Gastric Cancer
-
Upload
victor-aguilar-morocho -
Category
Documents
-
view
266 -
download
3
Transcript of Gastric Cancer

Gastric CancerElwyn C Cabebe, MD, Adjunct Clinical Faculty, Department of Internal Medicine, Division of Medical Oncology, Stanford University School of MedicineVivek K Mehta, MD, Radiation Oncologist, Director, Center for Advanced Targeted Radiotherapies, Department of Radiation Oncology, Swedish Cancer Institute, Seattle, Washington; George Fisher, MD, PhD, Associate Professor, Department of Internal Medicine, Division of Medical Oncology, Stanford University School of Medicine
Updated: Dec 7, 2010
Introduction
Background
Gastric cancer was once the second most common cancer in the world. In most developed countries,
however, rates of stomach cancer have declined dramatically over the past half century. In the
United States, stomach malignancy is currently the 14th most common cancer.
Decreases in gastric cancer have been attributed in part to widespread use of refrigeration, which
has had several beneficial effects: increased consumption of fresh fruits and vegetables; decreased
intake of salt, which had been used as a food preservative; and decreased contamination of food by
carcinogenic compounds arising from the decay of unrefrigerated meat products. Salt and salted
foods may damage the gastric mucosa, leading to inflammation and an associated increase in DNA
synthesis and cell proliferation. Other factors likely contributing to the decline in stomach cancer
rates include lower rates of chronic Helicobacter pylori infection, thanks to improved sanitation and
use of antibiotics, and increased screening in some countries.[1 ]
Nevertheless, gastric cancer is still the second most common cause of cancer-related death in the
world, and it remains difficult to cure in Western countries, primarily because most patients present
with advanced disease. Even patients who present in the most favorable condition and who undergo
curative surgical resection often die of recurrent disease. However, 2 studies have demonstrated
improved survival with adjuvant therapy: a US study using postoperative chemoradiation[2 ]and a
European study using preoperative and postoperative chemotherapy.[3 ]
Anatomic aspects

The molecular biology responsible for carcinogenesis, tumor biology, and response to therapy in
stomach cancer are active areas of investigation but are not addressed in this review. Instead, this
article focuses on clinical management, which first requires a thorough understanding of gastric
anatomy.
An image depicting stomach anatomy can be seen below.
Stomach and duodenum, coronal section.

The stomach begins at the gastroesophageal junction and ends at the duodenum. The stomach has
3 parts: the uppermost part is the cardia; the middle and largest part is the body, or fundus; and the
distal portion, the pylorus, connects to the duodenum. These anatomic zones have distinct histologic
features. The cardia contains predominantly mucin-secreting cells. The fundus contains mucoid cells,
chief cells, and parietal cells. The pylorus is composed of mucus-producing cells and endocrine cells.
The stomach wall is made up of 5 layers. From the lumen out, the layers include the mucosa, the
submucosa, the muscularis layer, the subserosal layer, and the serosal layer. The peritoneum of the
greater sac covers the anterior surface of the stomach. A portion of the lesser sac drapes posteriorly
over the stomach. The gastroesophageal junction has limited or no serosal covering. The right
portion of the anterior gastric surface is adjacent to the left lobe of the liver and the anterior
abdominal wall. The left portion of the stomach is adjacent to the spleen, the left adrenal gland, the
superior portion of the left kidney, the ventral portion of the pancreas, and the transverse colon.
The site of stomach cancer is classified on the basis of its relationship to the long axis of the
stomach. Approximately 40% of cancers develop in the lower part, 40% in the middle part, and 15%
in the upper part; 10% involve more than one part of the organ. Most of the decrease in gastric
cancer incidence and mortality in the United States has involved cancer in the lower part of the
stomach; the incidence of adenocarcinoma in the cardia has actually shown a gradual increase.
Pathophysiology
Ooi et al identified 3 oncogenic pathways that are deregulated in the majority (>70%) of gastric
cancers: the proliferation/stem cell, NF-kappa β, and Wnt/beta-catenin pathways. Their study
suggests that interactions between these pathways may play an important role in influencing disease
behavior and patient survival.[4 ]
Understanding the vascular supply of the stomach allows understanding of the routes of
hematogenous spread. The vascular supply of the stomach is derived from the celiac artery. The left
gastric artery, a branch of the celiac artery, supplies the upper right portion of the stomach. The
common hepatic artery branches into the right gastric artery, which supplies the lower portion of the
stomach, and the right gastroepiploic branch, which supplies the lower portion of the greater
curvature.
Understanding the lymphatic drainage can clarify the areas at risk for nodal involvement by cancer.
The lymphatic drainage of the stomach is complex. Primary lymphatic drainage is along the celiac
axis. Minor drainage occurs along the splenic hilum, suprapancreatic nodal groups, porta hepatis,
and gastroduodenal areas.
Frequency
United States
The American Cancer Society estimates that 21,130 cases of gastric cancer will be diagnosed in
2009 (12,820 in men, 8,310 in women) and that 10,620 persons will die of the disease.[5 ]Gastric
cancer is the seventh leading cause of cancer deaths.
International
Once the second most common cancer worldwide, stomach cancer has dropped to fourth place, after
cancers of the lung, breast, and colon and rectum. However, stomach cancer remains the second
most common cause of death from cancer. The American Cancer Society estimates that in 2007
there were an estimated one million new cases, nearly 70% of them in developing countries, and
about 800,000 deaths.[1 ]

Tremendous geographic variation exists in the incidence of this disease around the world. Rates of
the disease are highest in Asia and parts of South America and lowest in North America.[1 ]The
highest death rates are recorded in Chile, Japan, South America, and the former Soviet Union.
Mortality/Morbidity
The 5-year survival rate for curative surgical resection ranges from 30-50% for patients with stage II
disease and from 10-25% for patients with stage III disease. Because these patients have a high
likelihood of local and systemic relapse, some physicians offer them adjuvant therapy. The operative
mortality rate for patients undergoing curative surgical resection at major academic centers is less
than 3%.
A review of 8 trials by Rothwell et al found allocation to aspirin reduced death caused by cancer.
Individual patient data were available from 7 of the 8 trials. Benefit was apparent after 5 years of
follow-up. The 20-year risk of cancer death was also lower in the aspirin group for all solid cancers. A
latent period of 5 years was observed before risk of death was decreased for esophageal,
pancreatic, brain, and lung cancers. A more delayed latent period was observed for stomach,
colorectal, and prostate cancer. Benefit was only seen for adenocarcinomas in lung and esophageal
cancers. The overall effect on 20-year risk of cancer death was greatest for adenocarcinomas.[6 ]
Race
The rates of gastric cancer are higher in Asian and South American countries than in the United
States. Japan, Chile, and Venezuela have developed a very rigorous early screening program that
detects patients with early stage disease (ie, low tumor burden). These patients appear to do quite
well. In fact, in many Asian studies, patients with resected stage II and III disease tend to have better
outcomes than similarly staged patients treated in Western countries. Some researchers suggest that
this reflects a fundamental biologic difference in the disease as it manifests in Western countries.
In the United States, Asian and Pacific Islander males and females have the highest incidence of
stomach cancer, followed by black, Hispanic, white, American Indian, and Inuit populations.
Sex
In the United States, gastric cancer affects slightly more men than women; the American Cancer
Society estimates that in 2009, 12,820 new cases will occur in men and 8,310 in women.[5 ]Worldwide, however, gastric cancer rates are about twice as high in men as in women.[1 ]
Age
Most patients are elderly at diagnosis. The median age for gastric cancer in the United States is 70
years for males and 74 years for females. The gastric cancers that occur in younger patients may
represent a more aggressive variant or may suggest a genetic predisposition to development of the
disease.
Clinical
History
In the United States, about 25% of stomach cancer patients present with localized disease, 31%
present with regional disease, and 32% present with distant metastatic disease; the remainder of
cases surveyed were listed as unstaged.
Early disease has no associated symptoms; however, some patients with incidental complaints are
diagnosed with early gastric cancer. Most symptoms of gastric cancer reflect advanced disease.

Patients may complain of indigestion, nausea or vomiting, dysphagia, postprandial fullness, loss of
appetite, melena, hematemesis, and weight loss.
Late complications include pathologic peritoneal and pleural effusions; obstruction of the gastric
outlet, gastroesophageal junction, or small bowel; bleeding in the stomach from esophageal varices
or at the anastomosis after surgery; intrahepatic jaundice caused by hepatomegaly; extrahepatic
jaundice; and inanition resulting from starvation or cachexia of tumor origin.
Physical
All physical signs are late events. By the time they develop, the disease is almost invariably too far
advanced for curative procedures.
Signs may include a palpable enlarged stomach with succussion splash; hepatomegaly; periumbilical
metastasis (Sister Mary Joseph nodule); and enlarged lymph nodes such as Virchow nodes (ie, left
supraclavicular) and Irish node (anterior axillary). Blumer shelf (ie, shelflike tumor of the anterior
rectal wall) may also be present. Some patients experience weight loss, and others may present with
melena or pallor from anemia.
Paraneoplastic syndromes such as dermatomyositis, acanthosis nigricans, and circinate erythemas
are poor prognostic features.
Other associated abnormalities also include peripheral thrombophlebitis and microangiopathic
hemolytic anemia.
Causes
Gastric cancer may often be multifactorial, involving both inherited predisposition and environmental
factors.[7 ]Environmental factors implicated in the development of gastric cancer include diet,
Helicobacter pylori infection, previous gastric surgery, pernicious anemia, adenomatous polyps,
chronic atrophic gastritis, and radiation exposure.
Diet
A diet rich in pickled vegetables, salted fish, salt, and smoked meats correlates with an increased
incidence of gastric cancer.[7 ]
A diet that includes fruits and vegetables rich in vitamin C may have a protective effect. [8 ]
Smoking
Smoking is associated with an increased incidence of stomach cancer in a dose-dependent manner,
both for number of cigarettes and for duration of smoking.
Smoking increases the risk of cardiac and noncardiac forms of stomach cancer.[9 ]Cessation of
smoking reduces the risk.
A meta-analysis of 40 studies estimated that the risk was increased by approximately 1.5- to 1.6-fold
and was higher in men.[10 ]
Helicobacter pylori infection
Chronic bacterial infection with H pylori is the strongest risk factor for stomach cancer.

H pylori may infect 50% of the world's population, but many fewer than 5% of infected individuals
develop cancer. It may be that only a particular strain of H pylori is strongly associated with
malignancy, probably because it is capable of producing the greatest amount of inflammation. In
addition, full malignant transformation of affected parts of the stomach may require that the human
host have a particular genotype of interleukin (IL) to cause the increased inflammation and an
increased suppression of gastric acid secretion. For example, IL-17A and IL-17F are inflammatory
cytokines that play a critical role in inflammation. Wu et al found that carriage of IL-17F 7488GA and
GG genotypes were associated with an increased risk of gastric cancer.[11 ]
H pylori infection is associated with chronic atrophic gastritis, and patients with a history of prolonged
gastritis have a sixfold increased risk of developing gastric cancer. Interestingly, this association is
particularly strong for tumors located in the antrum, body, and fundus of the stomach but does not
seem to hold for tumors originating in the cardia.[12 ]
Previous gastric surgery
Previous surgery is implicated as a risk factor. The rationale is that surgery alters the normal pH of
the stomach, which may in turn lead to metaplastic and dysplastic changes in luminal cells.[13 ]
Retrospective studies demonstrate that a small percentage of patients who undergo gastric polyp
removal have evidence of invasive carcinoma within the polyp. This discovery has led some
researchers to conclude that polyps might represent premalignant conditions.
Genetic factors
Some 10% of stomach cancer cases are familial in origin.
Genetic factors involved in gastric cancer remain poorly understood, though specific mutations have
been identified in a subset of gastric cancer patients. For example, germline truncating mutations of
the E-cadherin gene (CDH1) are detected in 50% of diffuse-type gastric cancers, and families that
harbor these mutations have an autosomal dominant pattern of inheritance with a very high
penetrance.[14 ]
Other hereditary syndromes with a predisposition for stomach cancer include hereditary
nonpolyposis colorectal cancer, Li-Fraumeni syndrome, familial adenomatous polyposis, and Peutz-
Jeghers syndrome.
Epstein-Barr virus
The Epstein-Barr virus may be associated with an unusual (<1%) form of stomach cancer,
lymphoepithelioma-like carcinoma.
Pernicious anemia
Pernicious anemia associated with advanced atrophic gastritis and intrinsic factor deficiency is a risk
factor for gastric carcinoma.
Gastric ulcers
Gastric cancer may develop in the remaining portion of the stomach following a partial gastrectomy
for gastric ulcer.
Benign gastric ulcers may themselves develop into malignancy.

Obesity
Obesity increases the risk of gastric cardia cancer.
Radiation exposure
Survivors of atomic bomb blasts have had an increased rate of stomach cancer. Other populations
exposed to radiation may also have an increased rate of stomach cancer.
Bisphosphonates
A large cohort study examined whether use of oral bisphosphonates was associated with an
increased risk of esophageal or gastric cancers. No significant difference was observed for increased
risk of esophageal or gastric cancers between the bisphosphonate cohort and the control group.[15 ]
Differential Diagnoses
Esophageal Cancer Gastroenteritis, Bacterial
Esophageal Stricture Gastroenteritis, Viral
Esophagitis Lymphoma, Non-Hodgkin
Gastric Ulcers Malignant Neoplasms of the Small Intestine
Gastritis, Acute
Gastritis, Atrophic
Gastritis, Chronic
Workup
Laboratory Studies
The goal of obtaining laboratory studies is to assist in determining optimal therapy.
A CBC count can identify anemia, which may be caused by bleeding, liver dysfunction, or poor
nutrition. Approximately 30% of patients have anemia.
Electrolyte panels and liver function tests also are essential to better characterize the patient's
clinical state.
Carcinoembryonic antigen (CEA) is increased in 45-50% of cases.
Cancer antigen (CA) 19-9 is elevated in about 20% of cases.
Imaging Studies
Esophagogastroduodenoscopy has a diagnostic accuracy of 95%. This relatively safe and simple
procedure provides a permanent color photographic record of the lesion. This procedure is also the
primary method for obtaining a tissue diagnosis of suspected lesions. Biopsy of any ulcerated lesion
should include at least 6 specimens taken from around the lesion because of variable malignant
transformation. In selected cases, endoscopic ultrasound may be helpful in assessing depth of
penetration of the tumor or involvement of adjacent structures.
Double-contrast upper GI series and barium swallows may be helpful in delineating the extent of
disease when obstructive symptoms are present or when bulky proximal tumors prevent passage of
the endoscope to examine the stomach distal to an obstruction (more common with

gastroesophageal [GE]-junction tumors). These studies are only 75% accurate and should for the
most part be used only when upper GI endoscopy is not feasible.
Chest radiograph is done to evaluate for metastatic lesions.
CT scan or MRI of the chest, abdomen, and pelvis assess the local disease process as well as
evaluate potential areas of spread (ie, enlarged lymph nodes, possible liver metastases).
Endoscopic ultrasound allows for a more precise preoperative assessment of the tumor stage.
Endoscopic sonography is becoming increasingly useful as a staging tool when the CT scan fails to
find evidence of T3, T4, or metastatic disease. Institutions that favor neoadjuvant chemoradiotherapy
for patients with locally advanced disease rely on endoscopic ultrasound data to improve patient
stratification.
Histologic Findings
Adenocarcinoma of the stomach constitutes 90-95% of all gastric malignancies. The second most
common gastric malignancies are lymphomas. Gastrointestinal stromal tumors formerly classified as
either leiomyomas or leiomyosarcomas account for 2% of gastric neoplasms (see Gastric Stromal
Tumors). Carcinoids (1%), adenoacanthomas (1%), and squamous cell carcinomas (1%) are the
remaining tumor histologic types.
Adenocarcinoma of the stomach is subclassified according to histologic description as follows:
tubular, papillary, mucinous, or signet-ring cells, and undifferentiated lesions.
Pathology specimens are also classified by gross appearance. In general, researchers consider
gastric cancers ulcerative, polypoid, scirrhous (ie, diffuse linitis plastica), superficial spreading,
multicentric, or Barrett ectopic adenocarcinoma.
Researchers also employ a variety of other classification schemes. The Lauren system classifies
gastric cancer pathology as either Type I (intestinal) or Type II (diffuse). An appealing feature of
classifying patients according to the Lauren system is that the descriptive pathologic entities have
clinically relevant differences.
Intestinal, expansive, epidemic-type gastric cancer is associated with chronic atrophic gastritis,
retained glandular structure, little invasiveness, and a sharp margin. The pathologic presentation
classified as epidemic by the Lauren system is associated with most environmental risk factors,
carries a better prognosis, and shows no familial history.
The second type, diffuse, infiltrative, endemic cancer, consists of scattered cell clusters with poor
differentiation and dangerously deceptive margins. Margins that appear clear to the operating
surgeon and examining pathologist often are determined retrospectively to be involved. The
endemic-type tumor invades large areas of the stomach. This type of tumor is also not recognizably
influenced by environment or diet, is more virulent in women, and occurs more often in relatively
young patients. This pathologic entity is associated with genetic factors (such as E-cadherin), blood
groups, and a family history of gastric cancer.
Staging
The 2006 American Joint Committee on Cancer (AJCC) Cancer Staging Manual presents the
following TNM classification system for staging gastric carcinoma:[16 ]
Primary tumor

TX - Primary tumor (T) cannot be assessed
T0 - No evidence of primary tumor
Tis - Carcinoma in situ, intraepithelial tumor without invasion of lamina propria
T1 - Tumor invades lamina propria or submucosa
T2 - Tumor invades muscularis propria or subserosa
T3 - Tumor penetrates serosa (ie, visceral peritoneum) without invasion of adjacent
structures
T4 - Tumor invades adjacent structures
Regional lymph nodes
NX - Regional lymph nodes (N) cannot be assessed
N0 - No regional lymph node metastases
N1 - Metastasis in 1-6 regional lymph nodes
N2 - Metastasis in 7-15 regional lymph nodes
N3 - Metastasis in more than 15 regional lymph nodes
Distant metastasis
MX - Distant metastasis (M) cannot be assessed
M0 - No distant metastasis
M1 - Distant metastasis
Prognostic features
Two important factors influencing survival in resectable gastric cancer are depth of cancer invasion
through the gastric wall and presence or absence of regional lymph node involvement.
In about 5% of primary gastric cancers, a broad region of the gastric wall or even the entire stomach
is extensively infiltrated by malignancy, resulting in a rigid thickened stomach, termed linitis plastica.
Patients with linitis plastica have an extremely poor prognosis.[17 ]
Margins positive for presence of cancer are associated with a very poor prognosis.
The greater the number of involved lymph nodes, the more likely the patient is to develop local and
systemic failure after surgery.
In a study by Shen and colleagues,[18 ]the depth of tumor invasion and gross appearance, size, and
location of the tumor were 4 pathologic factors independently correlated with the number of
metastatic lymph nodes associated with gastric cancer.
Lee and colleagues found that surgical stage, as estimated during curative resection for gastric
cancer, complemented the pathologically determined stage for determining prognosis. Survival was
significantly poorer among patients with pathologic Stages II, IIIa, and IIIb disease in whom
intraoperative staging overestimated the extent of pathological stage.[19 ]
Staging
Stage 0 - Tis, N0, M0
Stage IA - T1, N0 or N1, M0
Stage IB - T1, N2, M0 or T2a/b, N0, M0
Stage II - T1, N2, M0 or T2a/b, N1, M0 or T2, N0, M0

