Headache for Medical Finals (based on Newcastle university learning outcomes)
Transcript of Headache for Medical Finals (based on Newcastle university learning outcomes)
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
1/30
Hospital Based Practice Acute Severe Headache.
Headache is the most common neurological symptoms.
o About 4.1% have chronic daily headaches.
Patients get very worried about ones that persist.
Cause of significant morbidity.
History.
o Normal SOCRATES questions.
o Tempo of onset
o Signs of meningism
o Rhythm
o Time of day it comes one
o Affect of coughing/ position
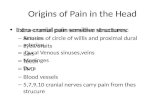
Causes.
Pattern Causes
Solitary acute episode Infection.
Meningitis Encephalitis
Abscess
Vascular events
Intracranial haemorrhage (especially
subarachnoid)
Venous sinus thrombosis
Occasionally infarction due to arterial
dissection.
Trauma
First presentation of other types.
Progressive headache Raised intracranial pressure
(including benign intracranial hypertension)
Giant cell arteritis
Tumour
Hydrocephalus
Episodic headache/ facial pain Migraine
Cluster headache
Trigeminal neuralgia
Coital cephalgia
Chronic headache/ facial pain Tension headache/ analgesic rebound headache.
Postherpetic neuralgiaPost head injury
Pagets disease of the skull
Other causes of facial pain Dental problems
Temporomandibular joint
Ears/ nose/ sinusesCervical spine
Eye
MI (rarely)
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
2/30
Examination
Raised intracranial pressure.
o Worsened by.
Coughing
Sneezing
Leaning down
o Worse in the morning
o Visual disturbances.
Papilloedema
o Nausea & Vomiting
o Diplopia.
False localizing CN VI palsy.
o Altered level of consciousness
o Bradycardia
o Hypertension.
Mainly if acute or severe
o Decebrate posturing
o Death.
Meningism
o Irritability.
o Neck stiffness
o Kernigs sign.
Hamstring spasm & pain on knee extensiono Brudzinskis sign.
Neck flexion causes leg flexion
o Signs of infective meningitis
Delerium
Fever
Petechial rash.o Signs of sub arachnoid haemorrhage
Retinal (subhyaloid) haemorrhage
Arteriovenous malformation bruit
CN III palsy
Direct pressure from posterior communicating artery aneurysm.
Signs of temporal arteritis.
o Temporal artery tenderness
o Loss of temporal artery pulsation.
May be overlying erythema
o Optic atrophy
o Low grade pyrexia.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
3/30
Investigations.
If history suggestive of temporal arteritis.
o ESR
o Temporal artery biopsy
If history suggests some other diagnosis, treat as appropriate.
o Migraine
o Tension headache
o Coital cephalgia
o Cluster headache
o Temporomandibular joint pain.
If diagnosis not clear, or suggests intracranial pathology.
o CT head scan.
May show
Blood
Tumour
Abscess
Hydrocephalus
o If CT normal, perform lumbar puncture.
CSF leucocytosis.
Meningitis
High CSF pressure.
Benign intracranial hypertension
Dural sinus thrombus.
Xanthochromia
Subarachnoid haemorrhage.
o If SAH suspected, do angiography, which may show.
Berry aneurysm
Arteriovenous malformation.
FBC.
o Normocytic normochromic anaemia suggests chronic pathology.
Temporal arteritis
Tuberculous meningitis
o Leucocytosis seen in infection
ESR.
o High in temporal arteritis
o Also raised in. Chronic infection
Pregnancy
Temporal artery biopsy.
o 100% specific.
o Due to patchy nature of inflammation, not very sensitive.
CT or MRI.
o Will show blood, tumour, abscess and hydrocephalus.
o If tumour is suspected, use contrast enhancement to better define the extent.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
4/30
Lumbar puncture.
o Never perform if raised ICP possible.
Causes coning.
o CSF should be sent to lab for assessment for meningitis and SAH.
Glucose
Protien
MC&S Cytology.
Xanthrochromia
Cerebral angiography.
o Perform if surgery is being considered for SAH.
o Identifies and locates berry aneurysms and arteriovenous malformations.
Visual fields.
o Serial measure in patients with benign intracranial hypertension
o Monitors due to the risk of optic nerve infarction.
Electroencephalography.
o Herpes simplex will give characteristic features
Tension headache
Defined as headaches that occur.
o On 15 or more days a month
o Pain is.
Bilateral pressing or tightening
Non pulsating
Mild or moderate intensity
Doesnt worsen with physical activity.o No more than one feature of.
