GASTRO INTESTINAL TRACT PHARMACOLOGY - 2
description
Transcript of GASTRO INTESTINAL TRACT PHARMACOLOGY - 2

GASTRO INTESTINAL TRACT PHARMACOLOGY - 2
LECTURE 8

The Gastrointestinal Tract
•Gastroesophageal Reflux Disease (GERD)•Peptic Ulcer Disease (PUD)•Duodenal Ulcer•Nausea•Emesis•Diarrhea•Constipation•IBS

Vomiting
• The act of vomiting and the sensation of nausea that accompanies it are protective reflexes that serve to rid the stomach and intestine of toxic substances and prevent their further ingestion
• Vomiting or throwing up is forcing the contents of the stomach up through the esophagus and out of the mouth.
• Nausea is the feeling of having an urge to vomit. It is often called being sick to your stomach.

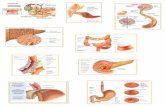
Vomiting Centre (medulla)
StomachSmall intestine
Higher cortical centres
Chemoreceptor Trigger Zone
(area prostrema, 4th ventricle)
Memory, fear, anticipationSensory input (pain, smell, sight)
SurgerySurgery
Labyrinths
Anaesthetics
Vomiting Reflex
Neuronal pathways
Factors which can cause nausea & vomiting
Chemotherapy
Chemotherapy
Radiotherapy
Opioids
Sites of action of drugs
5HT3antagonists
Sphincter modulators
Histamine antagonistsMuscarinic antagonists
Gastroprokinetic agents
BenzodiazepinesHistamine antagonistsMuscarinic antagonistsDopamine antagonists
Cannabinoids

Vomiting Centre (medulla)
Cerebral cortex
Anticipatory emesisSmellSight
Thought
Vestibular nucleiMotion
sickness
Pharynx & GIT
Chemo & radio therapy Gastroenteritis
(vagus)
Chemoreceptor Trigger Zone
(CTZ)(Outside BBB)
Cancer chemotherapyOpioids
Muscarinic, 5 HT3 & Histaminic H1
5 HT3 receptors
Dopamine D2
5 HT3,,Opioid Receptors
Muscarinic Histaminic H1
Pathophysiology of Emesis

Indications of antiemetics
1- Chemotherapy-induced vomiting2- Post irradiation vomiting3- Postoperative vomiting4- Vomiting of pregnancy5- Motion sickness

Group of drugs used as antiemetics
Serotonin 5 HT3 Antagonists:
Dopamine D2 Antagonist:
Anticholinergics:
H1 Antihistaminics

Serotonin 5 HT3 AntagonistPotent antiemetics
Mechanism of action:1- Peripheral 5-HT3 receptor blockade on intestinal vagal afferents. 2- Central 5-HT3 receptor blockade in the vomiting center and chemoreceptor trigger zone
Antiemetic action is mainly against:Emesis mediated by vagal stimulation (e.g. postoperative and chemotherapy)
High first pass metabolism
Excreted by liver & kidney
No dose reduction in renal insufficiency but needed in hepatic insufficiency

Drugs Available1. Ondansetron
2. Granisetron
3. Dolasetron
4. Palonosteron
Indications1) Chemotherapy induced nausea and vomiting
2) postradiation nausea & vomiting
3) Vomiting of pregnancy
4) Postoperative vomiting

Adverse EffectsThe most common adverse effects are:
1- Headache and dizziness
2- Constipation or diarrhoea

Corticosteroids
Corticosteroids have antiemetic properties Mechanism of action: possibly by suppressing
peritumoral inflammation and prostaglandin production.
Use: to enhance efficacy of 5HT3 receptor antagonists in the treatment of chemotherapy-induced vomiting.

Phenothiazines• Phenothiazines as promethazine are antipsychotic agents
• Use: • Chemotherapy-induced vomiting• Radiotherapy-induced vomiting• postoperative nausea and vomiting
• Mechanism of the antiemetic action: inhibition of central dopamine, muscarinic and H1 histamine receptors receptors

Butyrophenones• Butyrophenones as droperidole are antipsychotic agents• Mechanism of the antiemetic action: inhibition of central
dopamine receptors• Use: • Chemotherapy-induced vomiting• Radiotherapy-induced vomiting• postoperative nausea and vomiting• Adverse effects: droperidol may prolong the QT inter,
therefore, it should not be used in patients with QT prolongation (should only be used in patients who have not responded adequately to alternative agents).