Stage IIIA - T2a/b, N2, M0 or T3, N1, M0 or T4, N0, M0
Stage IIIB - T3, N2, M0
Stage IV - T1-3, N3, M0 or T4, N1-3, M0, or any T, any N, M1
Survival rates
Stage 0 - Greater than 90%
Stage Ia - 60-80%
Stage Ib - 50-60%
Stage II - 30-40%
Stage IIIa - 20%
Stage IIIb - 10%
Stage IV - Less than 5%.
Spread patterns
Cancer of the stomach can spread directly, via lymphatics, or hematogenously.
Direct extension into the omenta, pancreas, diaphragm, transverse colon or mesocolon, and
duodenum is common.
If the lesion extends beyond the gastric wall to a free peritoneal (ie, serosal) surface, then peritoneal
involvement is frequent.
The visible gross lesion frequently underestimates the true extent of the disease.
The abundant lymphatic channels within the submucosal and subserosal layers of the gastric wall
allow for easy microscopic spread.
The submucosal plexus is prominent in the esophagus and the subserosal plexus is prominent in the
duodenum, allowing proximal and distal spread.
Lymphatic drainage is through numerous pathways and can involve multiple nodal groups (eg,
gastric, gastroepiploic, celiac, porta hepatic, splenic, suprapancreatic, pancreaticoduodenal,
paraesophageal, and paraaortic lymph nodes).
Hematogenous spread commonly results in liver metastases.
Treatment
Surgical Care
Type of surgery
In general, most surgeons in the United States perform a total gastrectomy (if required for negative
margins), an esophagogastrectomy for tumors of the cardia and gastroesophageal junction, and a
subtotal gastrectomy for tumors of the distal stomach.
A randomized trial comparing subtotal with total gastrectomy for distal gastric cancer revealed similar
morbidity, mortality, and 5-year survival rates.[20 ]
Because of the extensive lymphatic network around the stomach and the propensity for this tumor to
extend microscopically, traditional teaching is to attempt to maintain a 5-cm surgical margin
proximally and distally to the primary lesion.

Lymph node dissection
The extent of the lymph node dissection is somewhat controversial.
Many studies demonstrate that nodal involvement indicates a poor prognosis, and more aggressive
surgical approaches to attempt to remove involved lymph nodes are gaining popularity.
Two randomized trials compared D1 (perigastric lymph nodes) with D2 (hepatic, left gastric, celiac,
and splenic arteries, as well as those in the splenic hilum) lymphadenectomy in patients who were
treated for curative intent. In the largest of these trials, postoperative morbidity (43% versus 25%)
and mortality (10% versus 4%) were higher in the D2 group.[21,22 ]
Most critics argue that these studies were underpowered and overestimated benefit. In addition, a
recent randomized trial found a much lower rate of complications than those earlier trials. Degiuli et
al reported complication rates of 17.9% and 12% with D2 and D1 dissections, respectively — a
statistically insignificant difference — and postoperative mortality rates of 2.2% and 3%, respectively.[23 ]
D2 dissections are recommended by the National Comprehensive Cancer Network over D1
dissections. A pancreas- and spleen - preserving D2 lymphadenectomy is suggested, as it provides
greater staging information, and may provide a survival benefit while avoiding its excess morbidity
when possible.
Outcome
The 5-year survival rate for a curative surgical resection ranges from 60-90% for patients with stage
I, 30-50% for patients with stage II disease, and 10-25% for patients with stage III disease.
Because these patients have a high likelihood of local and systemic relapse, some physicians offer
adjuvant therapy.
Consultations
Specialists recommend obtaining consultations freely in the management of most malignancies, and
gastric carcinoma is no exception. The gastroenterologist, surgical oncologist, radiation oncologist,
and medical oncologist work closely as a team.
Follow-up
Deterrence/Prevention
A diet that includes fruits and vegetables rich in vitamin C may have a protective effect.
Complications
Direct mortality rate within 30 days after a surgical procedure for gastric cancer has been reduced
substantially over the last 40 years. Most major centers report a direct mortality rate of 1-2%.
Early postoperative complications include anastomotic failure, bleeding, ileus, transit failure at the
anastomosis, cholecystitis (often occult sepsis without localizing signs), pancreatitis, pulmonary
infections, and thromboembolism. Further surgery may be required for anastomotic leaks.
Late mechanicophysiologic complications include dumping syndrome, vitamin B-12 deficiency, reflux
esophagitis, and bone disorders, especially osteoporosis.

Postgastrectomy patients often are immunologically deficient, as measured by blastogenic and
delayed cutaneous hypersensitivity responses.
Prognosis
Unfortunately, only a minority of patients with gastric cancer who undergo a surgical resection will be
cured of their disease. Most patients have a recurrence.
Patterns of failure
Several studies have investigated the patterns of failure after surgical resection alone. Studies that
depend solely on the physical examination, laboratory studies, and imaging studies may
overestimate the percentage of patients with distant failure and underestimate the incidence of local
failure, which is more difficult to detect.
A reoperation series from the University of Minnesota may offer a more accurate understanding of
the biology of the disease. In this series of patients, researchers surgically reexplored patients 6
months after the initial surgery and meticulously recorded the patterns of disease spread. The total
local-regional failure rate approached 67%. The gastric bed was the site of failure in 54% of these
cases, and the regional lymph nodes were the site of failure in 42%. Approximately 26% of patients
had evidence of distant failure. The patterns of failure included local tumor regrowth, tumor bed
recurrences, regional lymph node failures, and distant failures (ie, hematogenous failures and
peritoneal spread). Primary tumors involving the gastroesophageal junction tended to fail in the liver
and the lungs. Lesions involving the esophagus failed in the liver.[24 ]
Adjuvant therapy
The pattern of failure prompted a number of investigations into adjuvant therapy. The rationale
behind radiotherapy is to provide additional local-regional tumor control. Adjuvant chemotherapy is
used either as a radiosensitizer or as definitive treatment for presumed systemic metastases.
Adjuvant radiotherapy
Moertel and colleagues randomized postoperative patients with advanced gastric cancer to receive
40 Grays (Gy) of radiotherapy or 40 Gy of radiotherapy with 5-FU as a radiosensitizer and
demonstrated improved survival associated with the combined-modality therapy.[25 ]
The British Stomach Cancer Group reported lower rates of local recurrence in patients who received
postoperative radiotherapy than in those who underwent surgery alone.[26 ]
The update of the initial Gastrointestinal Tumor Study Group series revealed higher 4-year survival
rates in patients with unresectable gastric cancer who received combined-modality therapy than in
those who received chemotherapy alone (18% vs 6%).[27 ]
In a series from the Mayo Clinic, patients were randomized to receive postoperative radiotherapy
with 5-FU or surgery alone, and improved survival was demonstrated in patients receiving adjuvant
therapy (23% vs 4%).[28 ]
Intraoperative radiotherapy
Some authors suggest that intraoperative radiotherapy (IORT) shows promising results.
This alternative method of delivering radiotherapy allows for a high dose to be given in a single
fraction while in the operating room so that other critical structures can be avoided.

The National Cancer Institute randomized patients with grossly resected stage III/IV gastric cancer to
receive either 20 Gy of IORT or 50 Gy of postoperative external beam radiation. Local failure was
delayed in the patients treated with IORT (21 mo vs 8 mo). Although the median survival duration
also was higher (21 mo vs 10 mo), this figure did not reach statistical significance.[29 ]
Adjuvant chemotherapy
Numerous randomized clinical trials comparing combination chemotherapy in the postoperative
setting to surgery alone did not demonstrate a consistent survival benefit.
Recent meta-analyses have shown a hint of statistical benefit. In one meta-analysis of 13
randomized trials, adjuvant systemic chemotherapy was associated with a significant survival benefit
(odds ratio for death, 0.80; 95% CI, 0.66-0.97). In subgroup analysis, there was a trend toward a
larger magnitude of effect for trials in which at least two thirds of the patients had node-positive
disease.[30 ]
A postoperative chemoradiation study was prompted in part by the patterns of local failure often
preceding systemic spread.
Adjuvant chemoradiotherapy
A randomized phase III study performed in the United States, Intergroup 0116, demonstrated a
survival benefit associated with postoperative chemoradiotherapy compared with surgery alone.[2 ]
In this study, patients underwent an en bloc resection.
Patients with T3 and/or N+ adenocarcinoma of the stomach or gastroesophageal junction were
randomized to receive a bolus of 5-fluorouracil (5-FU) and leucovorin (LV) and radiotherapy or
observation.
Patients who received the adjuvant chemoradiotherapy demonstrated improved disease-free survival
(from 32% to 49%) and improved overall survival rates (from 41% to 52%) compared to those who
were merely observed.
This regimen is considered the standard of care in the United States.
Neoadjuvant chemotherapy
Neoadjuvant chemotherapy may allow downstaging of disease to increase resectability, decrease
micrometastatic disease burden prior to surgery, allow patient tolerability prior to surgery, determine
chemotherapy sensitivity, reduce the rate of local and distant recurrences, and ultimately improve
survival.
A European randomized trial also demonstrated survival benefit when patients were treated with 3
cycles of preoperative chemotherapy (epirubicin, cisplatin, and 5-fluorouracil) followed by surgery
and then 3 cycles of postoperative chemotherapy compared with surgery alone. The benefit was
comparable to that obtained with postoperative chemoradiation in the US trial.[3 ]However, the Gastric
Chemotherapy Group for Japan did not demonstrate a significant survival benefit with neoadjuvant
chemotherapy.
Choice of preoperative and postoperative chemotherapy versus postoperative chemotherapy and
radiation remains controversial, and an ongoing United States Intergroup study, CALGB 80101, will
look more closely at that question.

Advanced unresectable disease
Many patients present with distant metastases, carcinomatosis, unresectable hepatic metastases,
pulmonary metastases, or direct infiltration into organs that cannot be resected completely.
In the palliative setting, radiotherapy provides relief from bleeding, obstruction, and pain in 50-75% of
patients. The median duration of palliation is 4-18 months.
Surgical procedures such as wide local excision, partial gastrectomy, total gastrectomy, simple
laparotomy, gastrointestinal anastomosis, and bypass also are performed with palliative intent, with a
goal of allowing oral intake of food and alleviating pain.
Platinum-based chemotherapy, in combinations such as epirubicin/cisplatin/5-FU or
docetaxel/cisplatin/5-FU, represents the current first-line regimen. Other active regimens include
irinotecan and cisplatin and other combinations with oxaliplatin and irinotecan.
Results of cisplatin-based chemotherapy have been largely discouraging, with median time to
progression of 3-4 months and overall survival of approximately 6-9 months despite reported
response rates of up to 45%. Early results reported in 2007 by Japanese clinicians suggest some
improvement in both response rates and survival with the oral fluoropyrimidine S-1 used alone or in
combination with cisplatin.[31 ](S-1 combines 3 investigational drugs: tegafur, a prodrug of 5-FU;
gimeracil, an inhibitor of fluorouracil degradation; and oteracil or potassium oxanate, a GI tract
adverse-effect modulator.) These results remain to be confirmed by ongoing studies in Europe and
North America.
Bevacizumab, a monoclonal antibody against vascular endothelial growth factor (VEGF) is currently
being evaluated for use in advanced gastric cancer.[32 ]
Novel treatment strategies may be guided by the use of gene signatures.[33 ]Kim et al reported that
combined overexpression of MYC, EGFR, and FGFR2 predicts a poor response of metastatic gastric
cancer to treatment with cisplatin and fluorouracil.[34 ]
Ishido et al reported that in patients receiving S-1 chemotherapy after gastrectomy for advanced
gastric cancer, intratumoral mRNA expression of thymidylate synthase (TS) is an independent
prognostic factor for response to chemotherapy. In 39 patients who received postoperative S-1,
recurrence-free survival and overall survival were significantly longer in patients with low TS
expression than in those with high TS expression (P=0.021 and 0.016, respectively), whereas in 40
patients treated with surgery only, TS expression did not correlate with survival.[35 ]
Overexpression of human epidermal growth factor receptor 2 (HER2) is a significant negative
prognostic factor for gastric cancer. In the international ToGA trial (trastuzumab with chemotherapy in
HER2-positive advanced gastric cancer), about 22% of patients with advanced gastric cancer were
found to have tumors that overexpressed HER2. In this phase III trial, 594 patients with HER2-
positive advanced gastric cancer were randomized to receive standard chemotherapy alone or
chemotherapy plus trastuzumab (Herceptin). Overall survival with trastuzumab was 13.8 months,
compared with 11.1 months in the chemotherapy group (hazard ratio, 0.74, P = .0046).[36 ]
Although modest, this 2.7-month improvement in overall survival is clinically meaningful in this group
of patients, who have a poor prognosis. In addition to the impact on overall survival, trastuzumab
improved all of the secondary end points, including progression-free survival (increased from 5.2 mo
to 6.7 mo; P = .002) and overall response rate (increased from 34.5% to 47%; P =.0017).

Trastuzumab was approved in October of 2010 for the treatment of HER2-overexpressing metastatic
gastric or gastroesophageal junction adenocarcinoma. It is administered in combination with cisplatin
and capecitabine or 5-fluorouracil in patients who have not received prior treatment for metastatic
disease. The trastuzumab dose consists of an initial cycle of 8 mg/kg intravenously (IV) infused over
90 minutes, followed by subsequent cycles of 6 mg/kg IV infused over 30-90 minutes every 3 weeks.
Treatment is continued until the disease progresses.
Patient Education
Multimedia
For excellent patient education resources, visit eMedicine's Esophagus, Stomach, and Intestine
Center. Also, see eMedicine's patient education article, Stomach Cancer.
Multimedia
Gastroesophageal Reflux DiseasePiero Marco Fisichella, MD, Assistant Professor of Surgery, Stritch School of Medicine, Loyola University; Director, Esophageal Motility Center, Loyola University Medical CenterMarco G Patti, MD, Professor of Surgery, Director, Center for Esophageal Diseases, University of Chicago Pritzker School of Medicine
Updated: Apr 28, 2009
Introduction
Background

Gastroesophageal reflux is a normal physiologic phenomenon experienced intermittently by most
people, particularly after a meal. Gastroesophageal reflux disease (GERD) occurs when the amount
of gastric juice that refluxes into the esophagus exceeds the normal limit, causing symptoms with or
without associated esophageal mucosal injury (ie, esophagitis).
For excellent patient education resources, visit eMedicine's Heartburn/GERD/Reflux Center and
Esophagus, Stomach, and Intestine Center. Also, see eMedicine's patient education articles
Gastroesophageal Reflux Disease (GERD), Heartburn, and Heartburn/GERD Medications.
Pathophysiology
The physiologic and anatomic factors that prevent the reflux of gastric juice from the stomach into the
esophagus include the following:
The lower esophageal sphincter (LES) must have a normal length and pressure and a
normal number of episodes of transient relaxation (relaxation in the absence of swallowing).
The gastroesophageal junction must be located in the abdomen so that the diaphragmatic
crura can assist the action of the LES, thus functioning as an extrinsic sphincter. The
presence of a hiatal hernia disrupts this synergistic action and can promote reflux (see
image below).
Barium swallow indicating hiatal hernia.
Esophageal clearance must be able to neutralize the acid refluxed through the LES.
(Mechanical clearance is achieved with esophageal peristalsis. Chemical clearance is
achieved with saliva.)
The stomach must empty properly.
Abnormal gastroesophageal reflux is caused by the abnormalities of one or more of the following
protective mechanisms:
A functional (frequent transient LES relaxation) or mechanical (hypotensive LES) problem of
the LES is the most common cause of gastroesophageal reflux disease (GERD).
Certain foods (eg, coffee, alcohol), medications (eg, calcium channel blockers, nitrates,
beta-blockers), or hormones (eg, progesterone) can decrease the pressure of the LES.
Obesity is a contributing factor in gastroesophageal reflux disease (GERD), probably
because of the increased intra-abdominal pressure.
From a therapeutic point of view, informing patients that gastric refluxate is made up not only of acid
but also of duodenal contents (eg, bile, pancreatic secretions) is important.

Frequency
United States
Heartburn is a common problem in the United States and in the Western world. Approximately 7% of
the population experience symptoms of heartburn daily. An abnormal esophageal exposure to gastric
juice is probably present in 20-40% of this population, meaning 20-40% of the people who
experience heartburn do indeed have gastroesophageal reflux disease (GERD). In the remaining
population, heartburn is probably due to other causes. Because many individuals control symptoms
with over-the-counter (OTC) medications and without consulting a medical professional, the condition
is likely underreported.
Mortality/Morbidity
In addition to the typical symptoms of gastroesophageal reflux disease (GERD) (eg,
heartburn, regurgitation, dysphagia), abnormal reflux can cause atypical symptoms, such as
coughing, chest pain, and wheezing. Additional atypical symptoms from abnormal reflux
include damage to the lungs (eg, pneumonia, asthma, idiopathic pulmonary fibrosis), vocal
cords (eg, laryngitis, cancer), ear (eg, otitis media), and teeth (eg, enamel decay).
Approximately 50% of patients with gastric reflux develop esophagitis (see image below).

