Gastrointestinal Bleeding Rajeev Jain, M.D.. GI Bleeding Background Acute Upper GI Bleed Acute Lower...
-
Upload
mervin-isaac-horton -
Category
Documents
-
view
246 -
download
5
Transcript of Gastrointestinal Bleeding Rajeev Jain, M.D.. GI Bleeding Background Acute Upper GI Bleed Acute Lower...

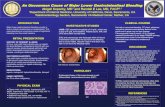
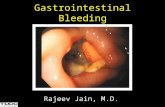
Gastrointestinal Bleeding
Rajeev Jain, M.D.

GI Bleeding
• Background
• Acute Upper GI Bleed
• Acute Lower GI Bleed

Clinical PresentationDefinitions
Hematemesis: bloody vomitus (bright red or coffee-grounds)
Melena: black, tarry, foul-smelling stool
Hematochezia: bright red or maroon blood per rectum
Occult: positive guaiac test
Symptoms of anemia: angina, dyspnea, or lightheadedness

Clinical Presentation
• Reflection of bleeding:–Site
–Etiology
–Rate

Initial Patient Assessment Hemodynamic Status

Resuscitation• 2 large bore peripheral IV’s• Colloid (normal saline or lactated Ringer’s)• Transfuse packed RBCs
– In elderly, goal Hct 30%– In young, goal Hct 20-25%– In cirrhotics, goal Hct 25-28%
• Correct coagulopathy• Reassess hemodynamics

History
• Prior history of bleeding• Previous gastrointestinal illnesses• Previous surgery• Other medical conditions (ie, cirrhosis)• Medications
– Aspirin, NSAIDs, & anti-platelet agents– Anticoagulants– ? SSRIs
• Abdominal pain, weight loss

Physical Exam & Labs
• Focused but thorough– Look for markers of liver disease
• Laboratory studies– CBC– INR– Electrolytes– Type and crossmatch RBCs

Acute BleedingChanges Before and After 2 Liter Bleed
0
1
2
3
4
5
6
Before During 24-72 Hrs
VO
LU
ME
( L
)
Plasma RBC
27%45%45%

Location of Bleeding
• Upper– Proximal to Ligament of Treitz– Melena (100-200 cc of blood)– Azotemia– Nasogastric aspirate
• Lower– Distal to Ligament of Treitz– Hematochezia

Acute UGIBDemographics
• Annual incidence of hospitalization: 100/100,000 persons
• 80% self-limited• Mortality stable at 10%• Continued or recurrent bleeding -
mortality 30-40%

• Cause of bleeding
• Severity of initial bleed
• Age of the patient
• Comorbid conditions
• Onset of bleeding during hospitalization
Acute UGIBPrognostic Indicators

NASOGASTRIC ASPIRATE
STOOL COLOR
MORTALITY RATE (%)
Clear Red, brown, or black 10
Coffee Grounds Brown or black 10
Red 20
Red Blood Black 10
Brown 20
Red 30
Acute UGIBPrognostic Indicators
Tedesco et al. ASGE Bleeding Survey. Gastro Endo. 1981.

Acute UGIBDifferential Diagnosis

• Peptic ulcer disease– Gastric ulcer– Duodenal ulcer
• Mallory-Weiss tear• Portal hypertension
– Esophagogastric varices
– Gastropathy
• Esophagitis
• Dieulafoy’s lesion• Vascular anomalies• Hemobilia• Hemorrhagic
gastropathy• Aortoenteric fistula• Neoplasms
– Gastric cancer– Kaposi’s sarcoma
Acute UGIBDifferential Diagnosis

DIAGNOSES % OF TOTAL
Duodenal ulcer 24Gastric erosions 23Gastric ulcer 21Varices 10Mallory-Weiss tear 7Esophagitis 6
Acute UGIBFinal Diagnoses of the Cause in 2225
Patients
Tedesco et al. ASGE Bleeding Survey. Gastro Endo. 1981.

DIAGNOSES % OF TOTAL
Peptic ulcer 55 Varices 14 Angioma 6 Mallory-Weiss tear 5 Erosions 4 Tumor 4
Acute UGIBCauses in CURE Hemostasis Studies
(n=948)
Savides et al. Endoscopy 1996;28:244-8.

Acute UGIBCORI Database: 7822 EGDs b/n 1999-2001
Boonpongmanee S. et al. Gastrointest Endosc 2004;59:788-94.

