automation.Designs for biopsy and orientationcassettes (on edge samples such asgall bladder, cyst wall) are inprogress. Clinical studies to quantifythe efficiencies achieved by theParaform® system are planned.
Insert and outer frame, separate and assembled

IntroductionThe need for cost containmentcontinues unabated throughout theclinical laboratory, including histo-logy. In response to these pressures,some steps in the histology processhave been successfully automated inrecent years. Automated tissueprocessing, staining, and cover-slipping are the prime examples.Conversely, embedding is a time-consuming step that has resistedinnovation. Redundancy of manualeffort occurs at the time of grossingwhen tissue is placed in the cassette,and when the processed tissue ismanually removed from the cassetteand placed in an embedding mold.Streamlining this process would behighly desirable.
Recently developed syntheticmaterials resist the chemical environ-ment of fixation and processing, yetpossess a soft consistency similar toparaffin, allowing them to be success-fully microtomed. The Paraform®
cassette system uses one of thesenew materials to successfully addressthis challenge.
Description of SystemThe Paraform® cassette designedfor a single large piece of tissue orseveral large pieces of tissue is
described. The Paraform® cassettesystem has a rigid outer framesimilar to that of a traditionalcassette. The outer frame is easilymanipulated by hand and has aslanted surface for handwriting ormachine printing of an accessionnumber.
An inner insert composed of a softflexible material forms the bottomand inner sides of the cassette. Thesame material forms the lid. Theinsert bottom, sides, and lid arefenestrated similar to a traditionalcassette to allow passage ofsolutions.
Ratchets along the inner side of theinsert permit each corner of the lidto be lowered to the appropriateheight to securely hold the tissue inplace between the lid and the bot-tom of the insert. By this means, theproper placement and orientation ofthe tissue, determined at the time ofgrossing, are maintained throughoutthe remainder of the process.
The inner insert is held in placeby small tabs on the outer frame.To manually embed, the cassetteis placed over an embeddingmold. The insert with lid is pushedas a unit downward which releasesthe insert from the outer frame.The freed insert is pusheddownward until contact is madewith the bottom of the well. Thewell is filled with paraffin, and theblock is released as usual aftercooling.
Preliminary ResultsThe material forming the innerinsert and lid resists the harshchemical environment of fixationand processing. No significantswelling or change in consistencyhas been observed during fixationwith formalin or other commonlyused fixatives. The material is alsoresistant to various decalcificationsolutions. The material has beentested with various processingcycles using xylene, xylenesubstitutes, and acetone, withoutsignificant swelling or change inconsistency.
The paraffin blocks produced usingthe Paraform® cassettes are similarin appearance to traditional blocks,except that the insert is visible inthe block. The material has a softconsistency similar to paraffin,which allows it to be microtomedwithout dulling of blades morequickly than would be expected bycutting traditional blocks.Microtomy of blocks made usingthe Paraform® system requiresminimal change from the usualprocedure. The block is facedwhich removes the bottom of theinsert and exposes the tissue. Afterthis is accomplished, ribbons aremade in the usual manner,mounted, and prepared forstaining.
The material has little affinity forstains. With routine H&E stain,the material may be faintly visibleon the periphery of the slide, butwould likely remain unnoticed if onewere not specifically looking for it.No interference with routine histo-chemical or immunohistochemicalstains has been observed.
The Paraform® system has thepotential to positively impact workflow. Time is saved during the em-bedding step because histo-technologists do not have toreopen cassettes or directlymanipulate tissue. The amount oftime saved may be substantial withcassettes containing multiple piecesof tissue, i.e., prostatic chips, discfragments, etc.
Future DirectionsThe large tissue cassette is designedfor large flat or irregular pieces oftissue (uterus, breast, prostaticchips, autopsy sections, etc.) whichgenerally require only proper tissueplacement in the cassette.Additional cassette designs are inprogress appropriate for smallbiopsy specimens and larger piecesof tissue requiring orientation onedge such as gall bladder wall orcyst wall. The majority of tissueroutinely encountered can likely beappropriately handled by only a fewcassette designs.
Insert and outer frame, side view. Right image displaysdownward displacement for embedding step
Paraform blocks, before and after facing
29

30
Since the Paraform® cassette systemmaintains tissue placement/orienta-tion once the lid is closed, automa-tion of the embedding step becomespossible. Machine operationsrequired include manipulation ofcassettes by means of the rigid outerframe, downward displacement ofthe inner insert into a mold,dispensing of paraffin, and ejectionof the block. A prototype system isin development.
ConclusionThe Paraform® cassette system holdspromise to improve work flow in thehistology laboratory by reducingredundancy in the grossing and em-bedding steps. Time is saved in themanual mode, but greater efficiencyis anticipated by automating theprocess. Time savings can addresssuch issues as total direct costs andthe shortage of trained, experiencedhistotechnologists for both routinework and special techniques.
All in a Day’s Work !Vinnie Della Speranza,
Scientific Editor
All in a Day’s Work! is a salute tothe efforts of histotechs everywhere,those unsung heroes who often gounrecognized for their contributionsto the advancement of health andscience. Please contact the editor ifyou would like to see your workfeatured in this column.
Nowhere is the “art” in histo-technology more apparent thanat Ward’s Natural ScienceEstablishment, Inc. of Rochester,New York. While most of us may notbe familiar with Ward’s, few of us
have gone untouched by thisremarkable facility. Rememberthose frogs you might have dissectedin junior high school, or thosemicroscopic preparations of parasiteovum you had to memorize for theparasit final in college? Well, there isa very good chance that your schoolobtained those materials andcountless others at Ward’s.
Sounds simple enough until you stopand think about the huge volume ofbiologic (and other) specimens andmaterials required to satisfy theneeds of educational facilities aroundthe country, and in fact, the globe!Ward’s is one of only two suppliersfor such material in the country but isunique in that, unlike it’s competitor,Ward’s will custom prepare teachingmaterials to your specifications.Another attribute that is somewhatunique in this modern electronic age,is that you will always speak directlyto a customer service agent at Ward’swhen you call during regular businesshours. So your needs receive theirimmediate attention.
This past Spring, Mary Georger,Manager for the Microscope SlideDepartment at Ward’s, invitedme to visit her workplace. Therethey produce over 600,000 slideseach year, representing over1800 different catalog items rangingfrom Amoebae to Zygnema. Priorto my arrival there, I wonderedwhat could be so special about thisplace, especially as I drove up tothis non-descript building set back
Kidney, H&E, 10�
Kidney, H&E, 20�
Fallopian tube, Keratin, 10�
Fallopian tube, H&E, 20�
Fallopian tube, H&E, 50�
Endocervix, PAS, 20�
Anna Woolston and Kathy Stone checking the finalproduct before shipping.

