HealthNet Homecare NewApproachComprehensive Report ...
Transcript of HealthNet Homecare NewApproachComprehensive Report ...

This report describes our judgement of the quality of care at this location. It is based on a combination of what wefound when we inspected and a review of all information available to CQC including information given to us frompatients, the public and other organisations
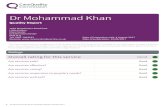
Ratings
Overall rating for this location Good –––
Are services safe? Good –––
Are services effective? Good –––
Are services caring? Not sufficient evidence to rate –––
Are services responsive? Good –––
Are services well-led? Good –––
Mental Health Act responsibilities and Mental Capacity Act and Deprivation of LibertySafeguardsWe include our assessment of the provider’s compliance with the Mental Capacity Act and, where relevant, MentalHealth Act in our overall inspection of the service.
We do not give a rating for Mental Capacity Act or Mental Health Act, however we do use our findings to determine theoverall rating for the service.
Further information about findings in relation to the Mental Capacity Act and Mental Health Act can be found later inthis report.
HeHealthNealthNett HomecHomecarareeQuality Report
Unit 3 Ardane ParkPhoenix AvenuePontefractWest YorkshireWF7 6EPTel:08000833060Website:www.healthnethomecare.co.uk
Date of inspection visit: 16 August 2019Date of publication: 31/10/2019
1 HealthNet Homecare Quality Report 31/10/2019

Letter from the Chief Inspector of Hospitals
HealthNet Homecare is operated by HealthNet Homecare (UK) Limited.
The service has a team of nurses which provides clinical homecare services to patients in community settings who havechosen to be treated at home rather than in hospital or as outpatients. This is in line with the NHS five-year-forward viewthat anticipates the further extension of clinical homecare services.
The service provides specialist medicines which patients administer themselves at home with appropriate support andtraining.Specific services regulated were the provision of nurses to administer medications, the provision of nurses toinitially administer medications until the patient is confident to undertake self-administration and guidance for patientswho want to administer themselves.
Although registered in July 2018, the first HealthNet home nurse visit took place in March 2019.
We inspected this service using our comprehensive inspection methodology. We carried out an unannouncedinspection on 16 August 2019.
To get to the heart of patients’ experiences of care and treatment, we ask the same five questions of all services: are theysafe, effective, caring, responsive to people's needs, and well-led? Where we have a legal duty to do so we rate services’performance against each key question as outstanding, good, requires improvement or inadequate.
Throughout the inspection, we took account of what people told us and how the provider understood and compliedwith the Mental Capacity Act 2005.
The service provided was community health service for adults.
We rated this service as Good overall because:
• The service had a training policy in place and provided mandatory training in key skills to all staff and made sureeveryone completed it.
• Staff completed and updated risk assessments for each patient through individual referral forms.
• Each external provider had a signed project agreement in place, detailing the service specific requirementsincluding associated key performance indicators.
• We saw records were clear, up to date and easily available to authorised staff. Staff recorded information in a clearand accurate way as well as consent.
• The service complied with National Midwifery Council (NMC) regulations and followed national guidelinesdeveloped by the National institute for Health and Care Excellence (NICE).
• All staff had the right qualifications, skills, knowledge and experience to do their job at the time of appointment,when they took on new responsibilities and on a continuous basis.
• HealthNet Homecare completed competency assessments for the administration of all medicines prescribed.
• Policies and procedures were up to-date, and available to staff.
• We saw the team worked well together and observed positive communication between the chairman of thecompany, clinical managers, nurse manager, superintendent pharmacist, nurses, support and administrative staff.
• The service had effective links, including individual patient reviews, with homecare teams within NHS trusts andwas able to discuss patient needs before and at the time of referral.
Summary of findings
2 HealthNet Homecare Quality Report 31/10/2019

• Out of hours appointments were arranged when convenient to the patient and in different settings if safe and moreconvenient to the patient.
• The service had investigated complaints and learning had been identified and shared with the nursing team andexternal providers of service.
• Managers were approachable, supportive and effective and had the skills and knowledge to ensure patientsreceived a quality service and we observed the registered manager promoted a positive culture that supported andvalued staff.
• The service had developed a vision designed to help the NHS drive improved patient outcomes and independencefor patients and their families.
• The service used technology to streamline services and had developed a portal system for patients and NHSclinicians to improve the quality and effectiveness of the service.
• All patients said they were extremely satisfied or satisfied with the homecare service received.
• The service had initiated an employee council with the aim of allowing employees to discuss with board memberstheir views on the business and working conditions.
Sarah Dronsfield
Head of Hospitals Inspection North Region, on behalf of the Chief Inspector of Hospitals
Professor Ted BakerChief Inspector of Hospitals
Summary of findings
3 HealthNet Homecare Quality Report 31/10/2019

Our judgements about each of the main services
Service Rating Summary of each main service
Communityhealthservices foradults
Good –––
The service had received 165 patient referrals and hadundertaken approximately 400 home visits since theservice began in March 2019. The majority of referrals(92%) were for patients who needed training in theadministration of asthma medicines
Summary of findings
4 HealthNet Homecare Quality Report 31/10/2019