Peptic esophagitis. A rapid urease test (RUT) is performed on the
esophageal biopsy sample. The result is positive for esophagitis.
Esophagitis is classified into the following 4 grades based on its severity: o Grade I – Erythema
o Grade II – Linear nonconfluent erosions
o Grade III – Circular confluent erosions
o Grade IV – Stricture or Barrett esophagus. Barrett esophagus is thought to be
caused by the chronic reflux of gastric juice into the esophagus. Barrett esophagus
occurs when the squamous epithelium of the esophagus is replaced by the
intestinal columnar epithelium (see image below). o
Esophagogastroduodenoscopy indicating Barrett esophagus.
o Barrett esophagus is present in 8-15% of patients with gastroesophageal reflux
disease (GERD) and may progress to adenocarcinoma (see images below) o
Gastroesophageal reflux disease (GERD)/Barrett
esophagus/adenocarcinoma sequence.

o
Endoscopy demonstrating intraluminal esophageal cancer.
o See Esophageal Cancer.
Race
White males are at a greater risk for Barrett esophagus and adenocarcinoma than other
populations.
Sex
No sexual predilection exists. Gastroesophageal reflux disease (GERD) is as common in
men as in women.
The male-to-female incidence ratio for esophagitis is 2:1-3:1. The male-to-female incidence
ratio for Barrett esophagus is 10:1.

Age
Gastroesophageal reflux disease (GERD) occurs in all age groups.
The prevalence of gastroesophageal reflux disease (GERD) increases in people older than
40 years.
Clinical
History
Gastroesophageal reflux disease (GERD) can cause typical (esophageal) symptoms or atypical
(extraesophageal) symptoms. However, a diagnosis of gastroesophageal reflux disease (GERD)
based on the presence of typical symptoms is correct in only 70% of patients.
Typical (esophageal) symptoms include the following: o Heartburn is the most common typical symptom of gastroesophageal reflux disease
(GERD). Heartburn is felt as a retrosternal sensation of burning or discomfort that
usually occurs after eating or when lying down or bending over. o Regurgitation is an effortless return of gastric and/or esophageal contents into the
pharynx. Regurgitation can induce respiratory complications if gastric contents spill
into the tracheobronchial tree. o Dysphagia occurs in approximately one third of patients because of a mechanical
stricture or a functional problem (eg, nonobstructive dysphagia secondary to
abnormal esophageal peristalsis). Patients with dysphagia experience a sensation
that food is stuck, particularly in the retrosternal area.
Atypical (extraesophageal) symptoms include the following: o Coughing and/or wheezing are respiratory symptoms resulting from the aspiration
of gastric contents into the tracheobronchial tree or from the vagal reflex arc
producing bronchoconstriction. Approximately 50% of patients who have GERD-
induced asthma do not experience heartburn. o Hoarseness results from irritation of the vocal cords by gastric refluxate and is often
experienced by patients in the morning. o Reflux is the most common cause of noncardiac chest pain, accounting for
approximately 50% of cases. Patients can present to the emergency department
with pain resembling a myocardial infarction. Reflux should be ruled out (using
esophageal manometry and 24-h pH testing if necessary; see image below) once a
cardiac cause for the chest pain has been excluded. Alternatively, a therapeutic trial
of a high-dose proton pump inhibitor (PPI) can be tried. o

Ambulatory pH monitoring indicating episodes of reflux correlating
with the heartburn experienced by the patient.
Physical
The physical examination is noncontributory.
Causes
See Pathophysiology.
Differential Diagnoses
Achalasia Esophagitis
Cholelithiasis Gastritis, Chronic
Coronary Artery Atherosclerosis Irritable Bowel Syndrome
Esophageal Cancer Peptic Ulcer Disease
Esophageal Spasm
Other Problems to Be Considered
Some studies have shown that gastroesophageal reflux disease (GERD) is highly prevalent in
patients who are morbidly obese and that a high body mass index (BMI) is a risk factor for the
development of this condition.[1,2,3,4,5,6 ]
The mechanism by which a high BMI increases esophageal acid exposure is not completely
understood. Increased intragastric pressure and gastroesophageal pressure gradient, incompetence
of the LES, and increased frequency of transient LES relaxations may all play a role in the
pathophysiology of gastroesophageal reflux disease (GERD) in patients who are morbidly obese.
To further support the hypothesis that obesity increases esophageal acid exposure is the
documentation of a dose-response relationship between increased BMI and increased prevalence of
gastroesophageal reflux disease (GERD) and its complications. Therefore, the pathophysiology of
GERD in patients who are morbidly obese might differ from that of patients who are not obese. The
therapeutic implication of such a premise is that the correction of reflux in patients who are morbidly
obese might be better achieved with a procedure that first controls obesity.
Workup

Laboratory Studies
Laboratory tests are seldom useful in establishing a diagnosis of gastroesophageal reflux
disease (GERD).
Imaging Studies
Barium esophagogram o A barium esophagogram is particularly important for patients with gastroesophageal
reflux disease (GERD) who experience dysphagia. o A barium esophagogram can show the presence and location of a stricture and the
presence and shape of a hiatal hernia.
Esophagogastroduodenoscopy (EGD) o EGD identifies the presence and severity of esophagitis and the possible presence
of Barrett esophagus (see image below). o
Esophagogastroduodenoscopy indicating Barrett esophagus.
o EGD also excludes the presence of other diseases (eg, peptic ulcer) that can
present similarly to gastroesophageal reflux disease (GERD). o Although EGD is frequently performed to help diagnose gastroesophageal reflux
disease (GERD), it is not the most cost-effective diagnostic study because
esophagitis is present in only 50% of patients with GERD.
Other Tests
Esophageal manometry o Esophageal manometry defines the function of the LES and the esophageal body
(peristalsis). o Esophageal manometry is essential for correctly positioning the probe for the 24-
hour pH monitoring.
Ambulatory 24-hour pH monitoring o Ambulatory 24-hour pH monitoring is the criterion standard in establishing a
diagnosis of GERD with a sensitivity of 96% and a specificity of 95%. o Ambulatory 24-hour pH monitoring quantifies the gastroesophageal reflux and
allows a correlation between the symptoms of reflux and the episodes of reflux. o Patients with endoscopically confirmed esophagitis do not need pH monitoring to
establish a diagnosis of gastroesophageal reflux disease (GERD).
Indications for esophageal manometry and prolonged pH monitoring include the following:

o Persistence of symptoms while taking adequate antisecretory therapy, such as PPI
therapy o Recurrence of symptoms after discontinuation of acid-reducing medications
o Investigation of atypical symptoms, such as chest pain or asthma, in patients
without esophagitis o Confirmation of the diagnosis in preparation for antireflux surgery
Radionuclide measurement of gastric emptying o Although delayed gastric emptying is present in as many as 60% of patients with
gastroesophageal reflux disease (GERD), this emptying is usually a minor factor in
the pathogenesis of the disease in most patients (except in patients with advanced
diabetes mellitus or connective tissue disorders). o Patients with delayed gastric emptying typically experience postprandial bloating
and fullness in addition to other symptoms.
Treatment
Medical Care
Treatment of gastroesophageal reflux disease (GERD) is a stepwise approach. The goals are to
control symptoms, to heal esophagitis, and to prevent recurrent esophagitis or other complications.
The treatment is based on lifestyle modification and control of gastric acid secretion.
Lifestyle modifications include the following: o Losing weight (if overweight)
o Avoiding alcohol, chocolate, citrus juice, and tomato-based products
o Avoiding large meals
o Waiting 3 hours after a meal before lying down
o Elevating the head of the bed 8 inches
Pharmacologic therapy o Antacids were the standard treatment in the 1970s and are still effective in
controlling mild symptoms of gastroesophageal reflux disease (GERD). Antacids
should be taken after each meal and at bedtime. o Histamine H2-receptor antagonists are the first-line agents for patients with mild to
moderate symptoms and grades I-II esophagitis. Histamine H2 receptor antagonists
are effective for healing only mild esophagitis in 70-80% of patients with
gastroesophageal reflux disease (GERD) and for providing maintenance therapy to
prevent relapse. Tachyphylaxis has been observed, suggesting that pharmacologic
tolerance can reduce the long-term efficacy of these drugs. o Additional H2 blocker therapy has been reported to be useful in patients with severe
disease (particularly those with Barrett esophagus) who have nocturnal acid
breakthrough. o PPIs are the most powerful medications available for treating this condition. These
agents should be used only when gastroesophageal reflux disease (GERD) has
been objectively documented. PPIs work by blocking the final step in the H+ ion
secretion by the parietal cell. They have few adverse effects and are well tolerated
for long-term use. However, data have shown that PPIs can interfere with calcium
homeostasis and aggravate cardiac conduction defects. These agents have also
been responsible for hip fracture in postmenopausal women.[7 ] o A research review by the Agency for Healthcare Research and Quality (AHRQ)
concluded, on the basis of grade A evidence, that PPIs were superior to histamine
H2-receptor antagonists for the resolution of gastroesophageal reflux disease
(GERD) symptoms at 4 weeks and healing of esophagitis at 8 weeks.[8 ]In addition,

the AHRQ found no difference between individual PPIs (omeprazole, lansoprazole,
pantoprazole, and rabeprazole) for relief of symptoms at 8 weeks. For symptom
relief at 4 weeks, esomeprazole 20 mg was equivalent, but esomeprazole 40 mg
superior, to omeprazole 20mg.[8 ] o Prokinetic agents improve the motility of the esophagus and stomach. These agents
are somewhat effective but only in patients with mild symptoms; other patients
usually require additional acid-suppressing medications, such as PPIs. Long-term
use of prokinetic agents may have serious, even potentially fatal, complications and
should be discouraged.
Surgical Care
Approximately 80% of patients have a recurrent but nonprogressive form of gastroesophageal reflux
disease (GERD) that is controlled with medications. Identifying the 20% of patients who have a
progressive form of the disease is important, because they may develop severe complications, such
as strictures or Barrett esophagus. For patients who develop complications, surgical treatment
should be considered at an earlier stage to avoid the sequelae of the disease that can have serious
consequences.
Indications for fundoplication include the following: o Patients with symptoms that are not completely controlled by PPI therapy can be
considered for surgery. Surgery can also be considered in patients with well-
controlled gastroesophageal reflux disease (GERD) who desire definitive, one-time
treatment. o The presence of Barrett esophagus is an indication for surgery. Whether acid
suppression improves the outcome or prevents the progression of Barrett
esophagus remains unknown, but most authorities recommend complete acid
suppression in patients with histologically proven Barrett esophagus. o The presence of extraesophageal manifestations of gastroesophageal reflux
disease (GERD) may indicate the need for surgery. These include the following: (1)
respiratory manifestations (eg, cough, wheezing, aspiration); (2) ear, nose, and
throat manifestations (eg, hoarseness, sore throat, otitis media); and (3) dental
manifestations (eg, enamel erosion). o Young patients
o Poor patient compliance with regard to medications
o Postmenopausal women with osteoporosis
o Patients with cardiac conduction defects
o Cost of medical therapy
Laparoscopic fundoplication o Laparoscopic fundoplication is performed under general endotracheal anesthesia.
Five small (5- to 10-mm) incisions are used (see image below). The fundus of the
stomach is wrapped around the esophagus to create a new valve at the level of the
gastroesophageal junction. o

Laparoscopic Nissen fundoplication.
o The essential elements of the operation are as follows:
Complete mobilization of the fundus of the stomach with division of the
short gastric vessels
Reduction of the hiatal hernia
Narrowing of the esophageal hiatus
Creation of a 360° fundoplication over a large intraesophageal dilator
(Nissen fundoplication)o Laparoscopic fundoplication lasts 2-2.5 hours. The hospital stay is approximately 2
days. Patients resume regular activities within 2-3 weeks. o Approximately 92% of patients obtain resolution of symptoms after undergoing
laparoscopic fundoplication. o The AHRQ found, on the basis of limited evidence, that laparoscopic fundoplication
was as effective as open fundoplication for relieving heartburn and regurgitation,
improving quality of life, and decreasing use of antisecretory medications.[8 ]
Several randomized clinical trials have challenged the benefits of surgery in controlling
gastroesophageal reflux disease (GERD). o Lundell followed up his cohort of patients for 5 years and did not find surgery to be
superior to PPI therapy.[9 ] o Spechler found that, at 10 years after surgery, 62% of patients were back on
antireflux medications.[10 ] o A very rigorous, randomized study by Anvari et al reestablished surgery as the
criterion standard in treating gastroesophageal reflux disease (GERD).[11 ]The
investigators showed that, at 1 year, the outcome and the symptom control in the
surgical group was better than that in the medical group.[11 ]

o A British multicenter randomized study conducted by Grant et al also compared
surgical treatment versus medical therapy in patients with documented evidence of
gastroesophageal reflux disease (GERD).[12 ]The type of laparoscopic fundoplication
was decided by the respective surgeons. Individuals who had received medication
for their condition had taken them for a median of 32 months before participating in
the study. o The investigators reported that by 12 months, 38% of those who had undergone
surgery were taking reflux medication compared with 90% of the individuals
randomized to medical management.[12 ]In addition, other health measure favored
the randomized surgical group.
Long-term results of laparoscopic antireflux surgery have shown that, at 10 years, 90% of
patients are symptom free, and only a minority still takes PPIs.[13 ]
Medication
The goals of pharmacotherapy are to prevent complications and to reduce morbidity in patients with
gastroesophageal reflux disease (GERD).
H2-Receptor Antagonists
H2-receptor antagonists are reversible competitive blockers of histamine at the H2 receptors,
particularly those in the gastric parietal cells where they inhibit acid secretion. The H2 antagonists
are highly selective, do not affect the H1 receptors, and are not anticholinergic agents. Although
intravenous (IV) administration of H2 blockers may be used to treat acute complications
(eg, gastrointestinal bleeding), the benefits are not yet proven.
Ranitidine (Zantac)
Inhibits histamine stimulation of the H2 receptor in gastric parietal cells, which, in turn, reduces
gastric acid secretion, gastric volume, and hydrogen concentrations.
Dosing
Adult
150 mg PO bid (300 mg PO bid or 150 mg qid)
Pediatric
<12 years: Not established
>12 years
PO: 1.25-2.5 mg/kg/dose q12h; not to exceed 300 mg/d
IV/IM: 0.75-1.5 mg/kg/dose q6-8h; not to exceed 400 mg/d
Interactions
May decrease the effects of ketoconazole and itraconazole; may alter the serum levels of ferrous
sulfate, diazepam, nondepolarizing muscle relaxants, and oxaprozin
Contraindications

Documented hypersensitivity
Precautions
Pregnancy
B - Fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Precautions
Caution in patients with renal or liver impairment; if changes in renal function occur during therapy,
consider adjusting the dose or discontinuing treatment
Cimetidine (Tagamet)
Inhibits histamine at H2 receptors of gastric parietal cells, which results in reduced gastric acid
secretion, gastric volume, and hydrogen concentrations.
Dosing
Adult
400 mg PO bid (800 mg bid or 400 mg PO qid)
Pediatric
Not established
Suggested dose is 1-2 mg/kg/d PO/IV divided q6h; not to exceed 40 mg/d
Interactions
Can increase blood levels of theophylline, warfarin, tricyclic antidepressants, triamterene, phenytoin,
quinidine, propranolol, metronidazole, procainamide, and lidocaine
Contraindications
Documented hypersensitivity
Precautions
Pregnancy
B - Fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Precautions
Elderly people may experience confusional states; may cause impotence and gynecomastia in young
males; may increase the levels of many drugs; adjust the dose or discontinue treatment if changes in
renal function occur
Famotidine (Pepcid)
Competitively inhibits histamine at H2 receptor of gastric parietal cells, resulting in reduced gastric
acid secretion, gastric volume, and hydrogen concentrations.
Dosing

Adult
20 mg PO bid (40 mg bid)
Pediatric
Not established; 1-2 mg/kg/d PO/IV divided q6h suggested; not to exceed 40 mg/dose
Interactions
May decrease the effects of ketoconazole and itraconazole
Contraindications
Documented hypersensitivity
Precautions
Pregnancy
B - Fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Precautions
If changes in renal function occur during therapy, consider adjusting the dose or discontinuing
treatment.
Nizatidine (Axid)
Competitively inhibits histamine at the H2 receptor of the gastric parietal cells, resulting in reduced
gastric acid secretion, gastric volume, and hydrogen concentrations.
Dosing
Adult
150 mg PO bid (300 mg PO qhs)
Pediatric
Not established
Interactions
None reported
Contraindications
Documented hypersensitivity
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Caution in patients with renal or liver impairment; if changes in renal function occur during therapy,
consider adjusting the dose or discontinuing treatment

Proton Pump Inhibitors
Proton pump inhibitors inhibit gastric acid secretion by inhibition of the H+/K+ ATPase enzyme system
in the gastric parietal cells. These agents are used in cases of severe esophagitis and in patients
whose conditions do not respond to H2 receptor antagonist therapy.
Omeprazole (Prilosec)
Used for up to 4 wk to treat and relieve symptoms of active duodenal ulcers. May use for up to 8 wk
to treat all grades of erosive esophagitis.
Dosing
Adult
20 mg PO qd or bid
Pediatric
Not established
Interactions
May decrease the effects of itraconazole and ketoconazole; may increase the toxicity of warfarin,
digoxin, and phenytoin
Contraindications
Documented hypersensitivity
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Bioavailability may increase in the elderly.
Lansoprazole (Prevacid)
Inhibits gastric acid secretion. Used for up to 8 wk to treat all grades of erosive esophagitis.
Dosing
Adult
15-60 mg PO qd or 15 mg bid
Pediatric
Not established
Interactions
May decrease the effects of ketoconazole and itraconazole; may increase theophylline clearance

Contraindications
Documented hypersensitivity
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Consider adjusting the dose in patients with liver impairment.
Rabeprazole (Aciphex)
For short-term (4- to 8-wk) treatment and relief of symptomatic erosive or ulcerative GERD. In
patients not healed after 8 wk, consider additional 8-wk course.
Dosing
Adult
20 mg PO qd for 4-8 wk
Pediatric
Not established
Interactions
None reported
Contraindications
Documented hypersensitivity
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Symptomatic response does not exclude the possibility of malignancy.
Esomeprazole (Nexium)
S-isomer of omeprazole. Inhibits gastric acid secretion by inhibiting H+/K+ ATPase enzyme system at
secretory surface of gastric parietal cells.
Dosing
Adult
20-40 mg PO qd for 4-8 wk

Pediatric
Not established
Interactions
None reported
Contraindications
Documented hypersensitivity
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Symptomatic relief with proton pump inhibitors may mask the symptoms of gastric malignancy.
Prokinetics
Prokinetic agents increase LES pressure to help reduce reflux of gastric contents. They also
accelerate gastric emptying.
Metoclopramide (Reglan)
GI prokinetic agent that increases GI motility, increases resting esophageal sphincter tone, and
relaxes pyloric sphincter.
Dosing
Adult
10 mg PO qid
Pediatric
Not established
Interactions
May antagonize the effects of metoclopramide; opiate analgesics may increase metoclopramide
toxicity in the CNS
Contraindications
Documented hypersensitivity; pheochromocytoma or GI hemorrhage, obstruction, or perforation;
history of seizure disorders
Precautions
Pregnancy
B - Fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Precautions

Caution in patients with a history of mental illness and Parkinson disease
Follow-up
Complications
Esophagitis (esophageal mucosal damage) occurs in approximately 50% of patients with
gastroesophageal reflux disease (GERD).
Barrett esophagus is one of the most serious complications of gastroesophageal reflux
disease (GERD), because it may progress to cancer (see images below).