Mild nausea
Photophobia
Phonophobia
Pain can last minutes days.
Main differential diagnosis is migraine.
o Many experts dispute that the extra features of photphobia, phonophobia and nausea
should be included in definition of tension headache.
Other differentials include.
o New daily, persistant headache
o Medication overuse headache.
o Chronic migraine
o Hemicrania continua
Neurologically normal
Incidence
About 2 2.5% suffer tension headaches. About 2:1 Female to male ratio
Symptoms start before age of 10 in 1.5% of patients.
Prevelence decreases with age
Family history of some form of chronic headache in 40%.
o Similar rates in identical and non identical twins.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
5/30
Management
Amitriptyline.
o Reduces symptom
Duration
Frequency.
o Side effects.
Dry mouth
Drowsiness
Weight gain
Mitarzapine.
o Reduces symptom.
Duration
Frequency
Intensity
o RCT found similar effects with mitarzapine and amitriptyline.
Mitarzapine has less side effects.
o Side effects.
Dizziness
Drowsiness Increased appetite & weight
Serotonin reuptake inhibitors.
o Similar effect to amitriptyline
o Less side effects than amitriptyline.
o Side effects.
Transient nausea
Anorexia
Irritability
Benzodiazipines.
o Some possible effects.
o Side effects.
Altered mental state
Poisoning
Depression
Dependence
Botox.
o Can improve symptoms.
o Side effects.
Facial weakness
Difficulty with swallowing
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
6/30
Disturbed local sensation
Vertigo
Pain at injection site
Muscle cramps
Flu like symptoms
Subjective feeling of.
Neck weakness & pain Temporomandibular joint pain.
Conventional acute analgesia has no effects, and can cause analgesia induced headache.
o Can convert an acute headache into a chronic one
o Caffeine can relieve an acute headache, but perpetuate a chronic headache.
Non drug therapy.
Cognitive behavioural therapy.
o Effective by 6 months.
o About as effective as amitriptyline
o No side effects
Acupuncture.
o Laser acupuncture can improve headache
Duration
Frequency
Intensity
Indian head massage.
o No effect
Relaxation and electromyographic biofeedback.
o No effect
o Requires expensive equipment and staff.
Migraine.
Many people with migraine or analgesia induced headaches can also have background headaches,
which resemble tension headaches.
o Very important to take a good history to look for alternative diagnosis and elicit
Features
Prodrome
Accompanying feature
Clinical features.
o Unilateral headache
o Pulsating character
o Photphobia
o Reccurrent natureo Last up to 30 hours.
o Aura
Visual chaos
Hemianopia
Hemiparesis
Dysphasia
Dysarthria
Ataxia.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
7/30
With basilar migraine.
o Can cause tenderness all over the face and head.
o Diagnostic criteria in absence of aura.
> 5 headaches
Lasting 4 72 hours
With either.
Nausea Vomiting
Photophobia
Phonophobia
And 2 or more of:
Unilateral
Pulsating
Interference with normal life
Worsened by routine activity.
Pathogenesiso Old theory
Cerebral oligaemia leading to the aura.
Cerebral and extracranial hyperaemia leading to the headache.
Undelrying cause of vascular abnormalities may be dysfunction of sensory
modulation of craniovascular afferent nerves.
Attacks are associated with changes in plasma serotonin.
o MRI evidence shows cerebral oedema, dilatation of intracerebral vessels and reduced
water diffusion are not associated with vascular territories.
Primary event may be neurological after all.
Triggers.
o CHOCOLATE.
CHocolate orCHeese.
Oral contraceptive pill
Caffeine (or caffeine withdrawal)
alcohOL
Anxiety
Travel
Exercise
o In 50%, no trigger is found
o In only a few does avoiding triggers prevent all attacks
Associations.
o Obesity
o Patent foramen ovale
Catheter closure may help.
Differentials.
o Cluster or tension headaches
o Cervical spondylosis
o Hypertension
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
8/30
o Intercranial pathology
o Sinisitis/ Otitis media
o Tooth caries
o TIA
o Migraine is rarely a sign of serious pathology
o Dont expend too much time looking for. Antiphospholipid antibody
Microemboli
Vascular malformationso However, these factors are important in some.
Prophylaxis.
o Mainly used if frequency > 2 times in a month.
o If one drug doesnt work after 3 months, try another.
o > 65% will achieve an attack frequency reduction of 50%
o Pizotifen.
Serotonin antagonist.
