Gallbladder & bile duct Carcinoma Dr. m. h.khosravi.
-
Upload
agatha-clark -
Category
Documents
-
view
222 -
download
0
Transcript of Gallbladder & bile duct Carcinoma Dr. m. h.khosravi.
• Incidence
2 – 4 % of all GI tumor
F/M : 2-3 / 1
0/4 % in random autopsy
1% incidentally in cholecystectomy
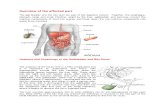
Carcinoma of the Gall bladder
Etiology
• 90% have gall stones
• Polypoid lesions, particulary larger than 10 mm
• Porcelain gallbladder
• Choledochal cysts
Pathology
• Adenocarcinomas is 80-90%
• histologic subtypes are papillary, nodular, and tubular.
• Cancer spreads through the lymphatics, venous drainage, and with direct invasion
Clinical Manifestations
• abdominal discomfort, right upper quadrant pain, nausea, and vomiting.
• less common: Jaundice, weight loss, anorexia, ascites, and abdominal mass
Treatment
• Surgery is the only curative option
• Tumors limited to the muscular layer (T1) need simple cholecystectomy
• tumor invades the perimuscular connective tissue without extension beyond the serosa or into the liver (T2 tumors)need extended cholecystectomyThat includes resection of liver segments IVB and V, and lymphadenectomy of the cystic duct, and pericholedochal,portal, right celiac, and posterior pancreatoduodenal lymph node
tumors that grow beyond the serosa or invade the liver or other organs (T3 and T4 tumors),need extended right hepatectomy (segments IV, V,VI, VII, and VIII)
Prognosis
• 5-year survival rate of all patients is less 5%
• median survival is 6 months.
• median survival in distant metastasis is only 1 to 3 months.
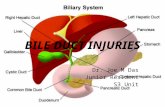
Bile Duct Carcinoma
• Incidence autopsy incidence is about 0.3%
overall incidence of is about 1.0 per
100,000 people per year
M/F : 1.3 /1
Etiology
Primary sclerosing cholangitis
choledochal cysts ulcerative colitis
hepatolithiasis biliary-enteric anastomosis infection with Clonorchis or in chronic typhoid carriers.
Pathology
• Adenocarcinomas is Over 95%
• Anatomically divided into distal, proximal, or perihilar tumors.
• Bismuth-Corlette classification
Clinical Manifestations
• Painless jaundice
• Pruritus,
• mild right upper quadrant pain,
• anorexia,
• fatigue,
• weight loss
Treatment
• Surgical excision is the only potentially curative treatment
• unresectable perihilar cholangiocarcinoma need Roux-en- Y cholangiojejunostomy to segment II or III bile ducts or to the right hepatic duct
• Perihilar tumors involving the bifurcation or proximal common hepatic duct (Bismuth-Corlette type I or II) need local tumor excision with portal lymphadenectomy cholecystectomy, common bile duct excision, and bilateral Roux-en- Y hepaticojejunostomies.
• tumor involves the right or left hepatic duct (Bismuth-Corlette type lIIa or lIIb)need right or left hepatic lobectomy,
• Distal resectable tumor need pancreatoduodenectomy (Whipple procedure).
• Distal unresectable tumor need Roux-en- Y hepaticojejunostomy,cholecystectomy, and gastrojejunostomy
• unresectable tumor on diagnostic evaluation need stent