Glutamate and GABA synthesis, release, transport and ... and GABA... · Glutamate and GABA...
Transcript of Glutamate and GABA synthesis, release, transport and ... and GABA... · Glutamate and GABA...

Neurochemistry International 61 (2012) 546–558
Contents lists available at SciVerse ScienceDirect
Neurochemistry International
journal homepage: www.elsevier .com/locate /nc i
Glutamate and GABA synthesis, release, transport and metabolism as targetsfor seizure control
Nicole M. Rowley a, Karsten K. Madsen b, Arne Schousboe b, H. Steve White a,⇑a Department of Pharmacology and Toxicology, Anticonvulsant Drug Development Program, University of Utah, Salt Lake City, UT 84108, USAb Department of Pharmacology and Pharmacotherapy, Faculty of Health and Medical Sciences, University of Copenhagen, 2100 Copenhagen, Denmark
a r t i c l e i n f o
Article history:Available online 18 February 2012
Keywords:PharmacologyTransgenic animalsAntiepileptic drugs
0197-0186/$ - see front matter � 2012 Elsevier Ltd. Adoi:10.1016/j.neuint.2012.02.013
⇑ Corresponding author. Address: Department of PAnticonvulsant Drug Development Program, UniversiSuite 3211, Salt Lake City, UT 84108, USA. Tel.: +1 804049.
E-mail address: [email protected] (H. Steve Wh
a b s t r a c t
The synthesis, release, reuptake, and metabolism of the excitatory and inhibitory neurotransmittersglutamate and GABA, respectively, are tightly controlled. Given the role that these two neurotransmit-ters play in normal and abnormal neurotransmission, it is important to consider the processes wherebythey are regulated. This brief review is focused entirely on the metabolic aspects of glutamate andGABA synthesis and neurotransmission. It describes in limited detail the synthesis, release, reuptake,metabolism, cellular compartmentation and pharmacology of the glutamatergic and GABAergic syn-apse. This review also provides a summary and brief description of the pathologic and phenotypic fea-tures of the various genetic animal models that have been developed in an effort to provide a greaterunderstanding of the role that each of the aforementioned metabolic processes plays in controllingexcitatory and inhibitory neurotransmission and how their use will hopefully facilitate the develop-ment of safer and more efficacious therapies for the treatment of epilepsy and other neurologicaldisorders.
� 2012 Elsevier Ltd. All rights reserved.
1. Introduction
The two most important neurotransmitters in the brain are glu-tamate and GABA. These two neurotransmitters control excitatoryand inhibitory neurotransmission, respectively (Hassel and Din-gledine, 2006; Olsen and Betz, 2006; Schousboe and Waagepeter-sen, 2008). Alteration of the balance in neurotransmission cancontribute to increased or decreased seizure activity (Schousboeand White, 2009). Since the mainstay of seizure control resideslargely with pharmacotherapy, it is not surprising that a numberof the available therapies either directly or indirectly shift thebalance away from excitatory neurotransmission in favor of inhib-itory neurotransmission. Neurotransmission typically involvesbiosynthesis, packaging, release, receptor interaction and inactiva-tion of the neurotransmitter. The present review will focus on adiscussion of the potential therapeutic targets associated withglutamate and GABA homeostasis, i.e. the pertinent metabolizingenzymes and the plasma membrane-associated high affinitytransporters.
ll rights reserved.
harmacology and Toxicology,ty of Utah, 417 Wakara Way,1 581 6447; fax: +1 801 581
ite).
2. Enzymes involved in glutamatergic and GABAergicneurotransmission
Enzymes that catalyze reactions in which glutamate is either asubstrate or a product include amino transferase, glutamatedehydrogenase, glutaminase, and glutamine synthetase. Aminotransferases always utilize glutamate and a-ketoglutarate (aKG)as a pair of substrates together with another amino acid and itscorresponding keto-acid (Fig. 1). Examples of pertinent amino-transferases are aspartate aminotransferase (AAT) and alanineaminotransferase (ALAT). Of these, AAT plays an important rolein mitochondrial glutamate metabolism (McKenna et al., 2006).
2.1. Biosynthesis of glutamate
Glutamate dehydrogenase (GDH) catalyzes the reaction be-tween glutamate, aKG, and ammonia using NAD+ or NADP+ asthe co-enzyme (McKenna et al., 2006). In the brain, this reactionnormally proceeds as an oxidative deamination, i.e. glutamate isoxidized to aKG and ammonia (Cooper et al., 1979; Schousboeand Waagepetersen, 2007). However, in glutamatergic neurons inwhich there may be a high content of ammonia in discrete micro-environments of the mitochondria (see below), the reaction mayconstitute reductive amination, i.e. formation of glutamate fromaKG and ammonia (Bak et al., 2005; Waagepetersen et al., 2000).

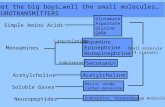
Fig. 1. Cartoon summarizing the synthesis, packaging, release, transport, and metabolism of glutamate and GABA. Glutaminase converts glutamine to glutamate, which isconverted to GABA by GAD in GABAergic neurons. The neurotransmitters are subsequently transported by vesicular transporters into vesicles for release. Upon release,neurotransmitters are taken up by high affinity membrane transporters into neurons and surrounding glia where they can be recycled or metabolized via several enzymes.Abbreviations: 2-OG, 2-oxoglutarate; AAT, aspartate aminotransferase; Aralar, aspartate-glutamate carrier; Asp, aspartate; EAAT, excitatory amino acid transporter; GABA-T,GABA transaminase; GAD, glutamic acid decarboxylase; GAT, GABA transporter; GDH, glutamate dehydrogenase; SSA, succinic semialdehyde; TCA, tricarboxylic acid cycle;vGAT, vesicular GABA transporter; vGlut, vesicular glutamate transporter.
N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558 547
Glutaminase, which is often referred to as phosphate activatedglutaminase (PAG) since it is stimulated by phosphate, catalyzesthe hydrolysis of the amide group of glutamine to form glutamateand ammonia (Kvamme et al., 2001). The activity and expression ofPAG is higher in neurons than in astrocytes with the highest valuesin glutamatergic neurons (Hogstad et al., 1988; Zaganas et al.,2001). It should be noted that an immunohistochemical study ofthe cerebellum found PAG immunoreactivity only in neuronal ele-ments (Laake et al., 1999).
Glutamine synthetase (GS) catalyzes the reverse reaction, whichis an ATP-dependent reaction that is responsible for the formationof glutamine from glutamate and ammonia (Fig. 1). Importantly,this enzyme is exclusively expressed in astrocytes (Norenbergand Martinez-Hernandez, 1979), making both glutamatergic andGABAergic neurons dependent on astrocytic delivery of the precur-sor glutamine for transmitter biosynthesis (Bak et al., 2006).
2.2. Pharmacology of glutamate metabolizing enzymes
2.2.1. PAGThe glutamate synthesizing enzyme PAG is highly regulated.
PAG is activated not only by phosphate but also by phosphorylatedcompounds such as trinucleotides (Weil-Malherbe, 1972). Interest-ingly, PAG is also activated by the TCA cycle intermediates succi-nate and citrate, albeit to a lesser extent than by phosphate(Kvamme et al., 1988). It is also of physiological and functionalimportance that this enzyme is inhibited by its products, ammoniaand glutamate. Interestingly, the inhibition by ammonia is muchless pronounced for the astrocytic than the neuronal enzyme(Hogstad et al., 1988; Kvamme et al., 1982). It is of pharmacologicalinterest that the compound 6-diazo-5-oxo-L-norleucine (DON) isan efficacious inhibitor of PAG (Shapiro et al., 1979) and can beused to investigate the functional importance of PAG in glutama-
tergic and GABAergic neurotransmission (Bradford et al., 1989;Conti and Minelli, 1994). In the present context it is of interest thatDON has been shown to protect seizure-susceptible mice fromconvulsions (Chung and Johnson, 1984).
2.2.2. GDHGDH is important in glutamatergic and GABAergic neurotrans-
mission as it directly regulates the glutamate concentration andindirectly modulates GABA levels by altering the availability ofprecursors. GDH is potently inhibited by GTP and activated byADP (Plaitakis and Zaganas, 2001). The amino acid leucine alsoactivates GDH, an effect that is synergistic with ADP (Plaitakisand Zaganas, 2001). While it may not be pharmacologically rele-vant, it is of considerable interest that GDH is inhibited by antipsy-chotic drugs such as chlorpromazine and haloperidol (Shemisa andFahien, 1971). It appears, however, that the potency of these drugsas inhibitors of GDH is quite low relative to blood levels observedin patients treated with chlorpromazine and haloperidol (Coueeand Tipton, 1990). It must be kept in mind that, in addition tothe ubiquitous GDH1 isozyme, humans express a unique GDH2 iso-form (Plaitakis and Zaganas, 2001) that exhibits a higher sensitivityto haloperidol. In this example, haloperidol may affect GDH inhumans at clinically relevant blood levels (Plaitakis et al., 2011).
2.2.3. GSAs stated above, GS is a key enzyme in the glutamate-glutamine
cycle and plays a major role in the brain homeostasis of glutamate,glutamine and ammonia. Hence, compounds that inhibit this en-zyme are of potential importance for studies that aim to elucidatethe functional role of GS in glutamatergic and GABAergic neuro-transmission. The most widely used compound to selectively inhi-bit GS is L-methionine sulfoximine (MSO), which at a concentrationof 5 mM in the presence of ATP almost completely inhibits the

548 N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558
enzyme (>90%) in an irreversible manner (Rowe et al., 1969).Inhibition of GS by MSO precipitates seizures (Tapia, 1975) and ithas been shown using MSO that GABA synthesis from glutamine,which is transferred to neurons from surrounding astroglia cells,is prevented by inhibition of GS (Sonnewald et al., 1993). Thismay be related to the convulsant action of MSO (Gershoff and El-vehjem, 1951; Tapia et al., 1967; Tews and Stone, 1964). The asso-ciation between the convulsant action of MSO and its ability toinhibit GS has, however, been questioned (Sellinger et al., 1968).More importantly from a clinical perspective, it has recently beenshown that MSO channels ammonia into alanine synthesis by theconcerted action of GDH and ALAT by preventing the synthesis ofglutamine under conditions of hyperammonemia (Dadsetan et al.,2011). This may be important since elevated brain glutamate levels,as seen during liver failure and hepatic encephalopathy, can lead toastrocytic swelling and brain edema (Albrecht et al., 2007, 2010).
2.3. Transgenic animals associated with altered glutamatergicmetabolizing enzymes
As summarized in Table 1, transgenic animals that display al-tered expression of GS, GDH, and PAG are available. Homozygousknockout of GS is lethal. Interestingly, heterozygotes do not displayspontaneous seizure activity. However, they are more susceptibleto hyperthermia-induced seizures, or experimental febrile seizures(van Gassen et al., 2009). Transgenic animals with an increase inGDH activity display increased glutamate levels and synaptic, neu-ronal, and dendritic loss in select brain regions. The frequency andamplitude of mEPSCs are significantly increased in GDHTg animals.Despite the increase in mEPSC frequency and amplitude observedin these animals, there is no evidence that they have increased sei-zure susceptibility (Bao et al., 2009). PAG knockout mice have im-paired respiratory function and die shortly after birth. Neuronscultured from these mice show altered evoked EPSCs but nochange in mEPSCs (Masson et al., 2006). Hence, glutamatergictransmission is persistent but altered in PAG knockout mice, sup-porting the importance of other glutamate-synthesizing pathways.The phenotypes of transgenic animals of glutamatergic metaboliz-ing enzymes are summarized in Table 1.
2.4. Biosynthesis of GABA
GABA metabolism is less complex than that of glutamate. Asfirst demonstrated by Roberts and Frankel (Roberts and Fran-kel,1950), GABA is synthesized by decarboxylation of glutamateby glutamic acid decarboxylase (GAD). GAD exists in two isoforms,GAD65 and GAD67, which have different molecular weights (65 and67 KDa), catalytic and kinetic properties, and subcellular localiza-tion (see (Walls et al., 2010, 2011). As discussed below, this is ofimportance for seizure control. Degradation of GABA requiresGABA-transaminase (GABA-T) to convert GABA to succinic semial-dehyde (SSA) by transamination with the co-substrates glutamateand aKG. SSA is subsequently oxidized by SSA dehydrogenase(SSADH) to succinate, a constituent of the TCA cycle. Alternatively,SSA can be reduced by c-OH-butyric acid dehydrogenase (GHBDH)to c-OH-butyric acid which can activate GABAB receptors (Kaup-mann et al., 2003).
Table 1Phenotypic features of transgenic animals that target enzymes involved in glutamate met
Pathway component Epilepsy-related phenotype
EnzymesGS+/� Homozygous KO lethal. Increased susceptibility to inGDH Tg Increased GDH levels, glutamate release, mEPSC freqPAG�/� Altered glutamatergic transmission. KO lethal within
Abbreviations: GS, glutamine synthetase; GDH, glutamate dehydrogenase; Tg, transgeni
2.5. Pharmacology of GABA metabolizing enzymes
2.5.1. GADInhibition of GAD, the GABA synthesizing enzyme, is known to
produce convulsions (Tapia and Pasantes, 1971). Since GAD isdependent on pyridoxal phosphate as the co-enzyme, carbonyltrapping agents like derivatives of hydrazine are generally convul-sant in nature (Tapia, 1975). Interestingly, aminooxyacetic acidwill act as a convulsant at high doses while at lower doses it isan anticonvulsant (Tapia, 1975). This is best explained by the factthat it inhibits GABA-T more potently than it inhibits GAD (Scho-usboe et al., 1974; Wu and Roberts, 1974). In this context it shouldbe noted that the convulsant 3-mercaptopropionic acid (Lamar, Jr.,1970) is a more potent inhibitor of GAD than of GABA-T (Scho-usboe et al., 1974; Wu and Roberts, 1974).
