Giltbrook Surgery NewApproachComprehensive Report ... · •...
Transcript of Giltbrook Surgery NewApproachComprehensive Report ... · •...

This report describes our judgement of the quality of care at this service. It is based on a combination of what we foundwhen we inspected, information from our ongoing monitoring of data about services and information given to us fromthe provider, patients, the public and other organisations.
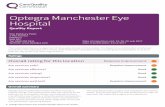
Ratings
Overall rating for this service Outstanding –
Are services safe? Good –––
Are services effective? Good –––
Are services caring? Outstanding –
Are services responsive to people’s needs? Outstanding –
Are services well-led? Good –––
GiltbrGiltbrookook SurSurggereryyQuality Report
492 Nottingham RoadGiltbrookNottinghamNG16 2GETel: 0115 938 3191Website: www.giltbrooksurgery.nhs.uk
Date of inspection visit: 28 January 2016Date of publication: 10/03/2016
1 Giltbrook Surgery Quality Report 10/03/2016

Contents
PageSummary of this inspectionOverall summary 2
The five questions we ask and what we found 4
The six population groups and what we found 9
What people who use the service say 14
Detailed findings from this inspectionOur inspection team 15
Background to Giltbrook Surgery 15
Why we carried out this inspection 15
How we carried out this inspection 15
Detailed findings 17
Overall summaryLetter from the Chief Inspector of GeneralPractice
We carried out an announced comprehensive inspectionat Giltbrook Surgery on 28 January 2016. The overallrating for this practice is outstanding.
Please note that when referring to informationthroughout this report, for example any reference to theQuality and Outcomes Framework (QOF) data, this relatesto the most recent information available to the CareQuality Commission (CQC) at that time.
Our key findings were as follows:
• There was an open and transparent approach to safetyand an effective system in place for reporting andrecording significant events, and we saw evidence thatlearning was applied from events.
• Staff assessed patients’ needs and delivered care inline with current evidence based guidance. Staff hadthe skills, knowledge and experience to delivereffective care and treatment.
• Feedback from patients about their care, and theirinteractions with all practice staff, was consistently and
strongly positive. Patients said they were treated withcompassion, dignity and respect and they wereinvolved in their care and decisions about theirtreatment.
• Patients said they found it easy to make anappointment with a GP. Routine appointments couldbe booked within a week, with urgent appointmentsbeing available the same day. Advanced bookingscould be made without restriction on timescales.
• The practice used clinical audits to review patientcare and we observed how outcomes had been usedto improve services as a result.
• The practice had good facilities and waswell-equipped to treat patients and meet their needs.The size of the building limited the number of servicesprovided on site, but the practice were activelyexploring opportunities for re-location in the futurewith service commissioners.
• The practice planned and co-ordinated patient carewith the wider multi-disciplinary team to plan anddeliver effective and responsive care to keepvulnerable patients safe. This approach had impactedon unplanned hospital admissions and attendance atAccident and Emergency.
Summary of findings
2 Giltbrook Surgery Quality Report 10/03/2016

• There was a strong and proactive leadership structurewithin the practice, and staff told us that they werewell-supported and felt valued by the partners.
• High standards were promoted and owned by anenthusiastic and motivated practice team withevidence of highly effective team working.
• The practice reviewed the way it delivered services asa consequence of feedback from patients and from thepatient participation group. For example, it hadreviewed its use of the patient name display facility inthe waiting area in response to concerns aboutconfidentiality.
We saw several areas of outstanding practice including:
• The practice had commenced a communitypharmacy pilot project from November 2015. Thisplaced a prescribing community pharmacist withinthe practice for two days each week. Although a fullevaluation was awaited, the project had alreadyreceived positive feedback from patients. More than100 patients had been seen in the first two monthsand initial outcomes demonstrated improvements incare. For example, a reduction in the number ofmedications prescribed with between 10-15%patients having at least of one of their prescribedmedications stopped.
• A ‘homely remedies for minor ailments’ system hadbeen developed by the practice in conjunction withthe pharmacist for use within a local care home. Thisenabled the care home to commence agreed drugs
for minor ailments such as indigestion andconstipation to ensure the patient receivedtreatment at the earliest possible opportunity. Thiswas used with the proviso that the GP was contactedif symptoms persisted beyond 48 hours.
• The practice undertook a comprehensive analysis ofthe Friends and Family Test (FFT) returns, and hadformulated action plans in response to suggestionsfrom patients to enhance patient satisfaction andexperience. For example, in response to late runningappointments, the practice were informing patientsto book longer appointments if they had more thanone issue to discuss, and were also auditing waitingtimes for each clinician.
• The practice had achieved highly in delivering NHShealth checks and had consistently overachievedagainst target figures. For example, current datashowed that the practice had achieved 124% of itstarget in the first three-quarters of 2015-16.
• We saw many examples in which the practice teamdelivered outstanding care for their patients to keepthem safe and well. For example, checkingvulnerable patients had access to heat and foodduring poor weather, and ensuring that patients witha mental health condition were collecting theirprescribed medicines.
Professor Steve Field (CBE FRCP FFPH FRCGP)Chief Inspector of General Practice
Summary of findings
3 Giltbrook Surgery Quality Report 10/03/2016

The five questions we ask and what we foundWe always ask the following five questions of services.
Are services safe?
• There was an open and effective system in place for reportingand recording significant events. Lessons were shared to makesure actions were taken to improve safety in the practice. Forexample, a back-up system had been implemented to ensurethat all patients received their scheduled INR test (this is a testused to assess blood clotting, primarily used for patients takingwarfarin). This followed an incident when a test was missed.
• When there were unintended or unexpected safety incidents,we saw evidence that people received support, an apology andwere told about any actions to improve processes to preventthe same thing happening again.
• The practice had clearly defined and embedded systems,processes and practices in place to keep people safe andsafeguarded from abuse.
• Risks to patients and the public were assessed andwell-managed including procedures for infection control andother site-related health and safety matters.
• Medicines, including vaccines and emergency drugs, werestored safely and appropriately with good systems to monitorand control stock levels.
• The practice had effective systems in place to deal with medicalemergencies.
• The practice ensured staffing levels were sufficient at all timesto respond effectively to patient need.
Good –––
Are services effective?
• Data showed patient outcomes were in line with local andnational averages. The practice had achieved an overall figureof 91.6% for the Quality and Outcomes Framework in 2014-15.This was 3.5% below the CCG and 1.9% below the nationalaverages. However, the most up to date figures provided by thepractice (but not yet verified and published) demonstrated thatthe performance had improved.
• Staff assessed needs and delivered care in line with currentevidence based guidance.
• Clinical audits demonstrated quality improvement.• Staff had the skills, knowledge and experience to deliver
effective care and treatment. There was a clear process tosupport the training and development of staff.
Good –––
Summary of findings
4 Giltbrook Surgery Quality Report 10/03/2016

