Greg Warren, MA, MBA President/CEO Baltimore Substance Abuse System, Inc.
64
Medications and Substance Abuse Treatment: The Clinical and Financial reasons for Putting It Into Practice Greg Warren, MA, MBA President/CEO Baltimore Substance Abuse System, Inc.
-
Upload
bethany-jackson -
Category
Documents
-
view
225 -
download
2
Transcript of Greg Warren, MA, MBA President/CEO Baltimore Substance Abuse System, Inc.
- Slide 1
- Greg Warren, MA, MBA President/CEO Baltimore Substance Abuse System, Inc.
- Slide 2
- Workshop Outline Introductions and objectives Baltimore Buprenorphine Initiative Review basic principles The Challenge of Change Practical issues Wrap up
- Slide 3
- Workshop Objectives Describe principles for thinking about incorporation of medications Provide framework for change as related to incorporation of medications Share practical tools that can apply to incorporation of medications Describe real-life successful models for integrating medications Interactive sharing of ideas, challenges and solutions to incorporating medications into substance abuse treatment
- Slide 4
- Slide 5
- Baltimore Achievements Innovative Practice by Agency recognition by federal Agency for Healthcare Research and Quality 2008. National Association of County and City Health Officials (NACCHO) Model Practice Award 2009. Network for the Improvement of Addiction Treatment (NIATx) iAward for Innovation in Behavioral Healthcare Services 2010. 5
- Slide 6
- BSAS is a quasi-public agency incorporated in 1990. It was established by the Baltimore City Health Department to manage the Center for Substance Abuse Treatments Targeted Cities Project. In 1995, BSAS became responsible for the management of the publicly-funded substance abuse treatment and prevention service system and is now an independent 501 3-C organization. The Chairman of the 27 member Board is the Citys Health Commissioner.
- Slide 7
- BSAS funds about 60 treatment, prevention, and intervention programs. Prevention 29 Residential 35 Outpatient 15 Medication Assisted 22 Ancillary Services Need analysis based on: The number of HIV cases Number of drug arrests Number of treatment admissions BSAS-Funded Programs Darker areas have high need
- Slide 8
- 71% Unemployed 50% < $10,000 per yr. 71% Unemployed 50% < $10,000 per yr. 83% Black, 16% White Less than 1% Hispanic 83% Black, 16% White Less than 1% Hispanic Characteristics of Clients in Baltimore City Programs FY 2009 70% between 30- 50 years of age 70% between 30- 50 years of age 13% Homeless 45% less than a 12 th grade education 45% less than a 12 th grade education 77% use tobacco 77% use tobacco 57% arrested in the past 2 years 60% male 60% male Treatment Episodes n = 21,000,.
- Slide 9
- Baltimore City Heroin addiction remains high Treatment capacity falls short of demand despite expansion in treatment system Estimated 30,000 individuals with opioid dependence ~4,000 methadone treatment slots Over 8,000 treatment admissions for opioids in FY 2009 Consequences from heroin addiction are severe Crime Family and community disruption Medical complications 1 in 48 Baltimore City residents are living with HIV and/or AIDS http://www.dhmh.state.md.us/AIDS/Data&Statistics/MarylandHIVEpiProfile122008.pdf
- Slide 10
- Slide 11
- Principle #1: Change Happens Accept change as a reality and an opportunity Nothing is permanent, but change Heraclitus 535-475 BCE It is not the strongest of the species that survive, nor the most intelligent, but the one most responsive to change Charles Darwin 1809-1882
- Slide 12
- Grant to PAC Transition As of Jan 1, 2010, the Maryland Primary Adult Care (PAC) Medicaid waiver program covers outpatient addiction treatment Assessment IOP/OP OMT Significant transition from grant to Medicaid fee-for- service funding mechanisms
- Slide 13
- Healthcare Reform H.R. 3590 Patient Protection and Affordable Care Act and Reconciliation Bill H.R. 4872 Implications for Substance Abuse Treatment Expands Medicaid eligibility to 133% of FPL SUD/MH services included in the basic benefits package required in exchange and for Medicaid recipients All plans in exchange must adhere to Wellstone/Domenici parity act provisions
- Slide 14