Peptic esophagitis. A rapid urease test (RUT) is performed on the
esophageal biopsy sample. The result is positive for esophagitis.
Endoscopy demonstrating intraluminal esophageal cancer.
Even though a prospective randomized trial has never been performed to compare PPIs to
laparoscopic fundoplication, the authors believe fundoplication is preferable for the following
reasons: o PPIs, although effective in controlling the acid component of the refluxate, do not
eliminate the reflux of bile, which some believe to be a major contributor to the
pathogenesis of Barrett epithelium. o Patients with Barrett esophagus tend to have lower LES pressure and worse
esophageal peristalsis than patients without Barrett esophagus. Patients with
Barrett esophagus are also exposed to a larger amount of reflux.

o A fundoplication offers the only possibility of stopping any kind of reflux by creating
a competent LES. However, until the definitive answer is known, the authors
recommend that patients with Barrett esophagus continue to undergo periodic
endoscopic surveillance even after laparoscopic fundoplication.
Respiratory complications include pneumonia, asthma, and interstitial lung fibrosis.
Prognosis
Most patients with gastroesophageal reflux disease (GERD) do well with medications,
although a relapse after cessation of medical therapy is common and indicates the need for
long-term maintenance therapy.
Identifying the subgroup of patients who may develop the most serious complications of
gastroesophageal reflux disease (GERD) and treating them aggressively is important.
Surgery at an early stage is most likely indicated in these patients.
After a laparoscopic Nissen fundoplication, symptoms resolve in approximately 92% of
patients.
Miscellaneous
Medicolegal Pitfalls
Esophageal manometry and pH monitoring are considered essential before performing an
antireflux operation. Endoscopy reveals that 50% of patients do not have esophagitis. The
only way to determine if abnormal reflux is present and if symptoms are actually caused by
gastroesophageal reflux is through pH monitoring.
Achalasia can present with heartburn. Only esophageal manometry and pH monitoring can
be used to distinguish achalasia from gastroesophageal reflux disease (GERD). Therapy is
completely different for the 2 conditions.
Multimedia
Media file 1: Esophagogastroduodenoscopy indicating Barrett esophagus.

Media file 2: Gastroesophageal reflux disease (GERD)/Barrett
esophagus/adenocarcinoma sequence.

Media file 3: Barium swallow indicating hiatal hernia.
Media file 4: Ambulatory pH monitoring indicating episodes of reflux correlating
with the heartburn experienced by the patient.
Media file 5: Laparoscopic Nissen fundoplication.


Media file 6: Peptic esophagitis. A rapid urease test (RUT) is performed on the
esophageal biopsy sample. The result is positive for esophagitis.
Media file 7: Endoscopy demonstrating intraluminal esophageal cancer.
References
Colon Cancer, AdenocarcinomaTomislav Dragovich, MD, PhD, Associate Professor of Medicine and Director of Clinical Gastrointestinal Cancer Program, Arizona Cancer Center, University of Arizona College of MedicineVassiliki L Tsikitis, MD, Assistant Professor of Surgery, Section of Surgical Oncology, University of Arizona Medical Center
Updated: Dec 23, 2010
Introduction
Background
Invasive colorectal cancer is a preventable disease. Early detection through widely applied screening
programs is the most important factor in the recent decline of colorectal cancer in developed
countries (see Deterrence/Prevention). Full implementation of the screening guidelines[1 ]can cut
mortality rate from colorectal cancer in the United States by an estimated additional 50%; even
greater reductions are estimated for countries where screening tests may not be widely available at
present. New and more comprehensive screening strategies are also needed.

Fundamental advances in understanding the biology and genetics of colorectal cancer are taking
place. This knowledge is slowly making its way into the clinic and being employed to better stratify
individual risks of developing colorectal cancer, discover better screening methodologies, allow for
better prognostication, and improve one’s ability to predict benefit from new anticancer therapies.
In the past 10 years, an unprecedented advance in systemic therapy for colorectal cancer has
dramatically improved outcome for patients with metastatic disease. Until the mid 1990s, the only
approved agent for colorectal cancer was 5-fluorouracil. New agents that became available in the
past 10 years include cytotoxic agents such as irinotecan and oxaliplatin,[2 ]oral fluoropyrimidines
(capecitabine and tegafur), and biologic agents such as bevacizumab, cetuximab, and panitumumab.[3 ]
Though surgery remains the definitive treatment modality, these new agents will likely translate into
improved cure rates for patients with early stage disease (stage II and III) and prolonged survival for
those with stage IV disease. Further advances are likely to come from the development of new
targeted agents and integration of those agents with other modalities such as surgery, radiation
therapy, and liver-directed therapies.
An image depicting standard colectomies for adenocarcinoma of the colon can be seen below.

Standard colectomies for adenocarcinoma of the colon.
Pathophysiology
Genetically, colorectal cancer represents a complex disease, and genetic alterations are often
associated with progression from premalignant lesion (adenoma) to invasive adenocarcinoma.
Sequence of molecular and genetic events leading to transformation from adenomatous polyps to
overt malignancy has been characterized by Vogelstein and Fearon.[4 ]The early event is a mutation
of APC (adenomatous polyposis gene), which was first discovered in individuals with familial
adenomatous polyposis (FAP). The protein encoded by APC is important in activation of oncogene c-
myc and cyclin D1, which drives the progression to malignant phenotype. Although FAP is a rare
hereditary syndrome accounting for only about 1% of cases of colon cancer, APC mutations are very
frequent in sporadic colorectal cancers.

In addition to mutations, epigenetic events such as abnormal DNA methylation can also cause
silencing of tumor suppressor genes or activation of oncogenes, compromising the genetic balance
and ultimately leading to malignant transformation.
Other important genes in colon carcinogenesis include KRAS oncogene , chromosome 18 loss of
heterozygosity (LOH) leading to inactivation of SMAD4 (DPC4), and DCC (deleted in colon cancer)
tumor suppression genes. Chromosome arm 17p deletion and mutations affecting p53 tumor
suppressor gene confer resistance to programmed cell death (apoptosis) and are thought to be late
events in colon carcinogenesis.
A subset of colorectal cancers is characterized with deficient DNA mismatch repair. This phenotype
has been linked to mutations of genes such as MSH2, MLH1, and PMS2. These mutations result in
so-called high frequency microsatellite instability (H-MSI), which can be detected with an
immunocytochemistry assay. H-MSI is a hallmark of hereditary nonpolyposis colon cancer syndrome
(HNPCC, Lynch syndrome), which accounts for about 6% of all colon cancers. H-MSI is also found in
about 20% of sporadic colon cancers.
Frequency
United States
The American Cancer Society estimated that 148,810 individuals would be diagnosed with colorectal
cancer and 49,960 would die from this disease in the United States in 2008.[5 ]
International
In 2003, the World Health Organization estimated that approximately 940,000 individuals were be
diagnosed with colorectal cancer worldwide and 492,000 died from it that year.
Mortality/Morbidity
Colorectal cancer is a major health burden worldwide. The incidence and mortality from colon cancer
has been on a slow decline over the past 20 years in the United States; however, colon cancer
remained the third most common cause of cancer-related mortality in 2008. A multitude of risk factors
have been linked to colorectal cancer, including heredity, environmental exposures, and
inflammatory syndromes affecting gastrointestinal tract.
A review of 8 trials by Rothwell et al found allocation to aspirin reduced death caused by cancer.
Individual patient data were available from 7 of the 8 trials. Benefit was apparent after 5 years of
follow-up. The 20-year risk of cancer death was also lower in the aspirin group for all solid cancers. A
latent period of 5 years was observed before risk of death was decreased for esophageal,
pancreatic, brain, and lung cancers. A more delayed latent period was observed for stomach,
colorectal, and prostate cancer. Benefit was only seen for adenocarcinomas in lung and esophageal
cancers. The overall effect on 20-year risk of cancer death was greatest for adenocarcinomas.[6 ]
Race
Recent trends in the United States suggest a disproportionally higher incidence and death from colon
cancer in African Americans than in whites. Hispanic persons have the lowest incidence and
mortality from colorectal cancer.
Sex
The incidence of colorectal cancer is about equal for males and females.
Age

Age is a well-known risk factor for colorectal cancer, as it is for many other solid tumors. The timeline
for progression from early premalignant lesion to malignant cancer ranges from 10-20 years. The
incidence of colorectal cancer peaks at about age 65 years.
Clinical
History
Due to increased emphasis on screening practices, colon cancer is now often detected during
screening procedures. Other common clinical presentations include iron-deficiency anemia, rectal
bleeding, abdominal pain, change in bowel habits, and intestinal obstruction or perforation. Right-
sided lesions are more likely to bleed and cause diarrhea, while left-sided tumors are usually
detected later and could present with bowel obstruction.
Physical
Physical findings could be very nonspecific (fatigue, weight loss) or absent early in the disease
course. In more advanced cases, abdominal tenderness, macroscopic rectal bleeding, palpable
abdominal mass, hepatomegaly, and ascites could be present on physical examination.
Causes
Colorectal cancer is a multifactorial disease process, with etiology transcending genetic factors,
environmental exposures (including diet), and inflammatory conditions of digestive tract.
Though much about colorectal cancer genetics remains unknown, current research indicates that
genetic factors have the greatest correlation to colorectal cancer. Hereditary mutation of the APC
gene is the cause of familial adenomatous polyposis (FAP), where affected individuals carry an
almost 100% risk of developing colon cancer by age 40 years.
Hereditary nonpolyposis colon cancer syndrome (HNPCC, Lynch syndrome) carries about 40%
lifetime risk of developing colorectal cancer; individuals with this syndrome are also at increased risk
for urothelial cancer, endometrial cancer, and other less common cancers. Lynch syndrome is
characterized by deficient mismatch repair (dMMR) due to inherited mutation in one of the mismatch
repair genes, such as hMLH1, hMSH2, hMSH6, hPMS1, hPMS2, and possibly other undiscovered
genes. HNPCC is a cause of about 6% of all colon cancers. Although the use of aspirin may reduce
the risk of colorectal neoplasia in some populations, a study by Burn et al found no effect on the
incidence of colorectal cancer among carriers of Lynch syndrome with use of aspirin, resistant starch,
or both.[7 ]
Dietary factors are the subject of intense and ongoing investigations.[8 ]Epidemiological studies have
linked increased risk of colorectal cancer with a diet high in red meat and animal fat, low-fiber diet,
and low overall intake of fruits and vegetables. Factors associated with lower risk include folate
intake, calcium intake, and estrogen replacement therapy. However, most of these studies were
retrospective epidemiological studies and have yet to be validated in prospective, placebo-controlled,
interventional trials.
Lifestyle choices such as alcohol and tobacco consumption, obesity, and sedentary habits have also
been associated with increased risk for colorectal cancer.
Association between body mass index (BMI) and risk of colorectal adenomas and cancer has been
reported, but few studies have had adequate sample size for conducting stratified analyses. Jacobs
et al pooled data from 8,213 participants in 7 prospective studies of metachronous colorectal
adenomas to assess whether the association between BMI and metachronous neoplasia varied by

sex, family history, colorectal subsite, or features of metachronous lesions. Exploratory analyses
indicated that BMI was significantly related to most histologic characteristics of metachronous
adenomas among men but not among women. The researchers concluded that body size may affect
colorectal carcinogenesis at comparatively early stages, particularly among men.[9 ]
Inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease also carry an increased
risk of developing colorectal adenocarcinoma. The risk for developing colorectal malignancy
increases with the duration of inflammatory bowel disease and the greater extent of colon
involvement.
Differential Diagnoses
Arteriovenous malformation (AVM) Ileus
Carcinoid/Neuroendocrine Tumors and Rare Tumors of GI Tract Ischemic bowel
Crohn Disease Small Intestinal Carcinomas
Diverticulosis, Small Intestinal Ulcerative Colitis
Gastrointestinal Lymphoma
Workup
Laboratory Studies
Laboratory studies are done with a goal of assessing patients organ function (liver, kidneys) in
anticipation of diagnostic and therapeutic procedures (imaging, biopsy, surgery, chemotherapy) and
also to estimate tumor burden (CEA level).
Complete blood cell count
Chemistries and liver function tests
Serum carcinoembryonic antigen (CEA) should be obtained preoperatively as it carries
prognostic value and when highly elevated may indicate more advanced, disseminated
disease.
Imaging Studies
Adequate imaging of the chest and abdomen should be obtained for staging purposes,
ideally preoperatively. o Chest radiograph or chest CT scan
o Abdominal barium study to better delineate primary lesion preoperatively
o Abdominal/pelvic computerized tomography (CT scan), contrast ultrasound of the
abdomen/liver, and abdominal/pelvic MRI are appropriate for imaging abdomen and
liver, for the purpose of staging.
Positron emission tomography (PET) scans are emerging as a very useful modality for
staging and assessment of colorectal cancers. The newest addition, a fusion PET-CT scan,
allows for detection of metastatic deposits and has added tissue-based resolution of CT
scan. Of note, some histologies, especially a mucinous signet-ring cell variant of colorectal
cancer, may not be well visualized on a PET scan.
Procedures
A suspicion of colorectal cancer diagnosis warrants rectal examination and colonoscopy with
a biopsy of suspicious lesion. o Colonoscopy

o Sigmoidoscopy
o Double contrast barium enema
After tissue diagnosis is confirmed, further workup is driven by the clinical setting (eg,
profuse bleeding and obstruction may require an emergent surgery), patient status and
comorbidities, and presenting symptoms.
Histologic Findings
The microscopic appearance of colon adenocarcinomas may be that of well-differentiated or poorly
differentiated glandular structures. Normal topological architecture of colonic epithelium in terms of a
crypt-villous axis is lost.
Staging
The TNM staging system has become the international standard for staging of colorectal cancer. It
uses 3 descriptors: T for primary tumor, N for lymph nodal involvement, and M for metastasis.
In turn, these are divided into the following categories:
Tumor categories
Tx:No description of the tumor's extent is possible because of incomplete information.
Tis: In situ carcinoma; the tumor involves only the muscularis mucosa
T1: The cancer has grown through the muscularis mucosa and extends into the submucosa
T2:The cancer has grown through the submucosa and extends into the muscularis propria
T3: The cancer has grown through the muscularis propria and into the outermost layers of
the colon but not through them; it has not reached any nearby organs or tissues
T4a: The cancer has grown through the serosa (visceral peritoneum)
T4b: The cancer has grown through the wall of the colon and is attached to or invades
nearby tissues or organs
Node categories
Nx:No description of lymph node involvement is possible because of incomplete information
N0:No cancer in nearby lymph nodes
N1a:Cancer cells found in 1 nearby lymph node
N1b:Cancer cells found in 2 to 3 nearby lymph nodes
N1c:Small deposits of cancer cells found in areas of fat near lymph nodes, but not in the
lymph nodes themselves.
N2a:Cancer cells found in 4 to 6 nearby lymph nodes
N2b: Cancer cells found in 7 or more nearby lymph nodes
Metastasis categories
M0:No distant spread seen
M1a: The cancer has spread to 1 distant organ or set of distant lymph nodes
M1b:The cancer has spread to more than 1 distant organ or set of distant lymph nodes, or
has spread to distant parts of the peritoneum
Table 1. TNM Staging System for Colon Cancer

Stage Primary Tumor (T) Regional Lymph Node (N)
Remote Metastasis (M)
Stage 0 Carcinoma in situ (Tis) N0 M0
Stage I
Tumor may invade submucosa (T1) or muscularis propria (T2)
N0
M0
Stage II
Tumor invades muscularis (T3) or adjacent organs or structures (T4)
N0
M0
Stage IIA T3 N0 M0
Stage IIB T4a N0 M0
Stage IIC T4b N0 M0
Stage IIIA T1-4 N1-2 M0
Stage IIIB T1-4 N1-2 M0
Stage IIIC T3-4 N1-2 M0
Stage IVA T1-4 N1-3 M1a
Stage IVB T1-4 N1-3 M1b
Prognostic factors associated with staging
Patient prognosis is a function of clinical and histopathologic stage of colon cancer at diagnosis. In
addition to the well-established significance of standard pathological features such as depth of bowel
wall penetration (T), number of locoregional lymph nodes involved (N), and presence of extra-colonic
metastases (M), several other factors have been proven to be of importance (see list below). These
include number of harvested and processed lymph nodes, histologic grade, and evidence of
lymphovascular and perineural invasion.
Bowel obstruction at diagnosis, ulcerative growth pattern, perforation, and elevated preoperative
CEA level have all been shown to be associated with worse prognosis. Molecular prognostic factors
such as p53, loss of heterozygosity for 18q,[10 ]mutations of deleted in colon cancer gene (DCC),
EGFR amplification, and KRAS mutations have all been investigated but are not currently used as
prognostic factors in standard clinical practice.
Deficient mismatch repair (dMMR), which is associated with high frequency microsatellite instability
(H-MSI), has been recently shown to be associated with better clinical outcome for patients with
resectable colon cancer; this was based on a retrospective analysis of several large randomized
trials of adjuvant therapy for colon cancer.[11,12 ]In addition, it appears that patients with dMMR (H-MSI)
did not benefit from fluorouracil-based adjuvant therapy.[13 ]This may become a useful test for
prognosis and treatment planning in patients with resectable colon cancer.
Selected prognostic factors and 5-year relapse-free survival in patients with colorectal cancer, based
on the Mayo Clinic calculator (http://www.mayoclinic.com/calcs) for population of patients aged 60-69
years (data regarding numbers of lymph nodes analyzed is from Le Voyer el al, 2003[14 ]) are as
follows (prognostic factor, 5-year relapse-free survival):
T3N0 (11-20) nodes analyzed – 79%