31
well off the road. I thought that I’dpretty much seen all that there is tosee as far as histology labs go, but Iwould venture to say that Ward’s islike no environment you canpossibly imagine. My tour thererivals any museum I’ve visited, onlybetter because here I had thechance to go behind the scenes towitness this amazing operation.
Speaking of those frogs I men-tioned earlier, during my tourthrough the Preserved Materialssection, we came to a large roomwith stainless steel troughs about30 feet long by 6 feet wide and4 feet deep, one which seemed tocontain a gazillion bull frogs, andother small toads, bringing imagesof Budweiser commercialsimmediately to mind. They will besacrificed and injected with apigmented latex material into theveins and arteries to permit easydemonstration of the circulatorysystem to students. The facility alsoprovides mammals and fish, inaddition to amphibians, for studentcomparative anatomy labs.
In Osteology, bones, includinghuman ones are bleached andreassembled into skeletons. InGeology there literally were rocksand minerals everywhere, waiting tobe catalogued and packaged forshipping. In another area,entymology specimens (insects) areorganized into teaching collections.If you would like a treat, call and askfor their catalogue on CD-ROM.
Ward’s gets its name from itsfounder Henry Ward, a real life“Indiana Jones,” who traveledaround the world seven times, satatop Mount Sinai, survived smallpoxand an Arab desert battle, all beforethe turn of the century. As a youngboy, Henry developed a thirst fortravel and adventure that neverceased. At the age of twenty,Henry went to Europe to tutor aboyhood friend, Charles Wadsworth.Together, they traveled throughoutEurope, then crossed theMediterranean to Egypt anddescended the Nile. The collectionof fossils and minerals Wardgathered during this eight-monthexcursion can be viewed today atBuffalo’s Natural History Museum.Henry financed his studies ingeological studies at the ParisSchool of Mines by selling fossils.
During his travels as a young man,Ward learned that natural scienceresearch was enthusiastically sup-ported in Europe. He was soimpressed with the work he sawthere that he brought talentedosteologists and taxidermists fromFrance and Germany to work forhim in the U.S. When Americancolleges and universities finallycaught “collection fever,” Ward’sNatural Science Establishment hadits formal beginnings and over time,attracted many scientists who wenton to become world famous. In 1862,Vassar Women’s College commis-sioned Ward to prepare a collection,the first one that he would offer forsale, which was assembled on thecampus of the University ofRochester. Among the famouscharacters that Ward came incontact with was William F. Cody,better known as Buffalo Bill,who came to Rochester to engageWard in the preservation of buffaloheads. Ward also did business withP.T. Barnum of circus fame.Barnum’s elephant, Jumbo, wasthe largest in captivity. AfterJumbo’s death, Ward was commis-sioned to mount Jumbo’s skin andskeleton, a project that took almosttwo years, to preserve the 12-foothigh, 14-foot long, 6-ton corpse.
Dubbed the “Great MuseumBuilder,” Henry Ward’s last col-lecting passion was meteorites.His passion took him to Europe,Persia, Mexico, and Columbia atthe age of 71. In the early days ofsupplying museums, taxidermy andpaleontology were the largestdepartments. By the turn of thecentury, many museums hadpreparatory staffs of their own.Then schools began to teachscience, creating the need for allkinds of specimens and teachingaids. Today, the Biology departmentis composed of Preserved Materials,Osteology, Live Materials, Bio-technology, and the MicroscopeSlide Department.
If you think that your lab produceshigh quality slides, you must see theperfection prepared at Ward’sNatural Science Establishment. I hadan opportunity to view a number ofmicroscopic preparations, and thetalent in the laboratories at Ward’swas immediately apparent. TheMicroscope Slide Department iscomposed of Whole Mounts, Botany,Embryology, Zoology, and Histology.Carla and Lori in the embryologysection often prepare whole mountsof entire embryos. Many items areserially sectioned, with absolutely noroom for error. One lost section isdoom for the entire block. Onepopular item, whitefish eggs used todemonstrate the various stages ofmitosis, is prepared here. Threesections of each mitotic stage aremounted on a slide, for a total of
Bob Conlon mounting whole mounts.
Carla Thompson cutting serial sections in theEmbryology Section.

Meet two partners well-equipped for the high-volume demands of today’s histology laboratory.Together, Accu-Edge® DisposableBlades and the Accu-Cut® SRM™ 200Rotary Microtome — both fromTissue-Tek® — create the idealsectioning system.
Accu-Edge® blades, the most widelyused blades for over 20 years, areultrasharp, uniformly consistent,and undisputed in quality —virtually eliminating chattering,distortion, and striation.
With its compact, ergonomic design, the Accu-Cut®
SRM™ 200 minimizes hand stress and optimizesproductivity. (And comes complete
with lateral displacement,specimen orientation, retraction,and trimming.)
Section after section, ribbonafter ribbon, rely on thehardest-working partners intoday’s histology laboratory.
Contact your Sakura salesrepresentative today.Call 1-800-725-8723.Don’t delay.
Visit our web site atwww.sakuraus.com
Proven ReliabilitySakura Finetek U.S.A., Inc.
1750 West 214th StreetTorrance, CA 90501 U.S.A.
Phone: (800) 725-8723
Finally, a microtome that meets the quality of the Accu-Edge® blade.
The perfect partners for precision sectioning.

9 sections per slide. They sell morethan 2,000 of these slides each year,requiring the use of motorizedmicrotomes to get the job done. Theproblem is that none of the com-mercially available motorizedmicrotomes are fast enough, so theyhave adapted sewing machinemotors for their use.
If you are looking for new chal-lenges, come work in histology,where they may be silver staining400 slides at a time, preparing12,000 blood smears, or sectioningcelloidin blocks, a technique manyof us have only read about, on anygiven day. Or try the whole mountsection where Kathy, Anna, Phyllis,or Bob may ask you to dissect outthe mouth parts of grasshoppers.Healthcare advancements in indus-trialized nations make it necessaryfor Ward’s to get many of its speci-mens of infectious agents, includingparasites, from the far reaches of theglobe. In some cases, as with the frogembryology line in the Zoologysection, Ina may be growing her ownaerated fertilized frog’s eggs in thelab for her work at Ward’s. Ofcourse, you won’t find local sourceswhen you need camel fleas so…wellas a matter of fact, where does oneget camel fleas from Mary?
Words really cannot do justice tomy experience at Ward’s. I wish thatI could bring all of you back withme for a visit. I do wish however tocongratulate all of the techsworking with Mary who producethe finest work imaginable. Their
talent and pride shine through inevery specimen they prepare.
Today, Ward’s Natural ScienceEstablishment strives to continue inthe spirit of its founder, with hisinfinite sense of wonder, innovation,and dedication to enlighteningstudents of the natural sciences.All of Ward’s products come with alifetime guarantee. Mary recentlyreceived a frantic call from a clientwho had attempted to clean withxylene over 200 slides of celloidin-embedded material that were about40 years old, but upon receivingthem, she determined that theycouldn’t be salvaged so they will bereplaced with new stock at no costto the client—unbelievablecustomer support in this day andage. I have concluded from my visitthat if you need something Ward’sdoesn’t have, it probably doesn’texist.
If you’d like to learn more aboutWard’s Natural ScienceEstablishment or its product line,you can visit their web site atwww.wardsci.com or call1-800-962-2660.
Special thanks to Mary Georgerfor providing the backgroundinformation used in this article.
Using FrozenSections for High
Throughput TissueAnalysis in the Age
of MolecularPathologyDeborah Lawson
Millennium PharmaceuticalsCambridge, Massachusetts
Why Use Frozens?Preservation of RNA for molecularpathological analysis of disease isbecoming more and more importantas a tool for prediction, diagnosis,and prognosis of human disease.Progress in all areas of medical
research and new drug discoveriesare mainly due to the increasedcapabilities of scientists to analyzecells on a molecular basis; they arelooking at why mutations occur inDNA or RNA to make cells normalor pathological. Frozen sectionspreserve these structures best,sacrificing some morphology to lookat genetic and protein regulation.Utilization of frozen sections allowsus to better understand geneticregulation in tissues by betterpreserving these regulating proteins,enzymes, and cell signaling pieces ofRNA, which give us clues into howdisease processes work.
Many believe that frozen tissuealways looks like Swiss cheese andis loaded with artifact. Not true ifdone properly. Frozen tissue is usedroutinely in industry as a way ofgetting data quickly and efficiently.If frozen properly, tissue can lookalmost as good as paraffin sections.Frozen tissue is useful for doingin situ hybridization, as well asimmunohistochemistry, quickly andefficiently. Freezing has theadvantage of minimizing the loss ofRNA in situ, and it also minimizesthe masking of antigen binding sitesin immunohistochemistry whenlooking for low signal probes andhard-to-stain antibodies.
Tissue can be frozen either unfixedor fixed. An advantage to usingunfixed frozen sections is that tissuedoes not need to go through anytime-consuming processing. Iffreezing is done quickly andefficiently at the correcttemperatures, it has excellentmorphological preservation andlittle artifact. Shrinkage found informalin-fixed, paraffin-embeddedtissue is avoided in frozen tissue soanalysis of structure is more easilyaccomplished, especially whenmeasuring structures such as the sizeof infarct, as in the case of ischemicbrain. Fixed frozen tissue also hasthe advantage of a controlled,minimally fixed cross link inparaformaldehyde so one does nothave to use antigen retrieval as informalin-fixed paraffin sections.
All those who make it happen in the Microscope SlideDepartment at Wards.
33