• The skill mix of the practice team was kept under review tomeet the changing demands of GP practice.
• Annual appraisals and personal development plans were inplace for all staff.
• Staff worked with multidisciplinary teams to understand andmeet the range and complexity of people’s needs, in order todeliver care more effectively. Monthly meetings with widermembers of the healthcare team were held to review morecomplex and vulnerable patients.
• The practice had lower usage of Accident & Emergency (A&E) asa result of good GP access.
Are services caring?
• Data showed that patients rated the practice above CCG andnational averages in respect of care provided. For example, 90%of patients said the last GP they saw was good at involvingthem in decisions about their care compared to the CCGaverage of 80% and national average of 82%, according to theGP Patient survey.
• Patients we spoke with during the inspection and feedback onour comments cards strongly indicated they were treated withcompassion, dignity and respect and felt involved in decisionsabout their care and treatment.
• Information for patients about the services available was easyto understand and accessible.
• Throughout our inspection, we observed that staff treatedpatients with kindness and respect, and maintainedconfidentiality.
• We were informed that the GP partner would sometimes seepatients at the weekend with specific needs, for example,patients receiving palliative care. This ensured continuity ofcare for the patient and their family.
• The practice telephoned patients due to be discharged fromhospital to help plan their needs. Vulnerable patients werefollowed up by the practice if they failed to respond to calls orattend for appointments, and patients were contacted inextreme weather conditions to ensure they were safe.
• The practice monitored patient with mental health problems toensure they received their prescribed medications, andproactively contacted patients to discuss their care if they hadnot collected their medicines.
• The practice had a nominated carer’s champion who hadestablished links with the Carers Federation to gain up to dateinformation on available support services.
Outstanding –
Summary of findings
5 Giltbrook Surgery Quality Report 10/03/2016

• Views of external stakeholders were very positive in respect ofthe high level of care provided by the practice team and alignedwith our findings.
Are services responsive to people’s needs?
• The practice reviewed the needs of its local population andengaged with the NHS England Area Team and ClinicalCommissioning Group to secure improvements to serviceswhere these were identified. For example, the practice hadbeen approached by the CCG to pilot the impact of co-locatinga prescribing community pharmacist based within the practiceand they had agreed to be involved.
• The practice implemented suggestions for improvements andmade changes to the way it delivered services as aconsequence of feedback from patients and from the patientparticipation group. For example, the practice had renewed theupholstery and changed seating in the waiting area further tofeedback received via the PPG.
• People could access appointments and services in a way and ata time that suited them. Urgent appointments were availableon the day, and routine appointments could be booked in lessthan a week.
• Comment cards and patients we spoke to during the inspectionwere very positive about their experience in obtaining bothurgent and routine appointments. This was reinforced by thenational GP survey in January 2016 which found 91% patientsdescribed their experience of making an appointment as good.This was in comparison to a CCG average and national averageof 73%.
• The practice had implemented a system within a care home touse agreed drugs for minor ailments to ensure the patientreceived treatment at the earliest opportunity
• The practice had good facilities and was well equipped to treatpatients. The practice had a desire to provide more on siteservices and was exploring future opportunities for their sitewith their CCG and NHS England.
• Staff in two care homes told us the practice respondedpromptly to their clients’ needs, and worked with the carehome staff and family members to deliver the best care for theirpatients.
• Information about how to complain was available and easy tounderstand, and the practice responded quickly when issues
Outstanding –
Summary of findings
6 Giltbrook Surgery Quality Report 10/03/2016

were raised. Learning from complaints was shared with staff toimprove the quality of service, and we saw examples of thisincluding making sure that patients were proactively includedin agreeing decisions about their care.
Are services well-led?
• The practice had a clear vision and strategy to deliver highquality care and promote good outcomes for patients. Staffwere clear about the vision and their responsibilities in relationto this.
• There was strong and clear leadership structure and staff feltsupported by management.
• The practice engaged well with the CCG and other practiceswithin their locality.
• The CCG acknowledged the achievements of the practice. Theirconfidence in the practice was demonstrated by the CCGselecting the practice as a pilot site for the ongoing communitypharmacy project. The CCG had also nominated the practice foran award for their commitment the Family and Friends Test(FFT).
• The practice had a range of policies and procedures to governactivity, and standard operating procedures had been devisedfor all tasks to ensure these could be covered during absence ofkey individuals.
• The practice held regular meetings to discuss clinical issues,and wider staff meetings were arranged for other issues. Staffput forward the items for discussion at their meetings.
• There was an overarching governance framework whichsupported the delivery of the strategy and good quality care.This included arrangements to monitor and improve qualityand identify risk.
• The practice sought feedback from staff and patients, which itacted on. A recent staff survey had been completeddemonstrating a high level of satisfaction across the practiceteam.
• The Patient Participation Group (PPG) was active and influentialin informing practice developments. For example further toconcerns being raised about displaying patient names in thereception area, a system had been implemented to restrict thiswhere deemed appropriate. This had raised an important issuein respect of the need to protect confidentiality for particularpatients including children in foster care.
• There was a strong focus on continuous learning andimprovement at all levels.
Good –––
Summary of findings
7 Giltbrook Surgery Quality Report 10/03/2016

• All staff had received inductions and had received regularperformance reviews, and attended staff meetings.
• Effective succession planning ensured continuity of service andunderpinned practice development.
Summary of findings
8 Giltbrook Surgery Quality Report 10/03/2016

The six population groups and what we foundWe always inspect the quality of care for these six population groups.
Older people
• The practice offered proactive and personalised care to meetthe needs of older people. Care plans were in place for olderpatients with more complex needs. Monthly multi-disciplinarymeetings were held to review frail patients and those at risk ofhospital admission to plan and deliver care appropriate to theirneeds.
• It was responsive to the needs of older people, and offeredhome visits and urgent appointments for those who neededthem.
• The practice provided primary medical services to 14 residentsat a local care home for older people. We spoke with a managerof this home who was very satisfied with the care provided bythe GPs, and described the relationship with the practice asbeing extremely positive and responsive. They had quarterlymeetings with the partners and had liaised with the communitypharmacist based within the practice for advice and support.
• A ‘homely remedies for minor ailments’ system had beendeveloped for use within the care home. This enabled thehome to use agreed drugs for minor ailments such asindigestion and constipation to ensure the patient receivedtreatment at the earliest possible opportunity. If symptomspersisted for more than 48 hours, the GP would be contacted.
• Flu vaccination rates for the over 65s were 75.4% which wasslightly higher than the national figure of 73.2%.
• Nationally reported data showed that outcomes for patients forconditions commonly found in older people, includingrheumatoid arthritis and heart failure were in line with or abovelocal and national averages
• The practice prioritised older patients with no social supportduring adverse weather conditions and made sure they hadaccess to food and heat.
Outstanding –
People with long term conditions
• All clinical members of the practice team had lead roles inchronic disease management. For those patients with the mostcomplex needs and associated risk of hospital admission, thepractice team worked with health and care professionals todeliver a multidisciplinary package of care.
Good –––
Summary of findings
9 Giltbrook Surgery Quality Report 10/03/2016

