Gastro Intestinal Bleeding- Healthcare
-
Upload
baijayanti-nath -
Category
Healthcare
-
view
325 -
download
1
Transcript of Gastro Intestinal Bleeding- Healthcare
Slide 1
GASTRO INTESTINAL BLEEDINGSNDT WOMENS UNIVERSITY.L.T.COLLEGE OF NURSING.BAIJAYANTI NATH.M.SC. NURSING 1ST YEAR.
1
AIM &OBJECTIVES::AIM: After completion of the seminar the group will be able to understand the topic GIbleeding in a and can able to provide proper care to the GI bleeding patient.OBJECTIVES:At the end of the topic the group will be able to:Define GI bleeding.Identify upper and lower GI bleeding.Understand the etiology and pathophysiology of the GI bleeding.Classify the GI bleeding.Recognize the sign and symptoms of the upper and lower GI bleeding.Recognize the different diagnostic evaluation.Understand the medical ,surgical and nursing management of GI bleeding.
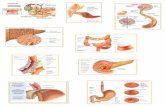
INTRODUCTIONGastrointestinal bleeding is among the most common gastrointestinal disorder.gi bleeding is not just a gestrodudenal disorder but may occur in anywhere in the alimentary tract. Bleeding is a symptom of upper and lower gi disorder. It may be oblivious in stool or occult(hidden).
DEFINITIONGastrointestinal bleeding(GI bleed), also known asgastrointestinal hemorrhage, is all forms ofbleedingin thegastrointestinaltract, from the mouth to the rectum. When there is significantbloodloss over a short time, symptoms may include vomiting redblood, vomiting blackblood, bloody stool, or black stool.
ETIOLOGY AND PATHOPHYSIOLOGYTrauma anywhere in the GI tract.Erosion or ulcer.Rupture of the enlarge vein.Inflammation and infection in alimentary tract.eg-esophegitis,gastritis etcalcohol and drug consumption.eg-NSAID aspirin containing compounds, anticuagulent.Vascular lesion disorder.Anal disorder.
CLASSIFICATION OF GI BLEEDING:
Upper GI Tract BleedingProximal to the Ligament of Treitz 70% of GI BleedsLower GI Tract bleedingDistal to the Ligament of Treitz 30% of GI Bleeds
UPPER GI BLEEDING:
UPPER GI bleeding is defined as bleeding from gastrointestinal tract proximal to ligament of Trietz. It usually manifests as hematemesis or melena, and when severe, may even lead to hematochezia.Clinical guidelines are recommended to predict out -come, including rebleeding, and mortality.Stigmata of a recent hemorrhge are endoscopic finding that predict outcome.
INCIDENCE:
170 patients/ 100,000 population /year.40% due to peptic ulcer(Most common). 80% are self-limited.
RISK FACTORS
NSAID useH. pylori infectionIncreased ageUpper GI Bleeding accounts for approximately 350,000 hospitalizations per year.
ETIOLOGY OF UPPER BLEEDS
Duodenal Ulcer-30%Gastric Ulcer-20%Varices-10%(Vague right upper quadrant pain, fever, nausea, vomiting, ascites, edema.Features of hepatic failures )Gastritis and duodenitis-5-10%Esophagitis-5%Mallory Weiss Tear-3%GI Malignancy-1%Dieulafoy LesionAV Malformation-angiodysplasia
SIGNS AND SYMPTOMS
Signs and symptoms of acute upper GI bleeding[1]include the following:Features due to blood loss :1.Haemetemesis,malena or haematochezia , Hyperactive bowel sound. 2.H/O CLD presenting with shock.3. H/O ESRD with sudden derange RFTs.4. Features of co-morbid illnesses - IHD, COPD, CHF,SEPTICEMIA,PT ON VENTILLATORY SUPPORT.On evaluation:1. Anemia2.Orthostatic changes of BP and HR 3.Shock
OTHERS:
HematemesisMelenaHematocheziaSyncopePresyncopeDyspepsiaEpigastric painHeartburnDiffuse abdominal painDysphagiaWeight lossJaundice
DIAGNOSISHISTORYEXAMINATIONEMERGENCY ENDOSCOPY???