Want to shorten your turnaroundtime? Freeze everything, thenprocess in paraffin as a backup.
Freezing Unfixed TissueFreezing tissues properly can bedone using a variety of methods.These include the use of dry ice,isopentane over liquid nitrogen, orethanol on dry ice. There areadvantages and disadvantages toeach of these. The method offreezing should be carefullyconsidered, tailoring it to thestructures one wants to examine.
The simplest of the above methodsis to take fresh tissue immediatelyafter excision and freeze it inpowdered dry ice for about5-10 minutes, depending on the sizeof the tissue. Then tissue may betransferred to the cryostat andsectioned unembedded. This tech-nique is very good for isotopicin situ hybridization using lowsignal probes, and works well forrodent tissues, especially brain.Sections are cut and placed ontosuperfrost plus or gold plus slides(Erie Scientific), with no subbingneeded. Slides are then laid flat atroom temperature until the sectionsare just dried onto the slides,collected at –20°C then transferredto –80°C at the end of the cuttingsession for storage. Sections can bestored in tightly closed boxes forup to eight months in some cases.Probes and antibodies must alwaysbe run with proper controls tomake sure no loss of signal hasoccurred with long term storage.
After cutting, tissue can be storedin small labeled plastic whirl-pakbags at –80°C for up to 1 year.Slides can then be removed fromthe –80°C when needed, brought toroom temperature, and fixed inyour fixative of choice, such ascold acetone, ethanol, or para-formaldehyde, depending on theprotocol to be used. The dry icemethod of freezing may producesome artifact, but for screeningtissues quickly, both in a clinicaland research setting, it is farsuperior than simply freezing in the
cryostat. Storage of tissue andslides has the one drawback ofhaving to use up extensive space ina –80°C freezer.
Unfixed tissue can also beembedded in OCT™ if it is smallenough and does not have moistureon the surface. Moisture on thesurface tends to make tissue pullaway from the OCT,™ especiallywhen dealing with brain includingthe attached dura. Never try toembed unfixed brain and then cutit. One is much better off with noembedding at all in the case ofbrain. If using unfixed tissue, theinternal temperature of the cryostatis also an important consideration,taking into account tissue type,species, and age of tissue (adult,postnatal, or embryonic). Ifsectioning adult brain, for example,the optimum cutting temperature is–16° to –18°C, but embryonic brainmay be better at –20°C due to thehigher water content. It is best tofreeze tissue embedded in OCT™rapidly over an ethanol/dry iceslurry, floating cryomolds (TissueTek), or peel away molds in theslurry. Freezing will take minutes.The only drawback to this methodis that writing on the molds tends tocome right off.
Liquid nitrogen-cooled isopentaneproduces the least amount ofartifact but is cumbersome to use.One must use a plastic cup orother vessel that will not crack atthese temperatures. Theisopentane is placed in the cupand the cup is immersed in liquidnitrogen that is placed in a dewar.Muscle biopsies are routinelyfrozen in this way with beautifulresults. The –160°C temperaturesnap freezes and preservesenzymes in the tissue. Brain canalso be done this way, but chill theisopentane only to –120°C using alow-temperature thermometer tomonitor the temperature. Lowertemperatures tend to cracksensitive nervous tissue.
Immersion of unembedded tissue inliquid nitrogen is not a desirable way
to freeze tissue.The tissue will crack,and bubbles from the nitrogen willproduce artifacts. However, if tissueis first embedded in OCT™ anddropped into liquid nitrogen, this willwork fine. Problems with thismethod include difficulty in fishingthe specimen out of the liquidnitrogen quickly, before it over-freezes, and orientation of thespecimen can be difficult because thesample tends to sink to the bottomof the nitrogen while freezing.
Freezing Fixed TissueProcessing fixed tissue for frozensections can be a long process, butfor certain situations whereexcellent results are needed with ahard-to-stain antibody, the resultsare worth it. The fixative of choiceis usually 4.0% paraformaldehydethat is freshly prepared. In our labwe always make all of ourprocessing solutions withdiethylpyrocarbonate (depc)-treated water to better preserveRNA, since we do in situprocessing of all of our specimens.
Equipment• 4.0% paraformaldehyde in
depc/PBS• PBS/depc• 10% sucrose, 20% sucrose,
30% sucrose made in depc/PBS• OCT™ (Sakura Finetek)• Cassettes for processing,
if tracking is necessary• Pencils for labeling cassettes• Permanent markers• Disposable plastic containers• Dissecting instruments of choice• Plastic bags for tissue storage, and
freezer boxes• Aluminum foil• Peel away molds and cryomolds• Latex or nitrile gloves• Lab coat• 95% ethanol, 70% ethanol• brain matrix• powdered dry ice• Safety glasses• 10% bleach• –80°C storage boxes
34