- Principle #2: Have a Method Use a systematic method for making changes to your program Individualize it Be flexible Acknowledge non-linear process of program change Examples NIATx model (www.niatx.net)www.niatx.net Transtheoretical models (http://www.attcnetwork.org/explore/priorityareas/techtrans/tools/chan gebook.asp)http://www.attcnetwork.org/explore/priorityareas/techtrans/tools/chan gebook.asp TAP 31: Implementing Change in Substance Abuse Treatment Programs www.samhsa.gov Adaptive models (http://www.drugabuse.gov/about/organization/despr/hsr/da- tre/DeSmetAdaptiveModels.html)http://www.drugabuse.gov/about/organization/despr/hsr/da- tre/DeSmetAdaptiveModels.html
- Slide 15
- Common Change Principles Know, and involve, your population Including community, patients, and staff Culture, attitudes, and knowledge level Pick, and equip, at least one leverage and additionally a change agent or champion in your program Given them appropriate authority and time Plan, do, reassess, revise and repeat
- Slide 16
- Principle #3: Data is Your Friend Make it simple and relevant Know it Use it Update it Knowledge is power Sir Francis Bacon 1561-1626
- Slide 17
- Principle #4: Why and Why Not? Keep asking the Why? questions Improves the process and the outcome Encourages critical thinking by everyone Helps articulate program messages Millions saw the apple fall, but Newton was the one who asked why Bernard M. Baruch 1870-1965 Ask the Why Not? questions Clarifies program vision Prevents stagnation I dream of things that never were, and ask why not? Robert F. Kennedy 1925-1968
- Slide 18
- Case Scenario You are an administrator of an urban facility that has been providing drug-free, outpatient substance abuse treatment for 30 years. Sixty percent of the funding for your organization comes from the state block grant. The Governor of your state has recently announced that he wants to double the number of individuals receiving buprenorphine by the year 2012. Your state agency enthusiastically supports this deliverable. How will your agency respond?
- Slide 19
- Questions for Consideration What does my program gain by incorporating medications? What do individuals accessing services in my program gain? What does my program risk by incorporating medications? What are the costs and how does my program sustain them? Others.
- Slide 20
- Questions for Case Scenario How will patients react to this? How will your staff react to this? What other issues do you need to consider? What are your next steps going to be?
- Slide 21
- Potential Challenges to Integrating Medications Program culture and philosophy Counselor attitudes and knowledge Patient, family, and community attitudes about medications
- Slide 22
- Problem Solving Form change team with representation from key stakeholder groups Gather and use data to identify critical measures to impact Patient surveys Staff surveys Relevant local and state data Outcomes for treatment as usual Ensure change team and others have sufficient information on medications to make informed decisions
- Slide 23
- Prescription Opioids Growing problem among adolescents and young adults* Allegany County -- 20% of 12 th graders reported ever having tried prescription opioids for non-medical purpose Talbot County 12% of 12 th graders reported currently using prescription opioids for non-medical purpose Effectively treated with buprenorphine** *Maryland Adolescent Survey: 2007http://www.marylandpublicschools.org/NR/rdonlyres/852505C8-7FDB-4E4E- B34E-448A5E2BE8BC/18944/MAS2007FinalReport_revised111808.pdf **Woody G. et al. JAMA 2008;300(17):2003-2011
- Slide 24
- Outcomes for Treatment As Usual Of 3753 admissions to Level I treatment in FY08, 51% retained for 90 days or more Of 11,013 treatment discharges in FY08, only Prince Georges county had smaller change in substance use Relapse rates high In methadone studies, 50-80% relapse within one year after detoxification 91% of patients receiving buprenorphine for 4 months had relapsed to prescription opioids within 2 months of taper* *Weiss R. et al. NIDA CTN Prescription Opioid Treatment Study. http://www.medscape.com/viewarticle/722342
- Slide 25