History Helpful to find out the site and causeHistory suggestive of acid peptic diseaseAlcoholic liver diseases / chronic hepatitis / CirrhosisHistory of anticoagulant / anti platelets / NSAIDS / Alcohol binge intake / steroidsHistory of Coagulation disorder / Blood Dyscrasias History of Epistaxis or Hemoptysis to rule out the GI source of bleedingPatients of CVA, BURN, Sepsis, Head Trauma may have stress ulcers
ON EXAMINATIONVITALSPulse = Thready,BP = Orthostatic HypotensionSKIN changesCirrhosis Palmer- erythema, spider angiomaBleeding diasthasis Purpura /EchymosisCoagulation Disorder Haemarthrosis, Muscle HematomaENT :- Look for clots (To rule out epistaxis P.N BLEED)P/A :- Liver , Spleen, Caput Medusa = CirrhosisEpigastric Tenderness = APD/ UlcerRespiratory, CVS, CNS For comorbid diseses
Diagnostic WorkupCBC
Bleeding &Coagulation profile (BT, CT,PT, a PTT)
Liver Function Test
Complete S. Biochemistry
Relevant lab test for underlying disease
BLOOD INV.ENDOSCOPYRADIO-IMAGING Barium Meal F.T.
Arteriography
USG/ Doppler USG
Radio nucleotide study (Tagged RBC scan)
Objectives in Acute GI bleeding:
AUGIBRapid AssessmentMonitor Hemodynamic StatusFluid ResuscitationRyle;s tube for Gastric Lavage
Self Limited Hemorrhage (80%)Continued bleeding (10-25%)Urgent endoscopyRecurrent HemorrhageElective Endoscopy (With in 24 48 hours)Definitive Therapy(If Necessary)Site not localizedLocalizedFurther Assessment (Extended EGD, Radio-isotope scan, Arteriography, Exploratory Laprotomy) Definitive Therapy
MANAGEMENTEndoscopic therapy: the goal of endoscopic therapy is to coagulate or thromboses the blood vessels the blood vessels.It is mainly useful to stop bleeding in patient with sever gastritis varises peptic ulcer,polyps,several techniques are used, including-Thermal probeMultipolar bipolar electrocuagulation probe.Argon plasma coagulation.Neodymium:yttrium-aluminium-garnet-laser.
Identify bleeding source(Pre- requisites for endoscopy):Bloody endoscopy field1. Naso-gastric tube(RT. esp. Wide bore) coffee coloured/clots/fresh blood aspirate may categorize these pts- Low/ Intermediate/High
2. Gastric Lavage saline with or without H2O2 prokinetic(erythromycin, metchlopromide) agents may be used. color and rapidity of clearing: clear fluid indicates absence of GH and pt may be subjected for endoscopy. 3. Risk of aspiration (insure airway/ E.T tube).Sleisenger and Fordtran's Gastrointestinal and Liver Disease Ninth Edition
NASOGASTRIC LAVAGEBenefits of lavage :Better visualization during endoscopy.Give crude estimation of rapidity of bleeding.Prevent the development of porto systemic encephalopathy in cirrhosis.Increases PH of stomach and hence decreases clot desolution due to gastric acid dilution During gastric lavage use saline and not use large volume of to avoid water intoxication.Gastric lavage should be done in alert and cooperative patient to avoid broncho-pulmonary aspiration
NASOGASTRIC LAVAGEIf gastric aspirate either is grossly bloody or yields coffee ground effort should be made to lavage the stomach before proceeding to diagnostic or therapeutic endoscopy. The presence of bloody gastric aspirate confirms UGI Bleed. A negative aspirate (16%) does not exclude an upper bleeding. For Example in case of duodenal ulcer due to absence of duodenogastric reflux aspirate is clear
MEDICAL THERAPYepinephrine during endoscopy is effective for acute hemostasis.epinephrine produces tissue edema and ultimately, pressure on the bleeding. To prevent rebleeding,injection therapy is often combined with other therapies.For variceal bleeding-vasoprasin used to produce vasoconstriction. It is used in those patient who do not respond to other therapies and are poor surgical risks. It is administered systematically in IV or intra-arterial route.Histamine receptor blockers or protons pump inhibitors are administers to decrease acid secretion.eg-renitidine,cimetidine.Eg-omeprazole ,pentoprazole.Antacids are used to nutrilizes the HCI .eg magnesium hydroxide,calciumhydroxide,sodium bicarbonate etc.Sedatives are sometimes used in restless patient.