Contents
PageSummary of this inspectionBackground to HealthNet Homecare 7
Our inspection team 7
Information about HealthNet Homecare 7
The five questions we ask about services and what we found 8
Detailed findings from this inspectionOverview of ratings 10
Outstanding practice 22
Areas for improvement 22
Summary of findings
5 HealthNet Homecare Quality Report 31/10/2019

HealthNet Homecare
Services we looked atCommunity health services for adults.
HealthNetHomecare
Good –––
6 HealthNet Homecare Quality Report 31/10/2019

Background to HealthNet Homecare
HealthNet Homecare services included healthcareprofessionals visiting patients at home to provide supportand training or regular home visits to administer themedicines until the patient is confident to administerthemselves. In all cases the clinical responsibility for thepatient remains with the clinical referring centre orprescriber.
HealthNet Homecare provided national patient support,dispensing, nursing support and controlled deliveryservices on behalf of the NHS, pharmaceutical companiesand the private sector. Most services were provided forNHS patients with 80% of the clinical homecare servicescost funded by the pharmaceutical company thatmanufactures the medicines.The remainder of theservices are commissioned directly by the NHS orprovided to private patients.
The service provided advice in relation to treatmentadministration, for example, sub-cutaneous injections(under the skin), nursing advice in relation to theadministration of treatment, storage of product, disposalof clinical waste and undertaking validated assessmentssuch as patient activation measure which describes theknowledge, skills and confidence a person has inmanaging their own health and care.
HealthNet Homecare is operated by HealthNet Homecare(UK) Limited. The service opened in 2018. It is based inPontefract, West Yorkshire. The service has had aregistered manager in post since 2018. We inspected theservice on 16 August 2019.
Our inspection team
The team that inspected the service comprised a CQClead inspector and a CQC medicines inspector. Theinspection team was overseen by Sarah Dronsfield, Headof Hospital Inspection, Yorkshire and Humber and NorthEast region.
Information about HealthNet Homecare
During the inspection, we visited HealthNet Homecaremain office in Pontefract, West Yorkshire. We spoke withseven members of staff including registered nurses,administrative staff, and senior managers.
There were no special reviews or investigations of theservice ongoing by the CQC at any time during the 12months before this inspection.
This was the service’s first inspection since registrationwith CQC, which found that the service was meeting allstandards of quality and safety it was inspected against.
The service did not report any never events, clinicalincidents or serious injuries.
Additional homecare nursing services were providedunder service level agreement.
Summaryofthisinspection
Summary of this inspection
7 HealthNet Homecare Quality Report 31/10/2019

The five questions we ask about services and what we found
We always ask the following five questions of services.
Are services safe?• The service had a training policy in place and provided
mandatory training in key skills to all staff and made sureeveryone completed it.
• Staff completed and updated risk assessments for each patientthrough individual referral forms.
• Each external provider had a signed project agreement inplace, detailing the service specific requirements includingassociated key performance indicators.
• We saw records were clear, up to date and easily available toauthorised staff. Staff recorded information in a clear andaccurate way as well as consent.
• The service complied with National Midwifery Council (NMC)regulations and followed national guidelines developed by theNational institute for Health and Care Excellence (NICE).
Good –––
Are services effective?• All staff had the right qualifications, skills, knowledge and
experience to do their job at the time of appointment, whenthey took on new responsibilities and on a continuous basis.
• HealthNet Homecare completed competency assessments forthe administration of all medicines prescribed.
• Policies and procedures were up to-date, and available to staff.• We saw the team worked well together and observed positive
communication between the chairman of the company, clinicalmanagers, nurse manager, superintendent pharmacist, nurses,support and administrative staff.
Good –––
Are services caring?• All patients said they felt supported in starting their medicines,
privacy and dignity had been maintained and they had beentreated with courtesy.
• Patients said they were extremely satisfied with theprofessionalism and politeness of staff (89%) and the overallquality of the service they received (83%).
Not sufficient evidence to rate –––
Are services responsive?• The service had effective links, including individual patient
reviews, with homecare teams within NHS trusts and was ableto discuss patient needs before and at the time of referral.
Good –––
Summaryofthisinspection
Summary of this inspection
8 HealthNet Homecare Quality Report 31/10/2019

• Out of hours appointments were arranged when convenient tothe patient and in different settings if safe and more convenientto the patient.
• The service had investigated complaints and learning had beenidentified and shared with the nursing team and externalproviders of service.
Are services well-led?• Managers were approachable, supportive and effective and had
the skills and knowledge to ensure patients received a qualityservice and we observed the registered manager promoted apositive culture that supported and valued staff.
• The service had developed a vision designed to help the NHSdrive improved patient outcomes and independence forpatients and their families.
• The service used technology to streamline services and haddeveloped a portal system for patients and NHS clinicians toimprove the quality and effectiveness of the service.
• The service had initiated an employee council with the aim ofallowing employees to discuss with board members their viewson the business and working conditions.
Good –––
Summaryofthisinspection
Summary of this inspection
9 HealthNet Homecare Quality Report 31/10/2019