Procedure1. Dissect out tissue and fix in
freshly prepared 4.0%paraformaldehyde for 2-48 hoursat 4°C (depending on size oftissue). This can be done withperfused or unperfused tissue. Forbrain, it is best to slice with abrain matrix before immersionfixation for better infiltration andpreservation. Fixation time willdepend on size of tissue.
2. Rinse tissue at room temperaturein 1X PBS/depc on shaker, with3 changes, 30 minutes each.
3. Place in 10%, 20% and 30%sucrose, respectively, at 4°C untiltissue sinks in each. Can take eachstep up to overnight.
4. Place in OCT™ for an hour toinfiltrate at 4°C.
5. Place in fresh OCT™ and freezeon an ethanol/dry ice slurry.
6. Store well wrapped in foil andplastic bags at –80oC until use.
In ConclusionIn this age of high throughputwork, frozen sections areunderutilized as a tool to get workout faster. Quality does not have tobe compromised in the process, butthe technologist needs to pay care-ful attention to detail in utilizingfreezing techniques. Frozen tissuewill be used more and more in thefuture because of the Chip or Arraytechnology that is being developed.Preservation of RNA for Arrayanalysis, as well as the morpho-logical tissue analysis, will becomepart of the molecular pathologyworkup for us all in the very nearfuture.
AcknowledgmentsI owe the example of freezing in powdered dry ice to my
friend and colleague at Millennium, Pei Ge. I amgrateful for all of her expert advice in the area ofin situ hybridization.
I owe the idea of the importance of the ideas ofimmunohistochemistry and molecular pathology toDr. Jules Elias, whose enthusiastic attitude for thesesubjects has infected me during the past 26 years.
References1. Elias, JM. Immunohistopathology: A Practical
Approach to Diagnosis. Chicago, Ill: ASCP Press;1990.2. Humasen, G. Animal and Tissue Techniques. 3rd ed.
San Francisco, Calif: W.H. Freeman; 1972:Chap 6.
How to Perform anElectronic LiteratureSearch, or Answer the
Question “HasAnyone Ever DoneThis Stain Before?”
Donna Montague, MSUniversity of Arkansas for Medical
Sciences, Orthopaedic Surgery4301 W. Markham St. Slot 644
Little Rock, AR 72205
IntroductionEver been asked this question?Ever asked it yourself? My bossasked me the other day if anyonehad ever published a method fordoing Gram’s stain in plastic (seeassociated article). As I started toanswer his question, it occurred tome that others might have thisproblem arise and need to knowhow to attack it. So, here followsthe attack plan I used that day andsome associated backgroundcomments.
BackgroundManual Method vs. ComputerSearches. In the early SearchizoicEra, you had to find that elusiveStonehenge-like buildingsomewhere on a university campuscalled a library. You’ve been inthem before, those stuffy oldbuildings with thousands of books.In the central prayer place calledthe Reference Section, thesebuildings contain row upon row ofsacred texts like, Annals Index,Biological Abstracts, ChemicalAbstracts, Science Citation Index,Current Contents and the MostHoly, Index Medicus. In order tofind an article on a particular stain,you had to look in each volume ofeach set of abstracts for the stain,by both subject and author. To becomprehensive, you also shouldlook in the index of severalhistology texts (see References andSuggested Reading) for the stainingprocedure and the tissue of interest.These printed procedures shouldhave references that you can track
down. This activity assumes youknow something about the stainand the person associated with theprocedure. You know what happenswhen you assume. After severaldays and several less strands ofhair, you may finally arrive at theconclusion that either (1) NO ONEhas ever done this before or (2) yousimply can’t find any referencesabout this stain. Now what? Cry?Pray? Find another profession?Jump for joy since you’re about tobe famous? Write your article, get itpublished and read in the nextissue’s Letters to the Editor (Elias,1990) you aren’t the first after all?Bummer.
The advent of personal computershas greatly accelerated the searchprocess and decreased the amountof false negative and false positivesearches. The U.S. National Libraryof Medicine (NLM), on the campusof the National Institutes of Health(NIH) in Bethesda, Maryland,houses over 5 million items relatedto biomedical sciences. The person-nel of the NLM created theMEDLARS system and theMEDLINE® database. MEDLINEis a computer-based search devicethat lists citations and abstractsfrom over 4,000 journals (all thoselisted in Index Medicus) publishedfrom 1966 to the present. That’sover 9 million references! This is afree search service, so if you haveaccess to a computer and access tothe worldwide web, you can searchthe journals in this system at theURL www.nlm.nih.gov at noadditional charge. If you want thefull-text version of the article youfind, sometimes you can get itthrough the publisher or NLM for amodest fee. Usually, I print a list ofthe articles the search finds for meand then camp out at my locallibrary until I find all the articles orrun out of bread crumbs, whichevercomes first. Several other searchdatabases are available through theNLM, including compilations ofAIDS clinical trials, chemicals, toxi-cology studies, and many more.Computer searches are, by far, fasterand more thorough.
35

Specific Example or How ToMEDLINE may be searched byAuthor, Subject Heading, Journal,Title, Search Field, or Keyword. Thekeyword search pattern looks forthe specific word (as it is spelled inthe query, see note1) in the Title,Abstract, Registry number word,and MeSH subject headings. Thismethod of searching the databasehas been, in my experience, themost effective strategy; i.e. returnedthe largest number of articles (hits).However, you do have to be sureto use a variety of words to coveryour topic since authors expresstheir ideas and techniques dif-ferently. Also, take advantage of thetruncation symbol offered withMEDLINE to capture varioussuffixes: adjectives as well as nouns,plural as well as singular, etc. Forexample, “pollut” will pick uppollute, polluting, polluted,pollution, and therefore is morecomprehensive than just using theword pollution. Keyword searchescan be combined using Booleanlogic operators “and” and “or.” Thishelps narrow the query to answerthe specific question at hand.
My boss asked, “Has anyone everdone a Gram’s stain in plastic?”
I asked, “What kind of plastic,GMA, MMA, or other?”
He said, “Yeah, any of those.”
There are several keywords to try inour search: “Gram stain,” “glycolmethacrylate,” “plastic,” and“histology.” Type these into thecomputer search page and you’ll getthe following hits from MEDLINE1966 to present:
Table 1. Keyword Search
Keyword Hits
Gram stain 979
glycol methacrylate 362
plastic 24,608
histology 26,894
Great! Now what. Do I have toread all these abstracts? No. Nowyou narrow your search fields usinglogic. Do any of the articles listboth “Gram stain” and “glycolmethacrylate” as keywords in theirtitle or abstract? Repeat thisquestion with all keywords in allcombinations. The results are:
Table 2. Narrowing the Search
Combined Search Terms Hits
Gram stain AND glycolmethacrylate 02
Gram stain AND plastic 3
Gram stain AND histology 14
Glycol methacrylate OR plastic 24,970
Plastic AND histology 97
Gram stain AND (glycolmethacrylate OR plastic) 3
Gram stain AND (glycol methacrylate OR plastic OR histology) 17
ConclusionSo now all I have to look at andread are 20 article abstracts to seeif any of them are related to thequestion my boss originally asked.What was that again? “Has anyoneever done a Gram’s stain onsections from tissues or tissueimplant composites embedded inany kind of plastic media?” No.Nobody has ever publishedanything in the journals covered byMEDLINE on this subject from1966 to the present.
1 Spelling is important. Ask anyone who has tried to“unsuscribe” from the Histonet. DCM
2 Notice in Table 1 that Gram stain returned 979 hits andthat glycol methacrylate returned 362 hits. If youlooked at each of these abstracts, all 1341, you’d beblind. Asking the computer to compare all the abstractsand list only those with BOTH Gram stain AND glycolmethacrylate in them nets you 0 abstracts. The patternof combined queries is referred to as Boolean logic.
AcknowledgmentsThanks are in order to Ms. Rena Sheffer of theUniversity of Arkansas Medical Sciences Library forpointing me to the National Library of Medicine’swebsite. We have a direct link to MEDLINE from ourdesktop computers through the library on campus. I useit daily. According to the NLM, over 350,000 literaturesearches are done using MEDLINE each day. A specialthank you goes out to the lady who taught the best andmost helpful course I took in college, Intro. to LibraryResearch and Resources, Mrs. Kathy Sanders.
References and Suggested Reading1. Elias JM. Letters to the editor – A bridge over
troubled waters. J Histotech. 1990;13(4):247.2. National Library of Medicine website: Available at:
www.nlm.nih.gov3. Carson FL. Histotechnology – A Self-Instructional Text.
2nd ed. Chicago, Ill:ASCP Press; 1997.4. Bancroft JD, Stevens A. Theory and Practice of
Histological Techniques. 4th ed. New York, NY:Churchill Livingstone; 1994.
Histonet:The List Server for
HistotechnologyLinda R. Margraf, MD
Associate Professor of Pathologyand Histonet Administrator
Herbert K. Hagler, PhDAssociate Professor of Pathology
and Histonet AdministratorUniversity of Texas
Southwestern Medical Centerat Dallas
Dallas, Texas 75235
IntroductionHave you ever had one of thesedays? Two technicians have called insick. One of the pathologists, visiblyagitated, has just returned a tray of
CorrectionHisto-Logic wishes to thankDr. Roy Korson of Burlington, VTfor informing us of an error thatappeared in the timeline“Countdown to the 21st Century”in our Spring ’99 issue. Wereported erroneously that WilliamHarvey described the circulationof blood in 1828. Dr. Korsonpoints out that “Wm. Harvey livedfrom 1578 – 1657 and that hisfamous treatise on the motion ofthe heart and the circulation of theblood first appeared in 1628.” Itseems that Harvey’s ideas wereslow to catch on, and experimentalproof confirming his theoriesdidn’t appear until 1828, twohundred years later, according toDr. Korson. This illustrates theneed to verify informationobtained from the internet and wethank Dr. Korson for sharing hisinsights on the matter.
36