Substituted Benzamides
• 1- Metoclopramide • 2- TrimethobenzamideMechanism of antiemetic action: Central
dopamine-receptor blockadeSide effects: (mainly extrapyramidal):1) Restlessness2) Dystonias3) Parkinsonian symptoms

H1 receptor antagonists and Anticholinergics
Use:prevention or treatment of motion sickness.Adverse effects: sedation, dizziness,confusion, dry mouth, cycloplegia,
and urinary retention.
.
Diphenhydramine dimenhydrinate
First generation H1 receptor blockers that have anticholinergic and sedating properties
Meclizine First generation H1 receptor blockers that have lesser anticholinergic and sedating properties
Hyoscine Muscarinic receptor blocker

Benzodiazepines
• Uses:• Benzodiazepines such as diazepam are used
prior to the initiation of chemotherapy to reduce anticipatory vomiting or vomiting caused by anxiety

Cannabinoids(Dronabinol)
• The mechanisms for the antiemetic effects is not known. • Pharmacokinetics.
readily absorbed after oral administration It undergoes extensive first-pass metabolism with limited systemic bioavailability after single doses Mmetabolites are excreted primarily via the biliary-fecal route
• Adverse effects include: 1. Euphoria or dysphoria, sedation and hallucinations 2. Abrupt withdrawal leads o withdrawal syndrome (restless, insomnia and
irritability)3. Autonomic effects (sympathetic) in the form of tachycardia, palpitation,
conjunctival injection, and orthostatic hypotension.• Use:
For the prevention of chemotherapy-induced nausea and vomiting

LAXATIVES• bulk laxatives
– =increasing the volume, not absorbed– methylcelulose, agar, psyllium seeds– no serious unwanted effects
• osmotic l.– not absorbed, osmosis - distension of colon– magnesium sulphate, magnesium hydroxide, lactulose– ADR: flatulence, cramps, diarhoea, electrolyte dist., tolerance
• stimulant l.– stimulation of enteric nerves - secretion, motility– bisacodyl, senna preparations– ! only for short-term use - nerve reduction

antidiarrhoeal agents I
• secretion, motility, decreased absorption• ! fluid and electrolyte balance - rehydration
• antiinfective agents…gastroenteritis– sever cases of Campylobacter - erythromycin,
ciprofloxacin
• antidiarrhoeal agents

antidiarrhoeal agents II• antimotility agents
– opiates, morphine - constipation, sphincter contraction– codeine, diphenoxylate, loperamide– ! drowsiness, dizziness, paralytic ileus
• adsorbents– adsorbing microorganisms and toxins– kaolin, pectin, charcoal

motility stimulants• = prokinetic drug• domperidone (Motilium) - D2 antagonist, also antiemetic
– oesophageal sphincter pressure…GERD– ! hyperprolactinemia
• metoclopramide (Paspertin) - DA antagonist and Ach agonist– increases gastric emptying - GERD– ! extrapyramidal side effects
• cisapride (Prepulsid) - 5-HT4 rec. agonist….Ach release– gut motility, no antiemetic action– withdrawn due to QT prolongation

Agents that increase GIT motility
1- Cholinergic agentsStimulate cholinergic receptors. Enhance contractions in an uncoordinated manner that produces no net propulsive activity. Not useful for treating motility disorders
2- Prokinetic agents enhance coordinated GIT propulsive motility. Prokinetic agents act at receptor sites on the motor neuron itself increasing the release of acetylcholine at the motor nerve terminal without interfering with the normal physiological pattern and rhythm of motility. Useful for treating motility disorders

Cholinergic Agents • Direct cholinergic agents • Stimulate cholinergic receptors in the wall of the GIT. 1- ACh is not used pharmacologically because:
it affects both nicotinic and muscarinic receptorsIt is degraded rapidly by acetylcholinesterase.
2- Bethanechol Muscarinic receptor agonist Resists enzymatic hydrolysis. In addition, it lacks real prokinetic efficacy,

Indirect cholinergic agents: Acetylcholinesterase Inhibitors. These drugs inhibit the degradation of ACh , allowing ACh to accumulate at sites of release.
Neostigmine has been used to treat paralytic ileus.

Inflammatory bowel disease
• Ulcerative colitis - diffuse mucosal inflammation - limited to colon - defined by location (eg proctitis;pancolitis)• Crohn’s disease - patchy transmural inflammation - fistulae; strictures - any part of GI tract - defined by location or pattern

Treatment options
1. Aminosalicylates2. Corticosteroids3. Thiopurines4. Ciclosporin5. Methotrexate6. Infliximab7. Surgery

Management of UC
• Acute to induce remission1. oral +- topical 5-ASA2. +- oral corticosteroids eg 40mg prednisolone3. Azathioprine (Chronic active)4. iv steroids/Colectomy/ ciclosporin (severe)
• Maintaining remission1. oral +- topical 5-ASA2. +- Azathioprine (frequent relapses)

Management of CD
• Acute to induce remission1. oral high dose5-ASA2. +- oral corticosteroids reducing over 8/523. Azathioprine (Chronic active)4. Methotrexate (intolerant of azathioprine)5. iv steroids/ metronidazole/elemental diet/surgery/infliximab• Maintaining remission1. Smoking cessation2. oral 5-ASA limited role3. +- Azathioprine (frequent relapses)4. Methotrexate (intolerant of azathioprine)5. Infliximab infusions (8 weekly)

ANTI CANCER AGENTS
NEXT LECTURE

THANK YOU