Overview of ratings
Our ratings for this location are:
Safe Effective Caring Responsive Well-led Overall
Community healthservices for adults Good Good Not rated Good Good Good
Overall Good Good Not rated Good Good Good
Detailed findings from this inspection
10 HealthNet Homecare Quality Report 31/10/2019

Safe Good –––
Effective Good –––
Caring Not sufficient evidence to rate –––
Responsive Good –––
Well-led Good –––
Are community health services for adultssafe?
Good –––
Mandatory training
The service provided mandatory training in keyskills to all staff and made sure everyone completedit.
• The ‘training of nursing staff’ policy (November 2018)outlined the training systems to enable nurses toacquire the skills, knowledge and qualifications toperform their duties and tasks. All nurses wererequired to attend induction and ongoing mandatorytraining and ensure all training records were up todate.
• Mandatory training relevant to the service providedhad been identified and included equality, diversityand human rights, moving and handling,safeguarding, basic life support and informationgovernance.
• Mandatory training was accessible online and face toface. The registered manager oversaw mandatorytraining requirements and allocated time for staff tocomplete.
• All mandatory training was recorded on electronicsystems which identified courses attended, thoseplanned and when individual training was needed. Allstaff mandatory training was up to date.
Safeguarding
Staff understood how to protect people from abuseand the service worked well with other agencies todo so.
• The service had a ‘safeguarding policy’ (April 2018) inplace. This aimed to ensure all staff were aware oflocal safeguarding guidance and reporting proceduresand fulfil their role in safeguarding people at risk. Theclinical operations manager was the nominatedsafeguarding lead, a safeguarding supervisor andtrained to level 5.
• Additionally, the policy stated that safeguardingconcerns must be reported immediately to thehealthcare professional who had referred the patient,fully documented in the patient record and thesafeguarding report form.
• Staff had access to the safeguarding policy andprocedures and safeguarding training was part of theservice’s mandatory training programme. Staff spokenwith described the escalation process if they hadsafeguarding concerns.
• We were assured staff had training on how torecognise and report abuse, and they knew how toapply it.
• All staff had completed safeguarding adult andchildren level 1 training and all nursing staff hadcompleted safeguarding adult and children level 2training.
• There were no safeguarding concerns reported to CQCin the twelve months before inspection.
Communityhealthservicesforadults
Community health services foradults
Good –––
11 HealthNet Homecare Quality Report 31/10/2019

• The ‘safeguarding vulnerable groups’ policy (April2018) committed the service to ‘…safeguarding thewelfare of people at risk, children and young peoplewho use its services or come in to contact with theorganisation’.
• The policy identified signs that may indicate a concernand how to report these to the patient’s referringhealthcare professional. It also explained how toreport concerns about others who were not patientsto the local authority.
Cleanliness, infection control and hygiene
The service controlled infection risk well.
• The service had an up to date infection preventionand control policy. The policy provided guidance onthe preparation and precautions to minimise the riskof spreading of infection from person to person in thedelivery of care.
• Specific guidance was given on hand hygiene,personal protective clothing, aseptic techniques(using practices and procedures and applying strictrules to minimize the risk of infection) and themanagement of blood and body fluids.
• The clinical operations manager monitored adherenceto the policy through shadowing clinical staff duringtheir visits to patients.
• During the pre-clinical call, staff identified risks anyissues which may affect the service and recordedthese on the ‘home risk assessment’, these includedissues that could impact upon care, such as patientand nurse safety, infection control and hand washingfacilities. If necessary, an individual patient protocolwas developed following the home risk assessment.
Environment and equipment
The service had suitable premises and equipmentand looked after them well.
• The service operated from a large building on abusiness park and had internal and external securityand external lighting covering the exterior of thebuilding and car parking area.
• Office space, records storage, a meeting and trainingroom and working areas were located within thepharmacy area of the ground floor.
• Device alerts were cascaded to the nursing team bythe registered manager through team meetings andmedicine alerts were cascaded by the pharmacymanager.
• The service provided uniforms and personalprotective clothing for clinical staff visiting patients intheir home.
• We were told staff now carried small sharps binsduring their visits to dispose of waste that containsmedical residue such as medically contaminatedneedles or syringes. This reduces the potential risk topeople and the environment.
Assessing and responding to patient risk
Staff completed and updated risk assessments foreach patient through individual referral forms.
• Patients were referred to the service by homecareteams directly through NHS trusts. Once a referral hadbeen received the service made a call to the patient toorganise the input they needed for the safeadministration of their medication.
• During the pre-clinical call, staff identified risks andissues which may affect the service and recordedthese on the ‘home risk assessment’. These includedthe presence of children and pets, accessibility,building hazards, parking availability and lighting.
• Further issues were identified that could impact uponcare such as floor surfaces, trip hazards, exit routesand potential unpredictable behaviour of the patient.Assessments for manual handling, lifting equipment,sharps bins and electrical equipment safety were alsorecorded. Individual patient protocols were developedfollowing the home risk assessment.
• The service had responded to guidance (20 August2019) from the Resuscitation Council (UK) on thesuggested requirement for nurses conducting homevisits by instigating a protocol for nurses to carry twoseparate doses of adrenaline in the event of anadverse reaction to medication (anaphylaxis).
• Following each visit the nurse stayed with the patientuntil they were confident it was safe to leave. Ifdeterioration in the patient was identified theycontacted the patient’s referrer for advice or theemergency services, if necessary.
Communityhealthservicesforadults
Community health services foradults
Good –––
12 HealthNet Homecare Quality Report 31/10/2019