the diagnostic gastrointestinalbiopsy slides to the lab. Hegrumbles that the slides have a hor-rible bubble artifact and he can’tinterpret them. They will need to berepeated as soon as possible. Thechief of Pathology was just on thephone wanting to know if you canperform an alcian yellow stain byWednesday, only problem is you’venever heard of an alcian yellowstain and it is not in the books onthe shelf. Now, one of the universityresearchers has come into the labsaying he needs you to find anantibody for interleukin-2 immuno-histochemistry that will work in rattissues. What on earth are you todo? One easy and fast (and free)solution is to turn to Histonet, theelectronic mail (email) list serverthat specifically addresses issues inhistotechnology. This article willdescribe what a list server is andhow it can improve the function ofyour histology or researchlaboratory. It will describe Histonet,one of the first and still most activelists devoted to the broad range oftopics in histotechnology.
List Server BasicsA list server is simply a computerthat runs software which will receiveincoming email messages and auto-matically reroute a copy of eachmessage to everyone on the sub-scriber list. Email uses the vastexpanse of the internet to allowalmost instantaneous communi-cation between networkedcomputers around the world. Somelist servers are designed to dis-seminate information only to thesubscribers on the list. Other lists,
however, encourage ongoing dialogbetween the subscribers so thatanyone with comments about atopic can contribute to the discus-sion. This allows a researcher in NewZealand to get input from labs inJapan, Germany, Great Britain, andCalifornia for the best parameters toset up a new immunostainingprotocol without ever leaving hisdesk. Most list servers allow thesubscribers to receive the messagesimmediately as they filter throughthe server (“real time”) or compiledas a batch of messages, known as adigest, usually issued every 24 hours.Many list servers have additionalfunctions, such as archives and FAQs(frequently asked questions) files soprevious comments regarding atopic can be retrieved. There arenow active lists covering a vast rangeof topics from archeology to zebrafish. Medical lists have become verypopular with physicians and medicalorganizations. Most medical spec-ialties have at least one email listdiscussing the optimal diagnoses,treatment modalities, and latestresearch findings in their area ofinterest. Several lists are nowdedicated to topics pertaining tomedical technology and selectedareas in histopathology.
There are a few important words ofcaution to consider before jumpingimmediately on a list. Lists, onoccasion, can be the targets ofspam or unsolicited mailings thatcan become irritating, if notfrustrating, to eliminate. Most listspertaining to medical andprofessional topics are fairly free ofthis problem compared to listscovering more general topics. It isimportant to remember that simplyreading an email message cannotcause a virus to infect your system,however, attachments should becarefully screened with an up-to-date virus detection program priorto opening. Some lists, such asHistonet, block attachments fromgoing through the system tominimize the risks to subscribers.And, as is always a concern withinformation posted on the internet,the validity of the information or
methodologies presented on a listshould be verified before makingany changes in your laboratory.
Each email list has its own set ofrules and operating protocols so itis best to remain a silent observerfor a while before jumping into theconversations on-line. Some listswill aggressively spurn any obviousneophytes or “newbies.” Email listsdiffer from chat rooms in that theaudience remains fairly stable, andmost subscribers only comment ontopics of shared interests. Histonethas been fortunate enough toattract a number of notedauthorities in histology who willtake the time to provide detailedanswers to questions about theirparticular areas of interest. Thisincludes people who can readilyanswer questions about eliminatingbubble artifact in biopsies, sendprotocols for alcian yellow stains,and find antibodies for immuno-stains on rat tissue.
HistonetThe Histonet list, which has been inoperation since January of 1996,now has over 1100 subscribers fromall over the world. Subscribersinclude hospital employees frommajor urban centers and small,isolated locales, universityresearchers, botanists, laboratoryworkers in government agencies,veterinary facilities, and a widevariety of commercial industrialventures. The questions promptingtopics of discussion are as diverse asthe participants. On a given day, adiscussion of the best procedures forantigen retrieval for immuno-histochemistry may be interspersedwith comments regarding dinosaurbone sectioning, and butterflypreservation methods. Most topicshowever, pertain to optimizing rou-tine diagnostic histologicprocedures, equipment selection,laboratory management, andhistotechnologist employmentopportunities.
Histonet is run using hardware andsoftware owned by the University ofTexas Southwestern Medical School
Linda Margraf, MD and Herb Hagler, PhD keepHistonet up and running.
37