• All patients with a long-term condition had a named GP andreceived a structured annual review to check their health andmedicines needs were being appropriately met.
• Whilst the practice had performed well in most QOF clinicalindicators, the achievement was below average for diabetes,chronic kidney disease and coronary heart disease. The overallachievement for diabetes indicators was 65% which was 22%below the CCG average and 24% below the national average.However, the practice were aware of this and had developedactions to address this. We saw practice data for the currentyear (which was not yet verified or published) but thisdemonstrated an improvement in QOF performance fordiabetes indicators.
• The practice nurse worked closely with the local Diabetes NurseSpecialist. Monthly joint clinics were organised between thetwo nurses, which included the initiation of insulin for patientswith diabetes.
• The practice had signed up to the ‘Year of Care’ programme forpatients with diabetes from April 2016. This scheme aids thepatient to self-manage their diabetes to a much greater extent,and facilitates a more constructive dialogue between thepatients and clinicians with regards to the ongoingmanagement of their condition.
• Ongoing liaison with the local respiratory nurse provided anexpert resource for patients with chronic obstructivepulmonary disease and asthma. Patients were referred into the‘Breathe Easy’ self-management programme, and forpulmonary rehabilitation when indicated. Self-managementbooklets produced by the CCG were available for thesepatients, and used to inform patients what to do if theirsymptoms worsened.
• QOF indicators for asthma were higher than CCG and nationalaverages. For example, 85.7% of patients with asthma receiveda review in the preceding 12 months, compared to the CCG andnational averages of 76.2% and 75.3% respectively.
• An ongoing pilot project in which a community pharmacist wasworking within the practice had allowed greater opportunitiesto review repeat medications for patients with more than onelong term condition, or review patients who were receivingmultiple medications.
Summary of findings
10 Giltbrook Surgery Quality Report 10/03/2016

Families, children and young people
• Urgent appointments were available every day toaccommodate children. The practice had a policy that allchildren under the age of five years old would be seen on thesame day.
• There were systems in place to identify and follow up childrenliving in disadvantaged circumstances and who were at risk, forexample, children who had a high number of A&E attendances.We were informed of examples when practice staff had referredchildren where safeguarding concerns had been identified.Effective liaison was in place between the practice and thehealth visiting team and school nurse.
• Immunisation rates were relatively high for all standardchildhood immunisations, and in line with local averages. Forexample, vaccination rates for children under two years oldranged from 93.5% to 100% compared against a CCG averageranging from 91.7% to 100%. A named member of the practiceteam monitored uptake of childhood vaccinations to enablethose who did not attend to be notified promptly.
• Patients told us that children and young people were treated inan age-appropriate way and were recognised as individuals,and we saw evidence to confirm this.
• Appointments with the practice nursing team were availableoutside of school hours, and the premises were suitable forchildren and babies. Toys were provided for children attendingthe surgery.
• Teenagers presenting at the surgery were seen on attendancewhenever possible to ensure they were seen at the time ofneed.
• Family planning advice was available on site, and the practicereferred patients requiring the fitting of coils and contraceptiveimplants to a local clinic in Nottingham.
• There were no dedicated baby changing facilities or room forbreast feeding, but patients would be directed to anappropriate room to enable some privacy.
Good –––
Working age people (including those recently retired andstudents)
• The needs of the working age population, those recently retiredand students had been identified and the practice had adjustedthe services it offered to ensure these were accessible, flexibleand offered continuity of care. This included good access to GPappointments and extended hours surgery were provided eachweek, including occasional Saturday mornings when required.
Good –––
Summary of findings
11 Giltbrook Surgery Quality Report 10/03/2016

• A nurse practitioner held daily telephone triage consultationswhich often meant patients’ concerns could be dealt withwithout the need for a face to face consultation at the practice.
• The practice was proactive in offering online services to bookGP appointments and repeat prescriptions.
• Health promotion and screening was provided that reflectedthe needs for this age group. The practice had over-achieved itstarget for 40-74 year old patients’ health checks.
• Flu clinics were held on a Saturday morning to improve accessto vaccinations for working patients.
• The practice’s uptake for the cervical screening programme was87.4% which was above the CCG average of 86.2% and thenational average of 81.8%.
People whose circumstances may make them vulnerable
• The practice held a register of patients living in vulnerablecircumstances including those with a learning disability.Homeless people could register with the practice.
• The practice informed us how they had arranged appointmentsspecifically to meet individual needs – for example, by ensuringa patient with a learning disability could be seen when no otherpatients were waiting in the surgery, as this created anxiety forthem.
• The practice provided care for residents in a local residentialunit for patients with a learning disability. We spoke to staff atthe home who praised the practice for being highly responsiveto their clients’ needs, and also reported the high level of careand support that was provided.
• The practice regularly worked with multi-disciplinary teams inthe case management of vulnerable people and informedpatients how to access various support groups and voluntaryorganisations.
• Staff knew how to recognise signs of abuse in vulnerable adultsand children. Staff were aware of their responsibilities regardinginformation sharing, documentation of safeguarding concernsand how to contact relevant agencies in normal working hoursand out of hours.
• The practice provided good care and support for patientsnearing the end of their life. Patients were kept under closereview by the practice in conjunction with the widermulti-disciplinary team, and a GP informed us that additionalvisits had been provided at the weekend to ensure continuity ofcare.
Outstanding –
Summary of findings
12 Giltbrook Surgery Quality Report 10/03/2016

• The practice had carried out annual health checks for peoplewith a learning disability, and 90% of patients had received anannual review in the last 12 months. It offered longerappointments for people with a learning disability.
• Annual training in learning disability awareness helped staffunderstand and respond to the needs of patients effectively.
• The practice was registered as a ‘safe house’ whereby anyvulnerable individual could come into the surgery, until theycould be collected by a family member or carer.
People experiencing poor mental health (including peoplewith dementia)
• The practice achieved 100% for mental health relatedindicators in QOF, which was above the CCG average of 93.8%and the national average of 92.8%
• 93.3% of patients diagnosed with dementia had had their carereviewed in a face-to-face consultation during 2014-15. Thiscompared to a CCG average of 87.7% and a national average of84%
• 86% of patients on the practice’s mental health register hadreceived an annual health check during 2014-15.
• The practice regularly worked with multi-disciplinary teams inthe management of people experiencing poor mental health,including those with dementia. The practice closely monitoredpatient compliance with their prescribed medications and tookaction to review any patients who were did not take them asprescribed.
• It carried out advance care planning for patients with dementia.• The practice told patients experiencing poor mental health and
patients with dementia about how to access services includingtalking therapies and various support groups and voluntaryorganisations. Some information was available for patients inthe waiting area including a self-help directory.
• Health checks were offered to carers and contingency planswere considered in case the carer became unwell.
Outstanding –
Summary of findings
13 Giltbrook Surgery Quality Report 10/03/2016

What people who use the service sayWe reviewed the national GP patient survey resultspublished on 7 January 2016. The results showed thepractice was performing above local and nationalaverages. 266 survey forms were distributed and 115 werereturned, which was equivalent to a 43% completion rate.
• 99% of patients found it easy to get through to thissurgery by phone compared to a CCG average of 71%and a national average of 73%.
• 96% of patients found the receptionists at thissurgery helpful compared to a CCG average of 87%and a national average of 87%.
• 95% of patients were able to get an appointment tosee or speak to someone the last time they triedcompared to a CCG average of 86% and a nationalaverage of 85%.
• 96% of patients said the last appointment they gotwas convenient compared to a CCG average of 91%and a national average of 92%.
• 91% of patients described their experience ofmaking an appointment as good compared to a CCGaverage of 73% and a national average of 73%.
• 83% of patients usually waited 15 minutes or lessafter their appointment time to be seen compared toa CCG average of 63% and a national average of 65%.
As part of our inspection we also asked for CQC commentcards to be completed by patients prior to our inspection.We received 147 comment cards of which 98% werepositive about the standard of care received, andemphasised the level of care provided by the practiceteam. Patients commented that the environment wasclean, that staff treated them with dignity and respect,and that they were very happy with the care provided.The three negative comments related to access to aparticular GP, the availability of appointments, andaccessing the computer for information during aconsultation. We also saw two emails received by thepractice that week from patients thanking the practice forhelping them.
We spoke with seven patients during the inspection. Allseven patients said that they were happy with the carethey received and thought that staff were committed andcaring. They told us that GP and nurse appointmentswere easy to book, and that they would always be seenon the day if urgent and in less than a week for a routineappointment. Patients told us that they were seen ontime and consent was sought where appropriate. Theeffects of any medicines were explained and agreed withpatients. One patient who was a carer explained theywere offered advice and signposted to sources ofsupport.
Summary of findings
14 Giltbrook Surgery Quality Report 10/03/2016