2.5.2. GABA-TLike GAD, GABA-T is a pyridoxal phosphate-dependent enzyme
(Schousboe et al., 1974). Thus, GABA-T is sensitive to carbonyltrapping agents. One of the most potent inhibitors of GABA-T isaminooxyacetic acid (Ki = 60 nM) (Schousboe et al., 1974). As such,it increases GABA levels and displays anticonvulsant activity in avariety of seizure models (Sarup et al., 2003; Tapia, 1975). The syn-thesis of the GABA analog, c-vinyl GABA (Lippert et al., 1977), hasbeen instrumental in the development of a novel antiepileptic drugthat acts by elevating synaptic GABA concentrations (Gram et al.,1988). This compound is a GABA-T substrate that displays irrevers-ible covalent binding to the active site of GABA-T upon transamina-tion and thus acts as a suicide, catalytic site-directed inhibitor(Lippert et al., 1977). This action explains the remarkable specific-ity displayed by c-vinyl GABA. Interestingly, its analog, c-acety-lenic-GABA, which also acts as a suicide inhibitor of GABA-T,inhibits GAD as well. It acts as an anticonvulsant drug against somebut not all types of experimentally induced seizures despite thefact that it is generally more potent as an inhibitor of GABA-T thanc-vinyl-GABA (Schechter et al., 1977a, 1977b). Due to its higherselectivity towards GABA-T relative to GAD, c-vinyl GABA wasdeveloped as a clinically active antiepileptic drug named vigabat-rin (Gram, 1990). Vigabatrin currently represents the only antiep-ileptic agent whose mechanism of action specifically relies oninhibition of GABA-T. Vigabatrin is also of particular interest be-cause it, like tiagabine (discussed in Section 4.5), emerged from amechanism-based drug discovery program.
2.6. Transgenic animals of GABA metabolizing enzymes
Animals lacking expression of GAD65, GAD67, and SSADH pro-vide insight into the role of each of these enzymes. GAD65 knockoutmice display no morphological abnormalities. Based on their ge-netic background, GAD65 knockout mice may or may not possessaltered basal GABA levels and/or display spontaneous seizuresand increased susceptibility to induced seizures. GAD65 knockoutsare also more susceptible to increased mortality compared to WTmice (Asada et al., 1996; Kash et al., 1997). Homozygous KO ofGAD67 is lethal due to formation of a cleft palate, and drastically re-duced GABA levels are observed. No increase in susceptibility topicrotoxin-induced seizures was observed in GAD67 heterozygous
abolism.
Reference(s)
duced seizures in heterozygotes van Gassen et al. (2009)uency and amplitude. No seizure phenotype Bao et al. (2009)36 h of birth Masson et al. (2006)
c; PAG, phosphate activated glutaminase.

Table 2Phenotypes of animals lacking enzymes associated withGABA metabolism.
Pathwaycomponent
Epilepsy-related phenotype Reference(s)
EnzymesGAD65�/� Spontaneous seizures leading to high mortality and increased susceptibility to induced
seizuresAsada et al. (1996) and Kash et al. (1997)
GAD67�/� Extreme decrease in GABA levels in homozygous KO. KO is lethal due to a cleft palate. Noseizure phenotype in heterozygotes
Asada et al. (1997)
SSADH�/� Absence-like seizures and EEG progressing to lethal status epilepticus. Alteredneurotransmitter metabolism
Chowdhury et al. (2007), Cortez et al. (2004), andGupta et al. (2003, 2004)
Abbreviations: GAD, glutamic acid decarboxylase; SSADH, succinic semialdehyde dehydrogenase.
N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558 549
animals (Asada et al., 1997).SSADH KO mice experience absence-like seizures during post-natal week two that progress to general-ized convulsive seizures in late post-natal week three, and areassociated with the onset of lethal status epilepticus (Cortezet al., 2004).No gross morphological deficits exist in the SSADHKO mice, although there is enhanced astrogliosis in the hippocam-pus (Hogema et al., 2001).SSADH KO mice exhibit an imbalance inseveral amino acids and their metabolism, including glutamine,GABA and glutamate (Chowdhury et al., 2007; Gupta et al.,2004). The phenotypic features of transgenic animals of GABAergicenzymes are summarized in Table 2.
2.7. Neuron-glia interactions in the biosynthesis of glutamate andGABA
Neurons cannot perform the net synthesis of glutamate andGABA from glucose due to the fact that neurons lack both the glu-tamine synthesizing enzyme, GS, and the prevailing anapleroticenzyme in the brain, pyruvate carboxylase (PC) (Bak et al., 2006;Norenberg and Martinez-Hernandez, 1979; Yu et al., 1983). Astro-cytes, on the other hand, express both of these enzymes and aretherefore obligatory for maintaining a supply of glutamine, theprecursor for glutamate and GABA (Bak et al., 2006). The exchangeof GABA, glutamate and glutamine is referred to as the glutamate-glutamine cycle (Bak et al., 2006). This was originally thought torepresent a stoichiometric exchange of glutamate and glutaminebetween neurons and astrocytes (Cotman et al., 1981), i.e. gluta-mate taken up by astrocytes would be quantitatively convertedto glutamine. It is, however, clear that this is not the case as gluta-mate in astrocytes can be oxidatively metabolized (Sonnewaldet al., 1997; Yu et al., 1982). The loss of glutamate is compensatedfor by de novo synthesis via pyruvate carboxylase which has beenshown to represent about 30% of the glutamate exchange relatedto glutamatergic activity (Oz et al., 2004).
In GABAergic neurons, glutamine released from astrocytes ap-pears to be an important precursor for GABA (Battaglioli and Mar-tin, 1991; Sonnewald et al., 1993; Walls et al., 2011) via formationof glutamate that is subsequently decarboxylated. It may be ofinterest that it has been shown using 13C-labeled precursors com-bined with magnetic resonance spectroscopy that conversion ofglutamine to GABA via glutamate may to a large extent involvethe mitochondrial TCA cycle (Waagepetersen et al., 2001). Hence,at least 50% of GABA synthesized by this pathway originates fromglutamate derived from aKG generated by the TCA cycle.
3. Release and termination of GABA and glutamateneurotransmitter activity
Release of intracellular GABA and glutamate to the extracellularspace can be accomplished by several mechanisms. Two of theseinclude: (1) A presynaptic action potential induces Ca2+-dependentexocytosis of vesicularly stored transmitter from the presynaptic
neuron into the synaptic cleft (Nicholls, 1989); (2) Reversal ofthe membrane-bound neurotransmitter transporter located eitheron pre- or postsynaptic neurons or adjacent astrocytes. A third pro-cess that can lead to release of intracellular glutamate and GABAinvolves the reversal of the cysteine/glutamate exchangers (Warret al., 1999), which can under certain conditions release non-vesic-ular GABA and glutamate to the extracellular space (Allen et al.,2004).
The release of neurotransmitters involves complex assemblyand release machinery that is outside the scope of this review(see Rizo and Rosenmund, 2008, for review and pertinent refer-ences). Rather, particular exocytotic proteins known to alter excit-ability will be described and the lessons learned from animalslacking these proteins will be discussed. Fig. 2 provides a very sim-plified schematic of these proteins. Synapsins are a family of pro-teins involved in the release of vesicles, and control the numberavailable for release.. Synaptic vesicle proteins control the regu-lated secretion of synaptic vesicles. SV2A and SV2B are the majorisoforms of synaptic vesicle protein 2. SV2A selectively enhanceslow-frequency neurotransmission and maintains the readilyreleasable pool of transmitters. Synaptotagmin-1 is localized tovesicle membranes and triggers calcium-dependent exocytosis.Munc proteins are important for vesicle priming prior to exocytoticrelease. The SNARE complex is a complex of proteins that mediatevesicle fusion. Three important proteins in the SNARE complex areSNAP-25, synaptobrevin, and syntaxin. All of the aforementionedproteins can alter neuronal excitability as discussed in section 3.1.
3.1. Transgenic animals of vesicular transporters
Knockout animals exist that lack the vesicular transporters forGABAand glutamate. The homozygous knockout of vGLUT1 maybe lethal (Wojcik et al., 2004), or animals may exhibit a severedecline in excitatory neurotransmission (Fremeau, Jr. et al.,2004).While no behavioral data exists, vGLUT1 KO animals displayaltered electrophysiological characteristics (Fremeau, Jr. et al.,2004; Wojcik et al., 2004).The homozygous KO of vGLUT2 is lethal.Heterozygous vGLUT2 animals do not display any EEG abnormali-ties; however, they are more susceptible to i.v.PTZ-induced sei-zures (Schallier et al., 2009).Neurons from vGLUT2 homozygousKO mice display drastically reduced EPSC amplitudes in the thala-mus but not hippcampus (Moechars et al., 2006). On average,vGLUT3 KO mice display one electrographic non-convulsive sei-zure per day. No morphological abnormalities have been describedin vGLUT3 KO mice (Seal et al., 2008). The knockout of vGAT islethal; these mice lack functional inhibitory synaptic transmissionand display several morphological abnormalities (Wojcik et al.,2006).
Several transgenic animals are available that display alterationsin the trafficking, packaging, and release of vesicularly stored neu-rotransmitters. Different constructs for a given protein may yielddiffering results and a full discussion is outside the scope of this re-

550 N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558
view. However, a brief overview is given here and in Table 3.Synap-sin KO mice exhibit various alterations in synaptic vesicle releasewhile displaying no anatomical abnormalities (Bogen et al., 2006;Li et al., 1995; Rosahl et al., 1995). Knockout mice of various synap-sins display spontaneous seizures and/or increased susceptibility toinduced seizures (Gitler et al., 2004; Li et al., 1995; Rosahl et al.,1995).While SV2B KO mice display no phenotype, SV2A andSV2A/SV2B double KO mice display spontaneous seizures and dieby two to three weeks of age. No differences were detected in mor-phology, synaptic formation, or EPSCs or IPSCs recorded from neu-rons cultured from SV2A, SV2B, or double KO mice. It is alsoimportant to note that KO of SV2A leads to a loss of function ofthe anticonvulsant drug levetiracetam (Lynch et al., 2004). Synapt-otagmin 1 KO mice die within two days of birth while heterozy-gotes display normal survival. There are no morphological orsynaptic formation differences between KO and WT animals. Syn-aptotagmin 1 is implicated in only synchronous release (Geppertet al., 1994).KO of Munc 13–1 yields a 90% reduction in excitatorypost-synaptic responses and weak animals that fail to feed anddie within a few hours of birth (Augustin et al., 1999). KO of Munc13–2 results in animals that experience sporadic seizures after12 months. Double KO of Munc 1 and 2 is lethal within one hourof birth. Embryonic neurons from these double KO animals displayno evoked or spontaneous release in electrophysiological studies(Varoqueaux et al., 2002). Munc 18–1 KO mice are born completelyparalyzed and die immediately after birth. Neurons from embry-onic KO mice reveal a loss of synaptic events despite functionalpost-synaptic receptors and ion channels (Verhage et al., 2000).
There are three major components that form the SNARE com-plex, all which have transgenic animals available: SNAP-25,VAMP/synaptobrevin, and syntaxin. The full KO of SNAP-25 abol-ishes evoked exocytotic release and mutants die at birth (Wash-bourne et al., 2002). Heterozygotes are indistinguishable fromWT mice; therefore, several different SNAP-25 gene-targetedmouse mutants with distinct phenotypes have been developed(for review and references see Bark, 2009). SNAP-25 deficiencycan lead to seizure activity, as well as pathological changes thatprogress with age (Bark, 2009; Tafoya et al., 2006; Washbourneet al., 2002). Mice completely lacking neuronal synaptobrevin-2experience impaired neurotransmission and early death (Schochet al., 2001) and the size and shape of vesicles is impaired whilethe number and docking are normal (Deak et al., 2004). In syntaxin1a KO mice, release parameters are not distinguishable from WTanimals, and KO mice survive and are viable (Fujiwara et al.,2006). In another study, mice lacking syntaxin 1a displayed noincreased mortality or phenotype, while mice that exclusivelyexpressed the open form of syntaxin 1b (1b open mutants) wereataxic and experienced lethal seizures at approximately twoweeks of age. Mice lacking syntaxin 1a displayed no differencesin EPSC characteristics, while 1b open mutants displayed a 40%increase in mEPSC frequency (Gerber et al., 2008). The interactionbetween Munc-18 and syntaxin 1a is regulated by cyclin depen-dent kinase 5 (Cdk5) (Shuang et al., 1998). KO of Cdk5 leads toincreased seizure susceptibility (Hawasli et al., 2009). The pheno-types of transgenic animals involved in the vesicular transport,trafficking, packaging, and release of neurotransmitters are sum-marized in Table 3.
4. Uptake of glutamate and GABA
The termination of GABAergic and glutamatergic neurotrans-mission and maintenance of extracellular GABA and glutamate lev-els is facilitated by high affinity transport proteins embedded inthe plasma membranes of neurons and astrocytes (Balcar andJohnston, 1972; Iversen and Kelly, 1975; Iversen and Neal, 1968).
4.1. Glutamate transporters
Glutamate transporters are expressed in the plasma membraneas well as in mitochondria and synaptic vesicles in glutamatergicneurons (Gegelashvili and Schousboe, 1997; Ozkan and Ueda,1998; Sluse, 1996). High affinity transporters for L-glutamate aswell as L- and D-aspartate have been found on both neurons andastrocytes with Km values ranging from 20–90 lM (Drejer et al.,1982, 1983; Schousboe et al., 1977). Isolation of a high affinity so-dium- and potassium-coupled glutamate transporter greatly aidedthe cloning of the glutamate transporters (Danbolt et al., 1990). Todate five plasma membrane glutamate transporters have beencloned and named GLAST (EAAT1) (Storck et al., 1992; Tanaka,1993), GLT-1 (EAAT2) (Pines et al., 1992), EAAC1 (EAAT3) (Kanaiand Hediger, 1992), EAAT4 (Fairman et al., 1995) and EAAT5 (Arri-za et al., 1997). Due to this confusing nomenclature, the abbrevia-tion excitatory amino acid transporter (EAAT) was introduced andwill be used throughout the remainder of this review. It is widelybelieved that EAAT1 and 2 are primarily localized on astrocytes,whereas EAAT3 is primarily localized postsynaptically on neurons(Danbolt, 2001).