Department of Pathology in Dallas,Texas. Currently, Histonet uses theLISTSTAR software from Quarter-deck Corporation (California) and,with the present number of sub-scribers, it processes more than50,000 outbound messages a day.A single old Macintosh, a cast-offfrom a departmental computerupgrade, busily receives and dis-tributes the messages around theclock to the subscribers fromnearly fifty countries around theglobe. The system is not withoutperils. Every one of the fairlyfrequent glitches in the University’sown servers or power supplies,affectionately known as “inter-mittent power interruptions” senda ripple of problems through thesystem, creating repeatingmessages or temporary “quietspells.” By frequently monitoringthe system, most of the problemsare never noticed by the sub-scribers. Additional challenges tothe list administrators includekeeping the address lists updated(it is amazing how frequentlypeople change addresses), andassisting in the spelling of the word“SUBSCRIBE.” Perhaps the mostimportant challenge in keeping a listsuch as Histonet running, is deter-mining the appropriate focus andcontent of the list’s messages. Asidefrom assuring the list remain free ofunsolicited advertising, theadministrators have allowed thesubscribers to determine what theyfeel is an appropriate use of theforum. Histonet appears to succeedso well as an open, friendlyexchange of information because ithas been embraced by a congenialand knowledgeable community ofhistotechnologists. Though contro-versies regarding the appropriate-ness of messages occasionally arise,they rarely detract from the use-fulness of the service. It is hoped theprogram (and the poor, tired, oldMacintosh) will keep running foryears to come.
If you are interested in subscribingto Histonet, send an email [email protected] put “subscribe” (spelled
correctly (!) and without quotationmarks) in the SUBJECT LINE ofthe message. If you have anyquestions about Histonet, pleasecontact Linda Margraf, MD [email protected].
WHAT ISCYTOLOGYANYWAY?
Kathleen A. DaSilva, SCT(ASCP)Cytology SupervisorUniversity Hospital Stony Brook, N.Y.
Caller: Cytology Department,please.
Operator: Psychology Department.Let me connect you.
Caller: No, not the PsychologyDepartment, thecytology department,C-Y-T-O-L-O-G-Y.
Operator: Oh, the cytologydepartment. Let meconnect you.
I’ve lost count how many timesI have heard that scenario duringmy career. In fact I am constantlyamazed that even some fellow medi-cal professionals are not aware ofwhat a cytologist really does. Hope-fully this article will shed some lighton the mystery of what cytology isabout and how far the field hascome over the past 50 years.
It all began with a doctor by thename of George Papanicolaou.Dr. Papanicolaou was born inGreece in 1883 and immigrated toAmerica in 1913. He obtainedemployment with the Department ofAnatomy at Cornell UniversityMedical College. While studying themenstrual cycle in guinea pigs,Dr. Papanicolaou obtained cellsamples from the vagina using apediatric speculum. In studying thesquamous cells, he found changes intheir morphology that correspondedto the different phases of themenstrual cycle.
Dr. Papanicolaou began to applywhat he had learned about the mor-phologic cell changes in guinea pigsand use it to study the hormonalstatus of human patients. He joinedforces with a gynecologist namedHerbert Traut. Together they beganto collect human samples, butDr. Papanicolaou soon made astartling discovery. He found bizarrecells in the smear from a womanwith cervical cancer. He thenrealized that with this new technique,he was not only able to study thehormonal status of patients but wasalso able to detect cervical cancer inasymptomatic patients at an earlyand curable stage! Their findingswere published in the AmericanJournal of Obstetrics andGynecology in 1941.
Since that landmark paper in 1941there has been a greater than70% decline in the cervical cancerdeath rate. The Pap smear has beensuch a success that, until recently, thisscreening technique has remainedvirtually unchanged since 1941.
Specimens are obtained using aspeculum that is inserted into thevagina to permit the cervix to bevisualized. A sample is taken usingany one of a variety of collectiondevices that have been developedover the years, including the Ayrespatula, which was introduced in1944, the cytobrush which appearedin the 1980s, or the “broom” orpapette which is the most recentdevice to appear on the scene. TheFig 1. Dr. George Papanicolaou
38

collection device is inserted into thecervical os, or opening, and rotatedto gently collect superficial cellsfrom the cervix and endocervix. Thecells are then smeared onto a glassslide and fixed immediately. Thefixatives of choice include ethanol(ethyl alcohol), which, although itprovides better nuclear detail, isinconvenient to transport, or a sprayfixative that is used to coat the cellson the slides which are much easierand less hazardous to transport. Thefixed slides are then sent off to thecytology lab for processing.
At the laboratory the slidesare stained with the traditionalPapanicolaou stain, a stainingmethod devised by Dr. Papanicolaouhimself, specifically for Pap smears.The Pap stain is a modification ofthe conventional hematoxylin-eosin(H&E) stain. Alcohol-basedcounterstains (OG & EA) are usedto highlight variations in cellmorphology (ie. cell maturity andmetabolic activity). There are severalbrands of these Pap stains on themarket, which are slight variants ofDr. Pap’s original formula,depending on how intense a bluestain you prefer. Over the years,there have been a number of refine-ments in cyto prep technique in-cluding the cytospin for hypocellularbody fluids, to automatic stainersand coverslippers, which havehelped tremendously to reduceturnaround time.
Most recently, we have witnessed theappearance of what is probably themost significant refinement to the
Pap smear to occur since its incep-tion, the development of monolayertechnology. Instead of a physiciansmearing the cells onto a glass slideafter collection, the sample is placedinto a liquid fixative solution. In thelaboratory, the sample may beplaced onto an instrument toprepare the monolayer preparation,or it may be prepared by hand,depending upon the technology thata laboratory chooses to use. The useof monolayer technology offerswonderful advantages that increasethe likelihood that abnormal cellswill be discovered by the cytotechduring screening. First, by avoidingthe use of smears prepared duringthe patient’s pelvic exam, we caneliminate variability in smearthickness and overall qualityinherent in a method that hastraditionally been performed bymany different physicians. Withmonolayer technology, all patientsamples are consistently prepared,regardless of who the patient’sphysician is. Another importantadvantage is that monolayertechnology eliminates blood,inflammation, and mucus commonlyfound in smears, which can hinderinterpretation. But perhaps mostimportant of all, it has beendiscovered that with the traditionalPap smear, up to 80% of thecollected cells are discarded on thecollection device. With monolayertechnology, the cells are transferredinto the preservative fluid, and thecollection device can be sent to thelaboratory as well. As a result, thecellular yield and the potential fordiscovering an abnormality isgreatly increased.
After the slides are stained andcoverslipped they are sent tothe cytologist for screening.The cytologist must look forchanges in cell morphology, whichmay indicate the presence of pre-cancerous or cancerous lesions.In essence, the cytologist must lookat every single cell on the slide,the equivalent of looking for aneedle in a haystack, in order to becertain that any abnormal cells thatmay be present are found andidentified. While the method acytologist uses to screen a slidehasn’t changed much over theyears, the microscopes that they usehave gone through a number ofchanges over the last 5 years. Mostsignificantly, modern microscopesare much more ergonomic, whichmakes it possible to avoid job-related maladies, such as carpaltunnel syndrome, that can comefrom hours spent at a microscopescreening slides. Newest on thescene, cytology has witnessed theappearance of computerizedrescreening devices, which are, withthe exception of one instrument,FDA approved only for qualitycontrol (rescreening a slidepreviously screened by acytologist). While there are somewho argue that computerrescreening affords greaterprotection to the patient becausehumans may fail to find abnormalcells because of fatigue, eyestrain,or other distractions, microscopicscreening, regardless of how it isperformed, can only be as good asthe slide being screened.A computer is no better at findingabnormal cells in a poorly madeslide than a human is, whichreinforces the importance and valueof monolayer technology.
Cytodiagnosis can be conducted onsamples from virtually any part ofthe body, utilizing a variety oftechniques to isolate cells from bodyfluids, mucus linings, and thesampling of even deep-seatedlesions with fine needle aspirationbiopsy, all of which offer the patientimportant alternatives to surgery fordiagnosis.
Fig 2. Pap smear collection devices, courtesy ofMedical University of South Carolina, Charleston SC
Fig 3. Conventional pap smear. 20�
39