Surgical therapy:
26
Etiology:
28
Dirverticular diseases
What is Diverticulosis?
Most common siteDiverticula can occur throughout the colon but are most common near the end of the left colon referred to as the sigmoid colon.
Risk factors
increasing age constipation a diet that is low in dietary fiberhigh intake of meat and red meat connective tissue disorders (such as Mara fan syndrome) that may cause weakness in the colon wall hereditary or genetic predisposition
What are the symptoms of diverticular disease?
Most patients with diverticulosis have few or no symptoms. The most common symptoms of diverticular disease include:abdominal cramping,constipation, anddiarrhea. These symptoms are related to difficulty in passing stool through the left colon, which is narrowed by diverticular disease.
Complication:The most common complication is diverticulitis which is a condition in which diverticuli in the colon rupture. Which results in infection in the tissues that surround the colon bleeding.Abscess, Perforation, and PeritonitisFistula
DIAGNOSIS:
Colonoscopy Barium X-rays (barium enemas) can be performed to visualize the colon. Diverticula are seen as barium filled pouches protruding from the colon wall.ultrasound and CT scan examinations of the abdomen and pelvis can be done to detect collections of pus.
Inflammatory bowel disease
Ulcerative colitisIs a form of inflammatory bowel disease, characterized by inflammation with ulcer formation in the lining of colon.
Site of involvment
Inflammation of the distal terminal ileum may occur
Bleeding per rectum.- Diarrhea (bloody diarrhea) with mucous.- Tenesmus, when the disease is confined to the rectum.-Abdominal discomfort.- Remissions & exacerbations.Clinical pictureintestinal
Extra intestinal manifestations
Ischemic colitis
a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply.
Site of ischemia
( depend on severity of ischemia)1-abdominal pain2-rectal bleeding3-diarrhea4-fever.
Clinical picture
Hemorrhoids
Predisposing factors:
Constipation.
Sitting for long periods of time.
Obesity.
Heavy Lifting.
48
Clinical Presentation :
Patients commonly present to a physician for two main reasons: Bleeding.
Protrusion.
Pain.
Anal Itching.
Diagnosis:
Mainly during the physical examination by: Inspection of the perianal region, with careful digital examination.AnoscopyStaging.
Angiodyplasia
It is a tourtious dilatations of submucosal and mucosal blood vessels are seen most often in the cecum or right colon
Neoplasm Neoplastic bleeding can be from a polyp or carcinoma.Colon cancer is the predominant cause of neoplastic bleeding and is responsible for around 10% of rectal bleeding in patients older than 50 years. The bleeding is usually low-grade and recurrent, occurring as a result of mucosal ulceration or erosion. Though neoplastic bleeding can present as bright red blood per rectum, it is unusual for it to cause massive colonic bleeding.
Coagulopathy(also calledclotting disorderandbleeding disorder) is a condition in which the bloods ability to clot is impaired. This condition can cause prolonged or excessive bleeding, which may occur spontaneously or following an injury or medical procedures.
DIAGNOSIS Despite improvement in diagnostic imaging & procedures, 10-20% of pts with Lower GIT bleeding have no demonstrable bleeding source.
Therefore, this complex problem requires systematic evaluation.
A- Initial EvaluationPatient's history: -aspirin, vascular disease, past bleeding episodes, liver cirrhosis, IBD, coagulopathy. -duration, frequency, stool colour.
Digital rectal examination Physical examination to assess the severity of bleeding: -HR , BP, postural changes.
B- Laboratory Tests
CBC ESR/ CRP
Coagulation profile
Liver function tests
Renal function tests
C- EndoscopyColonoscopy: Esophagogastroduodenoscopy:Small Bowel Visualization
Angiography
Performed after colonoscopy has failed to identify a bleeding site ,can detect bleeding at a rate of more than 0.5 mL/min.