The sequence homology of glutamate transporters is highlyconserved (>90%) amongst eukaryotes, with 38–65% sequencehomology among the different subtypes (Gegelashvili and Scho-usboe, 1997; Robinson and Dowd, 1997). The molecular structureof the glutamate transporters EAAT1 (Seal et al., 2000) and EAAT2(Grunewald and Kanner, 2000) has been proposed to be comprisedof eight transmembrane domains (TMDs) with a large extracellularloop between TMD3 and TMD4 containing N-glycosylation sites.Furthermore, the crystal structure of the glutamate transporterfrom Pyrococcushorikoshii (GltPh) has shed further light on thestructure of EAATs, confirming the eight TMD topology (Yernoolet al., 2004). However, the structure of GltPhdoes not exactly matchthat of the mammalian EAATs, and importantly the large extracel-lular loop between TMD3–4 is not present in GltPh (Yernool et al.,2004). Furthermore, it has been proposed that EAAT1, EAAT2,and GltPh exist as homo-multimers (Haugeto et al., 1996; Yernoolet al., 2004). The glutamate transporters utilize the electrochemicalgradient across the cell membrane to drive the uphill transport ofsubstrate. The stoichiometry of a single translocation cycle differsamongst the EAATs, but there is an absolute requirement for extra-cellular sodium influx and intracellular potassium efflux (Kannerand Sharon, 1978). It has been suggested for EAAT2 and 3 and GltPh
that three sodium ions and one proton are co-transported with glu-tamate into the cell while one potassium ion is transported out ofthe cell (Levy et al., 1998; Yernool et al., 2004; Zerangue and Kav-anaugh, 1996). For EAAT1 the co-transport of a proton was notdemonstrated (Klockner et al., 1993).
4.2. Pharmacology of glutamate transporters
Dysfunction of glutamate transporters has been implicated inseveral diseases such as epilepsy (Tanaka et al., 1997), amyotrophiclateral sclerosis (ALS), Alzheimer’s disease (Guo et al., 2003), andneuropathic pain (Mao, 2005). A common feature amongst thesediseases is neuronal cell death that can be caused by glutamate-in-duced excitotoxicity (Rothman and Olney, 1986). Neurodegenera-tion is implicated in the pathology of epilepsy and it is generallybelieved that the balance between inhibitory and excitatory neuro-transmission is tipped in favor of the latter.
Pharmacological approaches such as inhibiting glutamate trans-port or causing down regulation have been used in identifying thefunctional significance of each glutamate transporter subtypein vitro and in vivo; however, this strategy is without therapeuticsignificance. Quite to the contrary, it might lead to over-excitationand excitotoxicity. On the other hand, genetic overexpression of

Fig. 2. Cartoon illustrating the proteins involved in the docking of synaptic vesicles. Synapsins and SV2A allow regulation of the readily releasable pool of vesicles.Synaptobrevins, SNAP-25, and syntaxin form the SNARE complex, which binds directly with Munc-18 to allow fusion with the membrane and release of neurotransmitter.
N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558 551
EAAT2 in a mouse model of ALS significantly increases the lifespanof the mice, suggesting that elevated expression of EAAT2 can beneuroprotective (Guo et al., 2003). The underlying hypothesis forEAAT2-mediated neuroprotection is that glutamate excitotoxicityis limited due to enhanced uptake. However, overexpression ofEAAT2 is not always beneficial if the transporter reverses duringpathological situations (Yamada et al., 2006).
Interestingly, b-lactam antibiotics increase the expression andfunction of EAAT2 both in in vivo and in vitro models due to an in-crease in promoter activation. The experimental paradigms used toelucidate the neuroprotective action of the b-lactam antibiotic, cef-triaxone (CEF), include ischemia preconditioning (IPC) oxygen-glu-cose deprivation (OGD) of cultured neurons, which models theneurodegeneration sustained during ischemic injury (Rothsteinet al., 2005). It has been demonstrated that lethal OGD increasesglutamate release, causing neuronal death; however, subjectingthe neurons to a sublethal OGD insult 24 h prior to the lethalOGD insult induces resistance to neuronal cell death, partly bymediating an increase in EAAT2 function (Romera et al., 2004).CEF pretreatment 48 h prior to the lethal OGD insult preventedneuronal cell death. Moreover, it protected against THA- andTBOA-mediated motor neuron loss in an organotypic spinal cordmodel (Rothstein et al., 2005). The G93A SOD1 mouse is an animalmodel of ALS and shows reduced expression of EAAT2 near the on-set of clinical signs (Howland et al., 2002). When CEF treatmentwas initiated approximately at the onset of clinical signs (6–12 weeks), an increased survival time and a significant delay in lossof muscle strength and body weight was observed (Rothstein et al.,2005). Furthermore, Rothstein and coworkers have identified har-mine, a naturally occurring b-carboline alkaloid that up-regulatesnot only EAAT2 but also EAAT1 expression and function in vitroand in vivo. The EC50 for promoter activation is 3.2 lM and the on-set of toxicity is 30 lM. In spite of the up-regulation of proteinexpression in the G93A SOD1 mouse, no disease modification byharmine was reported (Li et al., 2011).
The use of b-lactam antibiotics as neuroprotective drugs mightnot be ideal when one considers the increasing problem ofmulti-drug resistant bacteria, which will have a more obviousand severe effect in already compromised patients. Moreover, the
dose needed to treat ALS is 5–6 times higher than the dose usedfor meningitis, and severe side effects often cause ALS patients todiscontinue the CEF treatment (Rawls et al., 2010). Inhibitors ofthe enzymeb-lactamase such as clavuanic acid and Tazobactam,as well as CEF, have been shown to inhibit planarian seizure-likeactivity induced by 3 mM of either cocaine or glutamate. Due tothe greater oral bioavailability of the b-lactamases versus b-lactamantibiotics and their negligible antibacterial effect, this class ofdrugs is of potential interest for managing CNS disorders (Rawlset al., 2010).
Further studies have revealed that activation of the nuclearreceptor peroxisome proliferator-activated receptor (PPAR) c usingthe agonist rosiglitazone is involved in the upregulation of EAAT2.Pretreatment with rosiglitazone 24 h prior to lethal OGD preventedneuronal cell death. This effect is reversed by dihydrokainate, dem-onstrating that the neuroprotective effect is mediated byEAAT2(Romera et al., 2007). Several other compounds have beenshown to enhance EAAT2 function including estrogens, glucocorti-coids, the novel neuroprotective compound MS-153, and riluzole,which is a registered drug for the treatment of ALS (Rilutek� fromSanofi-Avensis)(Azbill et al., 2000; Pawlak et al., 2005; Shimadaet al., 1999; Zschocke et al., 2005).
Interestingly, CEF induced upregulation of EAAT2 at doses of100 and 200 mg/kg but not 50 mg/kg, and was shown to signifi-cantly reduce cue-induced reinstatement of cocaine-seeking, butnot food-seeking, behavior in rats. Increased expression of EAAT2was found in both the prefrontal cortex and nucleus accumbenswhich is in agreement with the proposed hypothesis that relapseto cocaine-seeking behavior requires the release of glutamate fromthe prefrontal cortex projections to the nucleus accumbens. Thisplaces EAATs as potential key targets for the treatment of addiction(Sari et al., 2009).
4.3. Transgenic animals of glutamate transporters
As summarized in Table 4, the generation of several knockoutanimals havehelped to elucidate the function of the various EAATs.EAAT1 genetic KO in mice yields no overt seizure phenotype (Stof-fel et al., 2004) and no difference in kindling acquisition, but KO

Table 3Phenotypic features of animals lackingproteins involved in transport, trafficking, packaging, and release of vesicles.
Pathway component Epilepsy-related phenotype Reference(s)
Vesicular transportersvGlut1�/� Reduced evoked and field EPSP amplitudes, reduced glu release. Homozygous
KO may be lethal depending on constructFremeau et al. (2004) and Wojcik et al.(2004)
vGlut2+/� Homozygous KO lethal. In hets, no EEG phenotype but increased susceptibilityto induced seizures. Reduced EPSC amplitude in thalamus
Moechars et al. (2006) and Schallier et al.(2009)
vGlut3�/� Increased spike-wave activity with no motor seizures Seal et al. (2008)vGAT�/� Absence of vesicular release of GABA and glycine. KO lethal Wojcik et al. (2006)
Proteins involved in trafficking, packaging, and release of vesiclesSynapsin�/� Alterations in synaptic vesicle release. Spontaneous seizures and increased
susceptibility to induced seizures with the KO of various synapsinsBogen et al. (2006), Gitler et al. (2004), Liet al. (1995) and Rosahl et al. (1995)
SV2�/� No seizure phenotype in SV2B KO. SV2A and SV2A/B double KOs display spontaneousseizures leading to death. No alterations in EPSCs or IPSCs in cultured neurons for any SV2KO
Janz et al. (1999)
Synaptotagmin�/� Early lethality in homozygous KO. Decreased post-synaptic responses. Normal mEPSCs andcalcium-independent release
Geppert et al. (1994)
Munc 13�/� Reduced excitatory post-synaptic responses, normal IPSCs. Early death in Munc 13-1 KOs,sporadic spontaneous seizures in older (1 + years) Munc 13-2 KOs
Augustin et al. (1999) and Varoqueauxet al. (2002)
Munc 18�/� Loss of synaptic events. Paralyzed and die immediately at birth Verhage et al. (2000)SNAP 25�/� Altered synaptic function. Spontaneous seizure activity depending on construct Bark (2009) and Washbourne et al. (2002)VAMP/Synaptobrevin�/� Early death in homozygous KO. Alterations in release Deak et al. (2004) and Schoch et al. (2001)Syntaxin�/� Spontaneous lethal seizures and increased mEPSC frequency only in 1b open mutants Fujiwara et al. (2006) and Gerber et al.
(2008)
Abbreviations: vGlut, vesicular glutamate transporter; vGAT, vesivular GABA transporter, SV2, synaptic vesicle protein 2; Munc, mammalian uncoordinated; SNAP, synap-tosomal-associated protein; VAMP, vesicle-associated membrane protein.
Table 4Phenotype of animals lackingproteins involved in membrane transport of glutamate.
Pathwaycomponent
Epilepsy-related phenotype Reference(s)
Membrane transportersEAAT1
(GLAST)�/�No overt seizure phenotype. Alterations in susceptibility to induced seizures. Noalterations in EPSC amplitude or rise-time kinetics in cerebellar parallel fibersynapses
Nagatomo et al. (2007), Nikkuni et al. (2007), Stoffel et al. (2004),Tsuru et al. (2002), Watanabe et al. (1999) and Watase et al.(1998)
EEAT1 (GLAST)oligoknockdown
Excess glutamate and neurodegeneration leading to paralysis, but no seizurephenotype
Rothstein et al. (1996)
EAAT2 (GLT)�/� Spontaneous seizures Tanaka et al. (1997)EAAT2 (GLT)
oligoknockdown
Excess glutamate and neurodegeneration leading to paralysis, but no seizurephenotype
Rothstein et al. (1996)
EAAT3(EAAC1)�/�
No seizure phenotype. No alterations in synaptic currents, EPSC amplitude, orrise-time kinetics in cerebellar parallel fiber synapses
Huang et al. (2004a), Nikkuni et al. (2007), Peghini et al. (1997)
EAAT3 (EAAC1)oligoknockdown
Some spontaneous clonic and absence-like seizures. Decrease in mIPSCs Rothstein et al. (1996) and Sepkuty et al. (2002)
EAAT4�/� Increased or no alteration in amplitude and rise-time kinetics of EPSCs evoked bycerebellar parallel fiber stimulation
Huang et al. (2004a), Nikkuni et al. (2007) and Takayasu et al.(2005)
Abbreviations: EAAT, excitatory amino acid transporter; GLAST, glutamate aspartate transporter; GLT, glutamate transporter, EAAC, excitatory amino acid carrier.
552 N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558
mice displayed longer kindled seizures,a shorter latent period, andmore severe PTZ-induced seizures (Watanabe et al., 1999). Otherstudies, however, found that amygdale kindling of KO mice re-quired more time and that after-discharge duration was reducedin these mice (Nagatomo et al., 2007; Tsuru et al., 2002). In ratswhere EAAT1 levels were decreased by antisense oligonucleotideinfusion, progressive motor impairment culminating in hindlimbparalysis was observed, but no seizure phenotype emerged (Roth-stein et al., 1996). EAAT2 KO mice display spontaneous seizuresthat can be lethal, leading to a 50% survival rate at six weeks ofage. EEG performed on KO mice reveals high-voltage sharp wavebursts in response to a subthreshold PTZ dose that produces no re-sponse in WT animals (Tanaka et al., 1997). In rats, EAAT2 levelswere decreased 67% by antisense infusion and, although a motor
syndrome emerged, no seizure phenotype was observed (Rothsteinet al., 1996). Hippocampal slices from EAAT1 and EAAT2 KO micereveal that these transporters restrict the activation of mGluRs,while EAAT3 does not (Huang et al., 2004b).An EAAT1/EAAT2 dou-ble KO mouse was created, which displayed no overt seizure phe-notype (Stoffel et al., 2004).