Cytology has come a long way injust 50 short years. The value ofcytodiagnosis as an inexpensive toolto identify cellular abnormalities hasbeen embraced by the medicalcommunity, and in fact is relied uponquite heavily today. With thetechnological advances that haveoccurred in recent years and thoseappearing on the horizon, it wouldseem that cytology has a very brightfuture ahead of it.
References:1. Keebler CM, Somark TM. The Annual of
Cytotechnology. Chicago, Ill: American Society ofClinical Pathologists; 1993: 6-7, 411-448.
2. Allen SA. A Guide to Cytopreparation. AmericanSociety for Cytotechnology; 1995:59-93, 95-111.
3. A Communication of the Inernational Academyof Cytology. Cyto Paths, Issue 8, Spring 1999.Acta Cytologica. March-April 1993;43(1).
NSHers PartyLike It’s 1999
The National Society forHistotechnology (NSH) choseProvidence, Rhode Island for thisyear’s truly historic event — the 26thand last NSH meeting of the century.
Sakura, Allegiance, and RichardAllen were sponsors of anexciting Millennium Party held onOctober 16 that attracted more than900 partygoers. Five differentdecades were saluted — the 50sthrough the 90s — with colorfulcostumes, including varsity sweatersreminiscent of the 50s and Beachstyles of the 60s. Life-size cardboardcut-outs of James Dean, MarilynMonroe, Austin Powers, and othernotables represented the decadesand added to the fun.
In addition to a delectable buffetand bracing refreshments, populargames and activities kept everyonemoving — from Twister to BungeeRun, a Hula Hoop Contest toDance Lessons (Swing, ElectricSlide, Charleston), pool games tohair braiding. Even tattooing(fake ones, of course). What’s more,four lucky NSHers were selectedto enter a unique Cash Cube filledwith tons of swirling money. Theparticipants had seconds to grabas much cash as they could. When
the event was over, more than$800 had been given away!
An incredible live performanceby Takashi Tsuzuki from Sakuramade everyone believe that Elviswas truly in the house. And atmidnight, partygoers counteddown to the new century — outwith the old millennium and inwith the new — as balloonscascaded down from the ceiling.It was a great ending to a terrificparty.
Fig. 4. Monolayer preparation. 20�
40
Safe, efficient, economical• Certified technology for treating formalin waste• Complies with federal, state, and local ordinances
Four convenient product formsNeutralex™
• Premeasured powder pouch neutralizes 1 gallon in 15 minutes
Neutra-Pads™
• Grossing pad absorbs and neutralizes 10% formalinNeutra-Wipes™
• Convenient pop-up dispensing containerprovides fast accessibility to wipes
Neutra-Form™
• Fast, effective control agent for accidentalaldehyde spills
Call (800)725-8723 for more information.
Proven Reliability
©1998 Sakura Finetek U.S.A., Inc.
Neutralize the problem of formalin disposal and cleanup
Sakura
Tissue-Tek®
NEUTRA-GUARD™
Aldehyde Control System
Sakura Finetek U.S.A., Inc.Phone: (800) 725-8723

4141
Proven ReliabilitySakura Finetek U.S.A., Inc.
1750 West 214th StreetTorrance, CA 90501 U.S.A.
Phone: (800) 725-8723
Visit our web site at www.sakuraus.com
®
PULL. SNAP.FIX. PEEL.
Slide preparation made simple.
Obtain a suitably prepared liquid specimen.Pull the plunger until it locks in place todraw the sample. Snap the assembly open andtransfer the filter to a slide. Fix, blot, andallow to dry. Peel the filter from the slide.Four simple steps to high-quality, high-yield,low-cost monolayer slides.
With the Cyto-Tek® MonoPrep™ System,the high technology lies in the patenteddesign, not in the use, making the processeasy and affordable, and the resultsconsistent. For fine needle aspirates, urines,
bronchial washings and sputum, pleural andperitoneal cavity fluids, and CSF.Delivers an acceptableslide even from thesparsest urines.
Contact your Sakurasales representative today to schedule ademonstration.
Call 1-800-725-8723.Don’t delay. MonoPrep™ Slide: Sputum
Cyto-Tek® MonoPrep™ System
PULL. SNAP. FIX. PEEL.