T3N0 low grade – 73%
T3N0 (≤ 10 lymph nodes examined) – 72%
T3N0 high grade – 65%
T4N0 low grade – 60%
T4N0 high grade – 51%
T3N1 – 49%
T3N2 – 15%
A review of Surveillance, Epidemiology, and End Results (SEER) population-based data on colon
cancer by the AJCC Hindgut Taskforce found that that T1-2N2 cancers have a better prognosis than
T3-4N2,T4bN1 have a similar prognosis to T4N2, T1-2N1 have a similar prognosis to T2N0/T3N0,
and T1-2N2a have similar prognosis to T2N0/T3N0 (T1N2a) or T4aN0 (T2N2a); in addition,
prognosis for T4a lesions is better than T4b by N category. The number of positive nodes affects
prognosis. The Taskforce proposed the following revisions of the TN categorization for colon cancer[15
]:
Shift T1-2N2 lesions from IIIC to IIIA/IIIB
Shift T4bN1 from IIIB to IIIC
Subdivide T4/N1/N2
Revise substaging of stages II/III.
Treatment
Medical Care
Systemic chemotherapy
5-Fluorouracil remains the backbone of chemotherapy regimens for colon cancer, both in the
adjuvant and metastatic setting. In the past 10 years, it was established that combination regimens
provide improved efficacy and prolonged progression-free survival in patients with metastatic colon
cancer. In addition to 5-fluorouracil, oral fluoropyrimidines such as capecitabine (Xeloda) and tegafur
are increasingly used as monotherapy or in combination with oxaliplatin (Eloxatin) and irinotecan
(Camptosar). Some of the standard combination regimens employ prolonged continuous infusion of
fluorouracil (FOLFIRI, FOLFOX)[16 ]or capecitabine (CAPOX, XELOX, XELIRI). Availability of new
classes of active drugs and biologics for colorectal cancer pushed the expected survival for patients
with metastatic disease from 12 months 2 decades ago to about 22 months currently.
A meta-analysis of 6 randomized phase II and II trials examined the efficacy of capecitabine with
oxaliplatin (CAP/OX) compared with fluorouracil with oxaliplatin (FU/OX) in metastatic colorectal
cancer. CAP/OX resulted in a lower response rate but overall progression-free survival and overall
survival were not affected and were similar in both treatment regimens. Characteristic toxicity
occurred in the FU schedules and thrombocytopenia and hand-foot syndrome were more prominent
in the CAP regimens.[17 ]
In a phase III multicenter trial, Kim et al compared overall survival of second-line therapy for patients
with advanced colorectal carcinoma refractory to fluorouracil. Fluorouracil, leucovorin, and oxaliplatin
(FOLFOX4) (n=246) versus irinotecan (n=245) was compared (crossover to the other treatment was
mandated if disease progression occurred). Overall survival did not significantly differ between
FOLFOX4 and irinotecan; however, FOLFOX 4 improved response rate (RR) and time to progression
(TTP) compared with irinotecan (P=0.0009 for each RR and TTP). FOLFOX4 was associated with
more neutropenia and paresthesias.[18 ]

Key clinical questions relate to the most advantageous selection of drug combination and the
sequence of different treatment options in individual patients with colorectal cancer. This information
is to be derived from information on tumor biology, patient performance status, organ function, and
pharmacogenomics testing.
Adjuvant (postoperative) chemotherapy
The standard therapy for patients with stage III and some patients with stage II colon cancer for the
last 2 decades consisted of fluorouracil in combination with adjuncts such as levamisole and
leucovorin.[19,20,21 ]This approach has been tested in several large randomized trials and has been
shown to reduce individual 5-year risk of cancer recurrence and death by about 30%.
Two recent large randomized trials (MOSAIC and NASBP-C06) investigated the addition of
oxaliplatin to fluorouracil (FOLFOX4 and FLOX, respectively) and demonstrated a significant
improvement in 3-year disease-free survival for patients with stage III colon cancer. The addition of
irinotecan to fluorouracil in the same patient population provided no benefit based on the results from
two large randomized trials (CALGB 89803 and PETACC 3). Another randomized study, XACT,
demonstrated noninferiority of capecitabine (Xeloda) compared to 5-FU/leucovorin as adjuvant
therapy for patients with stage III colon cancer. A large trial comparing capecitabine plus oxaliplatin
(XELOX) versus FOLFOX has completed accrual, but survival data have not yet been reported.
The role of adjuvant chemotherapy for stage II colon cancer is controversial. A large European trial
(QUASAR) demonstrated small but significant benefit (3.6%) in terms of absolute 5-year survival rate
for those patients who received 5-fluorouracil/leucovorin versus those in the control group. Ongoing
adjuvant trials are investigating additional risk stratification of stage II colon cancer based on
clinicopathological and molecular markers (ECOG 5202 trial).
Though information on results of adjuvant therapy in stage II and III colon cancer is limited, a data set
assembled by the Adjuvant Colon Cancer Endpoints group with fluorouracil-based adjuvant therapy
was recently analyzed. The authors concluded that adjuvant chemotherapy provides significant
disease-free survival benefit because it reduces the recurrence rate particularly within the first 2
years of adjuvant therapy but with some benefit in years 3-4.[22 ]
Biologic agents
Bevacizumab (Avastin) was the first anti-angiogenesis drug to be approved in clinical practice and
the first indication was for metastatic colorectal cancer. This is a humanized monoclonal antibody to
vascular endothelial growth factor (VEGF) and a pivotal trial demonstrated improved progression-free
and overall survival when bevacizumab was added to chemotherapy (IFL, fluorouracil plus
irinotecan).
A pooled analysis of cohorts of older patients (aged 65 years or older) from 2 randomized clinical
trials examined the benefit of bevacizumab plus fluorouracil-based chemotherapy in first-line
treatment of metastatic colorectal cancer. The study concluded that adding bevacizumab to
fluorouracil-based chemotherapy improved overall survival and progression-free survival in older
patients as it does in younger patients, without increased risks of treatment in the older age group.[23 ]
Two other biologic agents approved for colorectal cancer are epidermal growth factor receptor
(EGFR)-targeted monoclonal antibodies. Cetuximab (Erbitux) is a chimeric monoclonal antibody
approved as monotherapy or in combination with irinotecan (Camptosar) in patients with metastatic
colorectal cancer refractory to fluoropyrimidine and oxaliplatin therapy.[24 ]

Panitumumab (Vectibix) is fully human monoclonal antibody and the current indication as a
monotherapy for patients with colorectal cancer in whom combination chemotherapy failed or was
not tolerated. A recent trial by Hecht et al evaluated panitumumab added to bevacizumab and
chemotherapy (oxaliplatin- and irinotecan-based) as first-line treatment of metastatic colorectal
cancer and concluded that the addition of panitumumab resulted in increased toxicity and decreased
progression-free survival.[25 ]
Two clinical trials investigated the role of panitumumab (fully human monoclonal antibody against the
EGFR) in the first-line[26 ]and in second-line[27 ]in combination with chemotherapy (FOLFOX and
FOLFIRI). The results of both studies suggest clinical benefit of adding panitumumab to
chemotherapy for patients with wild-type KRAS colorectal cancer, in terms of improving progression-
free survival (PFS) and response rate. Panitumumab becomes an option, or an alternative to
cetuximab, for those patients who have tumors without KRAS mutation. No head-to-head
comparisons between panitumumab containing combinations versus cetuximab or even
bevacizumab (anti-VEGFR monoclonal antibody) chemotherapy combinations in patients with wild-
type KRAS tumors have been reported, leaving it up to the oncologist to prioritize the choice or
sequence of monoclonals in this patient population.
Intratumoral KRAS gene mutation can predict sensitivity to anti-EGFR antibodies.[28 ]Investigators
from a large international trial exploring the benefit of adding cetuximab to first-line chemotherapy
with FOLFIRI (CRYSTAL Trial) reported that only patients with wild-type KRAS derived clinical
benefit from cetuximab. Patients with mutant KRAS had no clinical benefit from adding cetuximab to
chemotherapy and experienced only unnecessary toxicity. KRAS mutations are present in about 40%
of colon adenocarcinomas. Based on these results, testing for KRAS mutation has been already
added to cetuximab indication by European regulatory agency (EMEA) and is expected to be added
to United States indication by the FDA as well.
Bokemeyer et al examined the overall response rate when combining cetuximab with oxaliplatin,
leucovorin, and fluorouracil (FOLFOX-4), as opposed to the regimen without cetuximab, for first-line
treatment of metastatic colorectal cancer in a randomized study. They also examined the influence of
the KRAS mutation status. They concluded that the overall response rate for cetuximab plus
FOLFOX-4 was higher than with FOLFOX-4 alone though a statistically significant increase in odds
for a response with the addition of cetuximab could not be established, except in patients with KRAS
wild-type tumors, for whom the addition of cetuximab increased chance of response and lowered risk
of disease progression.[29 ]
Other mutations that involve some of the kinases downstream from KRAS (such as BRAF and PI3K)
are being investigated and may result in even more selective methods to identify patients that may
benefit from EGFR inhibition.
Radiation therapy
While radiation therapy remains a standard modality for patients with rectal cancer, the role of
radiation therapy is limited in colon cancer. It does not have a role in the adjuvant setting, and in
metastatic settings, it is limited to palliative therapy for selected metastatic sites such as bone or
brain metastases. Newer, more selective ways of administering radiation therapy such as
stereotactic radiotherapy (CyberKnife) and tomotherapy are currently being investigated and may
extend indications for radiotherapy in the management of colon cancer in the future.
A prospective, multicenter, randomized phase III study by Hendlisz et al compared the addition of
yttrium-90 resin to a treatment regimen of fluorouracil 300 mg/m2 IV infusion (days 1-14 q8wk) with
fluorouracil IV alone. Yytrium-90 was injected intra-arterially into the hepatic artery. Findings showed

that the addition of radioembolization with yytrium-90 significantly improved time to liver progression
and median time to tumor progression.[30 ]
Surgical Care
Surgery is the only curative modality for localized colon cancer (stage I-III) and potentially provides
the only curative option for patients with limited metastatic disease in liver and/or lung (stage IV
disease). The general principles for all operations include removal of the primary tumor with
adequate margins including areas of lymphatic drainage.
For lesions in the cecum and right colon, a right hemicolectomy is indicated. During a right
hemicolectomy, the ileocolic, right colic, and right branch of the middle colic vessels are
divided and removed. Care must be taken to identify the right ureter, the ovarian or testicular
vessels, and the duodenum. If the omentum is attached to the tumor, it should be removed
en bloc with the specimen.
For lesions in the proximal or middle transverse colon, an extended right hemicolectomy can
be performed where the ileocolic, right colic, and middle colic vessels are divided and the
specimen is removed with its mesentery.
For lesions in the splenic flexure and left colon, a left hemicolectomy is indicated. The left
branch of the middle colic vessels, the inferior mesenteric vein, and the left colic vessels
along with their mesenteries are included with the specimen.
For sigmoid colon lesions, a sigmoid colectomy is appropriate. The inferior mesenteric artery
is divided at its origin, and dissection proceeds toward the pelvis until adequate margins are
obtained. Care must be taken during dissection to identify the left ureter and the left ovarian
or testicular vessels.
Total abdominal colectomy with ileorectal anastomosis may be required for patients who
have been diagnosed with HNPCC, attenuated familial adenomatous polyposis, and
metachronous cancers in separate colon segments or at times in acute malignant colon
obstructions with unknown status of the proximal bowel.
The advent of laparoscopy has revolutionized the surgical approach of colonic resections for
cancers. The same oncologic principles are respected. Large prospective randomized trials have
demonstrated that there are no significant differences with regard to intraoperative or postoperative
complications, perioperative mortality rates, readmission or reoperation rates, or rate of surgical
wound recurrence. At a median follow-up of 7 years, no significant differences existed in the 5-year
disease-free survival rate (69% versus 68% in the laparoscopy-assisted colectomy [LAC] and open
colectomy groups, respectively) or overall survival (76% versus 75%). Overall laparoscopic
colectomy provides comparable oncologic outcomes (cause-specific survival, disease recurrence,
number of lymph nodes harvested) to those achieved with an open approach.[31,32,33,34,35,36 ]
Standard management of patients with metastatic disease is systemic chemotherapy. The proper
use of elective colon/rectal resections in nonobstructed patients with stage IV disease is a source of
continuing debate. Medical oncologists properly note the major drawbacks to palliative resection,
such as loss of performance status and risks of surgical complications that potentially lead to delay in
chemotherapy. However, surgeons understand that elective operations have lower morbidity than
emergent operations on patients who are receiving chemotherapy. Only randomized prospective
data could eventually demonstrate the survival benefit of palliative resection for patients with stage IV
colon cancer. Data presented at the American Society of Clinical Oncology 45th Annual Meeting in
2009 indicated that patients with asymptomatic surgically incurable colorectal cancer do not require
immediate surgery for primary tumor removal.[37 ]
During the past decade, colonic stents have introduced an effective method of palliation for
obstruction in patients with unresectable liver metastasis.

Curative intent resections of liver metastases have significantly improved long-term survival with
acceptable postoperative morbidity. A multivariate analysis of 1001 patients who underwent
potentially curative resection of liver metastases identified 5 factors as independent predictors of
worse outcome: size greater than 5 cm, disease-free interval of less than a year, more than one
tumor, primary lymph-node positivity, and CEA greater than 200 ng/mL.[38 ]
Although resection is the only potentially curative treatment for patients with colon metastases, other
therapeutic options, for those who are not surgical candidates, include thermal ablation techniques.
Cryotherapy uses probes to freeze tumors and surrounding hepatic parenchyma. It requires
laparotomy and can potentially have significant morbidity including liver cracking, thrombocytopenia,
and disseminated intravascular coagulation (DIC). Radiofrequency ablation (RFA) uses probes that
heat liver tumors and the surrounding margin of tissue to create coagulation necrosis. RFA can be
performed percutaneously, laparoscopically, or through an open approach. Although RFA has
minimal morbidity, local recurrence is a significant problem and is correlated with tumor size. Hepatic
arterial infusion (HAI) of chemotherapeutic agents such as FUDR is a consideration following partial
hepatectomy.
Standard colectomies for adenocarcinoma of the colon are depicted in the image below.


Standard colectomies for adenocarcinoma of the colon.
Consultations
Surgical consultation o Colorectal cancer, especially early stage disease, can be cured surgically.
Following diagnosis and staging, obtaining surgical consultation for the possibility of
resection may be appropriate. After surgery, the stage of the tumor may be
advanced depending on the operative findings (eg, lymph node involvement,
palpable liver masses, peritoneal spread). o In the care of patients with colorectal cancer and isolated liver metastases, consider
surgical consultation for possible resection. In some cases, resection of previously
unresectable liver metastases may become feasible after cytoreduction with
neoadjuvant chemotherapy. Therefore, ongoing involvement of the surgical
oncologist is very important in patient care, even if the tumor is not considered
resectable at the time of diagnosis. o In advanced disease, surgical intervention may be helpful in palliative care of
bleeding or obstruction.
Gastroenterology consultation o Gastroenterology consultation is critical for screening of high-risk individuals (ie,
people with family history of colorectal cancer or polyposis syndromes) and those
individuals who are found to be inappropriately iron deficient or to have occult blood
on screening fecal examination. A colonoscopy or sigmoidoscopy is necessary to
visualize the colon endoscopically, to obtain biopsies, or to resect polyps. GI
consultation may be necessary in the management of advanced disease. Recent
advent of colorectal stents allows a nonsurgical management of impending
obstruction in patients who present with unresectable, metastatic disease. o GI consultation is necessary in the follow-up of patients after surgical resection and
adjuvant chemotherapy. Patients must be screened for recurrent disease in the
colon by colonoscopic examination at 1 year after surgery and then every 3 years.
Diet
Abundant epidemiological literature suggests association of risk for developing colorectal cancer with
dietary habits, environmental exposures, and level of physical activity. Less is known about effect of
diet and physical activity on the recurrence of colon cancer. A prospective observational study
involving patients from the CALGB 89803 adjuvant trial demonstrated adverse effect with regards to
risk for recurrence and increased mortality for patients following a "Western" diet (high intake of red
meat, refined grains, fat, and sweets) compared to patients with a "prudent" diet (high intake of fruits
and vegetables, poultry, and fish).
In another observational study from the same cohort of patients, patients were prospectively
monitored and physical activity was recorded. The study concluded that physical activity reduces the
risk of recurrence and mortality in patients with resected stage III colon cancer.
Kirkegaarde et al reported that adherence to a "healthy life style" recommendations based on
physical activity, waist circumference, smoking, alcohol intake, and diet may significantly reduce
colorectal cancer risk, by about 23%.[39 ]
These interesting and important observations pave the way for future interventional studies involving
diet and physical activity in patients with stage II and III colon cancer.