In a patient with active GI bleeding, the radiologist first cannulates the superior mesenteric artery, because most of the hemodynamically significant bleeding originates in the right colon. The extravasation of contrast material indicates a positive study finding. If the findings from the study are negative, the inferior mesenteric artery is cannulated, followed by the celiac artery.
Once the bleeding point is identified,angiography offers potential treatment options,such as selective vasopressin drip and embolization.
E. Barium EnemaF. Abdominal Radiography /CT
Resuscitation and initial assessment.Localization of the bleeding site.Therapeutic intervention to stop bleeding at the site.
1) Resuscitation and Initial Assessment:
IV access and administration of normal saline. Rapid assessment of vital signs, including heart rate, blood pressure, pulse pressure, and urine output.Routine laboratory studies (CBC, electrolyte levels, and coagulation studies), blood should be typed and cross-matched. The patient's blood loss and hemodynamic status should be evaluated, and in cases of severe bleeding, the patient may require invasive hemodynamic monitoring .
Patients in shock should receive fluid volume replacement without delay. Colloid or crystalloid solutions may be used to achieve volume restoration before administering blood products. Red cell transfusion should be considered after loss of 30% of the circulating volume.
2) Localization of the Bleeding Site
In patients who are hemo-dynamically stable with mild to moderate bleeding or in patients who have had a massive bleed that has stabilized, colonoscopy should be performed initially. Once the bleeding site is localized, therapeutic options include coagulation and injection with vasoconstrictors or sclerosing agents. In cases of diverticular bleeding, bipolar probe coagulation, epinephrine injection, and metallic clips may be used. If recurrent bleeding is present, the affected bowel segment can be resected. In cases of angiodysplasia, thermal therapy, such as electro-coagulation or argon plasma coagulation, is generally successful.
3) Therapeutic intervention to stop bleeding at the site.
:Colonoscopy Colonoscopy is useful in radiation therapyinduced gastrointestinal (GI) bleeding and in the treatment of colonic polyp lesions. Endoscopic treatment of radiation-induced bleeding includes topical application of formalin, Nd:YAG laser therapy, and argon plasma coagulation. Neoplastic bleeding due to polyps requires polypectomy. Patients diagnosed with colonic tumors may require surgical resection.
Vasoconstrictive Therapy :In patients in whom the bleeding site cannot be determined based on colonoscopy and in patients with active LGIB, angiography with or without a preceding radionuclide scan should be performed to locate the bleeding site as well as to intervene therapeutically. Initially, Vasoconstrictive agents, such as vasopressin, epinephrine, propranolol can be used. Vasoconstriction reduces the blood flow and facilitates plug formation in the bleeding vessel. Although epinephrine and propranolol reduced mesenteric blood flow, they also caused a rebound increase in blood flow and recurrent bleeding.
Vasopressin causes severe vasoconstriction in the splanchnic bed. Vasopressin infusions are more effective in diverticular bleeding, which is arterial, as opposed to angiodysplastic bleeding, which is of the venocapillary type. Intra-arterial vasopressin infusions begin at a rate of 0.2 U/min, with repeat angiography performed after 20 minutes. The bleeding stops in about 91% of patients receiving intra-arterial vasopressin.If bleeding persists, the rate of the infusion is increased to 0.4-0.6 U/min. Once the bleeding is controlled, the infusion is continued in an intensive care setting for 12-48 hours and then tapered over the next 24 hours.
Superselective Embolization:
This therapeutic modality is useful in patients in whom vasopressin is unsuccessful or contraindicated.Embolization involves superselective catheterization of the bleeding vessel to minimize necrosis. Embolization with agents such as gelatin sponge, coil springs, polyvinyl alcohol, and oxidized cellulose. It is performed using a 3 French (F) microcatheter placed coaxially through the diagnostic 5F catheter.Once the bleeding vessel is identified, microcoils are used to occlude the bleeding vessel.Although microcoils are most commonly used, polyvinyl alcohol and Gelfoam are also used alone or in conjunction with microcoils.