42
Jan 21 University of Texas Health Sciences Center/San AntonioTeleconference, 12:00 pm Central TimeSpeaker: Steven Slap, MPhil, MA
“Microwave Processing Techniques for Microscopy”1-800-982-8868
Feb 18 University of Texas Health Sciences Center/San AntonioTeleconference, 12:00 pm Central TimeSpeaker: Gwendolyn Goss, BA, HT(ASCP)
“Hollande’s Solution as a Routine Fixative”1-800-982-8868
Mar 4 Colorado Society for HistotechnologySite: University of Colorado Health Science CenterContact: Sara Williams
303-861-6177Email: [email protected]
Mar 10 American Society of Clinical PathologistsTeleconference, 12:00 pm Central TimeSpeaker: Glenda Hoye, HT(ASCP)
“Reviewing Connective Tissue StainProcedures and Results”—for more details, contactASCP at (312) 738-1336 or Email [email protected]
Mar 11 Arkansas Society of HistotechnologySite: Baptist Medical Center, Little Rock, ARContact: Louellen McLemore
2394 Grant 73, Sheridan, AR 72150(W) 870-541-7541 (H) 870-942-4483
Mar 15-18 Florida Society of Histotechnology and NSH Region III MeetingSite: Delta Orlando Resort, Maingate Universal Studios,
Orlando, FLContact: Jerry Santiago
Veterans Affairs Medical Center1601 SW Archer Road (113), Gainesville, FL 32608(W) 352-376-1611 ext. 6432
Mar 17 University of Texas Health Sciences Center/San AntonioTeleconference, 12:00 pm Central TimeSpeaker: Clifford M. Chapman, MS,HTL(ASCP)
“Dermatopathology: A Guide for theHistotechnologist”1-800-982-8868
Mar 17-18 Kentucky Society of Histotechnology SymposiumSite: Holiday Inn, Louisville, KYContact: Renee Matherly
502-852-5587Email:[email protected]
Mar 17-19 NSH Region II MeetingSite: Holiday Inn & Holidome,
Downtown Williamsburg, VAContact: Frances Freund
804-288-6172 or 804-267-8134 (weekdays 9:00am-4:00pm)Fax: 804-267-8831
Mar 31 - New York State Histotechnological SocietyApr 1 Site: Holiday Inn, Saratoga Springs, NY
Contact: Sandra CummingsPO Box 81, Esperance, NY 12066(W) 518-875-6304Email: [email protected]
Apr 7 American Society of Clinical PathologistsTeleconference, 12:00 pm Central TimeSpeaker: Gwendolyn Goss, HT(ASCP)
“Regulations and Liabilities – Safeguarding theLaboratory Professional and Pathologist”—for more details, contact ASCP at (312) 738-1336 orEmail [email protected]
Apr 8-11 American Society of Clinical PathologistsSpring 2000 meeting—Boston, MAfor more details, contact ASCP at (312) 738-1336 or Email [email protected]
Apr 13-15 Texas Society for Histotechnology State MeetingSite: Camino Real Hotel, El Paso, TXContact: Kathy Dwyer
(W) 214-947-3538 (H) 972-223-5105May 11-13 Histology Society of Ohio State Meeting
Site: Clarion Westgate, Toledo, OHContact: Susan Black
5526 Whiteford Road, Sylvania, OH 43560(H) 419-885-8266 (W) 419-471-3702Fax: 419-479-6916Email: [email protected]
May 17-21 California Society for HistotechnologySymposium/ConventionSite: Doubletree Hotel, San Jose, CAContact: Linda McGlothlen
2325 Brindlewood Dr., Rancho Cordova, CA 95670(H) 916-635-3240 (W) 916-734-2534Email: [email protected]
May 18-20 Georgia Society for HistotechnologySite: The Georgia Center,
University of Georgia, Athens, GAContact: Connie Wavrin
(H) 770-452-8310 (W) 770-686-2385Email: [email protected]
May 18-20 Illinois Society for Histotechnologists State MeetingSite: Radisson Hotel, Schaumburg, ILContact: Cathy Locallo
Anatomic Pathology, University of Chicago Hospital5841 S Maryland Ave MC6101, Chicago, IL 60637(W) 773-702-8492Email: [email protected]
May 19-20 Missouri Society for HistotechnologySite: Elms Resort and SPA
Excelsior Springs, MOContact: Janet Kliethelmes
913-339-0484Jun 2 American Society of Clinical Pathologists
Teleconference: 12:00 pm Central TimeSpeaker: Richard W. Brown, MD
“Special Stains in the Histology Laboratory –an Update,”—for more details, contact ASCP at(312) 738-1336 or Email [email protected]
Jun 8-10 Arizona Society for HistotechnologySite: Doubletree Guest Suites, Phoenix, AZContact: Ethel Macrea
Ventana Medical Systems, Inc.3865 N. Business Center Drive, Tucson, AZ 85705(W) 520-690-2739Email: [email protected]
Jun 16 University of Texas Health Sciences Center/San AntonioTeleconference, 12:00 pm Central TimeSpeaker: Fiona E. Craig, MD
“Bone Marrow Specimen”1-800-982-8868
Sept 16-21 NSH SYMPOSIUM/CONVENTIONSite: Milwaukee, WisconsinContact: NSH Office
4201 Northview Drive, Suite 502Bowie, MD 20716-2604301-262-6221 Fax: 301-262-9188Email: [email protected] page: www.nsh.org
Oct 14-19 American Society of Clinical PathologistsFall 2000 meeting—San Diego, CASan Diego Marriott Hotelfor more details, contact ASCP at (312) 738-1336 orEmail [email protected]
Mark Your Calendar!Educational Opportunities in 2000

43
NEXT…NOW!
Sakura Finetek U.S.A., Inc.1750 West 214th Street
Torrance, CA 90501 U.S.A.Phone: (800) 725-8723Proven Reliability
Sakura Tissue-Tek® DRS™ 2000 Slide Stainer
©1998 Sakura Finetek U.S.A., Inc. Visit our web site at sakuraus.com
Stain multiple, different batchesat the same time…any timeWhy wait? The Tissue-Tek® DRS™ 2000Slide Stainer works the way you do. WithIntelligent Loading, the advanced computer letsyou load and stage multiple staining protocols atthe same time. Up to 11 groups of 40 slides forsingle methods. Select the program by name andadd baskets. Then walk away.
With 27 reservoirs and one drying station, theTissue-Tek® DRS™ 2000 Slide Stainer increasesproductivity and efficiency in a 6-sq-ft, space-saving, ingenious two-level design. The slide basketis totally compatible with the Tissue-Tek® SCA™Coverslipper for even greater efficiency.
Up to 20 methods,up to 50 stepsEach protocol can be programmed to perform up to 50 different user-determined steps.Each step can be precisely controlled for timing,agitation, and wash. Even define individualprogram and reagent names.
With Intelligent Loading, theTissue-Tek®
DRS™ 2000 Slide Stainer is a simply smarterinstrument—and instrument decision—for unsurpassed productivity andconsistency slide after slide,shift after shift.
Contact your Sakura Sales Specialist for more information.
®

To receive your own copy of Histo-Logic,® or to have someone added to themailing list, submit home address to: Sakura Finetek U.S.A., Inc.,1750 West 214th Street, Torrance, CA 90501.
The editor wishes to solicit information, questions, and articles relating tohistotechnology. Submit these to: Vinnie Della Speranza, Histo-Logic Editor,165 Ashley Avenue, Suite 309, Charleston, SC 29425. Articles, photographs,etc, will not be returned unless requested in writing when they are submitted.
BULK RATEU.S. POSTAGE
PAID<TO COME><TO COME>
Sakura Finetek U.S.A., Inc.1750 West 214th StreetTorrance, California 90501
HISTOLOGIC ®
T e c h n i c a l B u l l e t i n f o r H i s t o t e c h n o l o g y
®
NATIONAL SOCIETY FOR HISTOTECHNOLOGYAPPLICATION FOR MEMBERSHIP
Membership Year: June 1 – May 31 (renewal each May)
(PLEASE PRINT CLEARLY)
Social Security No. Lab Supervisor YES NO
Name
Home Address
City State Zip
Country Home Phone ( )
Place of Employment
Department
Work Address
City St./Prov. Zip
Country Work Phone ( ) Ext.
State Histology License No. (if applicable)
Student Membership(program director’s signature)
Mail information to: Home Address Work Address
INDICATECHECK ALL APPLICABLE BOXES: 1-Primary 2-Secondary
HT (ASCP) AA UniversityHTL (ASCP) BA/BS HospitalMT (ASCP) MA/MS Private LabCT (ASCP) PhD VeterinaryRT (CSLT) MD MarineART (CSLT) DVM BotanyOther Other EMNot Certified Research
Industrial
ANNUAL DUES: $40.00 STUDENT DUES: $20.00Half year dues ($20.00 New Member; $10.00 Student) applies fromJanuary to May only, with renewal June 1st at the yearly rate.NSH membership includes a subscription to the Journal of Histotechnology,published March, June, September, and December. NSH will apply $10.00 ofyour dues to the journal subscription.Remit fee with application, in US currency only.Mail to: NSH, 4201 Northview Drive, Suite 502 Bowie, MD 20716-2604Referred by NSH Member: (Name)
(Optional)
Payment Information: Check payable to National Society for Histotechnology Credit Card(Funds must be drawn in U.S. dollars on a U.S. bank)
Visa/Master Card Number Expiration Date: Month Year
Print Cardholder’s Name Amount to be charged
Signature Date
44