0.5 1 mg TDS
or 3 mg OD at night
Side effects.
Drowsiness
Weight gain
Increased effects of alcohol
Increased glaucoma risk
o Propanolol
40 120 mg BD POo Amitriptyline.
25 75 mg nocte
Side effects.
Drowsiness
Dry mouth
Blurred vision
o Second line prophylaxis include.
Valproate
400 600 mg BD
NSAIDs
Gabapentin
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
9/30
Topiramate
Treatment
o Dispersible, high dose aspirin.
600 mg QDS POo Paracetamol & Metoclopramide
1 g QDS & 5 mg TDS Give metoclopramide 10 minutes before paracetamol
Beware extrapyramidal side effects.
o Ketoprofen.
100 mg stat PO
o No evidence of any difference between ergotamine, NSAIDs and triptans/
In terms of QUALYs Rizatriptain is better than sumatriptain, which is better
than Cafergot.
Rizatriptain is fastest acting.
Rizatriptan and xolmitripan are available as fast dissolving wafers for buccal
administration
Imigrain recover is available over the counter
o Triptans.
Serotonin agonists
Constrict cranial arteries
Rare side effects include.
Arrythmias
Angian
MI
Contraindications.
Previous IHD
Coronary spasm
Uncontrolled hypertension
Recent lithium
SSRIs
Ergot use.
o Ergotamine
Serotonin agonist
Constricts cranial arteries
1 mg PO as headache starts.
Repeated every half an hour.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
10/30
Maximum of 3 mg in a day
Maximum of 6 mg in a week.
Can be more effectively given as suppositories.
2 mg ergotamine + 100 mg caffeine
Up to 2 in 24 hours
After use, have to have a break for > 4 days.
Emphasise risk of. Gangrene
Vascular damage
Contraindicated in.
COCP use
Peripheral vascular disease
IHD
Pregnancy
Breast feeding
Hemiplegic migraine
Raynauds disease
Liver or renal impairment.
Hypertension.
Cluster Headaches.
Prevelence of 1%
Peak onset of 20 40 years.
o Sometimes remit with increasing age.
Risk factors.
o Head or facial trauma
o Smoking
85% of sufferers are smokers
Stopping smoking once you have cluster headaches doesnt improve condition
o Family history
May be autosomal dominant, autosomal recessive or multifactorial inheritance
o Male gender
Features.
o Last 15 180 minuteso Unilateral
o Severe pain
o Occur up to 8 times a day
o Episodic in 80 90% of patients.
Clusters and remission
o Autonomic symptoms in 97%
Horners sydrome
Ptosis
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
11/30
Miosis
Eye watering or bloodshot
Runny or blocked nose
Sweating
Flushing
Occur during the attack. Occur on same side as pain
Ptosis and miosis may be constant, but intensified during attacks.
o Circadian rhythm
o Symptoms can shift to other side.
Some paitients can have their pain shift, but their autonomic disfuctnion remain
on the original side.
Episodic cluster headaches.
o 80 - 90% of patients have this type.
o Headaches occur daily few a few weeks, then period of remission.
o During active periods, patients can suffer up to 8 attacks a day
o Active periods can last anything from a week to a year.
o When in a bout, headaches can be triggered by.
Alcohol
Vasoactive substances
o When in remission, alcohol has no effect on headaches and patients are asymptomatic.
Chronic cluster headaches.
o No remissions, or remissions lasting less than 30 days.
o Can be primary
o Can be secondary as an evolution from the episodic form.
Examination.
No neurological abnormalities.
o If abnormalities found, investigate patient for secondary cause.
Some patients develop persistant miosis and ptosis.
CT/MRI to exclude abnormalities
o Mid line mass lesions or malformations are associated with cluster headaches.
Especially in older patients.
Treatment
Divided into abortion of the acute attack and prophylaxis to prevent recurrence.
Acute therapy.
o Oxyegn
100% oxygen in non rebreath mask is effective in stoping attacks.
Flow rate of 7 10 L/min
Give for at least 20 minutes in upright position.
60% of patients respond within 20 30 patients.
Be careful of the possibility of hypoxic drive patients.
o Triptans.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
12/30
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
13/30
Constipation
Dull headache
Second line prevention.
o Lithium.
78% of chronic cluster headache patients report benefit with lithium
prophylaxis.
No reported benefit for episodic patients. Monitor blood levels and keep them between 0.6 1.2 mmol/L
Recommended dose is 600 1500 mg OD
Ideally given as sustained release.