Our inspection teamOur inspection team was led by:
Our inspection team was led by a CQC Lead Inspector.The team included a GP specialist advisor, and anExpert by Experience. An expert by experience is aperson who has personal experience of using or caringfor someone who uses this type of service
Background to GiltbrookSurgeryGiltbrook Surgery is situated approximately ten kilometresnorth-west of Nottingham, close to junction 26 of the M1motorway.
The practice is run by a partnership between a GP and thepractice manager.
The practice has two GPs (one male and one female), oneof whom is a partner, and the other doctor is a part-timesalaried GP. The practice has a nurse practitioner and apart-time practice nurse, and part-time health careassistant. The clinical team is supported by a full-timepractice manager (who is also a partner) and a team of sixadministrative, secretarial and reception staff. The practicealso currently have an apprentice in post to support theadministration team.
The registered practice population of 4,297 arepredominantly of white British background, and are rankedin the third least deprived decile. The list size is graduallyincreasing creating challenges in terms of their existingpremises, which are being utilised to full capacity. The
practice age profile is broadly in line with national averagesbut has slightly higher percentages of patients aged 40-74years old, and slightly lower percentages of patients agedunder 40.
The practice opens from 8am until 6.30pm Monday toFriday. GP morning appointments are available from8.30am to between 11.30am and 1pm depending on whichday, and afternoon surgeries run from 1.30pm to 6pm on aMonday and Thursday, and from 3pm to 6pm on Tuesday,Wednesday and Friday. Extended hours GP surgeries areprovided from 7.30am to 8.30am on a Wednesday morning,and from 6.30pm until 8.15pm on a Monday evening.Occasional Saturday morning clinics are also provided inresponse to need, for example, when there is a bankholiday. The practice are considering the potential toextend the availability of Saturday clinical sessions.
The practice supports medical students as part of theireight week placement in general practice. It does notcurrently act as a training practice for GP registrars.
The practice has opted out of providing out-of-hoursservices to its own patients. When the practice is closedpatients are directed to Nottingham Emergency MedicalServices (NEMS) via the 111 service.
The practice holds a Personal Medical Services (PMS)contract to provide GP services which is commissioned byNHS England. A PMS contract is one between GPs and NHSEngland to offer local flexibility compared to the nationallynegotiated General Medical Services (GMS). The practicealso offers a range of enhanced services, including themonitoring of blood tests for patients with stable prostatecancer, which are commissioned by NHS Nottingham Northand East CCG.
GiltbrGiltbrookook SurSurggereryyDetailed findings
15 Giltbrook Surgery Quality Report 10/03/2016

Why we carried out thisinspectionWe inspected this service as part of our newcomprehensive inspection programme.
We carried out a comprehensive inspection of this serviceunder Section 60 of the Health and Social Care Act 2008 aspart of our regulatory functions. The inspection wasplanned to check whether the provider is meeting the legalrequirements and regulations associated with the Healthand Social Care Act 2008, to look at the overall quality ofthe service, and to provide a rating for the service under theCare Act 2014.
How we carried out thisinspectionBefore our inspection, we reviewed a range of informationthat we hold about the practice and asked otherorganisations including NHS England and NHS NottinghamNorth and East CCG to share what they knew.
We carried out an announced inspection on 28 January2016 and during our inspection:
• We spoke with staff including GPs, the practicemanager/partner, the practice nurse and a number ofreception and administrative staff. In addition, we spokewith the pharmacist and the project manager of thecommunity pharmacy project, a manager of the localcommunity health services teams, managers and carersat two local care homes regarding their experience ofworking with the practice team. We also spoke withseven patients who used the service, and arepresentative from the practice patient participationgroup.
• We observed how people were being cared for fromtheir arrival at the practice until their departure, andreviewed the information available to patients and theenvironment.
• We reviewed 147 comment cards where patients andmembers of the public shared their views andexperiences of the service.
• We reviewed practice protocols and procedures andother supporting documentation including staff filesand audit reports.
To get to the heart of patients’ experiences of care andtreatment, we always ask the following five questions:
• Is it safe?
• Is it effective?
• Is it caring?
• Is it responsive to people’s needs?
• Is it well-led?
We also looked at how well services are provided forspecific groups of people and what good care looks likefor them. The population groups are:
• Older people
• People with long-term conditions
• Families, children and young people
• Working age people (including those recently retiredand students)
• People whose circumstances may make themvulnerable
• People experiencing poor mental health (includingpeople with dementia)
Detailed findings
16 Giltbrook Surgery Quality Report 10/03/2016

Our findingsSafe track record and learning
There was an effective system in place for reporting andrecording significant events. Staff told us they would informthe practice manager of any incidents and there was also arecording form available on the practice’s computersystem.
The practice carried out a thorough analysis of thesignificant events. We were informed that actions wereimplemented to address issues at the earliest opportunity,and the findings were regularly discussed at clinical andwider staff meetings. We reviewed ten significant eventswhich had been recorded over the last 12 months. Lessonswere shared to make sure action was taken to improvesafety in the practice. For example, medicine had beenprescribed to a patient on the recommendation of ahospital doctor which was incorrect for their specific needs.Following the incident advice on new medications receivedfrom other clinicians was always reviewed to checkdosages and regimes were correct.
The practice had also worked with a GP from aneighbouring practice who shared outcomes from one oftheir own significant events to facilitate wider learning. Thisincluded the sharing of practice protocols to ensureconsistency and best practice.
When there were unintended or unexpected safetyincidents, people received support and an apology, andwere told about any actions to improve processes toprevent the same thing happening again.
The practice had a robust approach to informationreceived from the Medicines and Healthcare RegulatoryAgency (MHRA). We observed evidence of patient searchesfor each alert received and follow up actions being takenand documented to keep patients safe. A clear audit trailwas maintained to demonstrate the effectiveness of thesystem in place.
Overview of safety systems and processes
• Arrangements were in place to safeguard children andvulnerable adults from abuse that reflected relevantlegislation and local requirements and policies wereaccessible to all staff. The policies clearly outlined whoto contact for further guidance if staff had concernsabout a patient’s welfare. There was a lead GP for
safeguarding, with the appropriate safeguardingtraining at level 3. Meetings took place every 6-8 weeksbetween the GP safeguarding lead and practicemanager/partner with the health visitor and schoolnurse to discuss any children at risk, and these meetingswere documented and shared with the practice team.The health visitor attended the practice weekly toensure effective liaison with regards to any concerns.Staff demonstrated they understood theirresponsibilities for safeguarding and all had receivedtraining relevant to their role. We were informed of anevent where the team took prompt and effective actionto protect children at risk of harm.
Learning had been applied from a concern raised by apatient about displaying their name on the patient callscreen in reception. This issue had been explored by aPPG audit and whilst most patients were happy with thesystem, it did raise the need to protect the identity ofpatients such as those at risk of domestic violence orchildren in foster care.
• A notice in the waiting room and on the door of eachconsulting room advised patients that staff would act aschaperones, if required. All staff who acted aschaperones were trained for the role and had received adisclosure and barring check (DBS check). (DBS checksidentify whether a person has a criminal record or is onan official list of people barred from working in roleswhere they may have contact with children or adultswho may be vulnerable).
• The practice was clean and maintained to a highstandard. The practice nurse was the identified infectioncontrol clinical lead. There was an infection controlpolicy in place and staff had received training relevant totheir role. Annual infection control audits wereundertaken and we saw evidence that action was takento address any improvements identified as a result. Thepractice employed their own cleaner and haddeveloped cleaning schedules with robust monitoringto ensure high standards were maintained.
• The arrangements for managing medicines, includingemergency drugs and vaccinations, in the practice keptpatients safe. Prescription pads were securely storedand there were systems in place to monitor their use.Patient Group Directions were in place to allow nurses
Are services safe?
Good –––
17 Giltbrook Surgery Quality Report 10/03/2016