• The service did not have any situations whereemergency services were called to transfer patients toan acute trust or another healthcare provider withinthe twelve months before inspection.
Staffing
The service had enough staff with the rightqualifications, skills, training and experience tokeep people safe from avoidable harm and toprovide the right care and treatment.
• The service was managed by a clinical servicesdirector, a clinical operations manager and a nursemanager, supported by an administrator. The servicewas provided by a team of eight nurses. The numberof patients assigned to each nurse was monitored bythe clinical operations manager and nurse managerbased on the needs of the individual patients andgeographic location.
• We saw that all employees were subject toemployment checks defined by the ‘clinicalrecruitment procedure for nursing staff’ (November2018). This required the service to advertise vacancies,require completed application forms, confirm NMCregistration, details of RCN membership, professionalemployment history, undertake enhanced disclosureand barring service (DBS) checks and references.
• Further to the directly employed team, the service hadservice level agreements (SLAs) with external providersto supply nursing services. These SLAs had beendeveloped due to the geographical spread of theservice’s contracts with referrers. All staff providedwere subject to HealthNet Homecare policies andprocedures.
• As part of the nursing provider selection process, theservice requested completion of a comprehensive duediligence assessment and a self-declaration form bythe prospective partner organisation. As part of theprovider set up process, a master services agreementwas in place, and a data sharing agreement fortransfer of patient information.
• NMC registration was re-checked on an annual basisand a new DBS disclosure initiated when theemployee’s disclosure was two years old.
• The service had developed a pre-placement healthquestionnaire, a new starter checklist and a five-dayinduction programme for newly recruited clinical staff.
Records
Staff kept detailed records of appointments,referrals and completed consent documents.
• Under agreements with the referring hospitals and thepatient, the service received contact details to arrangenurse visits and/or calls to support the patient withtheir treatment and ascribed a unique identifier toeach patient.
• The service worked with the referring hospital team toensure they were fully aware of an individual’streatment. The individual nurse recorded andprovided feedback to the referring hospital team afterevery visit or call in relation to the service.
• Confidential information about the patient, theirmedical condition and treatment was held in anindividual patient file. This included the initialregistration form, home risk assessment, consent andnurse reports.
• Care and treatment at each visit was recorded on thehome visit record and the clinical evaluation form.These were then sent to the patient’s referrer.
• The service did not have access to patients’ medicalrecords with the exception of individual patient details(name, age, address, contact details, medicationprescribed), this was treated as personal and/orsensitive data.
• We saw records were clear, up to date and easilyavailable to authorised staff. Staff recordedinformation in a clear and accurate way whichincluded consent.
• Records were securely stored and managed on adatabase and paper records within locked cabinets.
Medicines
• The service had a medicine policy (November 2018).The policy identified the scope and responsibilities ofeach member of the nursing team and procedures tofollow during a patient visit.
• The policy identified that the nurse must make a clear,accurate, legible and immediate record of all
Communityhealthservicesforadults
Community health services foradults
Good –––
13 HealthNet Homecare Quality Report 31/10/2019

