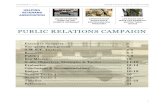
Helping High Risk Patients 20,000 Days Campaign Learning Session 3 11-12 March 2013
description
Transcript of Helping High Risk Patients 20,000 Days Campaign Learning Session 3 11-12 March 2013
-
Helping High Risk Patients
20,000 Days Campaign Learning Session 3 11-12 March 2013
Clinical Champion:Dr Harley Aish
Team Members:Damien Hannah (Localities); John Streeter (ProCare); Josey Lawrence (ProCare); Kate Moodabe (Localities); Keith Crump (ProCare); Nick Swain (ProCare/GAIHN); Pauline Sanders-Telfer; Louise McCarthy (GAIHN); Sharon Pearce
20,000 Days Support:Ian Hutchby (Improvement Advisor)Monique Davies (Project Manager)
-
Our project will.We aim to provide coordinated planned management of our identified high risk primary care patients reducing the demand for unplanned hospital admissions and bed days by 10% (1625 bed days)
Our targeted intervention is the development of a locality based primary /secondary physician role based in primary care with a focus of supporting general practitioners to improve the management of high risk medical patients with long term conditions. This is underway through the Localities initiatives via our Strategic Project Management Office.
Long term goal of each primary care locality having a designated medical team with a primary/secondary care physician working between the services so that the clinical network relationship is built around the patient journey not dislocated at the point of admission and discharge Improved management of patients identified with the PRM tool, who are at high risk of readmission as measured by reduction in predicted bed days
The development of physician clinics within primary care whereby the physician can review patient management with the primary care team and review specific patient care if appropriate
Improved and more appropriate referral to secondary care specialist services
Development of targeted continuing professional development for primary care teams
-
Who are High Risk Patients?.....Patients discharged from Counties facilities are allocated a risk score. The PARR algorithm looks at discharges in the previous month and uses criteria such as age, gender, ethnicity, deprivation score, distance to hospital from the home, and the number of admissions in the last 12 months as well as the associated principal and secondary diagnoses. Based on these criteria, a risk score is allocated. This score gives a percentage chance, or probability, of an unplanned readmission for that particular patient within 12 months.
The PARR scores for patients discharged in the previous month are sent to PHOs on the 5th day of each month. PHOs and practices then use the lists to identify patients who are both at high risk of readmission to hospital, and are amenable to treatment or other intervention. The cut-off score is currently nominated as 30%. Patients with a score of 30% or higher are classified as high risk.
-
High Risk Patients - Their GPs Location
The following table groups high risk patients according to where their GP is located:
**Enrolments per PHO register as at 30 September 2012Sharon Pearce: Counties Manukau Decision Support
High Risk Patients**Total Enrolments% of All High Risk Patients% of Total Enrolments in LocalityManukau2,728164,28436%1.7%Mangere/Otara2,218141,33130%1.6%
Eastern1,028107,11114%1.4%
Franklin60946,0988%1.3%Enrolled elsewhere93312%TOTAL7,516
-
Ethnicity of our High Risk PatientsSharon Pearce: Counties Manukau Decision Support48% of HR patients are of Maaori or Pacific ethnicity
Ethnic GroupHigh Risk Patients%European3,17242%Pacific2,18529%Maaori1,43719%Asian5718%Other/Unknown1512%TOTAL7,516100%
-
Driver Diagram
-
Change Packages
-
Predictive Risk Modelling Flow Chart
-
Categories for Triage of HRI
-
Most Successful PDSA Cycles?
PDSA: Otara GP Practice The Otara GP practice nurses completed a (VHIU) RAG assessment with 11 of the 23 HR patients identified for their practice in the previous month. The PDSA prediction found to be correct, 50% of patients were amenable to an intervention. Next PDSA: to repeat using the Trigger Tool in conjunction with the RAG form. Ask if VHIU for assistance with training in methodology for the nurses
PDSA: GPs doing the Identification of Contributors (Condition complexity, self management, palliative care, social determinants, mental health, other)
-
Measures SummaryMeasures related to AimGraphs of key measures- Which of your run charts would you give to senior leadership to use?Include Collaborative Dashboard
Ian?
-
Primary Care Interventions for High Risk Individuals PilotPrimary Care Interventions for High Risk Individuals Pilot Start Date: March, 2013 Timeframe: 12-18 monthsSummaryThis pilot is intended to support Primary Care in the management of High Risk Individuals through a suite of extended interventions and when required, co-ordination with secondary support and allied health services. The intention is to strengthen Primary Care as a patients home-base where required services outside of a practices resource can assist in the management of care. Locality SMOs and MDT expertise will be available for case conferences on a regular basis. There will be funding and invoicing support to assist in the process of care planning. Pilot Practices TBCHRI Definition20,000 per locality 30% risk of re-admission (PARR Report)Pilot PurposeTo increase management capability of HRIs in the Primary Care setting.To develop an HRI intervention tool with GPs to include services outside what available in the current funding structureIncreased access to services in a timely manner, which is appropriate for HRI care planning.To provide funding support and management mechanism for invoicing. Pilot ObjectivesTo develop an intervention tool appropriate to the HRI needs.To strengthen Primary Care as the home healthcare provider with patients.Increase access to necessary services in a timely manner with funding support.
-
Achievements to dateNow meeting weekly at ProCare, GraftonThe group have been meeting weekly since the last learning session and this has enabled us to progress our work and PDSA cyclesBetter management of high risk individuals (HRIs) the current situation?A Predictive Risk Algorithm (PRM) tool has been developed for patients at high risk of admission to hospital. Phase 2 which is underway at present, is looking to revise the algorithm incorporating primary care data which has shown to improve its predictive powerThe monthly PRM risk stratification reports are being sent from the three DHBs to all PHOs and reports of High Risk Individuals (HRIs) are delivered monthly to Procare Practices. The group are working on PDSAs on the formatting of the reports (i.e. individual vs practice lists) possible interventions areas and practice acceptance and readiness for provision of interventions for HRIsNext Steps?Work with Decision Support Services to establish automation processes Enhanced integrated care for high risk individuals - developing the intervention modelProgressing HRI pilot development with the Strategic Project Management Office, 2 GP practices per locality, practices have been identified via the locality managers and DHB for implementation of prototype service, with project brief completed