to administer medicines in line with legislation, andthere was a system for the production of Patient SpecificDirections to enable health care assistants to administervaccinations when appropriate.
• We reviewed five personnel files and found thatappropriate recruitment checks had been undertakenprior to employment. For example, proof ofidentification, references, qualifications, registrationwith the appropriate professional body and theappropriate checks through the Disclosure and BarringService.
Monitoring risks to patients
Risks to patients were assessed and well managed.
• There was a health and safety policy available and therewere procedures in place for monitoring and managingrisks to patient and staff safety. The practice had up todate fire risk assessments and carried out regular firetraining including trial evacuations. All electricalequipment had been checked to ensure the equipmentwas safe to use and clinical equipment was validated toensure it was working properly. The practice also had avariety of other risk assessments in place to monitorsafety of the premises such as control of substanceshazardous to health and legionella. We saw evidencethat clinical staff had received vaccinations to protectthem against hepatitis B.
• Arrangements were in place for planning andmonitoring the number of staff and mix of staff neededto meet patients’ needs. There was a rota system inplace for all the different staffing groups to ensure thatenough staff were on duty.
Arrangements to deal with emergencies and majorincidents
The practice had adequate arrangements in place torespond to emergencies and major incidents.
• There was an instant messaging system on thecomputers in all the consultation and treatment roomsand patient areas which alerted staff to any emergency.
• All staff had received annual basic life support training.
• The practice had a defibrillator available on thepremises and oxygen with adult and children’s masks.There was also a first aid kit and accident bookavailable.
• Emergency medicines were easily accessible to staff in asecure area of the practice and all staff knew of theirlocation. All the medicines we checked were in date andfit for use.
• The practice had an up to date comprehensive businesscontinuity plan in place for major incidents such aspower failure or building damage. The plan includedemergency contact numbers for staff.
Are services safe?
Good –––
18 Giltbrook Surgery Quality Report 10/03/2016

Our findingsEffective needs assessment
The practice had systems in place to keep all clinical staffup to date. The practice assessed needs and delivered careand treatment in line with relevant and current evidencebased guidance and standards, including National Institutefor Health and Care Excellence (NICE) guidelines, and localguidance, for example, in relation to prescribing. Thepractice monitored that these guidelines were followedthrough clinical discussions and audits.
Management, monitoring and improving outcomes forpeople
The practice used the information collected for the QualityOutcomes Framework (QOF) and performance againstnational screening programmes to monitor outcomes forpatients. (QOF is a system intended to improve the qualityof general practice and reward good practice). The mostrecent published results showed the practice had achieved91.6% of the total number of points available (comparedagainst a CCG average of 95.1% and a national average of93.5%, with a 9.5% exception reporting rate which was inline with local and national averages. Data from 2014-5showed;
• Performance for diabetes related indicators at 65.1%was below the CCG average of 87.3% and the nationalaverage of 89.2%. The practice had developed actions inresponse to this such as ensuring the more effectiverecall of patients, and performance was improved at thetime of our inspection and practice supplied datashowed the performance had improved on theseindicators.
• Data for 2014-15 showed the practice as being an outlierat 57.8% for patients with diabetes with a bloodpressure reading of 140/80mmHg or less. The nationalaverage was 78% for this indicator. This issue had beendiscussed at a clinical meeting with measures agreed toaddress this. The practice’s own data demonstrated thattheir performance on this indicator had improved to66% in the current year to date. It was also noted thatthey had a marginally lower exception rate compared tolocal averages for this indicator.
• The percentage of patients with hypertension havingregular blood pressure tests at 82.8% was slightly abovethe CCG average of 80.1%, but in line with the nationalaverage of 82%
• The achievement of 100% for mental health relatedindicators was above the CCG average of 93.8% and thenational average of 92.8%
• 93.3% patients with a diagnosis of dementia had theircare reviewed in a face to face consultation in thepreceding 12 months. This was 5.5% higher than theCCG average and 9.3% above the England average.
Clinical audits demonstrated quality improvement.
• There had been three full clinical audits completed inthe lastyear, where the improvements made wereimplemented and monitored.
• Findings were used by the practice to improve services.For example, a recent full cycle clinical audit wascompleted on prescribing the contraceptive pill forspecific patients with a potential risk of cardiovascularcomplications. The outcome was to reduce those at riskfrom specifically identified factors being prescribed thecontraceptive pill from 13 to five patients.
• A completed audit cycle demonstrated that patientswith atrial fibrillation (an irregular heart rate) werereviewed in line with NICE guidance to stop theprescribing of aspirin to reduce the risk of stroke, and toprescribe appropriate anticoagulation medicationwhere this was indicated.
• The practice participated in applicable local audits andbenchmarking. The CCG medicines management teamhad undertaken five medicines audit in the last year andhelped the practice to identify actions to improve safety.For example, an audit into a recent increase in antibioticprescribing recommended actions including shortercourses of antibiotics for specific conditions. Themedicines management team reported a goodrelationship with the practice and said they wereresponsive in resolving any identified issues. Thepractice had identified one of their administrators to bea medicines management facilitator to work with theCCG team on issues such as cost effectivenessalternative prescribing.
• The practice had also contributed to a research projecton gout with Nottingham University
Are services effective?(for example, treatment is effective)
Good –––
19 Giltbrook Surgery Quality Report 10/03/2016