medicines administered by the nurse or the patient, ifself-administered. Further the policy required thenurse to contact the emergency services immediatelyin the event of an emergency situation.
• The nurse must also report any adverse event/producttechnical complaint immediately in accordance withservice procedure.
• Transport and delivery of medicines was made byanother part of the company (HealthNet Logistics)direct to the patient’s home.
• The service provided home visit nursing services for arange of specific and separate medicines for thetreatment of asthma, inflammation, primaryimmunodeficiency, angioedema and hereditaryangioedema (rare diseases resulting from the lack ofproduction of a key regulator in the production ofbradykinin, leading to significant swelling ofextremities).
• The home visits provided training in subcutaneousinjection administration, subcutaneous infusionadministration and intravenous injection.
• The service had received 165 patient referrals and hadundertaken approximately 400 home visits since theservice began in March 2019. The majority of referrals(92%) were for patients who needed theadministration of asthma medicines.
Incident reporting, learning and improvement
The service had appropriate processes for staff toraise concerns and report incidents.
• The service had a clinical incident reporting procedure(November 2018). This policy contained guidance to‘report, log and review clinical incidents, significantclinical incidents and near miss situations’.
• The clinical services director was identified asresponsible for ensuring all incidents wereinvestigated and that findings and learning wascommunicated to the clinical team to reduce thechance of recurrence.
• The service had recorded six incidents that werereviewed to evidence policies and procedures had
been followed. These related to issues with treatmentadministration (x5) and one occasion where the nursewas asked to leave the patient’s home before the endof the post injection observation period.
• These resulted in seeking advice from the referringhealthcare professional and in one case a retrainingsession for the administrating nurse. There were nocircumstances where the service had to seek advicefrom medical professionals who requested the serviceusers to get immediate medical attention.
• Duty of candour is a regulatory duty that relates toopenness and transparency and requires providers ofhealth and social care services to notify patients (orother relevant persons) of certain ‘notifiable safetyincidents’ and provide reasonable support to thatperson. Staff were aware of this duty and the need tobe open and honest with patients where incidentsoccurred.
• The service had not applied the duty of candour asthere had been no incidents when this would berequired.
Are community health services for adultseffective?(for example, treatment is effective)
Good –––
Evidence-based care and treatment
The service provided care and treatment based onnational guidance and evidence of its effectiveness.
• The service complied with National Midwifery Council(NMC) regulations and followed national guidelinesdeveloped by the National institute for Health andCare Excellence (NICE), for example, the managementof asthma.
• Standard operating policies and procedures wereavailable to all staff and they knew where to accessguidance and policies if they needed clarification.
Communityhealthservicesforadults
Community health services foradults
Good –––
14 HealthNet Homecare Quality Report 31/10/2019

• HealthNet Homecare was a member of the NationalClinical Homecare Association (NCHA) representingand promoting organisations whose primary activity isto provide medical supplies, support and clinicalservices to patients in the community.
• The NCHA ensures standards are applied throughworking closely with the NHS National HomecareMedicines Committee, NHS Commercial MedicinesUnit, NHS England, NHS Scotland, NHS Trusts, andcommissioners to ensure patients who wish to receivehomecare can access high quality clinical homecareservices.
• The registered pharmacy complied with guidelinesfrom NHS England (last inspection July 2015), theGeneral Pharmaceutical Council (last inspection June2017), Medicines and Healthcare products RegulatoryAgency (last inspection July 2017) and the HomeOffice (pharmacy licence renewed May 2018).
Pain relief
• Nurses did not administer pain relief but referred thepatient to their medical professional if needed.
Patient outcomes
Staff monitored the effectiveness of care andtreatment and used the findings to improve them.
• Patient outcomes across the company were formallycaptured and reported in a series of operational andgovernance key performance indicator (KPI) reportsthat were provided to the NHMC, regional homecareservice leads and trusts. This included company-wideinformation, such as pharmacy performance, numberof clinical incidents ascribed to the prescribingprocess and financial returns.
• Those relevant to the regulated service includednumber of patient safety incidents (none), number ofduty of candour incidents (none), total number ofreported adverse drug reaction incidents (none) andtotal number of safeguarding incidents (none).
• Where more specific therapy related outcomes wererequired, these were measured and reported throughbespoke reporting mechanisms to trusts, for examplethe asthma control questionnaire (ACQ6), and thesewere then audited and used for patient specificassessment by the referring clinical teams.
• We saw that action had been taken immediately whenan audit by one particular referrer had shown that theACQ6, although completed, had not been returned tothe referrer. This involved further written instructions,face-to-face meetings with nurses and further training.
• HealthNet Homecare worked as an extension of thereferring homecare team, within detailed servicespecifications, and provided patient data relevant tothe patient pathway provided within the patient’s care.
Competent staff
The service made sure staff were competent for theirroles
• The service employed staff in compliance with the‘clinical recruitment procedure for nursing staff’ thatclarified the processes followed for all recruitment andselection in relation to securing approval to recruit,advertise a post, short-list, select and appointcandidates.
• All staff had the right qualifications, skills, knowledgeand experience to do their job at the time ofappointment, when they took on new responsibilitiesand on a continuous basis. We saw the service hadcompleted training needs analyses on an individualand team basis.
• The service had systems to ensure new staff had readand understood the contents of the staff handbookand had accessed, read and understood policies andprocedures.
• Adherence was checked through shadowing patientvisits, clinical supervision and appraisals. All staff hadreceived an appraisal within the last twelve months.
• The employee handbook provided for new staffincluded the company values, standards,whistleblowing policy, equal opportunities policy andtraining policy.
• The service checked the Nursing and MidwiferyCouncil (NMC) register to confirm nurses hadmaintained their registration.
• The service ‘training of nursing staff’ policy outlinedthe training systems to enable nurses to acquire theskills, knowledge and qualifications to perform theirduties and tasks. All nurses were required to attendinduction and ongoing mandatory training.
Communityhealthservicesforadults
Community health services foradults
Good –––
15 HealthNet Homecare Quality Report 31/10/2019