Complications:Colonic infarction, bowel wall injury, Intestinal ischemia and infarction.To prevent this complication, perform embolization as close as possible to the bleeding point in the terminal arteries.
ENOSCOPIC THERAPYEndoscopic control of hemorrhage is suitable for GI polyps and cancers, arteriovenous malformations, mucosal lesions, postpolypectomy hemorrhage, endometriosis, colonic and rectal varices.It can be achieved using thermal modalities or sclerosing agents.Absolute alcohol, morrhuate sodium, and sodium tetradecyl sulfate can be used for sclerotherapy of lower GI lesions.Endoscopic epinephrine injection is used commonly because of its low cost, easy accessibility, and low risk of complications.
Surgery
Emergent surgery is required in patients with (LGIB) if non operative management is unsuccessful. Indications of Surgery :Persistent hemodynamic instability with active bleeding.Persistent, recurrent bleeding.Transfusion of more than 4 units packed red bloods cells in a 24-hour, with active or recurrent bleeding.No contraindications exist with regard to surgery in hemodynamically unstable patients with active bleeding.
Segmental bowel resection and subtotal colectomy
Segmental bowel resection following precise localization of the bleeding point is a well-accepted surgical practice in hemodynamically stable patients. Subtotal colectomy is the procedure of choice in patients who are actively bleeding from an unknown source.Patients who are hemodynamically stable should have preoperative localization of the bleeding; once it is localized, intra-arterial vasopressin is used as a temporizing measure to reduce the bleeding before patients undergo segmental colectomy.If the it is not localized, a subtotal colectomy with ileoproctostomy is performed.
ComplicationsThe most common early postoperative complications are intra-abdominal bleeding, mechanical bowel obstruction, intra-abdominal sepsis, localized or generalized peritonitis, wound infection and/or dehiscence.
Intra-abdominal sepsis following colorectal surgery is a life-threatening complication and requires aggressive resuscitation.Systemic conditions (eg, severe blood loss and shock, poor bowel preparation, diabetes, malnutrition, hypoalbuminemia) may adversely affect anastomotic healing.
Changes in anatomy and physiology of the large bowel, high bacterial content, improper operative technique, and ischemia can cause anastomotic leak associated with abscess and intra-abdominal sepsis.
Delayed complications usually occur more than 1 week after surgery, the most common of which are anastomotic stricture, incisional hernia, and incontinence.
Nursing management of GI bleeding:
Nursing assessment:
Nursing Diagnosis:
Fluid volume deficit related to acute loss of blood, as well as gastric secretions.Ineffective tissue perfusion related to loss of circulatory volumeAnxiety related to upper to upper GI bleeding,hospitalization,source of bleeding.Decrease cardiac output related to blood loss.Risk for aspiration related to active blreeding
Impact of anticoagulation on rebleedings:
Anticoagulation should be stopped immediately.The prescence of mild to mod anticoagulation(INR 1.3-2.7) did not appear to alter the outcomes of endoscopic therapy.Patients who require an antiplatelet medication and have a history of ulcer bleeding will have less chance of recurrent bleeding if they take aspirin 81mg and a PPI daily compared with clopidogrel alone.
OTHER INTERVENTION
Vitals are monitoredAssessment of severity of blood loss :- An orthostatic decrease of 20 mm Hg in systolic blood pressure or increases in the pulse of 20 beats / min. indicate 10% blood loss, if pt is pulsless and in shock- > 20% loss.Order hemoglobin, hematocrit, BUN, grouping and cross matching of blood.Insertion of central venous line may be beneficial to measure adequacy of fluid replacement and perfusion of vital organ . Monitor urine output.Fluid resuscitation is done by crystalloids such as normal saline or RL if hypoalbuminemia is detected use colloids.Placing the patient in trendelenburg position to maintaine cerebral blood flow.
CONT1.Oxygen support to prevent hypoxia of tissues2.IV route - Crystaloid solution/Colloids|blood.3. Blood transfusion:maintain Hct at 30% in the elderly, esp. with comorbid deseases eg. CHF, CRF, IHD,COPD) 20-25% in younger pt 25-28% in portal HTNadministration of vit k4.In symptomatic thrombocytopenia (