We observed that the practice’s rate of attendances at theA&E department was low and they achieved the secondlowest rate amongst the 21 GP practices across the CCGarea. Some patients had accessed a nearby walk-in centrebut the practice was auditing those who attended A&E andthe walk-in services during GP surgery hours to determinetheir reasons for not coming to the practice. The practicewere using this as an opportunity to educate patientsabout the appropriate use of emergency and walk-inservices.
Effective staffing
Staff had the skills, knowledge and experience to delivereffective care and treatment.
• The practice had reviewed the skill mix within their teamand had introduced a nurse practitioner role in2013.This helped to improve access for patients byimplementing a triage system, as well as being able tosee patients that otherwise would have needed to seethe GP. The practice had also recruited a salaried GP inlate 2014 directly from the GP Vocational TrainingScheme. A new practice nurse appointment in the lasteighteen months had completed the clinical team andcreated stability to enable team development.
• The practice team had been enhanced from November2015 by the addition of a community pharmacist withinthe practice team as part of an ongoing pilot project tosite community pharmacy advice within GP practices.Despite this project being in its early stages, thepharmacist had undertaken a range of medicationreviews, advised the nurse on any prescribing concernsfor those patients attending for a review of theirdiabetes, instigated cost effective drug switches,provided pharmacy advice to the local care home, andhad seen some patients presenting with a minor illness.This role helped to give the GPs additional capacity tosee more complex patients, and offered patients a moreresponsive service with regards to keeping theirmedicines under close review. The pharmacist was alsomaking a valuable contribution to QOF achievements –for example by reviewing the medication of patientswith chronic kidney disease and ensuring these were inaccordance with NICE guidelines. An audit was plannedto be undertaken to measure the impact of this.
• We saw evidence of completed induction programmesfor newly appointed members of staff that covered suchtopics as safeguarding, infection prevention and control,fire safety, health and safety and confidentiality.
• The learning needs of staff were identified through asystem of appraisals, meetings and reviews of practicedevelopment needs. Staff had access to and made useof e-learning training modules as well as in-housetraining and training organised by their CCG. Staff hadreceived mandatory training that included safeguarding,fire procedures, basic life support and informationgovernance awareness. Staff also received annualtraining to raise their awareness of learning disabilities.
• The practice ensured role-specific training with updateswas undertaken for relevant staff e.g. for those reviewingpatients with long-term conditions, administeringvaccinations and taking samples for the cervicalscreening programme.
• All staff had received an appraisal within the last 12months, and mid-year reviews were in place to assesseach individual’s progress with agreed objectives. Thepractice manager/partner had arranged their ownappraisal with the Local Medical Committee (LMC) dueto their particular circumstances as a partner.
Coordinating patient care and information sharing
The information needed to plan and deliver care andtreatment was available to relevant staff in a timely andaccessible way through the practice’s electronic patientrecord. This included care plans and risk assessments,medical history, and investigation and test results.
The practice shared relevant information with otherservices in a timely way, for example when referring peopleto other services. The practice had developed their owncomprehensive guide on referrals listing where and how torefer to different services, and this was updated as newinformation was received. This meant referrals were sent tothe right place in a timely manner to enhance patientexperience and care. It also provided a useful referenceguide for new and temporary staff members.
Practice staff worked with other care services tounderstand and meet the range and complexity of people’sneeds and to assess and plan ongoing care and treatment.This included patients at risk of hospital admission, andthose at end of life. We saw an example of the electronicpalliative care co-ordination systems (EPaCCS) used to
Are services effective?(for example, treatment is effective)
Good –––
20 Giltbrook Surgery Quality Report 10/03/2016

share details of people’s care preferences and key detailsabout their care at end of life, for example, if they wereadmitted to hospital. This had meaningful and usefulinformation included to ensure the best care for the patientif needed by other providers.
We saw evidence that multi-disciplinary team meetingstook place on a monthly basis, including the communitymatron, district nursing team and Macmillan nurse, andthese discussions were well documented, with care plansbeing reviewed and updated accordingly.
Consent to care and treatment
• Staff sought patients’ consent to care and treatment inline with legislation and guidance.
• Staff understood the relevant consent anddecision-making requirements of legislation andguidance, including the Mental Capacity Act 2005. Aneasy information guide was available for staff if they hadany queries about their responsibilities.
• When providing care and treatment for children andyoung people, staff carried out assessments of capacityto consent in line with relevant guidance.
• Where a patient’s mental capacity to consent to care ortreatment was unclear the GP or practice nurseassessed the patient’s capacity and, where appropriate,recorded the outcome of the assessment. Care homestaff informed us how GPs had contributed towards bestinterest assessments and actively listened to the viewsof staff and relatives.
Health promotion and prevention
The practice provided smoking cessation support andadvice on weight management. Patients could also bereferred into a local service to help them stop smoking, andinto community based schemes to support weight loss.Clinicians from the practice had agreed to give a
presentation on prostate cancer to members of the RotaryClub, and also undertake opportunistic blood pressuremonitoring to identify any individuals who may need toattend their GP for a more formal clinical assessment.
The practice’s uptake for the cervical screening programmewas 87.4%, which was comparable to the CCG average of86.2% and above the national average of 81.8%. There wasa policy to offer telephone reminders for patients who didnot attend for their cervical screening test. The practicealso encouraged its patients to attend national screeningprogrammes for bowel and breast cancer screening anduptake was again generally in line with the CCG averageand slightly higher than the national percentages.
Childhood immunisation rates were comparable to CCGand national averages. For example, childhoodimmunisation rates for the vaccinations given to under twoyear olds ranged from 93.5% to 100% and five year oldsfrom 87.9% to 97%, and these were comparable to CCGaverages. Flu vaccination rates for the over 65s were 75.4%compared to a national average of 73.24%, and at riskgroups were 50.68% compared nationally to 55.97%.
Patients had access to appropriate health assessments andchecks. These included health checks for new patients andNHS health checks for people aged 40–74. During 2014-15,the practice had exceeded its health check targets. Theyhad invited 299 patients (against a target of 255) and hadcompleted 179 checks (against a target of 142) and this wasdelivered by the proactive approach undertaken by thepractice by encouraging patients to attend. The firstthree-quarters of 2015-16 showed this was beingmaintained in that the practice had achieved 124% of itstarget. This was recognised by the CCG who wereconsidering the potential of the practice being able toprovide this service for other local practices who werestruggling to meet targets. Appropriate follow-ups on theoutcomes of health assessments and checks were made,where abnormalities or risk factors were identified.
Are services effective?(for example, treatment is effective)
Good –––
21 Giltbrook Surgery Quality Report 10/03/2016