• The service had developed a process of clinicalsupervision to identify additional training needs andto ensure continuing professional development inaccordance with NMC requirements.
• HealthNet Homecare completed competencyassessments for the administration by the patient ofall medications prescribed.
Multidisciplinary working and coordinated carepathways
Staff of different kinds worked together as a team tobenefit patients.
• During the inspection, we saw the team worked welltogether and observed positive communicationbetween the chairman of the company, clinicalmanagers, nurse manager, superintendentpharmacist, nurses, support and administrative staff.
• The service ensured patients were suitable for theservice through visits to the healthcare setting beforethe start of homecare and discussion with the referringclinical team.
• Regular reviews were held with referrers to discuss theprogress of each individual patient receiving thehomecare service.
Health promotion
• The service did not take part in formal or specifichealth promotion activity with patients.
• However, we were told nurses had received training inpatient support and motivational interviewing. As partof these, staff were encouraged to discuss with asthmapatients the impact on their health of looking afterpets, and the consequences of smoking, in relation toself-management of their disease
Consent, Mental Capacity Act and Deprivation ofLiberty Safeguards
Staff understood how and when to assess whether apatient had the capacity to make decisions abouttheir care.
• Following referral, verbal consent to begin care andtreatment was during the initial patient telephonecontact.
• Written consent was obtained from all patients at theirfirst visit and following completion of an initialregistration form and home risk assessmentcompleted.
• The responsibility for undertaking mental capacityassessments and placing deprivation of libertysafeguards on a patient were the responsibility of thereferring hospital and healthcare professional.However, members of the team received mandatorytraining on capacity assessments, were aware ofpatient needs and alerted the referrer wherenecessary.
• The service had not had any patients referred who hadmental health needs. We discussed this with seniormanagers who said all patients would be assessed onan individual basis with the referrer and would not beaccepted if the nursing team did not have the requiredskills and competence.
Are community health services for adultscaring?
Not sufficient evidence to rate –––
Compassionate care
Staff cared for patients and their families withcompassion
• During inspection of the service we were not able toobserve patient visits.
• The service had carried out a patient satisfactionsurvey (May 2019). Responses had been received from18 patients.
• All patients said they felt supported in starting theirmedicines, privacy and dignity had been maintainedand they had been treated with courtesy. Patients saidthey were extremely satisfied with the professionalismand politeness of staff (89%) and the overall quality ofthe service they received (83%).
Emotional support
• During inspection of the service we were not able toobserve patient visits and were unable to evidenceemotional support.
Communityhealthservicesforadults
Community health services foradults
Good –––
16 HealthNet Homecare Quality Report 31/10/2019

Understanding and involvement of patients andthose close to them
Staff involved patients and those close to them indecisions about their care and treatment.
• The patient satisfaction survey showed all patientswere fully informed in decisions about their care andtreatment and had their treatment explained so theycould understand it.
• All patients said they felt supported in starting theirmedication, privacy and dignity had been maintainedand they had been treated with privacy and dignity.
Are community health services for adultsresponsive to people’s needs?(for example, to feedback?)
Good –––
Planning and delivering services which meetpeople’s needs
The service planned and provided services in a waythat met the range of needs of people accessinghomecare services.
• The service had effective links with homecare teamswithin NHS trusts and was able to discuss patientneeds before and at the time of referral.
• Agreements with the referring hospitals and thepatient included arrangements to tailor nurse visitsand/or support calls to the needs of the individual andat the time to suit the patient. Out of hoursappointments were arranged where more convenientto the patient.
• Any issues identified by the clinical team during visitsor through telephone contact were reported back tothe referring hospital team to ensure they were fullyaware about an individual’s treatment.
• The individual nurse recorded and provided feedbackto the referring hospital team after every visit or call.
• Home risk assessments identified the suitability ofundertaking patient visits within their ownenvironment, but if safe and more convenient to thepatient appointments took place in different settings,for example, halls of residence, GP surgeries.
Meeting the needs of people in vulnerablecircumstances
The service took account of patients’ individualneeds, it had a proactive approach to understandingindividual needs and promoted equality.
• Information about the services available, how to bereferred to the service and treatments available weredisplayed on the website and provided duringtelephone enquiries. The outline of the serviceexplained that the patient will be fully involved inplanning their care following agreement with thereferring hospital.
• The service had access to translation and telephoneinterpreting services, and in exceptionalcircumstances, the service used nominated familymembers, care workers and social workers tocommunicate with patients whose first language wasnot English.
• The service provided patients with a ‘patient, carer,service user information leaflet’. This detailed thenursing team and their adherence to NMC codes ofpractice including the needs of people in vulnerablecircumstances.
• Information provided committed the team to workwith the referring hospital team, to make sure theywere fully aware about an individual’s treatment onthe homecare service and to support this, the nurseprovided feedback to the referring hospital team afterevery visit or call in relation to the service.
• During the initial telephone contact with the patient,staff identified the right level of support for anindividual patient.
• The ‘equality and diversity’ policy (May 2018) statedthe service provided equality of opportunity andpromotes equality of opportunity and diversity with allcustomers, suppliers, sub-contractors, partners andworkforce.
Communityhealthservicesforadults
Community health services foradults
Good –––
17 HealthNet Homecare Quality Report 31/10/2019