- Treatment Programs 911 Broadway Center A Step Forward Baltimore City Needle Exchange Baltimore Community Resource Center Bon Secours ADAPT Cares Bon Secours New Hope Bon Secours - Next Passage Daybreak/MBA Dees Place Family Health Centers of Baltimore Harbel Prevention and Recovery JH CAP JH BPRU IBR Reach Man Alive Partners in Recovery Pauls Place Powell Recovery Recovery in Community Sinai SHARP Bup Sinai SHARP - OMT Total Health Care Tuerk House ICF & HH Tuerk House OP Turning Point UMD - ADAP UMD - DTC Total Sites: 28
- Slide 26
- Suboxone: 9 Drug Free: 5 Methadone:11 Other: 3
- Slide 27
- 27
- Slide 28
- Financial Considerations for Medication Assisted Treatment Programs
- Slide 29
- BHCA and the PAC expansion Cost per client to have a BHCA advocate:$142.47 Outpatient Cost Savings (based on $5,500 cost per slot): Cost of OP treatment with avg. LOS at 130 days:$1,964.00 Cost of OP treatment if client is insured within 60 days: $916.67 Cost of BHCA advocate + 60 days of OP Treatment: $1,059.14 Savings per patient: $904.86 Total savings in OP treatment, based on total of 50 OP slots, turnover 2.8x annually:* $126,680.40 Estimated savings for 800 clients (2 advocates): $723,888
- Slide 30
- BHCA and the PAC expansion Cost per client to have a BHCA advocate:$142.47 Methadone Cost Savings: Cost per patient in OMT Slot (avg) of 1 client per slot, annually: $4,000.00 Cost per patient if insured within 60 days: $657.53 Cost of BHCA advocate + client who obtains insurance within 60 days: $800.00 Savings per patient: $3,200.00 Total annual savings for 100 OMT slots: $320,000.00 Estimated savings for 400 clients (1 advocate): $1.28 million
- Slide 31
- What Does Your Program Look Like?
- Slide 32
- Other Issues Program policies on medication management Dispensing vs. only prescribing Clinical policies on medication recalls, pill counts, etc Laboratory testing Resources needed Additional staff Medication costs Supplies and equipment State and federal regulations and licensing requirements
- Slide 33
- Factors to Consider In Medication Management Policies Risk of medication diversion Medication safety and side effect profile Staff input Existing policies Urinalysis testing Approach to positive urines Approach to late or missed payments for services Program behavior policies
- Slide 34
- Dispensing vs. Only Prescribing Pros of Dispensing Better control over patient adherence More control over medication Additional, potentially reimbursable, contacts with patients Cons of Dispensing Need more equipment More paperwork for labeling and tracking medication Cost of purchasing medications
- Slide 35
- Medication Costs Buprenorphine (Suboxone) 8mg/2mg tablet -- $6.18 per pill ($371 per month for 16 mg daily) 2mg/0.5mg tablet -- $3.35 per pill Naltrexone Oral (Revia) -- $170 per month for 50 mg per day Injectable (Vivitrol)* -- $700 for once monthly injection Acamprosate (Campral) -- $360 per month for 666 mg thrice daily Topiramate (Topamax) -- $240 per month for 200 mg per day Buproprion SR (Zyban) $300 per month for 150 mg twice daily Varenicline (Chantix) -- $110 per month for up to 1 mg twice daily *MD Medicaid does not cover Vivitrol
- Slide 36
- Resources Needed Physician to prescribe medication Physician coverage for vacations and emergencies Malpractice insurance Nurse to dispense and/or administer medication if physician does not Supplies and equipment Appropriate storage of medications, if dispensing Bottles, caps, labels, label printing software, if dispensing POC buprenorphine urinalysis testing kits
- Slide 37
- Regulation and Licensure Requirements DATA 2000 allows qualified, office-based physicians to prescribe approved medications for treatment of opioid dependence Sublingual buprenorphine currently is only medication approved for this purpose Nurse practitioners are currently not allowed to prescribe buprenorphine Practices subject to regular DEA visits To prescribe SUD medications physicians need Active state medical license Current state controlled substances license Current Federal DEA license
- Slide 38
- Clinical Program Goals and Medications Increase retention Improve counseling attendance Increase program completion rates Provide treatment options for patients Improve abstinence rates Others..