Our findingsRespect, dignity, compassion and empathy
We observed that members of staff were courteous andvery helpful to patients and treated people dignity andrespect.
• Curtains were provided in consulting rooms to maintainpatients’ privacy and dignity during examinations,investigations and treatments. We observed thatconsultation and treatment room doors were closedduring consultations to ensure patient confidentiality.
• Reception staff offered patients a private room todiscuss sensitive issues, or if they appeared to bedistressed.
• Clinicians came into the reception area to call and greetpatients and offered assistance with mobility if this wasrequired.
The vast majority (98%) of the 147 patient CQC commentcards we received were positive about the serviceexperienced. Patients said they felt the practice offered anexcellent service and staff were helpful, caring and treatedthem with dignity and respect.
We also spoke with a member of the patient participationgroup. They told us they were satisfied with the careprovided by the practice and said their dignity and privacywas respected.
Results from the national GP patient survey showedpatients felt they were treated with compassion, dignityand respect. The practice was above average for itssatisfaction scores on consultations with doctors andnurses and interactions with receptionists. For example:
• 93% of patients said the GP was good at listening tothem compared to the CCG and national average of89%.
• 94% of patients said the GP gave them enough timecompared to the CCG and national average of 87%.
• 97% of patients said they had confidence and trust inthe last GP they saw compared to the CCG and nationalaverage of 95%.
• 91% of patients said the last GP they spoke to was goodat treating them with care and concern compared to theCCG average of 84% and the national average of 85%.
• 93% of patients said the last nurse they spoke to wasgood at treating them with care and concern comparedto the CCG and national average of 91%.
• 96% of patients said they found the receptionists at thepractice helpful compared to the CCG and nationalaverage of 87%.
Care planning and involvement in decisions aboutcare and treatment
Patients told us that they felt involved in decision makingabout the care and treatment they received. They also toldus they felt listened to and supported by staff and hadsufficient time during consultations to make an informeddecision about the choice of treatment available to them.Patient feedback on the comment cards we received wasalso positive and aligned with these views.
Results from the national GP patient survey showedpatients responded positively to questions about theirinvolvement in planning and making decisions about theircare and treatment. Results were in line with local andnational averages. For example:
• 92% of patients said the last GP they saw was good atexplaining tests and treatments compared to the CCGaverage of 86% and national average of 86%.
• 90% of patients said the last GP they saw was good atinvolving them in decisions about their care comparedto the CCG average of 80% and national average of 82%.
Staff told us that translation services were available forpatients who did not have English as a first language. Wesaw notices in the reception areas informing patients thisservice was available.
Patient and carer support to cope emotionally withcare and treatment
The practice identified patients who may be in need ofextra support. These included patients in the last 12months of their lives, carers, and those at risk of developinga long-term condition.
Notices in the patient waiting room told patients how toaccess a number of support groups and organisations, anda wide range of literature was available for patients.
The practice’s computer system alerted GPs if a patient wasalso a carer. The practice had identified 1.6% of thepractice list as carers, and identified new carers upon
Are services caring?
Outstanding –
22 Giltbrook Surgery Quality Report 10/03/2016

registration. Written information was available to directcarers to the support services available to them. Thepractice offered a more flexible approach in dealing withcarers, for example, they saw carers at short notice if thereappeared to be signs that they were struggling to cope.Health checks were offered to carers and contingency planswere considered in case the carer became unwell. Thepractice manager/partner was identified as the practiceCarer’s Champion and had established links with a localcarers’ charity.
We were informed of circumstances in which the GP hadvisited patients at the weekend to ensure continuity ofcare. The practice also told us that visits had been arrangedon occasions when vulnerable patients had failed to attendfor appointments or did not answer the telephone.
The practice made telephone contact with patients whowere in hospital when possible to help plan their needs atdischarge. During bad weather conditions in winter,
vulnerable patients were contacted to ensure they hadaccess to essential needs such as food and heating. Apatient informed us they had received a call from thepractice to check how their spouse was, even though thespouse was not a patient at the practice themselves.
The practice closely monitored patients with mental healthrelated-problems to ensure they were taking medication asprescribed, and took action to follow this up to ensurepatient safety. For example, this included checking ifmedicines were being received from another source if theyhad not been collected, or to ensure the patient continuedto take any necessary medicines until they had beenassessed by a clinician. Staff told us that if families hadexperienced bereavement, they were contacted to offercondolences. This call offered a patient consultation if thiswas required. The GP would also visit relatives following abereavement when this was deemed appropriate.
Are services caring?
Outstanding –
23 Giltbrook Surgery Quality Report 10/03/2016

Our findingsResponding to and meeting people’s needs
• The practice reviewed the needs of its local populationand engaged with the NHS England Area Team andClinical Commissioning Group (CCG) to secureimprovements to services where these were identified.For example, the community pharmacy pilot projectaimed to develop new models of care to test if thequality of patient care could be improved by utilisingthe skills of a community pharmacy prescriber within aGP practice. The practice was also in liaison with theircommissioners regarding the development of theirpremises in order to expand and deliver a wider range ofservices from their site to enhance patient care andexperience.
• The community pharmacy pilot project had ensuredpatients had their medication needs were reviewedregularly, whilst also improving access for those withminor ailments. The pharmacist role had alreadyproduced benefits to patients through liaison with thepractice team – for example, the nurse told us that apatient could not take their tablets due to the size, butdiscussion with the pharmacist initiated an immediatechange to two smaller tablets.
• The practice offered extended hours GP appointmentswhich were intended mainly for working patients whocould not attend during normal opening hours. Thesewere available on a Wednesday morning from 7.30amand a Monday evening between 6.30pm and 8.15pm.Occasional Saturday morning clinics were also offered,for example, when there was a Bank Holiday impactingon appointment availability during the week.
• There were longer appointments available for people,including those with a learning disability. The practiceinformed us how they had arranged appointmentsspecifically to meet individual needs – for example, byensuring a patient could be seen when no otherpatients were waiting in the surgery, as this createdanxiety for them.
• Home visits were available for patients who wouldbenefit from these, including older people.
• Same day appointments were available for children andthose with serious medical conditions.
• There were facilities for people with limited mobility onsite. The practice was reviewing the ramped access to
the main entrance as one wheelchair user wasencountering difficulties in using this safely. There wasno hearing loop available, although the practice hadassessed the needs of known patients with hearingdifficulties and formulated an individual plan to addressthis.
• A private area was available away from reception forsensitive or confidential discussions to take place.
• Care home staff told us that the practice provided ahighly responsive service to older patients, and thosewith learning disabilities. This included visiting on thesame day when this was required. A ward rounds hadbeen established at a local care home on a fortnightlybasis to review the ongoing needs of these patients.
• Translation services were available for patients whoneeded them. A log in screen was available in English,Polish and Mandarin. The PPG had surveyed ethnicity toselect the languages used on the log in.
• The PPG undertook fundraising events for the practice inorder to fund additional equipment for patients. Thisincluded a pulse oximeter (to measure oxygen levels inblood), and a new chair for patients in the treatmentroom.
• A community phlebotomist (a clinical support workerwho takes blood samples from patients) attended thepractice for three hours each week. The health careassistant and practice manager/partner provided aphlebotomy service for patients at other times.
Access to the service
The practice was open between 8am and 6.30pm Mondayto Friday. GP appointments were available from 8.30am tobetween 11.30am and 1pm depending on which day, andafternoon surgeries ran from 1.30pm to 6pm on a Mondayand Thursday, and from 3pm to 6pm on Tuesday,Wednesday and Friday. Extended hours GP surgeries wereprovided from 7.30am to 8.30am on a Wednesday morning,and from 6.30pm until 8.15pm on a Monday. In addition topre-bookable appointments that could be booked inadvance without restriction, urgent appointments werealso available on the day for people that needed them.
On the day of our inspection, we observed that anappointment was available with either of the GPs or thenurse practitioner within five working days.
Are services responsive to people’s needs?(for example, to feedback?)
Outstanding –
24 Giltbrook Surgery Quality Report 10/03/2016

Results from the national GP patient survey showed thatpatient’s satisfaction with how they could access care andtreatment was higher than local and national averages.People told us on the day that they were able to getappointments when they needed them.
• 88% of patients were satisfied with the practice’sopening hours compared to the CCG and nationalaverage of 75%.
• 99% of patients said they could get through easily to thesurgery by phone compared to the CCG average of 71%and national average of 73%.
• 91% of patients described their experience of making anappointment as good compared to the CCG andnational average of 73%.
• 83% of patients said they usually waited 15 minutes orless after their appointment time compared to the CCGaverage of 63% and national average of 65%.
Listening and learning from concerns and complaints
The practice had an effective system in place for handlingcomplaints and concerns.
• Its complaints policy and procedures were in line withrecognised guidance and contractual obligations forGPs in England.
• The practice manager/partner was the designatedresponsible person who handled all complaints in thepractice.
• We saw that information was available in a folder withinthe waiting area to help patients understand thecomplaints system.
We looked at three complaints received in the last 12months and found these were satisfactorily handle anddealt with in a timely way in an open and transparentmanner. Lessons were learnt from concerns andcomplaints and action was taken to as a result to improvethe quality of care. For example, further to the receipt of acomplaint regarding a consultation, the patient was invitedto re-attend the practice to discuss their concerns in moredepth. On reflection, the clinician felt that the opportunityto share the decision making with the patient had not beenutilised to the best effect during the initial consultation,and emphasised the importance of involving the patientfully in decisions about their care.
Are services responsive to people’s needs?(for example, to feedback?)
Outstanding –
25 Giltbrook Surgery Quality Report 10/03/2016