Also monitor.
Liver function
Renal function
Thyroid function
Side effects.
Thyroid dysfunction
Tremor
Renal dysfucntion
Due to danger and side effects, lithium only recommended in chronic cluster
headaches, and only when other drugs contraindicated or ineffective.
Lots of drugs interact with lithium.
Normally be increasing renal excretion
o Methysergide.
Evidence of benefit is limited.
Seems to be more effective in episodic headaches than chronic.
Normal dose is 4 8 mg OD.
Use caution when giving with triptans or other ergotamine derivatives
Side effects.
Nausea
Muscle cramps
Abdominal pain Pedal oedema
Do not use continuously for > 6 months.
High risk of pulmonary or retroperitoneal fibrosis with long term use.
o Corticosteroids.
Used to rapidly suppress attacks whilst longer acting agents take effect.
Medication of choice in periods of cluster activity of less than 2 months.
Up to 80% of patients will respond to steroid therapy.
Some patients will only respond to steroids, and so will need to take them
continuously.
Start dosage at 60 100 mg prednislone OD for 5 days.
After the 5 days, try and reduce dosage by 10 mg a day.
Third line prevention
o 10 20% of patients dont respond to previous lines of prophylaxis, or the headaches
become resistant.
o Following drugs have limited evidence supporting their use.
o Pizotifen.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
14/30
Antiserotonergic drug.
3 mg per day have been effective in trails
Only have modest effects
Side effects.
Tiredness
Weight gain
o Valproate. 5 20 mg/kg per day.
o Topiramate.
Effective therapy.
Recommended dose is at least 100 mg
Titrating up from 25 mg daily.
Side effects.
Cognitive disturbances
Paresthesia
Weightloss
Contraindicated in renal stones.
o Capsaicin.
Effective in two thirds of patients. 3 times a day nasally for 6 days on side that pain is.
o Many patients do better on combination therapies, rather than high dose of a single drug.
o A good starting point is
Verapamil at 240 480 mg + another drug.
Future treatments and those lacking evidence base
o Antiepileptics
Pregabalin
Levetiracetam
Zonisamide
o
Vanilloid/ cannaboid receptor agonists.o SC octrrotide.
o Surgery.
Consider if all drugs are ineffective, and secondary cause of headaches have
been ruled out.
Be cautious, as little data on long term effect.
Blocking the greater occipital nerve can be effective.
Should be tried first.
If patient has episodic headaches, be very careful when considering surgery near
the trigeminal structures as can cause:
Trigeminal neuralgia.
Anaesthesia dolorosa
o Sensation to that part of the face is lost, but pain remains.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
15/30
Deep brain stimulation of posterior inferior hypothalamus can be effective.
Procedure reversible
Normally well tolerated.
Still experimental.
Trigeminal neuralgia.
Clinical picture.o Paroxysms of intense, stabbing pain
o Lasts seconds
o Unilateral
o In trigeminal nerve distribution
Typically maxillary or mandibular branches.
o Face screws up in pain.
Tic Doloureux
o Aggrevated by.
Washing face
Shaving
Eating
Taling
Dental prostheses
Typical patient.
o Male
In Asians, 2:1 Female:Male ratio
o Over 50 years
Causes.
o Anomalous intracranial vessels compressing trigeminal root.
o Secondary causes (14%)
Aneurysm
Tumour
Chronic meningeal inflammation
MS Herpes zoster
Skull base malformation.
Eg. Chiari
Investigations.
o MRI to rule out secondary causes.
Treatment.o Carbamazepine.
Start at 100mg BD PO
Titrate up to a maximum of 400 mg QDS
o Phenytoin
200 400 mg OD POo Gabapentin.
300 mg on day 1
1300 mg BD on day 2
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
16/30
2800 mg TDS on day 3
Side effects.
Diarrhoea
Dry mouth
Dyspepsia
Vomiting
Peripherla oedema
Dizziness
o Lamotrigine.
o If drugs fail, surgical microvascular decompression may be needed.
Can be performed on the.
Peripherl nerve
Trigeminal ganglion
Nerve root.
Anomalous vessels are separated from the trigeminal root.
Stereotactic gamma knife surgery can work.
Limited by.
o Length of pain reliefo Time taken to get response to treatment.
Subarachnoid haemorrhage,.
Spontaneous bleeding into the subarachnoid space is often catastrophic.
Incidence.
o 8/100000 per year.
o Typically aged 35 65 years.