Activity
See Diet.
Medication
Commonly used combination regimens
Adjuvant therapy
5-Fluorouracil + leucovorin (weekly schedule, low dose leucovorin) o 5-Fluorouracil: 500 mg/m2 IV weekly for 6 weeks
o Leucovorin: 20 mg/m2 IV weekly for 6 weeks, administered before 5-fluorouracil
o Repeat cycle every 8 weeks for a total of 24 weeks.
LV5FU2 (de Gramont regimen) o 5-Fluorouracil: 400 mg/m2 IV bolus, followed by 600 mg/m2 IV continuous infusion
for 22 hours on days 1 and 2 o Leucovorin: 200 mg/m2 IV on days 1 and 2 as a 2-hour infusion before 5-fluorouracil
o Repeat cycle every 2 weeks for a total of 12 cycles.
Oxaliplatin + 5-fluorouracil + leucovorin (FOLFOX4) o Oxaliplatin: 85 mg/m2 IV on day 1
o 5-Fluorouracil: 400 mg/m2 IV bolus, followed by 600 mg/m2 IV continuous infusion
for 22 hours on days 1 and 2 o Leucovorin: 200 mg/m2 IV on days 1 and 2 as a 2-hour infusion before 5-fluorouracil
o Repeat cycle every 2 weeks for a total of 12 cycles.
Metastatic disease
Irinotecan + 5-fluorouracil + leucovorin (FOLFIRI regimen) o Irinotecan: 180 mg/m2 IV on day 1
o 5-Fluorouracil: 400 mg/m2 IV bolus on day 1, followed by 2400 mg/m2 IV continuous
infusion for 46 hours o Leucovorin: 400 mg/m2 IV on day 1 as a 2-hour infusion, prior to 5-fluorouracil
o Repeat cycle every 2 weeks.
Oxaliplatin + 5-fluorouracil + leucovorin (FOLFOX6) o Oxaliplatin: 100 mg/m2 IV on day 1
o 5-Fluorouracil: 400 mg/m2 IV bolus on day 1, followed by 2400 mg/m2 IV continuous
infusion for 46 hours o Leucovorin: 400 mg/m2 IV on day 1 as a 2-hour infusion, before 5-fluorouracil
o Repeat cycle every 2 weeks.
Oxaliplatin + 5-fluorouracil + leucovorin (mFOLFOX7) o Oxaliplatin: 100 mg/m2 IV on day 1
o 5-Fluorouracil: 3000 mg/m2 IV continuous infusion on day 1 for 46 hours
o Leucovorin: 400 mg/m2 IV on day 1 as a 2-hour infusion, before 5-fluorouracil
o Repeat cycle every 2 weeks.
Capecitabine + oxaliplatin (XELOX) o Capecitabine: 850-1000 mg/m2 PO bid on days 1-14
o Oxaliplatin: 100-130 mg/m2 IV on day 1
o Repeat cycle every 21 days.
FOLFOX4 + bevacizumab o Oxaliplatin: 85 mg/m2 IV on day 1

o 5-Fluorouracil: 400 mg/m2 IV bolus, followed by 600 mg/m2 IV continuous infusion
on days 1 and 2 o Leucovorin: 200 mg/m2 IV on days 1 and 2 as a 2-hour infusion before 5-fluorouracil
o Bevacizumab: 10 mg/kg IV every 2 weeks
o Repeat cycle every 2 weeks.
Antineoplastic Agent, Antimetabolite (pyrimidine)
5-Fluorouracil (5-FU, Adrucil, Efudex)
Fluoropyrimidine analog. Cell cycle-specific with activity in the S-phase as single agent and has for
many years been combined with biochemical modulator leucovorin. Mainstay of medical
chemotherapy for colorectal cancer for patients for more than 40 y. Has activity as single agent that
inhibits DNA replication and transcription. Cytotoxicity is cell-cycle nonspecific. Shown to be effective
in adjuvant setting. Classic antimetabolite anticancer drug with chemical structure similar to
endogenous intermediates or building blocks of DNA or RNA synthesis. 5-FU inhibits tumor cell
growth through at least 3 different mechanisms that ultimately disrupt DNA synthesis or cellular
viability. These effects depend on intracellular conversion of 5-FU into 5-FdUMP, 5-FUTP, and 5-
FdUTP. 5-FdUMP inhibits thymidylate synthase (key enzyme in DNA synthesis), which leads to
accumulation of dUMP, which then gets misincorporated into the DNA in the form of 5-FdUTP
resulting in inhibition of DNA synthesis and function with cytotoxic DNA strandbreaks. 5-FUTP is
incorporated into RNA and interferes with RNA processing. Current standard adjuvant therapy for
colon cancer involves combination 5-FU/LV chemotherapy. Saltz regimen (5-FU/LV/CPT11) now
standard first-line therapy for metastatic colon cancer. Because of toxicity, maximum of 400 mg/m2 of
5-FU and 100 mg/m2 of CPT11 can be used as starting dose. Levamisole is no longer an appropriate
component of adjuvant therapy.
Dosing
Adult
Bolus schedule: 425–600 mg/m2 weekly, with or without leucovorin
Protracted (pump) infusion: 200-300 mg/m2/24 h continuously
46 hour infusion (pump): 2400–3000 mg/m2/46 h, repeat every 14 days
Standard therapy: 500 mg/m2 IV weekly for 4 wk q6wk
Adjuvant therapy
Mayo Clinic regimen: 425 mg/m2/d IV bolus on days 1-5 after LV for 5 d every 4 wk; 6 mo of therapy
is current practice
Roswell Park regimen: Continuous infusion weekly for 6 wk; 2 wk off
Pediatric
Not established
Interactions
Increased risk of bleeding with anticoagulants, NSAIDs, platelet inhibitors, thrombolytic agents;
enhanced bone marrow toxicity with other immunosuppressive agents
Contraindications

Documented hypersensitivity, bone marrow suppression, serious infection, topical administration
contraindicated in pregnancy
Precautions
Pregnancy
D - Fetal risk shown in humans; use only if benefits outweigh risk to fetus
Precautions
Nausea, oral and GI ulcers, depression of immune system, and hemopoiesis failure (bone marrow
suppression) may occur; adjust dosage in renal impairment
Toxic effects include diarrhea, mucositis, myelosuppression, hand-foot syndrome (palmar-plantar
erythrodysesthesia), dry skin, hyperpigmentation, neurological toxicity (cerebellar ataxia), cardiac
toxicity
Capecitabine (Xeloda)
Fluoropyrimidine carbamate prodrug from of 5-fluorouracil (5-FU). Capecitabine itself is inactive.
Undergoes hydrolysis in liver and tissues to form the active moiety (fluorouracil), inhibiting
thymidylate synthetase, which in turn blocks methylation of deoxyuridylic acid to thymidylic acid. This
step interferes with DNA and to a lesser degree with RNA synthesis.
Dosing
Adult
1250 mg/m2 PO q12h pc for 2 wk followed by 1 wk of rest period; administer as 3-wk cycle
Pediatric
Not established
Interactions
Aluminum/magnesium hydroxide antacids or meals increase drug absorption; increased risk of
bleeding with anticoagulants (monitor INR and PT frequently), NSAIDs, platelet inhibitors,
thrombolytic agents; enhanced bone marrow toxicity with other immunosuppressive agents;
coadministration with leucovorin may cause diarrhea, dehydration, and death from severe
enterocolitis; may increase phenytoin levels
Contraindications
Documented hypersensitivity to drug or related products; severe renal impairment (CrCl <30
mL/min); dihydropyrimidine dihydrogenase (DPD) deficiency
Precautions
Pregnancy
D - Fetal risk shown in humans; use only if benefits outweigh risk to fetus
Precautions
Adjust dose in moderate renal impairment (CrCl 30-50 mL/min); discontinue drug if intractable
diarrhea, bone marrow suppression, myocardial ischemia, or stomatitis develop; caution in patients
that have received extensive pelvic radiation or alkylating therapy; hand and foot syndrome

characterized by numbness, dysesthesia/paresthesia, tingling, erythema, blistering, severe pain,
desquamation, and painless or painful swelling may occur
Toxic effects include diarrhea, hand-foot syndrome, nausea and vomiting, elevations in bilirubin and
transaminases, myelosuppression, neurologic syndrome (cerebellar ataxia), cardiac toxicity
Antidote, Folic Acid Antagonist
Leucovorin (Folinic acid, Citrovorum Factor)
Reduced form of folic acid that does not require enzymatic reduction reaction for activation. Allows
for purine and pyrimidine synthesis, both of which are needed for normal erythropoiesis. Current
standard therapy for colon cancer involves combination chemotherapy. Binds to and stabilizes
ternary complex of FdUTP (intracellular active metabolite of fluoropyrimidines) and thymidylate
synthetase (TS), augmenting cytotoxic effects of 5-fluorouracil. Used as an adjunct to fluorouracil.
Dosing
Adult
20-400 mg/m2 IV in combination with 5-fluorouracil
Standard therapy: 20 mg/m2 IV every wk for 4 wk q6wk
Adjuvant therapy: 20 mg/m2 IV before 5-FU on days 1-5 for 5 d q4wk (Mayo Clinic regimen); 6 mo of
therapy is current practice
Pediatric
Not established
Interactions
Decreases effect of methotrexate, phenytoin, phenobarbital, sulfamethoxazole and trimethoprim
combinations; increases toxicity of fluorouracil
Contraindications
Documented hypersensitivity; pernicious anemia or vitamin deficient megaloblastic anemias
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Do not administer intrathecally or intraventricularly
Toxic effects include skin rash, pruritus, facial flushing, and nausea and vomiting
Antineoplastic Agent, Miscellaneous
Irinotecan is a topoisomerase I inhibitor.
Irinotecan (Camptosar, CPT-11)

Semisynthetic derivative of camptothecin, an alkaloid extract from the Camptotheca acuminate tree.
Inactive in its parent form. Converted by the carboxylesterase enzyme to its active metabolite from,
SN-38.
SN-38 binds to and stabilizes the topoisomerase I-DNA complex and prevents the relegation of DNA
after it has been cleaved by topoisomerase I, inhibiting DNA replication. Effective in treatment of
colorectal cancer. Current standard therapy for metastatic colon cancer involves combination of 5-
FU/LV/CPT11 chemotherapy (see Standard Therapy).
Because of toxicity problems associated with Saltz regimen (5-FU/LV/CPT11), now standard first-line
therapy for metastatic colon cancer, maximum of 400 mg/m2 of 5-FU and 100 mg/m2 of CPT11 can
be used as starting dose.
Dosing
Adult
Monotherapy:
125 mg/m2 IV over 90 min weekly for 4 wk, followed by a 2-wk rest; schedule can be modified to 2 wk
followed by a 1-wk rest
300-350 mg/m2 IV on an every-3-wk schedule
180 mg/m2 IV as monotherapy or in combination with infusional 5-FU/LV on an every-2-wk schedule
Pediatric
Not established
Interactions
Concomitant administration with other antineoplastics may result in prolonged neutropenia and
thrombocytopenia in addition to increased morbidity/mortality
Contraindications
Documented hypersensitivity, severe diarrhea, febrile neutropenia, unresponsive or progressive
adenocarcinoma, and pregnancy
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Adverse effects include myelosuppression, alopecia, nausea, vomiting, and diarrhea (early and late),
and elevations in transaminases and bilirubin; monitor bone marrow function
Antineoplastic Agent, Alkylating Agent
Oxaliplatin is a platinum analog.
Oxaliplatin (Eloxatin, Diaminocyclohexane platinum, DACH-platinum)
Third-generation platinum-based antineoplastic agent used in combination with an infusion of 5-
fluorouracil (5-FU) and leucovorin for treatment of metastatic colorectal cancer in patients with
recurrence or progression following initial treatment with irinotecan, 5-FU, and leucovorin. Also
indicated for previously untreated advanced colorectal cancer in combination with 5-FU and

leucovorin. Covalently binds to DNA with preferential binding to the N-7 position of guanine and
adenine. DNA mismatch repair enzymes are unable to recognize oxaliplatin-DNA adducts in contrast
with other platinum-DNA adducts as a result of their bulkier size. Forms interstrand and intrastrand
Pt-DNA crosslinks that inhibit DNA replication and transcription. Cytotoxicity is cell-cycle nonspecific
with activity in all phases of the cell cycle.
Dosing
Adult
Day 1: 85 mg/m2 IV over 2 h; administer simultaneously with leucovorin 200 mg/m2; followed by 5-FU
400 mg/m2 IV bolus over 2-4 min, then 5-FU 600 mg/m2 IV continuous infusion in 500 mL D5W over
22 h
Day 2: Leucovorin 200 mg/m2 IV over 2 h, followed by 5-FU 400 mg/m2 IV bolus over 2-4 min, then 5-
FU 600 mg/m2 IV as a continuous infusion in 500 mL D5W over 22 h
Oxaliplatin can also be administered at 130 mg/m2 IV on a q3wk schedule
Pediatric
Not established
Interactions
May increase 5-FU serum concentration by approximately 20%
Contraindications
Documented hypersensitivity to oxaliplatin or other platinum compounds (allergic reactions may
present with facial flushing and rash, pneumonitis)
Precautions
Pregnancy
D - Fetal risk shown in humans; use only if benefits outweigh risk to fetus
Precautions
Anaphylaxis may occur within minutes of administration; may cause neurotoxicity with acute and
chronic forms (acute toxicity seen in 80-85% of all patients and is characterized by a peripheral
sensory neuropathy with distal paresthesias, visual and voice changes, often triggered or
exacerbated by exposure to cold), pulmonary fibrosis, bone marrow suppression, GI tract symptoms
(eg, nausea, vomiting, diarrhea, stomatitis), renal or hepatic toxicity (decrease dose), or
thromboembolism, myelosuppression; dilute IV only in dextrose-containing solution
Antineoplastic Agent, Monoclonal Antibody
Cetuximab (Erbitux)
Recombinant, human/mouse chimeric monoclonal antibody that specifically binds to the extracellular
domain of human epidermal growth factor receptors (EGFR, HER1, c-ErbB-1). Cetuximab-bound
EGF receptor inhibits activation of receptor-associated kinases, resulting in inhibition of cell growth,
induction of apoptosis, and decreased production of matrix metalloproteinase and vascular
endothelial growth factor.
Indicated for treating irinotecan-refractory, EGFR-expressed, metastatic colorectal carcinoma.

Treatment is preferably combined with irinotecan. May be administered as monotherapy if irinotecan
is not tolerated.
Dosing
Adult
First dose: 400 mg/m2 IV infused over 2 h
Weekly maintenance doses: 250 mg/m2 IV infused over 1 h
Not to exceed infusion rate of 10 mg/min (ie, 5 mL/min);
must administer with low-protein–binding 0.22 μ m in-line filter; premedication with an H1 antagonist
(eg, diphenhydramine 50 mg IV) recommended
Pediatric
Not established
Interactions
Limited data exist; none reported
Contraindications
None for metastatic colorectal carcinoma
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Caution with documented hypersensitivity, including allergy to murine proteins; may cause infusion-
related hypotension and airway distress (eg, bronchospasm, stridor, hoarseness), particularly with
the first infusion (90%); premedicate with diphenhydramine 50 mg IV; decrease dose with mild or
moderate (grade 1 or 2) infusion reaction and immediately and permanently discontinue with severe
(grade 3 or 4) infusion reactions; common adverse effects include acnelike rash, dry skin, pruritus,
tiredness or weakness, fever, diarrhea, constipation, abdominal pain, hypomagnesemia, infusion
reaction, paronychia, hypertrichia; may rarely cause interstitial lung disease; do not shake or dilute
solution; sunlight can exacerbate any skin reactions
Bevacizumab (Avastin)
Indicated in combination with a fluoropyrimidine-based chemotherapy as a first-line or second-line
treatment for metastatic colorectal cancer. Murine derived monoclonal antibody that inhibits
angiogenesis by targeting and inhibiting vascular endothelial growth factor (VEGF). Inhibiting new
blood vessel formation denies blood, oxygen, and other nutrients needed for tumor growth. Used in
combination with standard chemotherapy.
Dosing
Adult
5-10 mg/kg IV over 60 min q2wk until disease progression detected

Pediatric
Not established
Interactions
Coadministration with 5-fluorouracil increases incidence (2-fold) of serious and fatal arterial
thromboembolic events (ie, CVA, MI, TIAs, angina)
Contraindications
Documented hypersensitivity
Precautions
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Common adverse effects include hypertension, epistaxis, fatigue, thrombosis, increased risk of
bleeding, diarrhea, leukopenia, proteinuria, nephritic syndrome, headache, anorexia, and stomatitis;
may cause serious or fatal, but rare events including gastrointestinal perforation, intra-abdominal
infections, impaired wound healing, hemoptysis (particularly with lung cancers), reversible posterior
leukoencephalopathy syndrome (RPLS), nasal septum perforation, and internal bleeding; increases
risk of serious and fatal arterial thrombotic events with 5-fluorouracil
Do not initiate treatment for at least 28 days following major surgery, the surgical incision should be
fully healed; breastfeeding should be discontinued during and for at least 20 d following treatment
with bevacizumab
Panitumumab (Vectibix)
Recombinant human IgG2 kappa monoclonal antibody that binds to human epidermal growth factor
receptor (EGFR). Indicated to treat colorectal cancer that has metastasized following standard
chemotherapy.
Dosing
Adult
6 mg/kg IV infused over 60 min q2wk
Pediatric
Not established
Interactions
Data limited; none reported
Contraindications
None known
Precautions
Pregnancy

C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if
benefits outweigh risk to fetus
Precautions
Common adverse effects include rash (acneiform), paronychia, hypomagnesemia, fatigue, abdominal
pain, nausea, and diarrhea, pneumonitis; serious adverse effects include pulmonary fibrosis, severe
rash complicated by infections, infusion reactions (for grade I or II reaction, reduce infusion rate by
50%; for grade III or IV reaction, immediately discontinue permanently), ocular toxicity, abdominal
pain, vomiting, and constipation; administer using low-protein–binding filter
Follow-up
Further Outpatient Care
Pooled analysis form several large adjuvant trials reported that 85% of colon cancer recurrences
occur within 3 years from after resection of primary tumor. Therefore, patients with resected colon
cancer (stage II and III) should undergo regular surveillance for at least 5 years following resection.
An update of American Society of Clinical Oncology (2005) recommends physical examinations
every 3-6 months for the first 3 years, every 6 months during years 4 and 5, and subsequently at the
discretion of physician and based on individual risk assessment.
Serum CEA level should be checked every 3 months in patients with stage II or III disease for at least
3 years and every 6 months in years 4 and 5. Computerized tomography (CT) of the chest and
abdomen should be performed annually for at least 3 years after resection of primary tumor. All
patients with colon cancer should have preoperative or postoperative colonoscopy to document
absence of additional primary colon tumors or polyps. In the absence of high-risk pathology on the
first colonoscopy or increased susceptibility for colon cancer, follow-up colonoscopy should be
performed at 3 years after surgery and then, if normal, once every 5 years thereafter.
Deterrence/Prevention
Colorectal cancer prevention strategies are based on our understanding of colorectal carcinogenesis
and availability of pharmacologic agents that are effective yet minimally toxic. The efficacy of these
agents is usually first tested in high-risk populations.
Celecoxib (Celebrex), a selective cyclooxygenase-2 inhibitor was first tested in patients with familial
adenomatous polyposis (FAP). Celecoxib was effective in decreasing the number and size of polyps
on serial colonoscopies, which was the primary surrogate endpoint for this trial. The drug was
approved for FAP patients, although it remains to be seen if this intervention translates to reduced
cancer incidence and prolonged survival.
Other NSAIDs, such as sulindac and nonselective cyclooxygenase inhibitors were tested in lower risk
populations. Enthusiasm for cyclooxygenase-2 inhibitors as chemopreventive agents has dampened
because of a high incidence of cardiovascular toxicity (rofecoxib) in trial patients. An aspirin
prevention trial suggested a benefit in terms of polyp prevention with low-dose (81 mg) aspirin. Some
recent trials focused on combined inhibition of polyamine production and cyclooxygenase
inhibition. A recent report from a large randomized trial of a combination of sulindac and
dimethylformamine (DMFO), an inhibitor of ornithine decarboxylase (ODC), described a dramatic
effect of this combination in reducing polyp recurrence in patients with prior history of colon
polyps. Confirmatory trials are ongoing.[40 ]
Screening

The goal of colorectal cancer screening is to decrease mortality through diagnosis and treatment of
precancerous lesions (adenomatous colon polyps) and early curable cancerous lesions. The
evidence for the importance of early detection and removal of colorectal polyps in
preventing development of invasive cancer is mostly indirect but has been corroborated by data from
many trials.
In the United States, a Joint Guideline was developed by the American Cancer Society, US Multi-
Society Task Force on Colorectal Cancer, and the American College of Radiology. The Guideline
lists appropriate screening procedures and their indications and frequency based on projected
individual risks of developing colorectal cancer.
Their testing options for the early detection of colorectal cancer and adenomatous
polyps for asymptomatic adults aged 50 years and older can be summarized as follows:
Tests that detect adenomatous polyps and cancer o Flexible sigmoidoscopy every 5 years, or
o Colonoscopy every 10 years, or
o Double-contrast barium enema every 5 years, or
o computed tomographic colonography every 5 years
Tests that primarily detect cancer o Annual guaiac-based fecal occult blood test with high test sensitivity for cancer, or
o Annual fecal immunochemical test with high test sensitivity for cancer, or
o Stool DNA test with high sensitivity for cancer, interval uncertain
For individuals who carry an increased or high risk of developing colorectal cancer such as persons
with prior history of polyps, prior history of colorectal cancer, family history of colon cancer, or history
of inflammatory bowel diseases screening should start at an earlier age and be more frequent and
more stringent. Those genetically diagnosed or suspected of having hereditary familial syndromes
such as HNPCC or FAP should be treated as having high risk of developing colon and rectal cancer
and should adhere to a more intense surveillance protocol.[41 ]
Prognosis
The approximate 5-year survival rate for colorectal cancer patients in the United States (all stages
included) is 65%. Survival is inversely related to stage; patients with stage I have a 95% 5-year
survival rate, and those with stage III have only a 60% survival rate. For patients with metastatic,
stage IV disease, the 5-year survival rate is estimated at approximately 10% (see Staging).
Multimedia

Media file 1: Standard colectomies for adenocarcinoma of the colon.
References
Colon, AdenocarcinomaIsaac Hassan, MB, ChB, FRCR, DMRD, Former Senior Consultant Radiologist, Department of Radiology, St Bernard's Hospital, Gibraltar
Updated: Mar 2, 2009
Introduction
Background
Almost all colon cancers are primary adenocarcinomas, which are the third most common cancer in
both men and women in North America and Western Europe.