Peptic UlcersStigmata of Recent Hemorrhage (SRH)

Acute Peptic Ulcer BleedingPrognosis by SRH
Laine and Peterson. New Eng J Med 1994;331:717-27.

• Thermal– Bipolar probe– Monopolar probe– Argon plasma
coagulator– Heater probe
• Mechanical– Hemoclips– Band ligation
• Injection– Epinephrine– Alcohol– Ethanolamine– Polidocal
Endoscopic Therapy of PUD

Endoscopic Therapy of PUD
Laine and Peterson New Eng J Med 1994;331:717-27.

Peptic Ulcer BleedingAdjuvant Medical Therapy
• Erythromycin– 250 mg IV 30 minutes before
endoscopy decreases blood in stomach
• Proton pump inhibitor therapy– 80 mg IV bolus followed by 8
mg/hr continuous infusion for 72 hrs
– Reduced risk:• Rebleeding (NNT 12)• Surgery (NNT 20)
Leontiadis, G. et al. BMJ 2005;330:568

Mallory-Weiss Tear

Esophageal Varices

Variceal Band Ligation

Variceal Band Ligation

Variceal Band Ligation

• Octreotide• Cyclic octapeptide analog of
somatostatin• Longer acting than somatostatin• Equivalent to sclerotherapy and
improves endoscopic results
MEDICAL THERAPYAcute Variceal Bleeding

Transjugular Intrahepatic Portosystemic Shunt (TIPS)
IVC
Portal Vein
Splenic Vein
Coronary Vein

Aortoduodenal Fistula
Aorta
Duodenum
Graft
Fistula

Acute UGIB Surgery
• Recurrent bleeding despite endoscopic therapy
• > 6-8 units pRBCs

Acute LGIBDifferential Diagnosis

• Diverticulosis• Colitis
– IBD (UC>>CD)– Ischemia– Infection
• Vascular anomalies• Neoplasia• Anorectal
– Hemorrhoids– Fissure
• Dieulafoy’s lesion• Varices
– Small bowel– Rectal
• Aortoenteric fistula• Kaposi’s sarcoma
• UPPER GI BLEED
Acute LGIBDifferential Diagnosis

DIAGNOSES % OF TOTAL
Diverticulosis 40Vascular anomalies 30Colitis 21Neoplasia 14Anorectal 10Upper GI sites 10
Acute LGIBDiagnoses in pts with hemodynamic
compromise.
Zuccaro. ASGE Clinical Update. 1999.

Etiology of Acute LGIB
Strate LL. Gastroenterol Clin North Am. 2005 Dec;34(4):643-64.

Outcomes of Acute LGIB
Strate LL. Gastroenterol Clin North Am. 2005 Dec;34(4):643-64.

Diverticulosis

Diverticular Bleeding

Urgent Colonoscopy for the Diagnosis and Treatment of Severe Diverticular
Hemorrhage
• 121 pts with severe bleeding (>4 hrs after hospitalization)
• 1st 73 pts: no colonoscopic tx
• Last 48 pts eligible for colonoscopic tx
• Colonoscopy w/in 6-12 hrs

Urgent Colonoscopy for the Diagnosis and Treatment of Severe Diverticular Hemorrhage
Jensen DM, et al. New Eng J Med 2000:342:78-82.

Ischemic Colitis
• Most common form of intestinal ischemia
• Transient and reversible
• Abdominal pain• Watershed areas
– Splenic flexure– Rectosigmoid junction

Hemorrhoids

Bleeding AVM

Radiation Proctitis

• Incidence 0.3 - 3.0 %• Etiology Incomplete obliteration of
the vitelline duct.• Pathology50% ileal, 50% gastric,
pancreatic, colonic mucosa• Complications
– Painless bleeding (children, currant jelly)– Intussusception
Acute LGIBMeckel’s Diverticulum

Study Yield
% Comments
Colonoscopy 69-80 Therapeutic
Arteriography 40-78 1 ml/min,
risks
Tagged RBC Scan 20-72 Localization
Acute LGIBEvaluation
Zuccaro. ASGE Clinical Update. 1999.

• Annual incidence of hospitalization: – 20-30/100,000 persons
• Resuscitation• Exclude an UGI source• Most bleeding ceases• Colonoscopy• No role for barium studies
Acute LGIBKey Points