Caused by.
o 80% due to rupture of berry aneurysms
o 15% due to AV malformations
o
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
17/30
o Some are hereditary.
o Associations.
Polycystic kidneys
Coarctation of aorta
Ehlers Danlos syndrome
Symptoms.o 10% have sudden death.
o Headache.
Onset within seconds.
Maximal within minutes.
Meningism
o Vomiting
o Collapse
o Seizures
o Coma/ drowsiness.
May last for days.
Signs.
o
Neck stiffnesso Kernigs sign.
Takes about 6 hours to develop.o Retinal and subhyaloid haemorrhage
o Focal neurology,.
At presentation suggests sit of aneurysm or intracerebral haematoma.
Eg. Pupil changes suggest CN III palsy and posterior communicating
artery aneurysm.
Later on suggests
Ischemia from re bleeding or vasospasm
Hydrocephalus.
Differentials.
o Only 25% of patients with thunderclap headache in primary care have SAH.
In 50 60% no cause is found.o The others have.
Meningitis
Migraine
Intracerberal bleeds
Cerebral venous thrombosis.
Sentinal headaches.
o 6% of SAH patients have lesser headaches before their SAH.
Probably due to warning bleeds.o Not a reliable sign as recall bias clouds the picture.
o As surgery outcomes are now good for patients with few symptoms, be suspicious of any
severe, sudden onset headache. Particularly if associated with.
Neck pain
Back pain.
Investigations.
o Modern CT scanners can pick up > 90% of SAH within 48 hours of onset.
o Older ones may miss small bleeds.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
18/30
If clinical suspicion high, but CT ve, send for LP at 12 hours.
o CSF in SAH is uniformly bloody.
Becomes yellow and xanthochromic after a few hours.
o Supernatant from spun CSF is examined for breakdown products of haemoglobin.
Finding bilirubin in CSF is diagnostic.
Management.o Get immediate neurosurgical help if.
Reduced GCS
Progressive focal deficit
Suspected cerebellar haematoma
o Bed rest
o Closely monitor.
BP
Pupils
Coma level
Neurologyo Repeat CT if deteriorating
o
Prevent straining with stool softeners.
o Surgery.
Craiotomy and clipping of aneurysms can stop rebleeds.
Best option in those with few or no symptoms (Grade II or less)
If surgery likely, do prompt angiography.
Side effects.
o Intra operative rupture
o Post op epilepsy
Endoscopic Platinum coil insertion is an alternative.
Less invasive
Slightly higher rebleed rate
Intracranial stents and ballon remodelling allow treatment of wide neckedaneurysms.
Microcatheters can now pass through tortuous vessels to treat previously
unreachable aneurysms
AV malformations and fistulae may also benefit from endoscopic surgery.
o Medical.
Cautiously control severe hypertension
Analgesia for headache.
Best rest sedation for 4 weeks
Keep well hydrated.
running dry so as not to increase ICP causes more vasospasm.
Nimodipine.
60 mg every 4 hours PO/ 1 mg/h IV
Treat for 3 weeks.
Calcium channel blocker
Reduces vasospasm.
Give to all patients whos blood pressure allows it.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
19/30
Prognosis
o Death often occurs following re bleeding
Occurs in 30%
Often in the first few days.o Almost all death occurs in the first month.
o Oif those who survive the first month, 90% are still alive at 1 year.o Vascular spasm following a bleed often causes ischemia and permenant CNS deficit.
Surgery is not useful at the time if this happens, but may be so later.
Grade Signs Mortality (%)
I None 0
II Neck stiffness and cranial nerve palsies 11
III Drowsiness 37
IV Drowsy with hemiplegia 71
V Prolonged Coma 100
Prevention.
o Risk of surgery normally outweighs benefit of prophylactic surgery.
o Except, possibly, in young patients with
Aneurysms > 7 mm in diameter.
Aneurysms at junction of internal carotid and posterior communicating arteries.
Aneurysms at rostral basilar bifurcation
Uncontrolled hypertension
History of bleeds
o Surgery twice as risky if > 45 years.
o Relative risk of rupture for aneurysm > 7 mm across is 3.3.
o Relative risk of rupture for aneurysm > 12 mm across is 56
o Should screen patients with previous SAH who are also:
Smokers
Hypertensives Multiple aneurysms
Benign coital headache.
Also known as coital cephalgia.
Experienced as an explosive headache.
o Symptoms can be indistinguishable from SAH.
Can only make the diagnosis after excluding SAH.