- Slide 39
- Buy-In and Mix of Patients Listen to staff concerns Start small Have clear program and clinical policies for selection and management of patients on buprenorphine Model behavior Measure impact and celebrate successes Consult with peers
- Slide 40
- Resources Grant funds State Local government Foundations SAMHSA/CSAT Third party payers Bill for all reimbursable contacts Ensure patients enrolled in all entitlements they are eligible for Look at payer mix Partner with a community health center or local physician practice Partner with another treatment program
- Slide 41
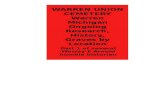
- Baltimore Buprenorphine Initiative
- Slide 42
- 42 Business Case for BBI in 2006 Baltimore needs more effective treatment for opioid dependence Review of literature and studies by UMBC Medical costs are increased for patients with drug abuse Opioid addicts on methadone consume far fewer Medicaid resources than addicts who go untreated Buprenorphine is economically viable alternative in city with limited methadone treatment capacity
- Slide 43
- BBI Goals Expand treatment for heroin addiction Access funding from larger medical care system Increase retention in treatment Link patients with ongoing medical care
- Slide 44
- Link from Treatment Program to Primary Care Is Key Initially 6 treatment providers In FY 2009 moved to 9 providers 58 continuing care physicians
- Slide 45
- 45 Transfer process Criteria for transfer Patient compliant with medication and counseling Patient opioid-free; reduced other drug use Patient responsible with take home medication and prescriptions Patient has insurance
- Slide 46
- BBI Results Currently, 357 patients receiving full BBI services in treatment program Approximately 6% drop-out from continuing care
- Slide 47
- Number of Clients Still in Counseling after Transfer 47
- Slide 48
- Achievements 4 times as many buprenorphine slots in Baltimore from 112 slots in 2008 to 506 slots in 2009 Four-fold increase in physicians trained to provide buprenorphine from 50 to 200 Patients receive buprenorphine within 48 hours of first treatment appointment 48
- Slide 49
- Sustaining Efforts Medicaid Primary Adult Care expansion Buprenorphine Medicaid Workgroup Increased Medicaid substance abuse service reimbursement rates BBI Clinical Guidelines Revise for PAC billing Recruiting for additional continuing care physicians 49
- Slide 50
- 6 months later The demand for buprenorphine has been overwhelming Patients are not getting PAC as quickly as you expected Clinical supervisors are wondering what to do with patients who continue to use cocaine or benzos BUT.. You just got your first check from Maryland Physicians Care for $20,000 and even got paid by Aetna for one patient Your treatment incompletion rate has gone from 50% to 39% You are getting many more self-referrals Staff morale has improved
- Slide 51
- Resources Healthcare Reform http://www.healthreform.gov/ http://www.healthreform.maryland.gov/ http://www.lac.org/index.php/lac/342 http://www.saasnet.org/drupal-6.6/taxonomy/term/18 ONDCP Drug Control Strategy Information: http://www.whitehousedrugpolicy.gov/strategy/
- Slide 52
- Resources Buprenorphine Information http://buprenorphine.samhsa.gov/bwns/index.html http://buprenorphine.samhsa.gov/bwns/tip43_curriculum.pdf http://buprenorphine.samhsa.gov/bwns/presentations.html Dispensing Regulations COMAR Title 10, Subtitle 19 (10.19.03) COMAR Title 10, Subtitle 13 (10.13.01) Federal DEA Controlled Substances Act Title 21, Chapter 13, Subchapter 1, Section C (http://www.justice.gov/dea/pubs/csa.html)http://www.justice.gov/dea/pubs/csa.html
- Slide 53
- Primary Adult Care A Limited Medical Assistance benefit
- Slide 54
- 54 Maryland Medicaid Provides benefits for an average more than 850,000 people one in 7 Marylanders Costs nearly $7 billion in state and federal funds PAC covers approximately 42,000 people (or 4.8% of the total Medicaid population)
- Slide 55
- 55 Program Enhancements Effective January 1, 2010 substance rates were increased for community providers HealthChoice and fee-for-service rates were increased Substance abuse was added to PAC
- Slide 56
- 56 What is PAC? The Primary Adult Care (PAC) Program began in July 2006 Federal eligibility requires that adults have dependent children to be Medicaid eligible. PAC was developed to provide benefits for adults without dependent children. Combined resources from state programs in public health and Medicaid A Medicaid program providing a limited benefit package for adults, including primary care, pharmacy, and outpatient health benefits to those over age 19 Eligible individuals must have incomes below 116% of the Federal Poverty Level (FPL) Administered through 5 participating Managed Care Organizations (MCOs)
- Slide 57
- 57 Who is eligible for PAC? Adults without dependent children 19 years or older who are: Maryland residents, Not on Medicare, and U.S. Citizens and legal residents ( five years residency) Enrollees do not need to have a medical disability to qualify Original income and asset requirements: For an individual: income less than 116% FPL and assets less than $4,000 For households greater than one: incomes less than 100% FPL and assets less than $6,000 April 1, 2009 - regulations changed to exclude asset requirements and income threshold is 116% FPL for all family sizes. This change mirrored standards for families with children. Most persons with children were also given the opportunity to receive full benefit package.