Our findingsVision and strategy
The practice had a clear vision to deliver high quality careand promote good outcomes for patients.
• The practice had a mission statement which wasdisplayed on their website and in the waiting areas andstaff knew and understood the values
• The practice had formulated a strategy and a supportingbusiness plan was under development which reflectedthe vision and values.
Governance arrangements
The practice had an overarching governance frameworkwhich supported the delivery of the strategy and goodquality care. This outlined the structures and procedures inplace and ensured that:
• There was a clear staffing structure and that staff wereaware of their own roles and responsibilities. Thepractice had reviewed their skill mix to deliver servicesmore effectively, for example the introduction of thenurse practitioner role provided greater opportunitiesfor patient access and alleviated some pressures on GPappointments.
• The practice had implemented a comprehensive rangeof policies and these were up to date and readilyavailable to all staff.
• The practice manager/partner had devised clearstandard operating procedures to ensure continuity oftasks during the absence of key members of the team.Information was well organised, easy to read and readilyaccessible. The practice manager/partner had createdalarms on their calendar to ensure that when tasks weredue, a prompt was received to ensure things did not getmissed. For example, renewal of professionalregistrations for clinicians.
• The practice had an established programme of clinicaland internal audit, which was used to monitor qualityand to make improvements
• There were robust arrangements for identifying,recording and managing risks, issues and implementingmitigating actions, and these were kept under regularreview. The practice partners understood their
performance and continually sought to improve this. Forexample in relation to the achievement for diabetes carewithin QOF indicators for 2014-15, the practice hadassessed ways to improve their performance and wereshowing improvements at the time of our inspection.
• The practice had worked with a local practice to shareoutcomes and learning from an external significantevent to improve safety and quality in the wider healthcommunity.
• Clinical staff received ongoing support for their rolewithin the practice. For example, the pharmacist had aweekly debrief with the GP partner to discuss cases, andthe health care assistant had a weekly meeting with thepractice nurse.
• The practice engaged well with their CCG. The GPpartner attended CCG Clinical Cabinet meetings and fedback relevant issues to the team. These meetingsprovided a valuable opportunity to benchmark thepractice and gain a comprehensive understanding ofthe performance of the practice within their CCG. Thisensured the practice were aware of any issues that theymay have to address. The partners also engaged inlocality meetings with other practices, and the practicemanager/partner attended the practice managerforums. A practice nurse forum was under developmentin the locality.
Leadership, openness and transparency
Following unanticipated changes in the leadership of thepractice approximately six years ago, the practice hadundergone a turbulent period. However, this wasaddressed with great resilience and strength to ensurecontinuity of the service for patients and used as anopportunity to reshape the service. This change instigatedthe new partnership which over the recent years hadredesigned and built an effective and passionate team witha record of achievement. The partners in the practice hadthe experience, capacity and capability to run the practiceand ensure high quality care. The partners were visible inthe practice and staff told us that they were approachableand always took the time to listen to all members of staff.
There was a clear leadership structure in place and staff feltsupported by management.
Are services well-led?(for example, are they well-managed and do senior leaders listen, learnand take appropriate action)
Good –––
26 Giltbrook Surgery Quality Report 10/03/2016

• Clinical staff meetings were held monthly, and full staffmeetings took place approximately every six to eightweeks.
• Staff told us that there was an open culture within thepractice and they were able to select the issues fordiscussion at the team meetings. Staff told us they feltconfident and supported to raise issues, and that thesewere acted upon.
• Staff said they felt valued and supported by the partnersin the practice. The partners encouraged all members ofstaff to identify opportunities to improve the servicedelivered by the practice.
Seeking and acting on feedback from patients, thepublic and staff
• The practice encouraged and valued feedback frompatients and staff and used this to continually evaluatetheir service and improve care for patients.
It had gathered feedback from patients through the patientparticipation group (PPG) and through surveys andcomplaints received. There was an active PPG which meton a quarterly basis, carried out patient surveys andsubmitted proposals for improvements to the practicemanagement team. For example, the PPG had surveyedpatients regarding the choice of background music used inthe waiting area following a criticism of the radio stationused by the practice. The 141 responses showed that only9% of patients agreed with the patient who raised theconcern and had expressed their own preferred station,and it was decided to use the station that the majority ofpatients had opted for. There was a notice board to informpatients about the PPG’s work and to encourage newmembers to join them.
• The practice routinely audited monthly feedback fromthe Family and Friends Test (FFT). The most recentreturns indicated that 98% of patients who respondedwould recommend the surgery to others. The feedbackin respect of “if we could change one thing” wasanalysed and actions were implemented in response tothe feedback received. The CCG had nominated thepractice for an award for the FFT work in recognition oftheir commitment to this programme.
• The practice had also gathered feedback from staffthrough a staff survey, and generally through staff
meetings, appraisals and discussion. The staff surveydemonstrated a high level of satisfaction. Staff told usthey would not hesitate to give feedback and discussany concerns or issues with colleagues andmanagement - for example, the practice nurse informedus that when she commenced her role, the layout offixed furniture in the room was not effective eitherergonomically or functionally. When this issue wasraised with the partners, alterations were made in orderfor the nurse to work more easily.
Continuous improvement
There was a focus on continuous learning andimprovement within the practice. The practice team wasforward thinking and actively engaged in schemes toimprove outcomes for patients in the area. The practicewas part of a pilot practice with NHS England on theirproject "Unlocking the potential of Unlocking the Potentialof Community Pharmacy: A Challenge Fund for CommunityPharmacy Transformation”. They had a pharmacist workingat the practice two days a week supporting the agreedcategory of patients. The CCG had invited the practice to beinvolved in this project due to their history of achievementand willingness to consider new ways of working. Therewere only six GP pilot sites chosen across the counties ofDerbyshire and Nottinghamshire. Whilst the project wasawaiting a formal evaluation from Nottingham University,the project had already achieved:
• Reductions in the number of medications prescribedwith between 10-15% patients having at least of one oftheir prescribed medications stopped
• Reductions in dosages of medicines by approximately5%
• An improved understanding by patients of theirmedication
• Effective support and advice to practice team staff toenhance patient care and experience
The practice were aware that their existing premises limitedtheir future vision for growth and the ability to host moreservices on site for their patients. There was also likely to beincreased demand from planned new housing in the localvicinity. An infrastructure bid was in progress with apotential to develop new purpose-built and enhancedpremises in the future.
Are services well-led?(for example, are they well-managed and do senior leaders listen, learnand take appropriate action)
Good –––
27 Giltbrook Surgery Quality Report 10/03/2016