May recur during subsequent orgasms
Will not cause persistant neurological disability.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
20/30
Meningitis
Presentation.
o Headahce
o Fevero Neck stiffness
Absent in 18% of patients
o Photophobia
May take hours days to develop.
o Rash.
Associated with macular rash that progresses to petechiae or purpura.
o Confusion & psychiatric disturbances or altered GCS.
Particularly in elderly with co morbidities
In immunocompromised.or neutropaenic, the only sign could be confusion.
o Focal neurological signs.
Complicate meningitis in about 15%
Can suggest.
Cerebral damage.
o Eg. Hemiparesis following venous infarction or arteritis.
Cranial nerve and brainstem involvement
o Basal exudation and inflammation
o Eg. Listeria monocytogenes meningitis.
Brain shift secondary to raised ICP
If focal signs or seizures are prominent, consider possibility of:
Brain abscess
Encephalitis
If papilloedema present, consider alternative diagnosis.
Complicates only 1% of meningitis.
Siezures are the presenting sign in > 30%
Predisposing factors.
o Usually none.
o Otitis media
o Mastoiditis
o Pneumonia
o Head injury
o Sickle cell disease
o Alcoholism
o Immunocompromise.
Causes in adults.
o Common.
Neisseria meningitides
Strep. pneumoniae
o Rarer.
Tend to affect elderly
Gram negative bacilli
Listeria
Assessment of severity.
o Mortality increases as consciousness decreases.
About 55% for comatose adults.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
21/30
o However, can proceed quickly in alert patients as well.
Management.
o Stabalize and resuscitate.
o Give oxygen
o CT scan.
Rule out raised ICP
Safest to use CT to determine safety of doing LP
Argument to say that this is only needed if.
o Decreased GCS
o Focal signs
o Papilloedema
o Signs suggesting impending cerebral herniation.
Discuss with senior collegue.
o Give empirical antibiotics.
Take blood cultures and LP before starting.
Dont wait for results before starting.
o Make definitive diagnosis with LP
o Review antibiotic treatemtn in light of LP result.
Consider Corticosteroid adjunct.
o Arrange for contacts tracing (including nursing and medical staff)
Give prophylactic antibiotics.
o Notify public health consultant
o Observe for and treat complications.
Antibiotic therapy.
o Follow hospital guidelines.o Adult patients with typical meningococcal rash.
IV benzylpenicillin 2.4 mg every 4 hours.o Adults < 50 without rash.
Cefotaxime 2g TDS
Ceftriaxone
2g BD
o Adults > 50 without rash.
Add 2g ampicillin every 4 hours to cover Listeria.
o If patient from are where penicillin and cephalosporin resistant pneumococci are
common (eg. Mediterranean countries).
Add IV vancomycin 500 mg QDS.
o If penicillin allergic. IV chloramphenicol 25 mg/kg + Vancomycin 500 mg QDS
If > 50, add co trimoxazole.
Discuss case with microbiologist.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
22/30
Lumbar puncture.
o Measure operating pressure.
Often raised to > 14 cm CSF in meningitis.
Very few reports of coning following procedure.
If pressure is raised.
Observations every 15 minutes.
Send for CT if not already done.
o Complications of meningitis
o Space occupying lesion, eg. Cerebral abscess.o Analysis of CSF.
Bacterial Viral TB
Appearance Turbid Clear Clear
Cells per mm3 5 2000 5 500 5 1000
Main cell type Neutrophil Lymphocyte Lymphocyte
Glucose (mM) Very low Normal Low
Protein (g/L) Often > 1 0.5 0.9 Often > 1
Other tests Gram stain
Bacterial antigen
PCR Ziehl - Neelsen
Fluorescent test
PCR
o WCC.
Bacterial meningitis typically causes high WCC with predominance of
neutrophils.
Low CSF WCC (0 20/mm3) with high bacterial count on Gram stain is
associated with poor prognosis.
o Glucose.
CSF: blood ratio < 3.1 in 70%
May be normal.
o Protien
Usually elevated
o Gram stain.
Positive in 60 90%
May be negative if there has been a delay between starting antibiotics and
lumbar puncture. Early antibiotics will also cause CSF culture yield to drop from 70 80% to
< 50%.o A bacterial CSF profile may appear in early stages of viral or TB meningitis.
Repeat CSF analysis will show transformation to luymphocytic predominance.
o Patients with CSF profile suggesting bacterial meningitis should be treated as such until
proven otherwise.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
23/30
Review of antiobiotics.
o If Gram ve diplococci are present.