- Slide 58
- 58 PAC Eligibility Income Limits Person(s) Monthly Income 1 $1,046 2 $1,408 3 $1,769 4 $2,131 5 $2,493 6 $2,854 7 $3,216 8 $3,577
- Slide 59
- 59 Which health services are covered? PAC Covers the following health services: Free primary health care Prescriptions drugs Co-payment of u p to $2.50 for generic drugs and $7.50 for brand name drugs (pharmacist can deny drug if copayment is not paid) Free in-office mental health services through a counselor or psychiatrist Limited lab and diagnostic services Community-based substance abuse services (January 2010) Facility fees for emergency room visits (January 2010) Some benefits are carved out and covered fee for service, including Specialty Mental Health System services and drugs, and HIV/AIDS drugs
- Slide 60
- 60 How are services provided? Managed Care Organizations receive a monthly capitation payment for each enrollee All MCOs must participate in HealthChoice to serve PAC enrollees 5 MCOs currently provide services to PAC enrollees Maryland Physicians Care Priority Partners United Jai (Baltimore City & County only) Amerigroup To search participating providers by MCO online: https://encrypt.emdhealthchoice.org/searchable/main.action https://encrypt.emdhealthchoice.org/searchable/main.action
- Slide 61
- 61 PAC Expansion of Services PAC was scheduled to expand services to enrollees in July 2009, but this has been delayed due to budget limitations In January 2010, there were program changes, including: Substance rates were increased for community providers Substance abuse services are covered Some emergency room services are covered
- Slide 62
- 62 Codes and Rates for Self-Referred Community-Based Substance Abuse Services ServiceCodeHCPC DescriptionUnit of ServiceNew Rate Comprehensive Substance Abuse Assessment (CSAA) H0001Alcohol and/or drug assessmentPer assessment$142 Individual Outpatient Therapy H0004Behavioral health counseling and therapy Per 15 minutes$20 Group Outpatient Therapy H0005Alcohol and/or drug services; group counseling by a clinician Per 60-90 minute session $39 Intensive OutpatientH0015Alcohol and/or drug services; intensive outpatients (treatment program that operates at least three hours/day and at least three days/week and is based on an individualized treatment plan), including assessment, counseling, crisis intervention, and activity therapies or education. Per diem (minimum two hours of service per session) Maximum four days per week $125 Methadone Maintenance H0020Alcohol and/or drug services; methadone administration and/or service (provision of the drug by a licensed program) Per week$80
- Slide 63
- 63 Total PAC Enrollment July 2006 December 2009
- Slide 64
- 64 Five Counties with Highest PAC Populations CountyJuly 2008 Share of PAC PopulationDec 2009 Share of PAC Population Baltimore City14,58650%19,46347% Baltimore County2,8149%4,26110% Prince George's2,0307%3,1268% Anne Arundel1,2624%2,3356% Montgomery1,4935%2,0275%