In rats, EAAT3levels were decreased in two different studies byantisense knockdown. In one study, a motor syndrome was ob-served in half of the animals and 85% of all animals displayed tonicforepaw extension and clonic seizures (Rothstein et al., 1996). Inanother study, an absence seizure-like phenotype and EEG pattern,a 50% decrease in hippocampal GABAlevels, and excessive excit-ability were found (Sepkuty et al., 2002). In contrast, genetic KOof EAAT3 in mice revealed no seizure phenotype and no morpho-

N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558 553
logical abnormalities (Huang et al., 2004a; Peghini et al., 1997). Nodifferences were observed in several electrophysiological parame-ters (Huang et al., 2004a; Nikkuni et al., 2007). In EAAT4 KO mice,mGluRs are more strongly activated than in WT mice (Nikkuniet al., 2007). In contrast, EAAT4 KO mice experience no differencein evoked EPSCs, although a long-lasting tail current did appearin an age-dependent manner in KO mice (Takayasu et al., 2005).EAAT4 KO mice possess no glutamate transporter current in Pur-kinje cell climbing fibers and no morphological abnormalities(Huang et al., 2004a).The phenotypes of transgenic animals of glu-tamate transporters are summarized in Table 4.
4.4. GABA transporters
GABA transporters (GATs) are expressed on the plasma mem-branes of neurons astrocytes (Iversen and Neal, 1968) and on syn-aptic vesicles (Kish et al., 1989). The isolation of an 80 kDaglycoprotein that showed a dependency for sodium and chloridefor transport and an estimated Km of 3 lM preceded the cloningof the GATs (Radian et al., 1986). Shortly following the findingsof Radian and colleagues, four GATs were cloned from several spe-cies. Unfortunately, this led to a confusing nomenclature that hasbeen listed in Table 5 along with the solute carrier (SLC) genenamesfor simplicity.
The mouse GATs, mGAT1–4, correspond to GAT-1, BGT-1, GAT-2, and GAT-3, respectively, in humans and rats. The standardizednomenclature proposed by the HUGO Gene Nomenclature Com-mittee will be used in this review unless otherwise stated.mGAT1–4 have an apparent Km values for GABA of 7, 79, 18, and0.7 lM (Liu et al., 1993), respectively, whereas the apparent Km
for the human GATs have been reported as 11, 18, 8.1, and0.56 lM, respectively (Kvist et al., 2009). The only major differencebetween the two species is the apparent fourfold higher Km in micefor the betaine-GABA transporter, BGT1. BGT1 also transports beta-ine, although with a lower Km (398 lM for mGAT2). GAT2 andGAT3 also have the capacity to transport b-alanine and taurine(Liu et al., 1993).The GATs move GABA against its concentrationgradient by utilizing the inward sodium gradient. The stoichiome-try for the transport process is two to three sodium ions, one chlo-ride ion, and one GABA molecule (Kanner, 1994).
The genes for GAT1, BGT1, GAT2, and GAT3 encode proteins of598, 614, 602, and 627 amino acids, respectively (Liu et al., 1992,1993). GAT1 seems to be somewhat more distantly related to theother GATs, sharing only 50% sequence homology, whereas the se-quence identity is 65–70% amongst BGT1, GAT2, and GAT3 (Milleret al., 2002).Crystallization of LeuT, a sodium-dependent bacterialLeucine transporter, has given great insight into the proteindynamics and translocation process of the SLC6 gene family,includ-ing the substrate binding pocket (Yamashita et al., 2005). The GATsare composed of 12 TMDs with the N- and C- termini located intra-cellularly (Chen et al., 2004) for review please see (Madsen et al.,2007).
The regional and cellular distribution of the GATs differs dra-matically within the brain. GAT1 and GAT3 are restricted to thebrain, whereas BGT1 and GAT2 are found in multiple other organs.
Table 5Nomenclature of GATs.
SLC gene SLC6a1 SLC6a12 SLC6a13 SLC6a11
Mouse GAT1 GAT2 GAT3 GAT4Human/rat GAT-1 BGT-1 GAT-2 GAT-3HUGO GAT1 BGT1 GAT2 GAT3
Abbreviations: SLC, solute carrier; GAT, GABA transporter; BGT, betaine-GABAtransporter.
GAT1, the most studied of the GATs, is expressed throughout thebrain (Durkin et al., 1995) along GABAergic pathways (Radianet al., 1990). GAT1 is primarily found on presynaptic GABAergicneurons and to a minor degree on distal processes in close proxim-ity to axon terminals forming symmetric synapses (Borden, 1996;Conti et al., 1998). The expression of GAT3 is much more restrictedcompared to the widespread expression of GAT1. GAT3 is primarilylocated on distal astrocytic processes that are in direct contact withGABAergic terminals and to a lesser degree on neuronal elements(Durkin et al., 1995; Minelli et al., 1996). The expression of BGT1and GAT2 are very limited and they partition to the basolateral sidein polarized MDCK cells, which is strikingly opposite to that ofGAT1 and GAT3 which localize to the apical side (Ahn et al.,1996). GAT2 seems to be highly abundant in the mouse neonatalbrain compared to the adult brain (Liu et al., 1993). In the adultrat brain, GAT2 shows strong expression in the leptomeningesand ependyma and weak expression in cortical neurons and astro-cytes. The opposed localization of GAT2 compared to GAT1 andGAT3 in MDCK cells is to some extent also paralleled in brain cells.GAT2 is found on dendrites and in axon terminals forming bothsymmetric and asymmetric synapses but away from areas withsynaptic specialization, contrary to GAT1. The localization ofGAT2 in distal astrocytic processes is similar to that of GAT1 andGAT3, whereas the localization of GAT2 to astrocytic cell bodiesand proximal processes is not (Conti et al., 1999). Although some-what controversial due to the unavailability of highly specific anti-bodies, BGT1 has been found throughout the adult brain (Bordenet al., 1995) and in the leptomeninges (Evans et al., 1996; Takanagaet al., 2001). BGT1 has also been found on pyramidal neurons in thecerebral cortex and hippocampus. Furthermore, BGT1 was foundon dendritic spines or small diameter dendrites in contact withasymmetric synapses (Zhu and Ong, 2004). Collectively, the local-ization of BGT1 and GAT2 suggest that their involvement in directsynaptic GABAergic neurotransmission is limited. Rather, they mayplay a more important role in the regulation of extrasynaptic GABAlevels.
4.5. Pharmacology of GABA transporters
As alluded to in section 2.5, a mechanism-based drug discoveryprogram established tiagabine as an anticonvulsant that selectivelyinhibits GAT1 (Nielsen et al., 1991). At the same time as Novo Nor-disk developed tiagabine, other companies like Parke-Davis/War-ner-Lambert and SKF were developing the GAT inhibitors CI-9and SK&F 89976A, respectively (Ebert and Krnjevic, 1990; Yungeret al., 1984); however, the clinical trials were terminated due toconsiderable adverse effects (Radulovic et al., 1993). The use oftiagabine as an anticonvulsant is limited to add-on therapy for par-tial epilepsy.
As described above, the heterogenous localization of GATs in theCNS places them strategically within and around the synapse onboth neurons and astrocytes (GAT1 and GAT3), and to the extrasy-naptic region (GAT2 and BGT1). Approximately 20% of releasedGABA is taken up by astrocytes (Schousboe, 2000). As described insections 2.5 and 2.7, GABA is subsequently converted to succinatevia GABA-T and SSADH, and replenishment of GABA precursor inneurons relies on the glutamine-glutamate cycle. In seizure-com-promised neuronal circuits where GABAergic neurotransmission isattenuated, reduction of neuronal GABA stores is unwanted and willlead to a further exacerbation of seizures. It has therefore been pro-posed that selective inhibition of astrocytic GABA transport wouldincrease extracellular levels of GABA, thus increasing presynapticuptake and recycling of GABA thereby avoiding transmitter drain-age and lowering seizure susceptibility (Schousboe et al., 1983).
GAT3 would be the obvious pharmacological target for selectiveastrocytic transport because it is located almost exclusively on

554 N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558
astrocytes and only to a minor degree on neurons, contrary toGAT1, which is the prevalent neuronal transporter with minorexpression on astrocytes. Unfortunately, the development of selec-tive GAT3 inhibitors has proven difficult. SNAP-5114, which alsoinhibits GAT2 and BGT1but has little activity for GAT1, is the mostcommonly used GAT3 inhibitor (Borden et al., 1994).
A series of astrocyte-selective inhibitors have been developed.The most potent of these is N-methyl-exo-THPO, which displaysan almost 10-fold selectivity for astrocytes compared to neurons(White et al., 2002). Interestingly, these compounds were all foundto be GAT1 selective (White et al., 2002). Due to the poor bloodbrain barrier penetration of N-methyl-exo-THPO, it was substi-tuted with a lipophilic aromatic side chain resulting in the interest-ing compound EF1502, which is selective for GAT1 and BGT1 butequipotent at neurons and astrocytes (Clausen et al., 2005).EF1502 was the first compound synthesized that inhibits BGT1and it has been extensively studied to elucidate the utility ofBGT1 as a pharmacological target for the treatment of seizures.EF1502 was shown to possess a broad anticonvulsant profile in ro-dent seizure models. Moreover, EF1502 was tested in combinationwith the GAT1 selective inhibitors, tiagabine and LU-32–176B,using the isobologram experimental design (Loewe, 1953) in theaudiogenic seizure-susceptible Frings mouse. A synergistic anti-convulsant effect was observed when EF1502 was combined witheither of the GAT1 selective compounds, whereas the combinationof the two GAT1 selective compounds tiagabine and LU-32–176Bresulted in an additive anticonvulsant effect. It was concluded fromthis study that inhibition of BGT1, rather than inhibition of GAT1,was likely responsible for the observed synergistic effects ofEF1502 with GAT1 inhibitors (White et al., 2005). Similarly,EF1502 was combined with the moderately selective GAT3 inhibi-tor, SNAP-5114, resulting in a synergistic anticonvulsant effect atsome dose mixtures, whereas tiagabine combined with SNAP-5114 resulted in an additive anticonvulsant interaction (Madsenet al., 2009). The cellular localization of the GATs was proposedto explain the results obtained by combining GAT inhibitors withdifferent subtype selectivity. Inhibition of GAT1, almost exclusivelyexpressed on presynaptic neurons within the synapse (Borden,1996; Conti et al., 1998), and GAT3, expressed on distal processesof astrocytes in close proximity to the synapse (Durkin et al.,1995; Minelli et al., 1996), results in increased synaptic GABA lev-els which activate synaptic GABA receptors that mediate inhibitoryneurotransmission. Combined inhibition of GAT1 and GAT3 there-fore only activates the synaptic GABA receptors. BGT1 is locatedoutside the synapse, probably on glutamatergic neurons (Zhu andOng, 2004), where there exists the potential of extrasynapticreceptor activation through locally elevated GABA levels. There-fore, the combined inhibitory effect of GAT1 and BGT1 or GAT3and BGT1 may result in the activation of two very different popu-lations of GABA receptors, namely synaptic benzodiazepine-sensi-tive and extrasynaptic benzodiazepine-insensitive GABA receptors,respectively. These have also been referred to as phasic and tonicGABA receptors, respectively. Taken together, these results high-light the mechanistic differences between tiagabine and EF1502
Table 6Phenotypes of animals transgenic for GABA membrane transporters.
Pathwaycomponent
Epilepsy-related phenotype
Membrane transportersGAT1 Tg Increased susceptibility to induced seizuresGAT1�/� Continuous tremor and slightly increased susceptibility to induced
decreased phasic inhibitory conductancesBGT1�/� No spontaneous seizure phenotype or increased susceptibility to in
Abbreviations: GAT, GABA transporter; Tg, transgenic; BGT, betaine-GABA transporter.
and support a functional role for BGT1 and extrasynaptic GABAA
receptors in mediating GABAergic neurotransmission.Recently, a study was conducted to highlight the mechanistic
difference between EF1502 and tiagabine in their ability to interactwith the selective extrasynaptic GABAA receptor agonist, gabox-adol (Madsen et al., 2011). Gaboxadol at low concentrations (1–3 lM) will selectively activate extrasynaptic GABAA receptors(Wafford and Ebert, 2006). Concentrations in this range areachieved by clinically relevant doses of gaboxadol, which has ahigher efficacy but lower potency than GABA at a4b3d-containingGABAA receptors (Cremers and Ebert, 2007; Storustovu and Ebert,2006; Wafford and Ebert, 2006). Gaboxadol was shown to protectagainst sound-induced seizures in the Frings mouse and induceataxia in CF1 mice. Combining gaboxadol with tiagabine orEF1502 resulted in an additive or antagonistic anticonvulsant ef-fect, respectively. Also, EF1502 was able to reverse the gabox-adol-induced ataxia while tiagabine was not. This clearlydemonstrates the difference in mechanism of action of tiagabineand EF1502. In order to antagonize the anticonvulsant effect ofgaboxadol and reverse the gaboxadol-induced ataxia, EF1502 islikely able to elevate the extrasynaptic GABA concentration, pre-sumably by inhibiting BGT1 (Madsen et al., 2011). A recent studythat produced a BGT1 knockout mouse didn’t reveal a BGT1-dependent seizure phenotype, and showed that BGT1 is presentin very low amounts in the brain compared to GAT1 as analyzedby mRNA levels (Lehre et al., 2011). However, this data doesn’t nec-essarily exclude BGT1 as an important pharmacological target, asthe global knockout of a transporter may involve complicateddevelopmental compensation, and low expression levels do notnecessarily preclude a function. Furthermore, brain BGT1 mRNAexpression has been shown to be altered in a model of epilepsy(Rowley et al., 2011). Hence, the determination of a functionalassociation between BGT1 and GABAergic neurotransmission re-mains under investigation.
