FRIEDMAN,...MERRILL, FRIEDMAN, WILSON AND MARSHALL McCullough (7). These authors produced a de-layed...
Transcript of FRIEDMAN,...MERRILL, FRIEDMAN, WILSON AND MARSHALL McCullough (7). These authors produced a de-layed...

THE PRODUCTIONOF "DELAYED TYPE" CUTANEOUSHYPERSENSITIVITYTO HUMANDONORLEUKOCYTESAS A RESULTOF THE
REJECTION OF SKIN HOMOGRAFTS*
By JOHNP. MERRILL, ELI A. FRIEDMAN, RICHARD E. WILSONANDDAVID C. MARSHALL
(From the Departments of Medicine and Surgery, Peter Bent Brigham Hospital andHarvard Medical School, Boston, Mass.)
(Submitted for publication July 5, 1960; accepted December 1, 1960)
A large body of evidence relates the immuneresponse accompanying the rejection of a skinhomograft to the type of immunologic reactionwhich manifests itself in guinea pigs and humanbeings as hypersensitivity of the "delayed type"(1). A classic example of this reaction is the de-layed type of inflammation and swelling that re-sults from the intradermal injection of tubercu-lin into a sensitized recipient. Of interest in thehomograft reaction is the fact that this tuberculinreactivity can be transferred from one animal toanother by means of sensitized lymphoid cells ascan transplantation immunity (1). In furthersupport of the analogy between these two types ofimmunity, Brent, Brown and Medawar have re-cently shown in guinea pigs that the rejection ofa skin homograft is accompanied by a delayed typeof cutaneous hypersensitivity to donor leukocytesadministered either as a suspension of living cellsor as a cell-free extract (2). The reaction elicitedby the intradermal injection of donor antigen iscalled by them "the direct reaction." A similartype of reaction reaching its maximum somewhatmore slowly and declining more slowly than thedirect reaction is produced by the intradermal in-j ection of cells from the lymph nodes of the sen-sitized homograft recipient into its donor. Thisresponse they call "the transfer reaction." Thepresent experiment reports extension of theseobservations to humans following the productionof transplantation immunity.
* This work was supported in part by the United StatesArmy Medical Research and Development Command,Department of the Army, under Contract no. DA-49-007-MD-429; the National Heart Institute, National Insti-tutes of Health (no. H-444-C10); and the Massachu-setts Heart Association.
METHODS
Nineteen human volunteers received full thickness skingrafts from 19 donors. Grafts were placed on the upperextremity along with a control autograft. Eight recipi-ents received two grafts and the remainder, one graft.The donor and recipient pairs varied from totally non-related individuals to parent and child and closely re-lated dizygotic twins. The time of beginning of grossrejection of the skin grafts, judged by edema and by lossof capillary blanching, ranged from 6 to 26 days. Fol-lowing the rejection of one or both homografts, intra-dermal tests were performed in the recipients employingleukocytes harvested from the peripheral blood of thedonor. Twenty-five to 30 ml of venous blood was col-lected in a syringe containing 1 ml (10 mg) of heparin(Liquaemin, Organon) and 1.5 ml of a 20 per cent solu-tion of dextran with an average molecular weight of188,000.1 A cork was placed on the needle of the syringe,the syringe inverted and blood allowed to sediment at40 C. When adequate sedimentation had occurred, aplasma and white cell layer remaining at the top of thesedimented column of blood was expressed slowly throughthe needle and the plasma and white cell-rich plasmawere harvested separately. Donor white cells (averagedose, two million cells), donor plasma and donor redblood cells were inj ected intradermally as were similarquantities of autologous white cells, plasma and redcells. In seven experiments, sonic lysate of donor cellswas also injected. This lysate was prepared by themethod of Billingham, Brent and Medawar (3), whoshowed it to contain antigenic material active in ac-celerating the rejection of transplanted skin. In allcases white cells, plasma and red cells from nondonorhumans were also injected. As controls, 51 patientswith various forms of disease were injected with autolo-gous and homologous white cells prepared in a similarfashion (4). The reactions were observed at 1, 8, 24and 48 hours. The criterion for a positive result was anerythematous area with at least a 10 mmarea of indura-tion, graded separately by two observers. Character-istically, a positive reaction began at 8 to 12 hours, wasmaximal at 24, and began to fade at 36 hours. The
1 Grade H, A. K. Larus Company, Bethlehem, Pa.; lotno. H12757.
631