Cecal carcinoma. A large polypoid cecal mass involves the ileocecal valve and
causes small bowel obstruction.
Colon cancers are the most common gastrointestinal (GI) carcinomas and have the best prognosis.
The 5-year survival rates of approximately 50% may be improved by screening and removal of
adenomatous polyps.[1 ]
Pathophysiology
Tumors of the colon arise as intramucosal epithelial lesions, usually in adenomatous polyps or
glands. As cancers grow, they invade the muscularis mucosa and lymphatic and vascular structures
to involve regional lymph nodes, adjacent structures, and distant sites, especially the liver.[2 ]
Frequency
United States
Colorectal cancer is the third most common cancer diagnosis and the third leading cause of death
from cancer. It is the most common GI cancer. The American Cancer Society has estimated that in
2008, over 148,000 people will be diagnosed with colorectal cancer and about 50,000 will die of
colorectal cancer; 72% will occur in the colon and 28% in the rectum. About 96% colorectal cancers
are adenocarcinomas.[3 ]
The highest rates of the disease are found in the northeastern and north central states, and the
lowest rates are in the southern and western states (except the San Francisco Bay area and Hawaii).
The incidence of colon cancer has risen since 1950, while the incidence of rectal cancer has
remained stable. The increased incidence of colon cancer is believed to be a result of an increased
intake of fat and beef and a decreased intake of fiber.
International
The incidence of colon cancer is highest in the westernized countries of North America, Northern
Europe, Australia, and New Zealand. Intermediate rates are found in Southern Europe, and low rates
are found in Africa, Asia, and South America. A 60-fold difference exists between those areas with
the highest incidence of colon cancer and those areas with the lowest incidence. More than 940,000
new cases of colorectal cancer and nearly 500,000 deaths associated with colorectal cancer are
reported worldwide each year (World Health Organization, 2003).

Mortality/Morbidity
The prognosis of patients with colon cancer relates to the stage of the disease at the time of
diagnosis and to initial treatment. Although a tumor, node, metastasis(TNM)–based international
classification and a computed tomography (CT) staging system have been developed recently, the
Dukes classification (or one of its modifications) is widely used (Table 1, below). Prognosis is also
affected by the histologic grade of the tumor.
The complications of colon cancer include obstruction (common), perforation (uncommon),
intussusception and ischemic colitis proximal to an obstructing tumor (rare), and fistula formation in
the small bowel, bladder, or vagina (rare).
Table 1. Dukes Classification and 5-Year Survival*[4 ]
Stage Description 5-Year Survival
A Limited to the bowel wall 83%
B Extension to pericolic fat; no nodes 70%
C Regional lymph node metastases 30%
D Distant metastases (liver, lung, bone) 10%
*Modified from Zinkin.[ 4 ]
Several factors increase the risk for colonic cancer.
High-fat, low-fiber diet
Patient age greater than 50 years
Personal history of colorectal adenoma or carcinoma (3-fold risk)
First-degree relative with colorectal cancer (3-fold risk)
Familial polyposis coli, Gardner syndrome, and Turcot syndrome (all patients develop
colorectal carcinoma unless they undergo a colectomy)
Juvenile polyposis syndrome, Peutz-Jeghers syndrome, and Muir-Torre syndrome (risk
increased slightly)
Hereditary nonpolyposis colorectal cancer (as many as 50% of patients are affected)
Inflammatory bowel disease o Ulcerative colitis (risk is 30% after 25 years)
o Crohn disease (4- to 10-fold risk)
Race
International incidences reflect dietary differences in fat and fiber intake rather than racial differences.
When a developing country adopts a Western diet, colon cancer rates rise. Similarly, immigrants
from a low-incidence country soon experience the approximate incidence rate of their adopted
country.
Sex
Males and females are equally affected.
Age
Of patients with colon cancer, 90% are older than 50 years. The highest incidence rates are in
individuals aged 70-85 years. Only 10% of patients are younger than 50 years.

Anatomy
The colon is 150 cm long and is subdivided into the cecum and the ascending, transverse,
descending, and sigmoid colons. The ileocecal valve forms the junction between the small and large
bowel and demarcates the cecum from the ascending colon. The transverse and sigmoid colons
have a mesentery and are entirely intraperitoneal. The ascending and descending colons are
partially extraperitoneal.
The superior mesenteric artery supplies the colon between the ileocecal valve and the splenic
flexure. The inferior mesenteric artery supplies the colon distal to the splenic flexure. The colon wall
comprises 4 layers, including the mucosa, submucosa, muscularis propria (inner circular layer and
outer longitudinal layer, comprising 3 narrow bands), and serosa.
Presentation
Colon cancers progress slowly and may be asymptomatic for as many as 5 years; however, patients
usually have occult blood loss from their tumors.
Symptoms depend on the location of the primary tumor. Cancers of the cecum and ascending colon
usually grow larger than left-sided tumors before symptoms occur. Fatigue, shortness of breath, and
angina resulting from microcytic hypochromic anemia are common presenting features. Vague
abdominal discomfort or a palpable mass may occur later, but obstruction is uncommon (unless the
ileocecal junction is involved) because of the larger diameters of the cecum and ascending colon.
Cancers of the descending and sigmoid colons may present with large bowel obstruction. Perforation
is rare but may occur as a result of distention proximal to the tumor (usually in the cecum) or locally
(at the site of the tumor). The primary tumor may be palpable in the abdomen. Overt rectal bleeding
is more common in tumors of the sigmoid colon, whereas occult bleeding is typical with proximal
tumors. A change in bowel habits may be the only presenting feature. Weight loss, jaundice, and
ascites are associated with advanced metastatic disease.[5 ]
Signs and Symptoms:
May be asymptomatic
Microcytic hypochromic anemia (fatigue, shortness of breath, angina)
Vague abdominal discomfort
Change in bowel habit
Palpable mass
Rectal bleeding (overt or occult)
Large bowel obstruction
Perforation (rare)
Jaundice
Ascites
Preferred Examination
Begin the evaluation with a history and physical examination, including a digital rectal
examination.
Inspect the stool, and test for occult blood.
Perform blood tests, including a full blood count, liver function tests, and carcinoembryonic
antigen (CEA) level.
Perform either a sigmoidoscopy (rigid or flexible), along with a double-contrast barium
enema study, or a colonoscopy.

CT scan colonography or virtual colonoscopy, to evaluate the entire colon, is described in
CT scan section of this article.
Limitations of Techniques
Sigmoidoscopy
The 60-cm flexible sigmoidoscope has greater range than the rigid sigmoidoscope, which, at best,
only reaches the distal sigmoid (20 cm).
Double-contrast barium enema
A double-contrast barium enema study detects most colon tumors (80-95%); however, flexible
sigmoidoscopy should precede the barium enema as it is more accurate in detecting small rectal
lesions. The double contrast barium enema has a low perforation rate (1 in 25,000).
Colonoscopy
Colonoscopy detects more adenomatous polyps than a barium enema, and polyps can be excised
during the procedure. Colonoscopy is approximately 3 times more expensive, has a much higher
perforation rate (1 in 1700) than barium enema, and fails to reach the cecum in 5-30% of patients.
Differential Diagnoses
Colitis, Ischemic
Colon, Diverticulitis
Colon, Polyps
Crohn Disease
Tuberculosis, Gastrointestinal
Ulcerative Colitis
Other Problems to Be Considered
Colon lymphoma
Metastases to the colon
Radiography

Polypoid carcinoma. A large, irregular lobulated mass is present in the
rectosigmoid junction.
Annular carcinoma of the sigmoid colon. The lumen of the sigmoid is narrowed
severely by the circumferential mass with mucosal destruction and the
overhanging edges or shouldering at the tumor margins.

Flat carcinoma in the transverse colon. A broad-based contour defect with central
ulceration.
Double-contrast barium enema. 18-mm sessile polyp in the sigmoid colon showing
crescent sign.

Double-contrast barium enema. Stalked 15-mm polyp in sigmoid colon.
Cecal carcinoma. A large polypoid cecal mass involves the ileocecal valve and
causes small bowel obstruction.

Colonic urticaria in ascending colon proximal to obstructing carcinoma in the
hepatic flexure.
Local perforation and paracolic collection in an annular carcinoma of the
descending colon.

Synchronous annular carcinomas in the ascending colon and splenic flexure.
Annular carcinoma of the transverse colon is associated with a 2-cm polyp in the
sigmoid colon.
Findings
Advanced carcinoma
Most colon cancers are relatively advanced, measuring 3-4 cm in diameter at diagnosis. The
appearance of the tumors on double-contrast barium enema reflects the 3 morphologic types:
polypoid, annular, or flat.
Polypoid lesions vary from small, smooth tumors to larger lobulated masses with an irregular
surface and an associated contour deformity along 1 margin of the bowel wall (Image 1).
The incidence of carcinoma in an adenomatous polyp is related to its size and surface
features: larger, more irregular ulcerated lesions are more likely to contain carcinoma.

Annular lesions result from irregular, circumferential masses that severely constrict the
bowel lumen. The margins of the carcinoma show overhanging edges, the tumor shelf or
shoulder (termed "apple-core" lesion). The mucosal folds in the narrowed segment are
destroyed; ulceration may be present (Image 2).
Flat lesions, which are rare, are visualized as a unilateral, broad-based, contour defect.
Ulceration may be present (Image 3). Flat lesions may infiltrate the bowel wall and, if
extensive, cause areas of nondistensibility.
Early carcinoma
Small carcinomas usually present as a polypoid mass with a smooth outline; they may be
indistinguishable from a benign polyp. Rarely, they may present as a small flat lesion (Image 3).
Radiologic appearances
Radiologically, a polypoid mass is visualized either as a filling defect in the barium column (single-
contrast study) or, more commonly, as a barium-coated soft tissue mass protruding into the air-filled
lumen (double-contrast study).
A sessile polyp may be visualized as a crescent (or ring) shadow on the bowel wall (Image 4).
Lobulation is common in polypoid lesions larger than 2 cm in diameter.
Pedunculated polyps have stalks that may be identified easily on profile (Image 5). When the stalk is
seen through the polyp itself, this results in a target (or Mexican hat) appearance. Malignant change
may occur in the head of a stalked polyp. A long (2 cm or more) thin (5 mm or less) stalk may hinder
the spread of carcinoma from the head of the polyp into the wall.
Risk of malignancy
The risk of malignancy in a polyp increases with its size. Risk is less than 1% in polyps with less than
a 1 cm diameter. This risk of malignancy increases to 5% in adenomas of 1-2 cm in diameter.
Patients with polyps larger than 2 cm have a risk of 11-50%. Thus, all polypoid lesions from 0.5-3 cm
require endoscopic removal and histologic examination.
Local complications
Findings that result from complications of the primary tumor include the following:
Obstruction: Large bowel obstruction usually results in an annular carcinoma in the sigmoid
or descending colon. Primary colonic adenocarcinoma accounts for 75% of large bowel
obstruction in adults. Small bowel obstruction may be caused by a cecal lesion involving the
ileocecal valve (Image 6).
Colitis and colonic urticaria: Colitis is a rare complication and occurs proximal to an
obstructing tumor. Colonic urticaria (a term describing confluent, polygonal raised areas)
may be present from submucosal edema caused by the raised intraluminal pressure
proximal to the obstruction (Image 7).
Intussusception: This is rare in adults and usually occurs in polypoidal cecal tumors.
Perforation: A localized perforation caused by tumor necrosis may result in a paracolic
abscess simulating an inflammatory process (Image 8). Perforation also may occur proximal
to an obstructing tumor, usually in the cecum.
Fistulation: A tumor may extend through the bowel wall and invade adjacent organs. Fistulas
also may form between the tumor and adjacent organs.

Synchronous lesions
Approximately 5% of patients with colon cancer have more than 1 cancer at diagnosis (Image 9).
Approximately 35% of patients with colon cancer have an adenomatous polyp (Image 10).
Second tumors are more likely to be overlooked.
Plain abdominal radiography
Plain abdominal radiographs are useful in patients presenting with large bowel obstruction or
perforation.
Free gas below the diaphragm is detected best by plain erect chest radiograph.
Rarely, mucin-producing colon cancers show calcification in the primary tumor and in hepatic and
peritoneal secondary deposits.
Degree of Confidence
Double-contrast barium enema detects approximately 90% of colonic tumors.
The overall detection rate for single-contrast barium enema is approximately 80% but is much lower
for small polypoid tumors. Colonoscopy and biopsy are recommended in patients whose findings are
equivocal.
False Positives/Negatives
False-positive findings
Residual stool may adhere to the bowel wall and mimic a tumor.
The ileocecal valve may mimic a cecal tumor.
A submucosal mass, such as a lipoma, benign mucosal adenoma, or hyperplastic polyp,
may be indistinguishable from a small polypoid cancer.
False-negative findings
Inadequate bowel preparation: Residual stool may obscure a carcinoma. A repeat
examination or colonoscopy is required.
Diverticulosis: When severe sigmoid diverticulosis is present, the incidence of missed
cancers increases.
Diverticulitis: Strictures and paracolic collections may mimic a neoplasm.
Small lesions: Small lesions may be missed in a dense pool of barium.
Errors of perception: These are responsible for more than 50% of cancers that are missed
on barium enema; a second reading performed by a different observer may reduce such
errors.
Multiple cancers: Second lesions are more likely to be overlooked (satisfaction of search
error).
Strictures: Inflammatory bowel disease, ischemic colitis, radiation colitis, and tuberculous
colitis may mimic malignant strictures.
Extrinsic compression: Extrinsic compression of the colon by an adjacent tumor may mimic a
primary colonic tumor.
Prominent peritoneal implants on the surface of the colon: Carcinomatosis from ovarian
cancer or advanced endometriosis, for example, can mimic a primary colonic tumor.

Computed Tomography
Preoperative CT. Cecal wall thickening and infiltration of the pericolic fat.
Preoperative CT. Cecal carcinoma with circumferential involvement of the cecal
wall.
Preoperative CT. Irregular soft tissue mass involving the sigmoid colon. There is
associated diverticular disease.

Enhancing 6 x 4 cm mass from recurrent carcinoma. Note enlarged left iliacus
muscle from malignant involvement.
Barium enema. Typical annular carcinoma in the proximal sigmoid colon with
adjacent diverticular disease (same patient as in Image 13 in Multimedia).
Retroperitoneal lymphadenopathy from cecal carcinoma.

Enlarged portal nodes (observed between inferior vena cava and portal vein);
hepatic metastases.
Contrast-enhanced CT showing liver metastases. Several low-density metastases
from the colonic primary tumor involve both lobes of the liver.

CT scan following a partial hepatectomy for a metastasis in the right lobe.
Chest radiograph. Pulmonary metastases from colon cancer.