Continue with benzylpenicillin or ampicillin.o If Gram +ve cocci diplococci present, change to:
2 g cefotaxime IV QDS
Consider Vancomycin 500 mg QDS
o If Gram +ve cocco bacilli present. Suggests Listeria.
Ampicillin 2 mg every 4 hours + gentamycin 5 mg/kg/day as single dose or split
into TDS.
o Adjuvant corticosteroids.
Reduces incidence of neurological sequelae.
Especially in pneumococcal meningitis.
Give in patients with.
Raised ICP
Stupor
Impaired mental status
Dose.
10 mg dexamethosome IV loading dose 4 6 mg PO QDS maintenance.
Prophylaxis for contacts.
o Give immediately.
o Adult contacts.
Rifampicin 600 mg BD for 2 days.
Ciprofloxacin 750 mg as single dose
o Children > 1 year.
Rifampicin 10 mg/kg BD for 2 days.
o Children 3 months 1 year.
Rifampicin 5 mg/kg BD for 2 days.
o Inform public health services when diagnosis made.
Can recommend on current best practice for prophylaxis.
Can assist with contact tracing.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
24/30
Complications.
o Raised ICP
Steroids
If evidence of brain shift or imending coning.
Mannitolo 1g/kg IV over 10 15 minutes.
o 250 ml of 20% solution for average adult.
Elevated head of bed to 30o.
Consider oral glycerol.
o Hydrocephalus.
Diagnosed by CT.
May require intraventricular shunt.
Discuss urgently with neurologists.
Can occur due to
Thickened meninges obstructing CSF flow.
Adherence of inflamed lining of aqueduct of Sylvius or 4th ventricular
outflow. Papilloedema may not be present.
o Seizures.
Treat as normal.
o Persistant pyrexia.
Suggest occult source of infection.
Carefully re examine patient.
Check oral cavity and ears.
o Focal neurological deficit.
May occur due to.
Arterial or venous infarction.
o Dont respond to anti coagulants.
Space occupying lesiono Eg. Subdural empyema.
Inflammation at base of skull can cause cranial nerve palsies.
Request CT scan if hasnt already been performed.
o Subdural empyema.
Rare complication.
Can cause.
Focal signs
Seizures
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
25/30
Papilloedmea
Requires urgent surgical drainage.
o DIC.
Ominous sign.
May require .
Platelets.
Fresh frozen plasma Discuss heparin use with neurologist and haematologist.
o SIADH.
Regularly check
Fluid balance
Electrolytes.
Lymphocytic CSF
Due to viral or TB meningitis.
Viral meningitis
o Clinically indistinguishable from acute bacterial meningitis.
o Normally self limiting.
TB meningitis.
o Usually preceded by history of malaise and systemic illness.
Can last days weeks.
o May present very acutely.
o Associated with.
Basal archnoditis
Vasculitis
Infarctions causing focal sings
Cranial nerve palsies Hydrocephalus with papilloedema
o Cryptococcal and syphilitis meningitis in the immunocompromised can present like TB
meningitis.
Causes.
o Viral.
Coxsackie
Echo
Mumps
Herpes simplex I
Varicella zoster
HIV
Lymphocytic choriomeningitis virus
o Non viral.
TB
Cryptococcus
Leptospirosis
Lyme disease
Syphilis
Brucellosis
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
26/30
Parameningeal infection with CSF reaction.
CSF findings.
o Usually demonstrates lymphocytosis.
Can start as demonstrating neutrophilso Important not to dismiss possibility of TB meningitis if CSF glucose is normal.
May be in 20% of cases.o Tuberculin may be negative in 20%
o M. Tuberculosis is seen in the initial CSF in 40% of patients with TB meningitis.
o Send SCF for viral and TB PCR.
Treatment.
o Viral meningitis normally requires only supportive measures.
o TB meningitis.
Dual therapy.
Pyrazinamide 30 mg/kg/day
Isoniazid 10 mg/kg/day
o Maximum isoniazid does of 600 mg/day.
o Give pyridoxine 10 mg/day to prevent isoniazid neuropathy.
Good CSF penetration.
If patient is conscious, for the first 3 months add.
Rifampicino 450 mg/day if weight < 50 kg
o 600 mg/day if weight > 50 kg.
Ethambutol
o 25 mg/kg/day
For the next 7 10 months give.
Rifampicin
o 450 mg/day if weight < 50 kg
o 600 mg/day if weight > 50 kg.