• The service was committed to treat customers fairlyand with respect and promoting an environment freefrom discrimination.
Learning from complaints and concerns
The service had a complaints policy and treatedconcerns and complaints seriously. Complaints wereinvestigated and lessons learned from the resultsand shared with all staff.
• The service had received ten complaints in the twelvemonths before inspection, three were about servicesprovided directly by HealthNet Homecare and theother seven related to services from externalproviders.
• Complaints related to incorrect referral (four), processnot followed (three), delays in beginning treatment(two) and nurse competence. All complaints had beenfully investigated and those relating to externalproviders of services had been discussed at regularmeetings through service level agreements. Theoutcome of each investigation was shared, and nonehad resulted in a complaint to the ombudsman.
• Learning had been identified and shared with thenursing team and external providers of service. Alloutcomes had been shared with the referring trust.
• All patients had been informed of complaint processesthrough the ‘patient, carer, service user informationleaflet’. The service provided patients with informationabout giving feedback, Patient Advisory and LiaisonServices and complaints processes.
• All staff were made aware of service standards andcomplaint processes through the inductionprogramme developed by the service.
Are community health services for adultswell-led?
Good –––
Leadership of services
Managers at all levels in the service had the rightskills and abilities to run a service providinghigh-quality sustainable care.
• The service's managing board was committed toserving the interests of the company and achievingsustainable growth. Members of the board wereresponsible for the management of the company,business policy and corporate strategy. An initialboard assurance framework and action plan toolkit(based on SMART principles) had been designed andwas being further developed at the time of inspection.
• The management structure consisted of the chairman,members of the board, directors and senior managers.The registered manager oversaw operationalmanagers, the nurse team and administrative staff andwas responsible for the everyday running of theservice.
• The registered manager was contactable to answerqueries or for discussion about all services andprocedures. The registered manager had the skills,knowledge and experience needed to effectivelymanage the service.
• At the time of inspection, the registered manager wasabout to change, the clinical operations manager wasdue to take on the role and following interview thiswas confirmed.
• Staff told us managers were approachable, supportiveand effective and had the skills and knowledge toensure patients received a safe quality service. Wewere told, and observed the registered managerpromoted a positive culture that supported andvalued staff, creating a sense of common purposebased on shared values.
• The service operated a ‘no blame’ culture toencourage team working both within the service andwith external organisations. There was a team culturewith a focus on professional standards, continuousprofessional development and appraisals.
Service vision and strategy
The service had a vision for what it wanted toachieve and workable plans to turn it into action.
• The service had developed a vision and a strategy toachieve its goals.
• The service vision recognised the needs of the patientby providing a direct to patient model offering:
Communityhealthservicesforadults
Community health services foradults
Good –––
18 HealthNet Homecare Quality Report 31/10/2019

▪ Service excellence based on reliability, flexibility,transparency and convenience;
▪ Delivery of services that are safe, effective, caring,responsive and well-led;
▪ Services that are easy for the NHS to implementand monitor; and
▪ Services that are cost effective and sustainable.
• The vision was designed to help the NHS driveimproved patient outcomes and independence forpatients and their families.
• The associated strategy aimed to facilitate the use oftechnology to ‘…deliver support programmes tailoredto the needs of the patient, the NHS andpharmaceutical clients’.
• To achieve this the service used technology tostreamline services, enabled direct data access,flexibility and reliability in line with patientexpectations, virtual clinical support services, face toface nurse training and support.
• Managers and staff understood how to apply thestrategy and monitor progress.
Culture within the service
Managers across the service promoted a positiveculture that supported and valued staff, creating asense of common purpose based on shared values.
• During the inspection we discussed the service withthe chairman, clinical director, clinical operationsmanager, nurse manager, superintendent pharmacistand members of the team. We saw staff workedtogether well as a team and there was an openculture.
• We saw a ‘no blame’ approach to the investigation ofcomplaints and the clinical operations manageraddressed performance issues through one to onefeedback with staff and on a team wide basis wherelearning had been identified.
• Staff spoke positively about their roles within theservice and staff felt supported in their work. Staff toldus they felt valued and supported by colleagues andthe registered manager. There was a strong emphasison the care and treatment of patients, carers and theirfamilies.
• Staff promoted openness and understood how toapply the duty of candour. Staff were aware of whatthe term duty of candour meant.
• Throughout our inspection, the registered managerresponded positively to feedback. This demonstrateda culture of openness and willingness to learn andimprove.
Governance, risk management and qualitymeasurement
The service systematically improved service qualityand safeguarded high standards of care by creatingan environment for good clinical care to flourish.
• Managers operated effective governance processes,throughout the service and with partner organisations.Staff at all levels were clear about their roles andaccountabilities, and they had opportunities to meet,discuss and learn from the performance of the service.
• The ‘corporate governance’ policy (April 2018) definedthe principles of governance used within the service –openness and inclusivity, integrity, accountability –and the governance framework.
• One aspect of the framework concentrated onimproving patient safety through maintainingconfidentiality, information governance, robustservice delivery processes, clear roles andresponsibilities and risk management.
• Each external provider had a signed projectagreement in place, detailing the service specificrequirements of each programme, includingassociated key performance indicators. Serviceperformance was discussed at regular reviewmeetings, the frequency determined by performanceand complemented by ongoing and continuedcommunication between service managers anddirectors.
• Board minutes (December 2018, March 2019) showeddiscussion of governance and risk issues and theservice had developed a ‘business impact analysis andrisk register’ (May 2019).
• The ‘business impact analysis and risk register’identified general risks and those associated with
Communityhealthservicesforadults
Community health services foradults
Good –––
19 HealthNet Homecare Quality Report 31/10/2019