4.6. Transgenic animals of GABA transporters
Table 6 summarizes the results obtained from transgenic ani-mals developed to evaluate the role of various GABA transporters.GAT1 KO mice display a continuous tremor in the limbs and tailand are slightly more sensitive than WT mice to PTZ-, but not bicu-culline-induced, seizures (Chiu et al., 2005). GAT3,vGAT, and GAD65
expression, as well as GABAA and GABAB receptor density, are notaltered in GAT1 KO mice (Chiu et al., 2005; Jensen et al., 2003).GAD65/67 was reported to be increased and tonic and phasic inhib-itory conductances are significantly enhanced in GAT1 KO mice(Bragina et al., 2008; Jensen et al., 2003). GAT1 overexpressingtransgenic (GAT1 Tg) mice display increased GABA uptake and in-creased seizure susceptibility to induced seizures (Ma et al., 2001a;Zhao et al., 2003). GAT1 Tg mice experience up-regulation of GA-BAA receptors and GLT1, and a reduction in asymmetric synapses(Ma et al., 2001a, 2001b). BGT1 KO mice display no seizure pheno-type (Lehre et al., 2011). The phenotypes of transgenic animals ofGABA transporters are summarized in Table 6.
Reference(s)
Ma et al. (2001a,b) and Zhao et al. (2003)seizures. Increased tonic but Bragina et al. (2008), Chiu et al. (2005) and
Jensen et al. (2003)duced seizures Lehre et al. (2011)

N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558 555
5. Conclusion/Perspectives
Excitatory and inhibitory tone within the CNS is set by the neu-rotransmitters glutamate and GABA, respectively. The processes bywhich each of these neurotransmitters is synthesized, released, re-moved from the synaptic and extrasynaptic cleft and metabolizedare all tightly regulated and have for many years been targets fordrug discovery. For the GABAergic synapse, knowledge of the path-ways whereby GABA is removed from the synaptic cleft (e.g.,GAT1) and metabolized (e.g., GABA-T) has led to the synthesisand development of two commercially available antiepilepticdrugs; i.e., tiagabine and vigabatrin, respectively. Furthermore,the recognition that GABA uptake is not limited to GAT1 but islikely controlled by at least three other GATs has fostered researchto understand the role of these transporters and whether they toorepresent viable targets for therapy development. Unfortunately,similar efforts to exploit the mechanisms through which glutamateis synthesized, released, and removed from the synaptic cleft havefailed to lead to the development of any commercially availableneuroprotective or antiepileptic therapies. However, it is impor-tant to note that attempts to increase the expression of glutamatetransporters has shown promise as a neuroprotective strategy forALS and other neurodegenerative disorders. The use of geneticallyaltered mice wherein the regulatory pathways controlling gluta-mate and GABA synthesis, release, reuptake, and metabolism havebeen altered are providing new and useful tools that could fosterthe development of new therapies for a number of neurologicaldisorders. The myriad of emerging animal models will also providegreater insight into the pathophysiology of CNS disorders at themolecular and genetic levels. Each new advance will open moreavenues for the early discovery and development of safer and moreefficacious therapies in the years to come.
Acknowledgments
The work has been financially supported by the Carlsberg Foun-dation (2009_01_0501), the Lundbeck Foundation (R19-A2199),and the NINDS,(NIH 1-N01-NS-4-2359).
References
Ahn, J., Mundigl, O., Muth, T.R., Rudnick, G., Caplan, M.J., 1996. Polarized expressionof GABA transporters in Madin-Darby canine kidney cells and culturedhippocampal neurons. J Biol Chem 271, 6917–6924.
Albrecht, J., Sonnewald, U., Waagepetersen, H.S., Schousboe, A., 2007. Glutamine inthe central nervous system: function and dysfunction. Front Biosci 12, 332–343.
Albrecht, J., Zielinska, M., Norenberg, M.D., 2010. Glutamine as a mediator ofammonia neurotoxicity: A critical appraisal. Biochem Pharmacol 80, 1303–1308.
Allen, N.J., Karadottir, R., Attwell, D., 2004. Reversal or reduction of glutamate andGABA transport in CNS pathology and therapy. Pflugers Arch 449, 132–142.
Arriza, J.L., Eliasof, S., Kavanaugh, M.P., Amara, S.G., 1997. Excitatory amino acidtransporter 5, a retinal glutamate transporter coupled to a chlorideconductance. Proc Natl Acad Sci U S A 94, 4155–4160.
Asada, H., Kawamura, Y., Maruyama, K., Kume, H., Ding, R., Ji, F.Y., Kanbara, N.,Kuzume, H., Sanbo, M., Yagi, T., Obata, K., 1996. Mice lacking the 65 kDa isoformof glutamic acid decarboxylase (GAD65) maintain normal levels of GAD67 andGABA in their brains but are susceptible to seizures. Biochem Biophys ResCommun 229, 891–895.
Asada, H., Kawamura, Y., Maruyama, K., Kume, H., Ding, R.G., Kanbara, N., Kuzume,H., Sanbo, M., Yagi, T., Obata, K., 1997. Cleft palate and decreased brain gamma-aminobutyric acid in mice lacking the 67-kDa isoform of glutamic aciddecarboxylase. Proc Natl Acad Sci U S A 94, 6496–6499.
Augustin, I., Rosenmund, C., Sudhof, T.C., Brose, N., 1999. Munc13-1 is essential forfusion competence of glutamatergic synaptic vesicles. Nature 400, 457–461.
Azbill, R.D., Mu, X., Springer, J.E., 2000. Riluzole increases high-affinity glutamateuptake in rat spinal cord synaptosomes. Brain Res 871, 175–180.
Bak, L.K., Schousboe, A., Waagepetersen, H.S., 2006. The glutamate/GABA-glutaminecycle: aspects of transport, neurotransmitter homeostasis and ammoniatransfer. J Neurochem 98, 641–653.
Bak, L.K., Sickmann, H.M., Schousboe, A., Waagepetersen, H.S., 2005. Activity of thelactate-alanine shuttle is independent of glutamate-glutamine cycle activity incerebellar neuronal-astrocytic cultures. J Neurosci Res 79, 88–96.
Balcar, V.J., Johnston, G.A., 1972. The structural specificity of the high affinity uptakeof L-glutamate and L-aspartate by rat brain slices. J Neurochem 19, 2657–2666.
Bao, X., Pal, R., Hascup, K.N., Wang, Y., Wang, W.T., Xu, W., Hui, D., Agbas, A., Wang,X., Michaelis, M.L., Choi, I.Y., Belousov, A.B., Gerhardt, G.A., Michaelis, E.K., 2009.Transgenic expression of Glud1 (glutamate dehydrogenase 1) in neurons:in vivo model of enhanced glutamate release, altered synaptic plasticity, andselective neuronal vulnerability. J Neurosci 29, 13929–13944.
Bark, C., 2009. SNAP-25 and gene-targeted mouse mutants. Ann N Y Acad Sci 1152,145–153.
Battaglioli, G., Martin, D.L., 1991. GABA synthesis in brain slices is dependent onglutamine produced in astrocytes. Neurochem Res 16, 151–156.
Bogen, I.L., Boulland, J.L., Mariussen, E., Wright, M.S., Fonnum, F., Kao, H.T., Walaas,S.I., 2006. Absence of synapsin I and II is accompanied by decreases in vesiculartransport of specific neurotransmitters. J Neurochem 96, 1458–1466.
Borden, L.A., 1996. GABA transporter heterogeneity: pharmacology and cellularlocalization. Neurochem Int 29, 335–356.
Borden, L.A., Dhar, T.G., Smith, K.E., Branchek, T.A., Gluchowski, C., Weinshank, R.L.,1994. Cloning of the human homologue of the GABA transporter GAT-3 andidentification of a novel inhibitor with selectivity for this site. ReceptorsChannels 2, 207–213.
Borden, L.A., Smith, K.E., Gustafson, E.L., Branchek, T.A., Weinshank, R.L., 1995.Cloning and expression of a betaine/GABA transporter from human brain. JNeurochem 64, 977–984.
Bradford, H.F., Ward, H.K., Foley, P., 1989. Glutaminase inhibition and the release ofneurotransmitter glutamate from synaptosomes. Brain Res 476, 29–34.
Bragina, L., Marchionni, I., Omrani, A., Cozzi, A., Pellegrini-Giampietro, D.E.,Cherubini, E., Conti, F., 2008. GAT-1 regulates both tonic and phasic GABA(A)receptor-mediated inhibition in the cerebral cortex. J Neurochem 105, 1781–1793.
Chen, N.H., Reith, M.E., Quick, M.W., 2004. Synaptic uptake and beyond: thesodium- and chloride-dependent neurotransmitter transporter family SLC6.Pflugers Arch 447, 519–531.
Chiu, C.S., Brickley, S., Jensen, K., Southwell, A., Mckinney, S., Cull-Candy, S., Mody, I.,Lester, H.A., 2005. GABA transporter deficiency causes tremor, ataxia,nervousness, and increased GABA-induced tonic conductance in cerebellum. JNeurosci 25, 3234–3245.
Chowdhury, G.M., Gupta, M., Gibson, K.M., Patel, A.B., Behar, K.L., 2007. Alteredcerebral glucose and acetate metabolism in succinic semialdehydedehydrogenase-deficient mice. evidence for glial dysfunction and reducedglutamate/glutamine cycling. J Neurochem 103, 2077–2091.
Chung, S.H., Johnson, M.S., 1984. Studies on sound-induced epilepsy in mice. Proc RSoc Lond B Biol Sci 221, 145–168.
Clausen, R.P., Moltzen, E.K., Perregaard, J., Lenz, S.M., Sanchez, C., Falch, E., Frølund,B., Bolvig, T., Sarup, A., Larsson, O.M., Schousboe, A., Krogsgaard-Larsen, P., 2005.Selective inhibitors of GABA uptake: synthesis and molecular pharmacology of4-N-methylamino-4,5,6,7-tetrahydrobenzo[d]isoxazol-3-ol analogues. BioorgMed Chem 13, 895–908.
Conti, F., Melone, M., De Biasi, S., Minelli, A., Brecha, N.C., Ducati, A., 1998. Neuronaland glial localization of GAT-1, a high-affinity gamma-aminobutyric acidplasma membrane transporter, in human cerebral cortex: with a note on itsdistribution in monkey cortex. J Comp Neurol 396, 51–63.
Conti, F., Minelli, A., 1994. Glutamate immunoreactivity in rat cerebral cortex isreversibly abolished by 6-diazo-5-oxo-L-norleucine (DON), an inhibitor ofphosphate-activated glutaminase. J Histochem Cytochem 42, 717–726.
Conti, F., Zuccarello, L.V., Barbaresi, P., Minelli, A., Brecha, N.C., Melone, M., 1999.Neuronal, glial, and epithelial localization of gamma-aminobutyric acidtransporter 2, a high-affinity gamma-aminobutyric acid plasma membranetransporter, in the cerebral cortex and neighboring structures. J Comp Neurol409, 482–494.
Cooper, A.J., McDonald, J.M., Gelbard, A.S., Gledhill, R.F., Duffy, T.E., 1979. Themetabolic fate of 13N-labeled ammonia in rat brain. J Biol Chem 254, 4982–4992.
Cortez, M.A., Wu, Y., Gibson, K.M., Snead III, O.C., 2004. Absence seizures in succinicsemialdehyde dehydrogenase deficient mice. a model of juvenile absenceepilepsy. Pharmacol Biochem Behav 79, 547–553.
Cotman, C.W., Foster, A., Lanthorn, T., 1981. An overview of glutamate as aneurotransmitter. Adv Biochem Psychopharmacol 27, 1–27.
Couee, I., Tipton, K.F., 1990. The inhibition of glutamate dehydrogenase by someantipsychotic drugs. Biochem Pharmacol 39, 827–832.
Cremers, T., Ebert, B., 2007. Plasma and CNS concentrations of Gaboxadol in ratsfollowing subcutaneous administration. Eur J Pharmacol 562, 47–52.
Dadsetan, S., Bak, L.K., Sorensen, M., Keiding, S., Vilstrup, H., Ott, P., Leke, R.,Schousboe, A., Waagepetersen, H.S., 2011. Inhibition of glutamine synthesisinduces glutamate dehydrogenase-dependent ammonia fixation into alanine inco-cultures of astrocytes and neurons. Neurochem Int 59, 482–488.
Danbolt, N.C., 2001. Glutamate uptake. Prog Neurobiol 65, 1–105.Danbolt, N.C., Pines, G., Kanner, B.I., 1990. Purification and reconstitution of the
sodium- and potassium-coupled glutamate transport glycoprotein from ratbrain. Biochemistry 29, 6734–6740.
Deak, F., Schoch, S., Liu, X., Sudhof, T.C., Kavalali, E.T., 2004. Synaptobrevin isessential for fast synaptic-vesicle endocytosis. Nat Cell Biol 6, 1102–1108.

556 N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558
Drejer, J., Larsson, O.M., Schousboe, A., 1982. Characterization of L-glutamate uptakeinto and release from astrocytes and neurons cultured from different brainregions. Exp Brain Res 47, 259–269.
Drejer, J., Larsson, O.M., Schousboe, A., 1983. Characterization of uptake and releaseprocesses for D- and L-aspartate in primary cultures of astrocytes and cerebellargranule cells. Neurochem Res 8, 231–243.
Durkin, M.M., Smith, K.E., Borden, L.A., Weinshank, R.L., Branchek, T.A., Gustafson,E.L., 1995. Localization of messenger RNAs encoding three GABA transporters inrat brain: an in situ hybridization study. Brain Res Mol Brain Res 33, 7–21.
Ebert, U., Krnjevic, K., 1990. Systemic CI-966, a new gamma-aminobutyric aciduptake blocker, enhances gamma-aminobutyric acid action in CA1 pyramidallayer in situ. Can J Physiol Pharmacol 68, 1194–1199.
Evans, J.E., Frostholm, A., Rotter, A., 1996. Embryonic and postnatal expression offour gamma-aminobutyric acid transporter mRNAs in the mouse brain andleptomeninges. J Comp Neurol 376, 431–446.