CT scan of cerebral metastasis from colon cancer. This is a rare site for metastases
from colonic cancer.
Enhancing mass in rectus sheath from metastasis from colon cancer (same patient
as in Image 14 in Multimedia).
Postradiotherapy inflammatory mass in the left iliac fossa. Note stranding into the
pericolic fat and presacral soft tissue swelling.
Dilated left ureter from inflammatory mass shown in Image 23 in Multimedia.
Findings

Indications for CT scan
CT scan is used for staging colon cancer before surgery, for assessing and staging recurrent
disease, and for detecting the presence of distant metastases.[6,7,8,9,10 ]
Preoperative CT scan is indicated if there is clinical suggestion of distant metastases or local
invasion of the adjacent organs or abdominal wall.
In older patients who may be unable to undergo colonoscopy or barium enema, modified CT scan
may be performed for primary detection of colorectal tumors.
Colonic tumors may be diagnosed on CT scan as an incidental finding.
Tumor staging: CT scan findings of primary colon cancer
CT scan staging (Table 2, below)or TNM staging (Table 3, below) systems may be used to assess
colonic neoplasms.
Table 2. CT Scan Staging System for Colonic Cancer*[11 ]
Stage Description
T1 Intraluminal polypoid mass; no thickening of bowel wall
T2 Thickened colonic wall > 6 mm; no periodic extension
T3a Thickened colonic wall plus invasion of adjacent muscle or organs
T3b Thickened colonic wall plus invasion of pelvic side wall or abdominal wall
T4 Distant metastases, usually liver, lung, or adrenal glands
* Modified from Thoeni.[ 11 ]
Table 3. TNM/Modified Dukes Classification System*[12 ]
TNM Stage Modified Dukes Stage Description
T1 N0 M0 A Limited to submucosa
T2 N0 M0 B1 Limited to muscularis propria
T3 N0 M0 B2 Transmural extension
T2 N1 M0 C1 T2, enlarged mesenteric nodes
T3 N1 M0 C2 T3, enlarged mesenteric nodes
T4 C2 Invasion of adjacent organs
Any T M1 D Distant metastases
*American Joint Committee on Cancer.[ 12 ]
Findings
A localized tumor may be seen on CT scan as an intraluminal or intramural mass of soft tissue
density adjacent to the gas-filled or contrast-filled bowel lumen; this is the appearance of a stage A
tumor (Tables 2 and 3). There is no mural thickening or pericolic fat invasion in stage A tumors. To

opacify the entire bowel, oral water-soluble contrast (1% Gastrografin) is administered at 12 hours
and at 2 hours before examination.
More advanced tumors are associated with thickening of the bowel wall (>6 mm) and infiltration of
the pericolic fat. Thin strands of tissue may extend from the tumor into the pericolic fat (Image 11).
Annular carcinomas are detected by a thickening of the bowel wall and narrowing of the lumen. This
thickening is concentric if the scanning plane is at right angles to the long axis of the bowel (Image
12).
Extracolonic tumor spread is indicated by a loss of tissue fat planes between the colon and
surrounding structures (Image 13). Invaded muscle may be enlarged (Image 14). The comparative
barium enema findings are shown in Image 15. Colonic tumors may invade the anterior abdominal
wall, liver, pancreas, spleen, or stomach.
Complications of the primary tumor
Obstruction, perforation, and fistula formation can be demonstrated by CT scan.
An intussuscepting colonic tumor may have a typical targetlike appearance with alternating rings of
soft tissue and fat on CT scan, if mesenteric fat is present between the intussusceptum and the
intussuscipiens.
A local perforation of a carcinoma may be associated with an extraluminal fluid collection.
N staging
Nodes greater than 10 mm in diameter are considered abnormal. CT scan is unable to distinguish
between enlarged benign nodes and enlarged malignant nodes. Furthermore, malignant foci may be
present in nodes less than 1 cm in diameter. Overall, 60% of affected nodes are detected by CT
scan.
Enlarged nodes may be detected in the mesentery and retroperitoneum (Image 16). Occasionally,
enlarged nodes are observed around the porta hepatis (Image 17).
Rectosigmoid tumors may metastasize to external iliac nodes.
M Staging
Hepatic metastases are the most common site of distant spread. Following injection of intravenous
contrast medium (Image 18), CT scan detects hepatic metastases as well-defined areas of low
density (compared with normal liver parenchyma) in the portal venous phase. In the earlier arterial
phase, hepatic metastases may show rim enhancement or become hyperdense or isodense (in
relation to normal liver).
Hepatic metastases may be suitable for surgical resection if they are small (usually <3 cm), number
fewer than 3, and are suitably located (Image 19), but others are suitable only for intra-arterial
chemotherapy or radiofrequency (RF) ablation (see Intervention).
Other common sites include the lungs, adrenal glands, peritoneum, and omentum.
Although pulmonary metastases may be detected by chest radiograph (Image 20), CT scan has a
higher sensitivity for small pulmonary metastases (<10 mm).

Adrenal metastases may occur in as many as 14% of patients with colon cancer. They manifest with
enlargement (>2 cm), asymmetry, and heterogeneity.
Bony and cerebral metastases are uncommon (Image 21).
Early cancers and polyps
Tumors less than 2 cm in diameter cannot be detected reliably by the standard CT scan technique.
In 1996, Vining introduced CT scan colonography (virtual colonoscopy) as a screening tool for the
detection of colorectal polyps and small cancers.[13 ]This technique involves a 3-dimensional computer
reconstruction from a volumetric data set that uses a workstation as well as distention of a clean
colon with air. Images are read as soft copy from the workstation using a combination of paging
through the 2-D axial images, aided by multiplanar and 3-D endoluminal images.
Multisectional helical scanners have reduced the time required to obtain the images (usually 30
seconds for each series; scans involve the patient in the prone and supine positions, using a reduced
tube current to minimize the radiation dose).
The length of time required for image analysis (currently ranging from 5-30 min) also has decreased
with the introduction of sophisticated software programs that enable a mathematically straightened
colon to be viewed. Advances in computer-aided diagnosis and novel methods of display are
expected to improve the performance of this test and reduce the reading time.
The sensitivity of virtual colonoscopy using multisectional helical scanners is greater than that of the
double-contrast barium enema. For polyps larger than 10 mm, it has a sensitivity of 91% but a
specificity of 76%. Sensitivity falls to 81% for 5- to 10-mm polyps. The examination has the
advantage of displaying incidental extracolonic findings as well. Data from several ongoing
retrospective and prospective multicenter trials are expected in the near future.
Colorectal cancer screening
CT colonography (virtual colonoscopy) has become an acceptable noninvasive option for colorectal
cancer screening that can reliably depict clinically important colorectal lesions. However, substantial
controversy remains regarding its exact role. Recent studies have shown that the sensitivity of CT
colonography may not be as high when performed and interpreted by radiologists who do not have
the required expertise and training. Significant lesions may be missed, and mucosal folds and
residual fecal matter may be misinterpreted as polyps, leading to unnecessary colonoscopy.
CT scan findings in recurrent colorectal cancer
A baseline CT scan study is obtained 3 months following resection of a colonic tumor and
reanastomosis. Recurrent tumor is staged by similar criteria as described above for primary cancers.
There is a local recurrence rate of 20-40% and a distant metastasis rate of approximately 35% after
curative resection. Most of these distant metastases occur within 2 years after surgery.
Although colonoscopy and barium enema reveal better mucosal detail of a local anastomotic
recurrence, CT scan is able to detect recurrence away from the anastomosis as well as
lymphadenopathy and distant metastases. A recurrent tumor mass is typically large and often
extrinsic to the bowel wall (see Images 14 and 22). CT scan criteria of a recurrent tumor include
invasion of adjacent structures, enlargement, and associated lymphadenopathy.
An inflammatory mass following surgery or radiation therapy may mimic a recurrent tumor and may
require biopsy for differentiation. Postoperative soft tissue masses are usually from granulation tissue

but may be the result of a hematoma or abscess. Of these, 60% decrease but 40% may remain
unchanged for up to 2 years. Both recurrent tumor and inflammatory masses can cause
hydronephrosis by ureteric obstruction (see Images 23 and 24).
Degree of Confidence
Degree of Confidence: Colonic lesions smaller than 2 cm usually are not detected. The accuracy and
quality of CT scan studies can be increased using air contrast (rectal air insufflation), smooth muscle
relaxants, and laxatives.
CT scan:
More accurately assesses stage T4 cancers. The spatial resolution of CT scan is too low to
distinguish T2 from T3 lesions.
Has a 50% sensitivity for local invasion; it does not distinguish between direct tumor
infiltration and an inflammatory reaction induced by radiation therapy or surgery (Image 23).
Detects as many as 60% of pericolic nodes. Small nodes (<1 cm in diameter) may contain
tumor and are not detected. Nodes may be enlarged because of other reasons, such as
infection.
Detects 90% of liver metastases as well-defined rounded areas of low density following
intravenous contrast medium (Image 18).
For polyps larger than 10 mm, CT scan colonography (virtual colonoscopy) has a sensitivity of 91%
but a specificity of 76%. Sensitivity falls to 81% for 5- to 10-mm polyps.
False Positives/Negatives
Colon cancer may be indistinguishable from a large benign tumor as well as from metastasis to the
colon (usually from an ovarian primary).
CT scan signs for colon cancer are not specific and may be caused by any disease associated with
focal thickening of the colonic wall. These diseases include diverticulitis, Crohn disease, ischemic
colitis, and tuberculous colitis.
In cachectic patients, the absence of fat planes is a result of nutritional status and not tumor invasion.
A paracolic collection may be seen in diverticulitis, as well as in local perforation of a carcinoma.
Chronic radiation changes in the pelvis may mimic recurrent colonic tumors and require biopsy for
differentiation.
Tumors in the transverse colon and colonic flexures may be visualized incompletely. A primary
gastric carcinoma with extension into the colon may be indistinguishable from a colonic tumor
involving the stomach.
Enlarged lymph nodes may result from inflammation rather than tumor. Lymph nodes of normal size
may contain tumor.
Hypodense hepatic lesions may be caused by simple cysts rather than metastases (Image 18).
Hemangiomas also may cause confusion.
Magnetic Resonance Imaging
Findings

MRI provides greater contrast between soft tissues than CT scan.
Colonic tumors have low signal intensity (similar to adjacent skeletal muscle) on T1-weighted
sequences, which facilitates their differentiation from high-signal perirectal fat. T2-weighted images
are used to detect pelvic sidewall invasion.[14 ]
Tumor enhancement can be achieved by paramagnetic agents such as gadolinium. Gadolinium-
based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine
[MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have
been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing
dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Fibrosing
Dermopathy. The disease has occurred in patients with moderate to end-stage renal disease after
being given a gadolinium-based contrast agent to enhance MRI or MRA scans.
NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches
on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the
whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet;
pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public
Health Advisory or Medscape.
The new technique of MRI colonography can detect colonic polyps greater than 1 cm in diameter and
will compete with CT scan colonography in screening programs.
Degree of Confidence
MRI has lower sensitivity and higher specificity than CT scanning in T staging. The techniques have
a similar overall accuracy in T staging, as well as a similar overall accuracy (approximately 60%) in
the detection of enlarged lymph nodes (N staging) and liver metastasis (M staging).
In detecting local recurrence, MRI has a higher sensitivity (91%) than CT scan (82%) and a higher
specificity (100%) than CT scan (69%).
Nevertheless, most centers tend to use CT scanning rather than MRI for staging and follow-up
imaging of colonic neoplasms because of their greater experience with and the wider availability of
CT scans. In addition, spiral CT scan (and the newer multislice CT scan) can assess the whole
abdomen and pelvis in a much shorter time than MRI.
False Positives/Negatives
Limitations of MRI are similar to those of CT scanning.
Colon cancer may be indistinguishable from a large benign tumor and from metastasis to the colon
(usually from an ovarian primary).
MRI signs for colon cancer are not specific and may be caused by any disease associated with focal
thickening of the colonic wall. These diseases include diverticulitis, Crohn disease, ischemic colitis,
and tuberculous colitis.
A paracolic collection may be seen in diverticulitis, as well as in local perforation of a carcinoma.
Chronic radiation changes in the pelvis may mimic recurrent colonic tumors and require biopsy for
differentiation.

Enlarged lymph nodes may result from inflammation rather than tumor. Lymph nodes of normal size
may contain tumor.
Ultrasonography
Ultrasound scan through the right lobe of the liver showing large hyperechoic
metastasis from colon cancer.
Ultrasound scan of a large cecal carcinoma showing concentric thickening of the
hypoechoic bowel wall by the tumor.

Ultrasound scan demonstrating intussuscepting cecal carcinoma.
Findings
The primary role of ultrasound (US) in patients with colon cancer is the detection of hepatic
metastases.
US has a detection rate of 70-90% for hepatic metastases, which reflects the operator dependence
of this modality, the range of equipment available, and the size of the individual metastasis.
Hepatic metastases from a colonic primary tumor are usually hyperechoic (increased echogenicity in
relation to normal liver; Image 25) but also may be hypoechoic (decreased echogenicity).
On US, a colonic tumor typically appears as an echo-poor mass with a hyperechoic center, which is
known as the target sign (Image 26).
Other findings include localized irregular colonic wall thickening, an irregular contour, lack of normal
peristalsis, and an absence of the normal layered appearance of the colonic wall.
US may detect a colonic tumor as a chance finding or may be used specifically in instances when a
palpable abdominal mass is observed that is consistent with a colonic tumor (Image 26).

Intussuscepting colonic tumors have a characteristic targetlike appearance from concentric rings of
soft tissue and mesenteric-fat density (Image 27).
Degree of Confidence
US usually cannot detect colonic tumors smaller than 2 cm.
US is difficult to use in rectosigmoid lesions.
False Positives/Negatives
US has a high false-negative rate for the detection of colonic tumors, with a sensitivity of 31-80%,
depending on tumor size, and cannot be used as a screening tool.
Conversely, US has a low false-positive rate, with a specificity greater than 90%. US may reduce the
need for more intrusive procedures in older patients and in those with advanced disease. Its primary
role in colon cancer management is to detect hepatic metastases, where it has a detection rate of 70-
90%.
Nuclear Imaging
Findings
Nuclear medicine has a small peripheral role in colon cancer.
Consider using radioimmunoscintigraphy with monoclonal antibody that recognizes CEA or tumor-
associated glycoprotein-72 to detect disease recurrence in the pelvis or extrahepatic abdomen.
Consider using positron emission tomography (PET) with fluorodeoxyglucose (FDG) to detect
recurrent disease.
Degree of Confidence
A recent study by Meta et al evaluated the impact of FDG-PET on the management of patients with
colorectal carcinoma.[15 ]They noted a change in the clinical stage and major management decisions
in approximately 40% of patients.
Of the changes in clinical stages in 25 patients, the disease was upstaged in 20 patients (80%) and
downstaged in 5 patients (20%). As a result of PET findings, physicians avoided major surgery in
41% of patients for whom surgery was the intended treatment.
False Positives/Negatives
False-positive results may occur with FDG from nonspecific inflammatory reactions following
radiotherapy or in patients with abscesses.
Intervention
Stent placement is a relatively simple procedure that rapidly improves the general condition of
patients with colonic obstruction.[ 16 ]
Consider placing metallic stents across obstructing carcinomas of the left colon as a temporary
measure to reduce the need for emergency surgery.
In patients unfit for surgery or with unresectable tumors, stents are used as a palliative procedure.
Intra-arterial chemotherapy may be performed in patients with unresectable tumors.

Similarly, intra-arterial chemotherapy via the hepatic artery may be used in the management of liver
metastases from colorectal tumors.
Lesional heating techniques such as radiofrequency (RF) ablation and interstitial laser
photocoagulation cause preferential tumor necrosis. RF electrodes or laser fibers are inserted into
the hepatic metastasis under CT scan or US control. Promising results (40% 5-year survival) have
been achieved from RF thermal ablation in selected patients with hepatic metastases from colorectal
cancer
Medicolegal Pitfalls
Failure to recognize the signs and symptoms of colon cancer
Failure to appropriately screen patients at various levels of risk
Failure to detect a carcinoma or polyp (>10 mm) by double-contrast barium enema or
colonoscopy
Failure to stage the carcinoma correctly using CT scan or MRI
Multimedia
Media file 1: Polypoid carcinoma. A large, irregular lobulated mass is present in
the rectosigmoid junction.

Media file 2: Annular carcinoma of the sigmoid colon. The lumen of the sigmoid is
narrowed severely by the circumferential mass with mucosal destruction and the
overhanging edges or shouldering at the tumor margins.
Media file 3: Flat carcinoma in the transverse colon. A broad-based contour defect
with central ulceration.

Media file 4: Double-contrast barium enema. 18-mm sessile polyp in the sigmoid
colon showing crescent sign.
Media file 5: Double-contrast barium enema. Stalked 15-mm polyp in sigmoid
colon.

Media file 6: Cecal carcinoma. A large polypoid cecal mass involves the ileocecal
valve and causes small bowel obstruction.
Media file 7: Colonic urticaria in ascending colon proximal to obstructing
carcinoma in the hepatic flexure.

Media file 8: Local perforation and paracolic collection in an annular carcinoma of
the descending colon.
Media file 9: Synchronous annular carcinomas in the ascending colon and splenic
flexure.

Media file 10: Annular carcinoma of the transverse colon is associated with a 2-cm
polyp in the sigmoid colon.
Media file 11: Preoperative CT. Cecal wall thickening and infiltration of the
pericolic fat.
Media file 12: Preoperative CT. Cecal carcinoma with circumferential involvement
of the cecal wall.

Media file 13: Preoperative CT. Irregular soft tissue mass involving the sigmoid
colon. There is associated diverticular disease.
Media file 14: Enhancing 6 x 4 cm mass from recurrent carcinoma. Note enlarged
left iliacus muscle from malignant involvement.
Media file 15: Barium enema. Typical annular carcinoma in the proximal sigmoid
colon with adjacent diverticular disease (same patient as in Image 13 in
Multimedia).

Media file 16: Retroperitoneal lymphadenopathy from cecal carcinoma.
Media file 17: Enlarged portal nodes (observed between inferior vena cava and
portal vein); hepatic metastases.

Media file 18: Contrast-enhanced CT showing liver metastases. Several low-density
metastases from the colonic primary tumor involve both lobes of the liver.
Media file 19: CT scan following a partial hepatectomy for a metastasis in the right
lobe.
Media file 20: Chest radiograph. Pulmonary metastases from colon cancer.

Media file 21: CT scan of cerebral metastasis from colon cancer. This is a rare site
for metastases from colonic cancer.
Media file 22: Enhancing mass in rectus sheath from metastasis from colon cancer
(same patient as in Image 14 in Multimedia).
Media file 23: Postradiotherapy inflammatory mass in the left iliac fossa. Note
stranding into the pericolic fat and presacral soft tissue swelling.
Media file 24: Dilated left ureter from inflammatory mass shown in Image 23 in
Multimedia.

Media file 25: Ultrasound scan through the right lobe of the liver showing large
hyperechoic metastasis from colon cancer.
Media file 26: Ultrasound scan of a large cecal carcinoma showing concentric
thickening of the hypoechoic bowel wall by the tumor.

Media file 27: Ultrasound scan demonstrating intussuscepting cecal carcinoma.
References
1. Bromer MQ, Weinberg DS. Screening for colorectal cancer--now and the near future. Semin
Oncol. Feb 2005;32(1):3-10.










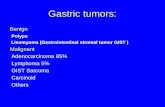




![[Ghiduri][Cancer]Gastric Cancer](https://static.fdocuments.net/doc/165x107/55cf9399550346f57b9de771/ghiduricancergastric-cancer.jpg)