utilities, plant and equipment, telecoms andinformation technology. The registered managerexplained that this was being developed andidentified high level risks only.
• The service had developed a portal system for patientsand NHS clinicians to improve the quality, flexibilityand effectiveness of the service and an educationalresource and had developed a ‘Future DigitalRoadmap’ leading to the provision of a suite ofcomplementary information technology innovations.
• The service was working towards offering ‘…fullyintegrated multi-dimensional healthcare solutions’tailored to the needs of the individual throughpatients having access to clinical professionals andappropriate support and information when they needit.
• Information governance was complied with anddefined by the ‘information governance and patientconfidentiality’ (July 2018), ‘HealthNet privacy notice’(May 2018) and ‘information governance; dealing witha subject access request’ (April 2019).
• Policies and procedures were for the operation of theservice and these were up-to-date, compliant withreview dates and available to staff.
Public and staff engagement
The service engaged well with patients to plan andmanage appropriate services and collaborated withpartner organisations effectively.
• Patients were asked to complete a patient/carerfeedback questionnaire at specified nurse visittimepoints. This enabled patients and carers tocomment upon the individual nurse performance,privacy and dignity and patient involvement indecisions about their care and treatment. A similarquestionnaire was used to obtain feedback onindividual nurses from other healthcare professionals.
• During the inspection, we saw the provider carried outa patient satisfaction survey (May 2019). All patientssaid they were extremely satisfied (83%) or satisfied(17%) with the homecare service received.
• Further, 78% of patients said they were extremelylikely to recommend the service to family and friends ifthey needed similar care and 22% were likely to do so.
• The service had plans to repeat the patientsatisfaction survey and introduce patient supportgroups.
• The service had initiated an employee council inSeptember 2018 with the aims of allowing employeesto discuss with board members their views on thebusiness and working conditions. A member of thenursing team attended the employee council.
• The employee council had discussed the results of theemployee survey conducted across all areas of thebusiness and developed actions in response.
• The survey showed 89% of staff were ‘clear about whatI am expected to achieve in my job’, 68% had ‘clear,measurable work objectives’, 79% said their ‘team iswell managed’ and 87% said ‘senior managers aresufficiently visible within the business’.
• However, the employee survey also identified thatonly 36% For all staff said they ‘receive regular andconstructive feedback on my performance’ and 48%said that morale was good where they work. It was notpossible to identify whether these applied to the nurseteam.
Innovation, improvement and sustainability
The service was committed to improving services bylearning from when things went well or wrong andpromoting training.
• The service had developed a portal system for patientsand NHS clinicians to improve the quality, flexibilityand effectiveness of the service and an educationalresource.
▪ Patients: enables patients to choose theirmethod, location and time of delivery to suit theirparticular needs. The portal allows the NHS toplace therapy-based training videos, orpatient-specific information online for patientsand their families to access. The portal was beingenhanced and upgraded to reflect the ideas andfeedback from patients and book nurse visitsonline.
▪ Clinicians: enables registration of patientsdirectly on the HealthNet system, and allowsclinicians to create prescriptions, providing realtime visibility for the homecare team ensuring
Communityhealthservicesforadults
Community health services foradults
Good –––
20 HealthNet Homecare Quality Report 31/10/2019

patient transition to homecare is seamless andtimely. This reduces the workload for clinical staff,improves convenience and lowers costs,significantly enhances patient safety through thereduction in transcribing errors and lost/mislaidprescriptions through the postal system. The
clinician portal was being further developed sothat nurse visit reports and delivery informationcan be automatically uploaded securely so thatany hospital clinical team can log on and see all ofthe nursing and medication delivery activityrelevant to their patients.
Communityhealthservicesforadults
Community health services foradults
Good –––
21 HealthNet Homecare Quality Report 31/10/2019

Outstanding practice
• Following risk assessments, the service offeredpatient appointments in different settings, forexample, halls of residence, GP surgeries.
• An initial board assurance framework and actionplan toolkit (based on SMART principles) had beendesigned and was being further developed at thetime of inspection.
• The service had developed a portal system forpatients and NHS clinicians to improve the quality,flexibility and effectiveness of the service and a‘Future Digital Roadmap’ leading to complementaryinformation technology tailored to the needs of theindividual patient.
Outstandingpracticeandareasforimprovement
Outstanding practice and areasfor improvement
22 HealthNet Homecare Quality Report 31/10/2019