Fairman, W.A., Vandenberg, R.J., Arriza, J.L., Kavanaugh, M.P., Amara, S.G., 1995. Anexcitatory amino-acid transporter with properties of a ligand-gated chloridechannel. Nature 375, 599–603.
Fremeau Jr., R.T., Kam, K., Qureshi, T., Johnson, J., Copenhagen, D.R., Storm-Mathisen,J., Chaudhry, F.A., Nicoll, R.A., Edwards, R.H., 2004. Vesicular glutamatetransporters 1 and 2 target to functionally distinct synaptic release sites.Science 304, 1815–1819.
Fujiwara, T., Mishima, T., Kofuji, T., Chiba, T., Tanaka, K., Yamamoto, A., Akagawa, K.,2006. Analysis of knock-out mice to determine the role of HPC-1/syntaxin 1A inexpressing synaptic plasticity. J Neurosci 26, 5767–5776.
Gegelashvili, G., Schousboe, A., 1997. High affinity glutamate transporters:regulation of expression and activity. Mol Pharmacol 52, 6–15.
Geppert, M., Goda, Y., Hammer, R.E., Li, C., Rosahl, T.W., Stevens, C.F., Sudhof, T.C.,1994. Synaptotagmin I: a major Ca2+ sensor for transmitter release at a centralsynapse. Cell 79, 717–727.
Gerber SH, Rah JC, Min SW, Liu X, de WH, Dulubova I, Meyer AC, Rizo J, Arancillo M,Hammer RE, Verhage M, Rosenmund C and Sudhof TC (2008) Conformationalswitch of syntaxin-1 controls synaptic vesicle fusion. Science321:1507-1510.
Gershoff, S.N., Elvehjem, C.A., 1951. The relative effect of methionine sulfoximine ondifferent animal species. J Nutr 45, 451–458.
Gitler, D., Takagishi, Y., Feng, J., Ren, Y., Rodriguiz, R.M., Wetsel, W.C., Greengard, P.,Augustine, G.J., 2004. Different presynaptic roles of synapsins at excitatory andinhibitory synapses. J Neurosci 24, 11368–11380.
Gram, L., 1990. Vigabatrin. In: Dam, M., Gram, L. (Eds.), ComprehensiveEpileptology. Raven Press, New York, pp. 631–640.
Gram, L., Larsson, O.M., Johnsen, A.H., Schousboe, A., 1988. Effects of valproate,vigabatrin and aminooxyacetic acid on release of endogenous and exogenousGABA from cultured neurons. Epilepsy Res 2, 87–95.
Grunewald, M., Kanner, B.I., 2000. The accessibility of a novel reentrant loop of theglutamate transporter GLT-1 is restricted by its substrate. J Biol Chem 275,9684–9689.
Guo, H., Lai, L., Butchbach, M.E., Stockinger, M.P., Shan, X., Bishop, G.A., Lin, C.L.,2003. Increased expression of the glial glutamate transporter EAAT2 modulatesexcitotoxicity and delays the onset but not the outcome of ALS in mice. HumMol Genet 12, 2519–2532.
Gupta M, Hogema BM, Grompe M, Bottiglieri TG, Concas A, Biggio G, Sogliano C,Rigamonti AE, Pearl PL, Snead OC, III, Jakobs C and Gibson KM (2003) Murinesuccinate semialdehyde dehydrogenase deficiency. Ann Neurol54 Suppl 6:S81–S90.
Gupta, M., Polinsky, M., Senephansiri, H., Snead, O.C., Jansen, E.E., Jakobs, C., Gibson,K.M., 2004. Seizure evolution and amino acid imbalances in murine succinatesemialdehyde dehydrogenase (SSADH) deficiency. Neurobiol Dis 16, 556–562.
Hassel, B., Dingledine, R., 2006. Glutamate. In: Siegel, G.J., Arganoff, B.W., Albers,R.W., Fisher, S.K., Uhler, M.D. (Eds.), Basic Neurochemistry: Molecular, Cellular,and Medical Aspects. Academic Press, New York, pp. 267–290.
Haugeto, O., Ullensvang, K., Levy, L.M., Chaudhry, F.A., Honore, T., Nielsen, M., Lehre,K.P., Danbolt, N.C., 1996. Brain glutamate transporter proteins formhomomultimers. J Biol Chem 271, 27715–27722.
Hawasli, A.H., Koovakkattu, D., Hayashi, K., Anderson, A.E., Powell, C.M., Sinton,C.M., Bibb, J.A., Cooper, D.C., 2009. Regulation of hippocampal and behavioralexcitability by cyclin-dependent kinase 5. PLoS One 4, e5808.
Hogema, B.M., Gupta, M., Senephansiri, H., Burlingame, T.G., Taylor, M., Jakobs, C.,Schutgens, R.B., Froestl, W., Snead, O.C., Diaz-Arrastia, R., Bottiglieri, T., Grompe,M., Gibson, K.M., 2001. Pharmacologic rescue of lethal seizures in mice deficientin succinate semialdehyde dehydrogenase. Nat Genet 29, 212–216.
Hogstad, S., Svenneby, G., Torgner, I.A., Kvamme, E., Hertz, L., Schousboe, A., 1988.Glutaminase in neurons and astrocytes cultured from mouse brain: kineticproperties and effects of phosphate, glutamate, and ammonia. Neurochem Res13, 383–388.
Howland, D.S., Liu, J., She, Y., Goad, B., Maragakis, N.J., Kim, B., Erickson, J., Kulik, J.,DeVito, L., Psaltis, G., DeGennaro, L.J., Cleveland, D.W., Rothstein, J.D., 2002.Focal loss of the glutamate transporter EAAT2 in a transgenic rat model of SOD1mutant-mediated amyotrophic lateral sclerosis (ALS). Proc Natl Acad Sci U S A99, 1604–1609.
Huang, Y.H., Dykes-Hoberg, M., Tanaka, K., Rothstein, J.D., Bergles, D.E., 2004a.Climbing fiber activation of EAAT4 transporters and kainate receptors incerebellar Purkinje cells. J Neurosci 24, 103–111.
Huang, Y.H., Sinha, S.R., Tanaka, K., Rothstein, J.D., Bergles, D.E., 2004b. Astrocyteglutamate transporters regulate metabotropic glutamate receptor-mediatedexcitation of hippocampal interneurons. J Neurosci 24, 4551–4559.
Iversen, L.L., Kelly, J.S., 1975. Uptake and metabolism of gamma-aminobutyric acidby neurones and glial cells. Biochem Pharmacol 24, 933–938.
Iversen, L.L., Neal, M.J., 1968. The uptake of [3H]GABA by slices of rat cerebralcortex. J Neurochem 15, 1141–1149.
Janz, R., Goda, Y., Geppert, M., Missler, M., Sudhof, T.C., 1999. SV2A and SV2Bfunction as redundant Ca2+ regulators in neurotransmitter release. Neuron 24,1003–1016.
Jensen, K., Chiu, C.S., Sokolova, I., Lester, H.A., Mody, I., 2003. GABA transporter-1(GAT1)-deficient mice. differential tonic activation of GABAA versus GABABreceptors in the hippocampus. J Neurophysiol 90, 2690–2701.
Kanai, Y., Hediger, M.A., 1992. Primary structure and functional characterization of ahigh-affinity glutamate transporter. Nature 360, 467–471.
Kanner, B.I., 1994. Sodium-coupled neurotransmitter transport: structure, functionand regulation. J Exp Biol 196, 237–249.
Kanner, B.I., Sharon, I., 1978. Active transport of L-glutamate by membrane vesiclesisolated from rat brain. Biochemistry 17, 3949–3953.
Kash, S.F., Johnson, R.S., Tecott, L.H., Noebels, J.L., Mayfield, R.D., Hanahan, D.,Baekkeskov, S., 1997. Epilepsy in mice deficient in the 65-kDa isoform ofglutamic acid decarboxylase. Proc Natl Acad Sci U S A 94, 14060–14065.
Kaupmann, K., Cryan, J.F., Wellendorph, P., Mombereau, C., Sansig, G., Klebs, K.,Schmutz, M., Froestl, W., van der Putten, H., Mosbacher, J., Brauner-Osborne, H.,Waldmeier, P., Bettler, B., 2003. Specific gamma-hydroxybutyrate-binding sitesbut loss of pharmacological effects of gamma-hydroxybutyrate in GABA(B)(1)-deficient mice. Eur J Neurosci 18, 2722–2730.
Kish, P.E., Fischer-Bovenkerk, C., Ueda, T., 1989. Active transport of gamma-aminobutyric acid and glycine into synaptic vesicles. Proc Natl Acad Sci U S A86, 3877–3881.
Klockner, U., Storck, T., Conradt, M., Stoffel, W., 1993. Electrogenic L-glutamateuptake in Xenopus laevis oocytes expressing a cloned rat brain L-glutamate/L-aspartate transporter (GLAST-1). J Biol Chem 268, 14594–14596.
Kvamme, E., Svenneby, G., Hertz, L., Schousboe, A., 1982. Properties of phosphateactivated glutaminase in astrocytes cultured from mouse brain. Neurochem Res7, 761–770.
Kvamme, E., Svenneby, G., Torgner, I.A., 1988. Glutaminases. In: Kvamme, E. (Ed.),Glutamine and Glutamate in Mammels. CRC Press, Boca Raton, pp. 53–67.
Kvamme, E., Torgner, I.A., Roberg, B., 2001. Kinetics and localization of brainphosphate activated glutaminase. J Neurosci Res 66, 951–958.
Kvist, T., Christiansen, B., Jensen, A.A., Brauner-Osborne, H., 2009. The four humangamma-aminobutyric acid (GABA) transporters: pharmacologicalcharacterization and validation of a highly efficient screening assay. CombChem High Throughput Screen 12, 241–249.
Laake, J.H., Takumi, Y., Eidet, J., Torgner, I.A., Roberg, B., Kvamme, E., Ottersen, O.P.,1999. Postembedding immunogold labelling reveals subcellular localizationand pathway-specific enrichment of phosphate activated glutaminase in ratcerebellum. Neuroscience 88, 1137–1151.
Lamar Jr., C., 1970. Mercaptopropionic acid: a convulsant that inhibits glutamatedecarboxylase. J Neurochem 17, 165–170.
Lehre, A.C., Rowley, N.M., Zhou, Y., Holmseth, S., Guo, C., Holen, T., Hua, R., Laake, P.,Olofsson, A.M., Poblete-Naredo, I., Rusakov, D.A., Madsen, K.K., Clausen, R.P.,Schousboe, A., White, H.S., Danbolt, N.C., 2011. Deletion of the betaine-GABAtransporter (BGT1; slc6a12) gene does not affect seizure thresholds of adultmice. Epilepsy Res. 95, 70–81.
Levy, L.M., Warr, O., Attwell, D., 1998. Stoichiometry of the glial glutamatetransporter GLT-1 expressed inducibly in a Chinese hamster ovary cell lineselected for low endogenous Na+-dependent glutamate uptake. J Neurosci 18,9620–9628.
Li, L., Chin, L.S., Shupliakov, O., Brodin, L., Sihra, T.S., Hvalby, O., Jensen, V., Zheng, D.,McNamara, J.O., Greengard, P., 1995. Impairment of synaptic vesicle clusteringand of synaptic transmission, and increased seizure propensity, in synapsin I-deficient mice. Proc Natl Acad Sci U S A 92, 9235–9239.
Li, Y., Sattler, R., Yang, E.J., Nunes, A., Ayukawa, Y., Akhtar, S., Ji, G., Zhang, P.W.,Rothstein, J.D., 2011. Harmine, a natural beta-carboline alkaloid, upregulatesastroglial glutamate transporter expression. Neuropharmacology 60, 1168–1175.
Lippert, B., Metcalf, B.W., Jung, M.J., Casara, P., 1977. 4-amino-hex-5-enoic acid, aselective catalytic inhibitor of 4-aminobutyric-acid aminotransferase inmammalian brain. Eur J Biochem 74, 441–445.
Liu, Q.R., Lopez-Corcuera, B., Mandiyan, S., Nelson, H., Nelson, N., 1993. Molecularcharacterization of four pharmacologically distinct gamma-aminobutyric acidtransporters in mouse brain [corrected]. J Biol Chem 268, 2106–2112.
Liu, Q.R., Mandiyan, S., Nelson, H., Nelson, N., 1992. A family of genes encodingneurotransmitter transporters. Proc Natl Acad Sci U S A 89, 6639–6643.
Loewe, S., 1953. The problem of synergism and antagonism of combined drugs.Arzneimittelforschung 3, 285–290.
Lynch, B.A., Lambeng, N., Nocka, K., Kensel-Hammes, P., Bajjalieh, S.M., Matagne, A.,Fuks, B., 2004. The synaptic vesicle protein SV2A is the binding site for theantiepileptic drug levetiracetam. Proc Natl Acad Sci U S A 101, 9861–9866.
Ma, Y., Hu, J.H., Zhao, W.J., Fei, J., Yu, Y., Zhou, X.G., Mei, Z.T., Guo, L.H., 2001a.Overexpression of gamma-aminobutyric acid transporter subtype I leads tosusceptibility to kainic acid-induced seizure in transgenic mice. Cell Res 11, 61–67.
Ma, Y.H., Zhou, X.G., Duan, S.H., Hu, J.H., Lu, B.F., Yu, Y., Mei, Z.T., Fei, J., Guo, L.H.,2001b. Overexpression of gamma-aminobutyric acid transporter subtype I leadsto cognitive deterioration in transgenic mice. Acta Pharmacol Sin 22, 340–348.