Isoniazid.
o 300 mg/day
Consult local respiratory/ infectious disease specialist for advice.
Different mycobacteria require different drug copmbinations.
Give corticosteroids if.
Raised ICP
Very high CSF protein levels.
o Cryptococcal meningitis.
Several regimens are used.
Two common ones last 6 weeks.
Amphotericin B as monotherpay.
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
27/30
o 0.6 1 mg/kg/day
Amphotericin B and Flucytosine dual therapy.
o Amp: 0.5 mg/kg/day
o Fluc: 150 mg/kg/day
Alternative in AIDS patients is Fluconazole.
400 mg/day initially
200 400 mg/day for 6 8 weeks.
Giant Cell arteritis
Commenest primary large vessel vasculitis.
o Oincidence of 1: 10000
Typically disorder of the elderly.
o Mean age of 70 years.
o Female: Male ratio of 2:1
Diagnosis is clinical, but supported by raised acute response proteins and temporal artery histology
o ESR
o CRP
o Thrombocytosis
Classical pathological discription is a segmented, granulomatous pan arteritis
Early stage changes may be simply
o Thickening of internal elastic lamina.
o Mononuclear cell infiltrate of wall.
Clinical features.
o Headache 90%
o Temporal artery tenderness 85%
o Scalp tenderness 75%
o Jaw claudication 70%
o Pulseless temporal artery 40%o Visual symptoms (including blindness) 40%
o Polymyalgic symptoms 40%
Proximal muscle stiffness without weakness or wasting
o Systemic features 40%
o Thickened/ nodular temporal artery 35%
o CVA or MI Rare
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
28/30
Investigations.
o FBC
Normochromic anaemia
Thrombocytosis
o LFTs
Elevated alkaline phophatase
o ESR > 50 mm in first hour.
95% sensitive
o CRP
Elevated
o CXR
To exclude underlying CA bronchus
o Urinalysis.
To exclude haematuria and protienuria
o Temporal artery biopsy.
Management.
o Immediate high dose prednisolone. Prevents blindness.
40 mg OD is normally sufficient.
60 80 mg may be used if patient already has visual symptoms.o All patients should have temporal artery biopsy within 48 hours of starting steroids to try
and confirm diagnosis.
May be negative due to skip lesion nature of disease.
Differential diagnosis is spondylisis.
Sinusitis
Symptoms.
o Blocked/ runny nose
o Frontal headache.
Worse on bending
o Chronic.
Post nasal drip
Cough
Frontal headache
Facial pain
Blcoked nose
Nasal polyps
History of allergic rhinitis
Signs.
o Tender over sinuses.
Above medial eyebrow
Bridge of nose
Below eyeso Pyrexia
Management.
o Saline nebulizers.
5 ml/ 2 4 hours.
o Beclamethosome nasal spray.
2 sprays to each nostril BDo Ephidrine nasal drops.
1 2 drops to each nostril QDS
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
29/30
Maximum of 7 days of therapy.
o If severe give Amoxycillin 500 mg TDS PO
Purulence mucus
Systemically unwell.
Complications.
o Local spread of infection.
Temperomandibular joint dysfunction
Caused by inflammation of TMJ
Can cause significant pain and dysfunction. Can be caused by any joint problems.
o Ankylosis
o Arthritis
o Trauma
o Dislocation
o Developmental abnormalities
o Neoplasia
Presentation
o Variable as can be due to any part of the joint.
Muscles
Nerves Tendons
Ligaments
Bone
Connective tissue
Teeth
o Commonly causes ear pain due to swelling of proximal tissues.
Signs and symptoms.
o Jaw pain
-
8/14/2019 Headache for Medical Finals (based on Newcastle university learning outcomes)
30/30
o Reduced jaw opening.
o Jaw clicking or popping
o Pressure on trigger points
o Toothache
o Ear ache
Causes.
o Overuse of muscles of mastication. Chewing gum continuously
Clenching teetho Infection
o Over opening mouth.
Treatment.
o Referral to a dentist.
o Repairing any damage to teeth.
o Simple pain relief.
May only give initial relief.o Low dose tricyclic antidepressants.
Due to anti muscarinci effect.
Nortriptyline
Amitriptyline.
o Correction of poor jaw action
Non repositioning stabilization splint may be helpful.
Biting on this too hard may worsen condition.
Anterior splint, which only has contact with front teeth, may help this
problem.o If these methods dont work, consider.
Arthrocentesis
Surgical reposition to correct congential abnormalities.
Replacement of the joints.