Madsen, K., White, H.S., Clausen, R.P., Frolund, B., Larsson, O.M., Krogsgaard-Larsen,P., Schousboe, A., 2007. Functional and Pharmacological aspects of GABA

N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558 557
transporters. In: Lajtha, A. (Ed.), Handbook of Neurochemistry and Molecularneurobiology. Springer-Verlag, Berlin Heidelberg, pp. 285–304.
Madsen KK, Clausen RP, Larsson OM, Krogsgaard-Larsen P, Schousboe A and WhiteHS (2009) Synaptic and extrasynaptic GABA transporters as targets for anti-epileptic drugs. J Neurochem109 Suppl 1:139–144.
Madsen KK, Ebert B, Clausen RP, Krogsgaard-Larsen P, Schousboe A and White HS(2011) The selective GAT inhibitors tiagabine and N-[4,4-bis(3-methyl-2-thienyl)-3-butenyl]-3-hydroxy-4-(methylamino)-4,5,6, 7-tetrahydrobenzo[d]isoxazol-3-ol (EF1502) exhibit mechanistic differences intheir ability to modulate the ataxia and anticonvulsant action of theextrasynaptic GABAA receptor agonist gaboxadol. J Pharmacol Exp Ther.
Mao, J., 2005. Glutamate transporter: an unexpected target for some antibiotics.Mol Pain 1, 5.
Masson, J., Darmon, M., Conjard, A., Chuhma, N., Ropert, N., Thoby-Brisson, M.,Foutz, A.S., Parrot, S., Miller, G.M., Jorisch, R., Polan, J., Hamon, M., Hen, R.,Rayport, S., 2006. Mice lacking brain/kidney phosphate-activated glutaminasehave impaired glutamatergic synaptic transmission, altered breathing,disorganized goal-directed behavior and die shortly after birth. J Neurosci 26,4660–4671.
McKenna, M.C., Gruetter, R., Sonnewald, U., Waagepetersen, H.S., Schousboe, A.,2006. Energy Metabolism of the Brain. In: Siegel, G.J., Arganoff, B.W., Albers,R.W., Fisher, S.K., Uhler, M.D. (Eds.), Basic Neurochemistry: Molecular, Cellular,and Medical Aspects. Academic Press, New York, pp. 531–557.
Miller, J.W., Kleven, D.T., Domin, B.A., Fremeau Jr., R.T., 2002. Cloned Sodium- (andChloride-) Dependent High-affinity Transporters for GABA, Glycine, Proline,Betaine, Taurine, and Creatine. In: Reith, M.E.A. (Ed.), NeurotransmitterTransporters: Structure, Function, and Regulation. Humana Press, Totowa,New Jersey, pp. 101–150.
Minelli, A., DeBiasi, S., Brecha, N.C., Zuccarello, L.V., Conti, F., 1996. GAT-3, a high-affinity GABA plasma membrane transporter, is localized to astrocyticprocesses, and it is not confined to the vicinity of GABAergic synapses in thecerebral cortex. J Neurosci 16, 6255–6264.
Moechars, D., Weston, M.C., Leo, S., Callaerts-Vegh, Z., Goris, I., Daneels, G., Buist, A.,Cik, M., van der Spek, P., Kass, S., Meert, T., D’Hooge, R., Rosenmund, C.,Hampson, R.M., 2006. Vesicular glutamate transporter VGLUT2 expressionlevels control quantal size and neuropathic pain. J Neurosci 26, 12055–12066.
Nagatomo K, Ueda Y, Doi T, Takaki M and Tsuru N (2007) Functional role of GABAtransporters for kindling development in GLAST KO mice. Neurosci Res57:319-321.
Nicholls, D.G., 1989. Release of glutamate, aspartate, and gamma-aminobutyric acidfrom isolated nerve terminals. J Neurochem 52, 331–341.
Nielsen, E.B., Suzdak, P.D., Andersen, K.E., Knutsen, L.J., Sonnewald, U., Braestrup, C.,1991. Characterization of tiagabine (NO-328), a new potent and selective GABAuptake inhibitor. Eur J Pharmacol 196, 257–266.
Nikkuni, O., Takayasu, Y., Iino, M., Tanaka, K., Ozawa, S., 2007. Facilitated activationof metabotropic glutamate receptors in cerebellar Purkinje cells in glutamatetransporter EAAT4-deficient mice. Neurosci Res 59, 296–303.
Norenberg, M.D., Martinez-Hernandez, A., 1979. Fine structural localization ofglutamine synthetase in astrocytes of rat brain. Brain Res 161, 303–310.
Olsen, R.W., Betz, H., 2006. GABA and Glycine. In: Siegel, G.J., Arganoff, B.W., Albers,R.W., Fisher, S.K., Uhler, M.D. (Eds.), Basic Neurochemistry: Molecular, Cellular,and Medical Aspects. Academic Press, New York, pp. 291–301.
Oz, G., Berkich, D.A., Henry, P.G., Xu, Y., LaNoue, K., Hutson, S.M., Gruetter, R., 2004.Neuroglial metabolism in the awake rat brain: CO2 fixation increases with brainactivity. J Neurosci 24, 11273–11279.
Ozkan, E.D., Ueda, T., 1998. Glutamate transport and storage in synaptic vesicles.Jpn J Pharmacol 77, 1–10.
Pawlak J, Brito V, Kuppers E and Beyer C (2005) Regulation of glutamate transporterGLAST and GLT-1 expression in astrocytes by estrogen. Brain Res Mol Brain Res2005 Jul 29;138 (1):1–7138:1–7.
Peghini, P., Janzen, J., Stoffel, W., 1997. Glutamate transporter EAAC-1-deficientmice develop dicarboxylic aminoaciduria and behavioral abnormalities but noneurodegeneration. EMBO J 16, 3822–3832.
Pines, G., Danbolt, N.C., Bjoras, M., Zhang, Y., Bendahan, A., Eide, L., Koepsell, H.,Storm-Mathisen, J., Seeberg, E., Kanner, B.I., 1992. Cloning and expression of arat brain L-glutamate transporter. Nature 360, 464–467.
Plaitakis, A., Latsoudis, H., Spanaki, C., 2011. The human GLUD2 glutamatedehydrogenase and its regulation in health and disease. Neurochem Int 59,495–509.
Plaitakis, A., Zaganas, I., 2001. Regulation of human glutamate dehydrogenases:implications for glutamate, ammonia and energy metabolism in brain. JNeurosci Res 66, 899–908.
Radian, R., Bendahan, A., Kanner, B.I., 1986. Purification and identification of thefunctional sodium- and chloride-coupled gamma-aminobutyric acid transportglycoprotein from rat brain. J Biol Chem 261, 15437–15441.
Radian, R., Ottersen, O.P., Storm-Mathisen, J., Castel, M., Kanner, B.I., 1990.Immunocytochemical localization of the GABA transporter in rat brain. JNeurosci 10, 1319–1330.
Radulovic, L., Woolf, T., Bjorge, S., Taylor, C., Reily, M., Bockbrader, H., Chang, T.,1993. Identification of a pyridinium metabolite in human urine following asingle oral dose of 1-[2-[bis[4-(trifluoromethyl)phenyl]methoxy]ethyl]- 1,2,5,6-tetrahydro-3-pyridinecarboxylic acid monohydrochloride, a gamma-aminobutyric acid uptake inhibitor. Chem Res Toxicol 6, 341–344.
Rawls, S.M., Karaca, F., Madhani, I., Bhojani, V., Martinez, R.L., Abou-Gharbia, M.,Raffa, R.B., 2010. Beta-lactamase inhibitors display anti-seizure properties in aninvertebrate assay. Neuroscience 169, 1800–1804.
Rizo, J., Rosenmund, C., 2008. Synaptic vesicle fusion. Nat Struct Mol Biol 15, 665–674.
Roberts, E., Frankel, S., 1950. Gamma-Aminobutyric acid in brain: its formation fromglutamic acid. J Biol Chem 187, 55–63.
Robinson MB and Dowd LA (1997) Heterogeneity and functional properties ofsubtypes of sodium-dependent glutamate transporters in the mammaliancentral nervous system. adv Pharmacol37:69–115.
Romera, C., Hurtado, O., Botella, S.H., Lizasoain, I., Cardenas, A., Fernandez-Tome, P.,Leza, J.C., Lorenzo, P., Moro, M.A., 2004. In vitro ischemic tolerance involvesupregulation of glutamate transport partly mediated by the TACE/ADAM17-tumor necrosis factor-alpha pathway. J Neurosci 24, 1350–1357.
Romera, C., Hurtado, O., Mallolas, J., Pereira, M.P., Morales, J.R., Romera, A., Serena, J.,Vivancos, J., Nombela, F., Lorenzo, P., Lizasoain, I., Moro, M.A., 2007. Ischemicpreconditioning reveals that GLT1/EAAT2 glutamate transporter is a novelPPARgamma target gene involved in neuroprotection. J Cereb Blood Flow Metab27, 1327–1338.
Rosahl, T.W., Spillane, D., Missler, M., Herz, J., Selig, D.K., Wolff, J.R., Hammer, R.E.,Malenka, R.C., Sudhof, T.C., 1995. Essential functions of synapsins I and II insynaptic vesicle regulation. Nature 375, 488–493.
Rothman, S.M., Olney, J.W., 1986. Glutamate and the pathophysiology of hypoxic–ischemic brain damage. Ann Neurol 19, 105–111.
Rothstein, J.D., Dykes-Hoberg, M., Pardo, C.A., Bristol, L.A., Jin, L., Kuncl, R.W., Kanai,Y., Hediger, M.A., Wang, Y., Schielke, J.P., Welty, D.F., 1996. Knockout ofglutamate transporters reveals a major role for astroglial transport inexcitotoxicity and clearance of glutamate. Neuron 16, 675–686.
Rothstein, J.D., Patel, S., Regan, M.R., Haenggeli, C., Huang, Y.H., Bergles, D.E., Jin, L.,Dykes, H.M., Vidensky, S., Chung, D.S., Toan, S.V., Bruijn, L.I., Su, Z.Z., Gupta, P.,Fisher, P.B., 2005. Beta-lactam antibiotics offer neuroprotection by increasingglutamate transporter expression. Nature 433, 73–77.
Rowe, W.B., Ronzio, R.A., Meister, A., 1969. Inhibition of glutamine synthetase bymethionine sulfoximine. Studies on methionine sulfoximine phosphate.Biochemistry 8, 2674–2680.
Rowley, N.M., Smith, M.D., Lamb, J.G., Schousboe, A., White, H.S., 2011. Hippocampalbetaine/GABA transporter mRNA expression is not regulated by inflammationor dehydration post-status epilepticus. J Neurochem 117, 82–90.
Sari, Y., Smith, K.D., Ali, P.K., Rebec, G.V., 2009. Upregulation of GLT1 attenuates cue-induced reinstatement of cocaine-seeking behavior in rats. J Neurosci 29, 9239–9243.
Sarup, A., Larsson, O.M., Schousboe, A., 2003. GABA transporters and GABA-transaminase as drug targets. Curr Drug Targets CNS Neurol Disord 2, 269–277.
Schallier, A., Massie, A., Loyens, E., Moechars, D., Drinkenburg, W., Michotte, Y.,Smolders, I., 2009. VGLUT2 heterozygous mice show more susceptibility toclonic seizures induced by pentylenetetrazol. Neurochem Int 55, 41–44.
Schechter, P.J., Tranier, Y., Jung, M.J., Bohlen, P., 1977a. Audiogenic seizureprotection by elevated brain GABA concentration in mice. effects of gamma-acetylenic gaba and gamma-vinyl GABA, two irreversible GABA-T inhibitors.Eur J Pharmacol 45, 319–328.
Schechter, P.J., Tranier, Y., Jung, M.J., Sjoerdsma, A., 1977b. Antiseizure activity ofgamma-acetylenic gamma-aminobutyric acid: a catalytic irreversible inhibitorof gamma-aminobutyric acid transaminase. J Pharmacol Exp Ther 201, 606–612.
Schoch, S., Deak, F., Konigstorfer, A., Mozhayeva, M., Sara, Y., Sudhof, T.C., Kavalali,E.T., 2001. SNARE function analyzed in synaptobrevin/VAMP knockout mice.Science 294, 1117–1122.
Schousboe, A., 2000. Pharmacological and functional characterization of astrocyticGABA transport: a short review. Neurochem Res 25, 1241–1244.
Schousboe, A., Larsson, O.M., Wood, J.D., Krogsgaard-Larsen, P., 1983. Transport andmetabolism of gamma-aminobutyric acid in neurons and glia: implications forepilepsy. Epilepsia 24, 531–538.
Schousboe, A., Svenneby, G., Hertz, L., 1977. Uptake and metabolism of glutamate inastrocytes cultured from dissociated mouse brain hemispheres. J Neurochem29, 999–1005.
Schousboe, A., Waagepetersen, H.S., 2007. GABA: homeostatic and pharmacologicalaspects. Prog Brain Res 160, 9–19.
Schousboe, A., Waagepetersen, H.S., 2008. GABA Neurotransmission: An overview.In: Lajtha, A. (Ed.), Handbook of Neurochemistry and Molecular Neurobiology.Springer, New York, pp. 213–226.
Schousboe, A., White, H.S., 2009. Glial Modulation of Excitability via Glutamatergicand GABA Transporters. In: Schwartzkroin, P.A. (Ed.), Encyclopedia of BasicEpilepsy Research. Academic Press, Oxford, pp. 397–401.
Schousboe, A., Wu, J.Y., Roberts, E., 1974. Subunit structure and kinetic properties of4-aminobutyrate-2-ketoglutarate transaminase purified from mouse brain. JNeurochem 23, 1189–1195.
Seal, R.P., Akil, O., Yi, E., Weber, C.M., Grant, L., Yoo, J., Clause, A., Kandler, K., Noebels,J.L., Glowatzki, E., Lustig, L.R., Edwards, R.H., 2008. Sensorineural deafnessand seizures in mice lacking vesicular glutamate transporter 3. Neuron 57,263–275.
Seal, R.P., Leighton, B.H., Amara, S.G., 2000. A model for the topology of excitatoryamino acid transporters determined by the extracellular accessibility ofsubstituted cysteines. Neuron 25, 695–706.
Sellinger, O.Z., Azcurra, J.M., Ohlsson, W.G., 1968. Methionine sulfoximine seizures.8. The dissociation of the convulsant and glutamine synthetase inhibitoryeffects. J Pharmacol Exp Ther 164, 212–222.
Sepkuty, J.P., Cohen, A.S., Eccles, C., Rafiq, A., Behar, K., Ganel, R., Coulter, D.A.,Rothstein, J.D., 2002. A neuronal glutamate transporter contributes toneurotransmitter GABA synthesis and epilepsy. J Neurosci 22, 6372–6379.

558 N.M. Rowley et al. / Neurochemistry International 61 (2012) 546–558
Shapiro, R.A., Clark, V.M., Curthoys, N.P., 1979. Inactivation of rat renal phosphate-dependent glutaminase with 6-diazo-5-oxo-L-norleucine. Evidence forinteraction at the glutamine binding site. J Biol Chem 254, 2835–2838.
Shemisa, O.A., Fahien, L.A., 1971. Modifications of glutamate dehydrogenase byvarious drugs which affect behavior. Mol Pharmacol 7, 8–25.
Shimada, F., Shiga, Y., Morikawa, M., Kawazura, H., Morikawa, O., Matsuoka, T.,Nishizaki, T., Saito, N., 1999. The neuroprotective agent MS-153 stimulatesglutamate uptake. Eur J Pharmacol 386, 263–270.
Shuang, R., Zhang, L., Fletcher, A., Groblewski, G.E., Pevsner, J., Stuenkel, E.L., 1998.Regulation of Munc-18/syntaxin 1A interaction by cyclin-dependent kinase 5 innerve endings. J Biol Chem 273, 4957–4966.
Sluse, F.E., 1996. Mitochondrial metabolite carrier family, topology, structure andfunctional properties: an overview. Acta Biochim Pol 43, 349–360.
Sonnewald, U., Westergaard, N., Schousboe, A., 1997. Glutamate transport andmetabolism in astrocytes. Glia 21, 56–63.
Sonnewald, U., Westergaard, N., Schousboe, A., Svendsen, J.S., Unsgard, G., Petersen,S.B., 1993. Direct demonstration by [13C]NMR spectroscopy that glutaminefrom astrocytes is a precursor for GABA synthesis in neurons. Neurochem Int 22,19–29.
Stoffel, W., Korner, R., Wachtmann, D., Keller, B.U., 2004. Functional analysis ofglutamate transporters in excitatory synaptic transmission of GLAST1 andGLAST1/EAAC1 deficient mice. Brain Res Mol Brain Res 128, 170–181.
Storck, T., Schulte, S., Hofmann, K., Stoffel, W., 1992. Structure, expression, andfunctional analysis of a Na(+)-dependent glutamate/aspartate transporter fromrat brain. Proc Natl Acad Sci U S A 89, 10955–10959.
Storustovu, S.I., Ebert, B., 2006. Pharmacological characterization of agonists atdelta-containing GABAA receptors: Functional selectivity for extrasynapticreceptors is dependent on the absence of gamma2. J Pharmacol Exp Ther 316,1351–1359.
Tafoya, L.C., Mameli, M., Miyashita, T., Guzowski, J.F., Valenzuela, C.F., Wilson, M.C.,2006. Expression and function of SNAP-25 as a universal SNARE component inGABAergic neurons. J Neurosci 26, 7826–7838.
Takanaga, H., Ohtsuki, S., Hosoya, K., Terasaki, T., 2001. GAT2/BGT-1 as a systemresponsible for the transport of gamma-aminobutyric acid at the mouse blood-brain barrier. J Cereb Blood Flow Metab 21, 1232–1239.
Takayasu, Y., Iino, M., Kakegawa, W., Maeno, H., Watase, K., Wada, K., Yanagihara, D.,Miyazaki, T., Komine, O., Watanabe, M., Tanaka, K., Ozawa, S., 2005. Differentialroles of glial and neuronal glutamate transporters in Purkinje cell synapses. JNeurosci 25, 8788–8793.
Tanaka, K., 1993. Expression cloning of a rat glutamate transporter. Neurosci Res 16,149–153.
Tanaka, K., Watase, K., Manabe, T., Yamada, K., Watanabe, M., Takahashi, K., Iwama,H., Nishikawa, T., Ichihara, N., Kikuchi, T., Okuyama, S., Kawashima, N., Hori, S.,Takimoto, M., Wada, K., 1997. Epilepsy and exacerbation of brain injury in micelacking the glutamate transporter GLT-1. Science 276, 1699–1702.
Tapia, R., 1975. Biochemical Pharmacology of GABA in CNS. In: Iversen, L.L., Iverson,S.D., Snyder, S.H. (Eds.), Handbook of Psychopharmacology. Plenum PublishingCorporation, New York, pp. 1–58.
Tapia, R., Pasantes, H., 1971. Relationships between pyridoxal phosphateavailability, activity of vitamin B 6 -dependent enzymes and convulsions.Brain Res 29, 111–122.
Tapia R, Pasantes H, Perez dlM, Ortega BG and Massieu GH (1967) Free amino acidsand glutamate decarboxylase activity in brain of mice during drug-inducedconvulsions. Biochem Pharmacol16:483-496.
Tews, J.K., Stone, W.E., 1964. Effectsof methioninesulfoximine on levels of freeamino acids and related substances in brain. Biochem Pharmacol 13, 543–545.
Tsuru N, Ueda Y and Doi T (2002) Amygdaloid kindling in glutamate transporter(GLAST) knockout mice. Epilepsia43:805-811.
van Gassen, K.L., van der Hel, W.S., Hakvoort, T.B., Lamers, W.H., de Graan, P.N.,2009. Haploinsufficiency of glutamine synthetase increases susceptibility toexperimental febrile seizures. Genes Brain Behav 8, 290–295.
Varoqueaux, F., Sigler, A., Rhee, J.S., Brose, N., Enk, C., Reim, K., Rosenmund, C., 2002.Total arrest of spontaneous and evoked synaptic transmission but normalsynaptogenesis in the absence of Munc13-mediated vesicle priming. Proc NatlAcad Sci U S A 99, 9037–9042.
Verhage, M., Maia, A.S., Plomp, J.J., Brussaard, A.B., Heeroma, J.H., Vermeer, H.,Toonen, R.F., Hammer, R.E., van den Berg, T.K., Missler, M., Geuze, H.J., Sudhof,T.C., 2000. Synaptic assembly of the brain in the absence of neurotransmittersecretion. Science 287, 864–869.
Waagepetersen, H.S., Sonnewald, U., Gegelashvili, G., Larsson, O.M., Schousboe, A.,2001. Metabolic distinction between vesicular and cytosolic GABA in culturedGABAergic neurons using 13C magnetic resonance spectroscopy. J Neurosci Res63, 347–355.
Waagepetersen, H.S., Sonnewald, U., Larsson, O.M., Schousboe, A., 2000. A possiblerole of alanine for ammonia transfer between astrocytes and glutamatergicneurons. J Neurochem 75, 471–479.
Wafford, K.A., Ebert, B., 2006. Gaboxadol–a new awakening in sleep. Curr OpinPharmacol 6, 30–36.
Walls, A.B., Eyjolfsson, E.M., Smeland, O.B., Nilsen, L.H., Schousboe, I., Schousboe, A.,Sonnewald, U., Waagepetersen, H.S., 2011. Knockout of GAD65 has majorimpact on synaptic GABA synthesized from astrocyte-derived glutamine. JCereb Blood Flow Metab 31, 494–503.
Walls, A.B., Nilsen, L.H., Eyjolfsson, E.M., Vestergaard, H.T., Hansen, S.L., Schousboe,A., Sonnewald, U., Waagepetersen, H.S., 2010. GAD65 is essential for synthesisof GABA destined for tonic inhibition regulating epileptiform activity. JNeurochem 115, 1398–1408.
Warr O, Takahashi M and Attwell D (1999) Modulation of extracellular glutamateconcentration in rat brain slices by cystine-glutamate exchange. J Physiol514(Pt 3):783–793.
Washbourne, P., Thompson, P.M., Carta, M., Costa, E.T., Mathews, J.R., Lopez-Bendito, G., Molnar, Z., Becher, M.W., Valenzuela, C.F., Partridge, L.D., Wilson,M.C., 2002. Genetic ablation of the t-SNARE SNAP-25 distinguishes mechanismsof neuroexocytosis. Nat Neurosci 5, 19–26.
Watanabe, T., Morimoto, K., Hirao, T., Suwaki, H., Watase, K., Tanaka, K., 1999.Amygdala-kindled and pentylenetetrazole-induced seizures in glutamatetransporter GLAST-deficient mice. Brain Res 845, 92–96.
Watase, K., Hashimoto, K., Kano, M., Yamada, K., Watanabe, M., Inoue, Y., Okuyama,S., Sakagawa, T., Ogawa, S., Kawashima, N., Hori, S., Takimoto, M., Wada, K.,Tanaka, K., 1998. Motor discoordination and increased susceptibility tocerebellar injury in GLAST mutant mice. Eur J Neurosci 10, 976–988.
Weil-Malherbe, H., 1972. Modulators of glutaminase activity. J Neurochem 19,2257–2267.
White, H.S., Sarup, A., Bolvig, T., Kristensen, A.S., Petersen, G., Nelson, N., Pickering,D.S., Larsson, O.M., Frølund, B., Krogsgaard-Larsen, P., Schousboe, A., 2002.Correlation between anticonvulsant activity and inhibitory action on glialgamma-aminobutyric acid uptake of the highly selective mouse gamma-aminobutyric acid transporter 1 inhibitor 3-hydroxy-4-amino-4,5,6,7-tetrahydro-1,2-benzisoxazole and its N-alkylated analogs. J Pharmacol ExpTher 302, 636–644.
White, H.S., Watson, W.P., Hansen, S.L., Slough, S., Perregaard, J., Sarup, A., Bolvig, T.,Petersen, G., Larsson, O.M., Clausen, R.P., Frølund, B., Falch, E., Krogsgaard-Larsen, P., Schousboe, A., 2005. First demonstration of a functional role forcentral nervous system betaine/{gamma}-aminobutyric acid transporter(mGAT2) based on synergistic anticonvulsant action among inhibitors ofmGAT1 and mGAT2. J Pharmacol Exp Ther 312, 866–874.
Wojcik, S.M., Katsurabayashi, S., Guillemin, I., Friauf, E., Rosenmund, C., Brose, N.,Rhee, J.S., 2006. A shared vesicular carrier allows synaptic corelease of GABAand glycine. Neuron 50, 575–587.
Wojcik, S.M., Rhee, J.S., Herzog, E., Sigler, A., Jahn, R., Takamori, S., Brose, N.,Rosenmund, C., 2004. An essential role for vesicular glutamate transporter 1(VGLUT1) in postnatal development and control of quantal size. Proc Natl AcadSci U S A 101, 7158–7163.
Wu, J.Y., Roberts, E., 1974. Properties of brain L-glutamate decarboxylase: inhibitionstudies. J Neurochem 23, 759–767.
Yamada, T., Kawahara, K., Kosugi, T., Tanaka, M., 2006. Nitric oxide produced duringsublethal ischemia is crucial for the preconditioning-induced down-regulationof glutamate transporter GLT-1 in neuron/astrocyte co-cultures. NeurochemRes 31, 49–56.
Yamashita, A., Singh, S.K., Kawate, T., Jin, Y., Gouaux, E., 2005. Crystal structure of abacterial homologue of Na+/Cl–dependent neurotransmitter transporters.Nature 437, 215–223.
Yernool, D., Boudker, O., Jin, Y., Gouaux, E., 2004. Structure of a glutamatetransporter homologue from Pyrococcus horikoshii. Nature 431, 811–818.
Yu, A.C., Drejer, J., Hertz, L., Schousboe, A., 1983. Pyruvate carboxylase activity inprimary cultures of astrocytes and neurons. J Neurochem 41, 1484–1487.
Yu, A.C., Schousboe, A., Hertz, L., 1982. Metabolic fate of 14C-labeled glutamate inastrocytes in primary cultures. J Neurochem 39, 954–960.
Yunger, L.M., Fowler, P.J., Zarevics, P., Setler, P.E., 1984. Novel inhibitors of gamma-aminobutyric acid (GABA) uptake: anticonvulsant actions in rats and mice. JPharmacol Exp Ther 228, 109–115.
Zaganas, I., Waagepetersen, H.S., Georgopoulos, P., Sonnewald, U., Plaitakis, A.,Schousboe, A., 2001. Differential expression of glutamate dehydrogenase incultured neurons and astrocytes from mouse cerebellum and cerebral cortex. JNeurosci Res 66, 909–913.
Zerangue, N., Kavanaugh, M.P., 1996. Flux coupling in a neuronal glutamatetransporter. Nature 383, 634–637.
Zhao, W.J., Ma, Y.H., Fei, J., Mei, Z.T., Guo, L.H., 2003. Increase in drug-inducedseizure susceptibility of transgenic mice overexpressing GABA transporter-1.Acta Pharmacol Sin 24, 991–995.
Zhu, X.M., Ong, W.Y., 2004. A light and electron microscopic study of betaine/GABAtransporter distribution in the monkey cerebral neocortex and hippocampus. JNeurocytol 33, 233–240.
Zschocke J, Bayatti N, Clement AM, Witan H, Figiel M, Engele J and Behl C (2005)Differential promotion of glutamate transporter expression and function byglucocorticoids in astrocytes from various brain regions. J Biol Chem 2005 Oct14;280 (41):34924–32 Epub 2005 Aug 3280:34924–34932.