MERRILL, FRIEDMAN, WILSON AND MARSHALL
9;d -Mw
C~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~.....* " ~ qA,4o
B
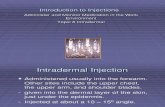
FIG. 1. HISTOLOGICAL SECTION OF SKIN BIOPSY FOR "POSITIVE" INTRADERMAL TEST AFTER
INJECTION OF DONORLEUKOCYTES. A. This field represents the deeper dermis; the cellularreaction seems more intense here than in the upper dermis, although the predominant cell is theneutrophilic polymorphonuclear cell. There are also moderate numbers of mononuclear cellsand occasional eosinophils. This is the distribution of cells seen in a delayed hypersensitivityreaction at 24 hours (hematoxylin and eosin; magnification X 400). B. Skin-epidermis andupper dermis of skin site shown at 24 hours after inoculation of autologous buffy coat. Littlenuclear debris is present and no intact leukocytes are noted. The defect in the lower field isincidental to the inoculation and contains fragmented collagen and occasional erythrocytes(hematoxylin and eosin; magnification X 400).
632

DELAYEDTYPE DERMALHYPERSENSITIVITY AFTER SKIN GRAFTING
TABLE I
Results in patients who rejected skin homografts
Number of grafts(one) (two)
Recipients 19 11 8
Positive reaction to intradermal Donor cells > nondonor cells 16leukocytes
Donor cells < nondonor cells 3Autologous cells 2
Donor lysate Positive 5Negative 2
volume of suspended cells was adjusted to 0.1 ml in a
tuberculin syringe. Injection of this amount of materialmay rise to an immediate bleb of 8 to 10 mm, whichgradually fades over a period of 6 to 8 hours and ischaracteristically accompanied by little induration. Onlythese reactions which increased from the twelfth to thetwenty-fourth hour were characterized as positive.
RESULTS
The 51 control patients injected with homolo-gous white cells [discussed in a previous paper
from this laboratory (4)] failed to react to them.The results of the patients who had rejected skinhomografts are summarized in Table I. In 16instances, the reaction to donor cells was greaterthan that to nondonor cells, although both were
positive by our criterion. In three instances, non-
donor cells gave rise to a greater reaction thanthat caused by specific donor cells. Two indi-viduals showed a positive reaction to their own
white cells, but in no instance was the reactiongreater than that to donor or nondonor homolo-gous cells. There were no positive reactions todonor red cells or to plasma alone. In five in-stances, injection of the water-soluble sonic ly-sates of donor cells induced a positive reactionwhich was uniformly less pronounced than that tofresh living cells. In all cases wherein reactionto donor lysate was positive, reactions to lysate ofnondonor homologous cells were also positive. Intwo instances, lysate of donor cells failed to cause
a positive reaction, whereas whole living cells in-duced a positive reaction. Histological sectionsof biopsies through a "positive" reaction and a
negative control are shown in Figure 1.2
DTSCUSSION
The significance of the positive intradermaltests depends largely upon the negative results in
2 Dr. Gustave J. Dammin has kindly prepared and de-scribed the histological material.
the control studies. In our control series, a groupof 51 patients with various diseases, including ac-tive rheumatic fever, showed negative reactions toboth autologous and homologous leukocytes simi-larly prepared in doses ranging from three tonine million cells per dose. Higher doses thanthis, even of autologous cells, may give positiveskin reactions in normal individuals. Lawrence(5) has reported a higher incidence of positiveskin reactions than that found in the present in-vestigation in control patients challenged withhomologous leukocytes intradermally. Hismethod of preparation, however, was differentfrom ours in that bovine fibrinogen was employedas the sedimenting agent, and the dosage of leu-kocytes in each intradermal site was not ascer-tained. Moreover, the total dosage of leukocytesfor each recipient was governed by the require-ments for the transfer of delayed sensitivity tobacterial antigens. Holman (6) found positivereactions to the intradermal injection of whitecells in one of six patients with rheumaticfever and in two of four patients with coronaryocclusion. Six normal individuals and ten otherpatients with various diseases had negative reac-tions. However, Holman found positive reactionsin two of five patients with rheumatoid arthritis.Two of seven patients with rheumatoid arthritiswhom we tested had positive reactions. Thislatter result is not surprising in view of the posi-tive reactions to the intradermal injection of au-tologous and homologous leukocytes in patientswith disseminated lupus erythematosus (4) andof the immunologic "overlap" between the twodiseases. Holman's technique differed from oursin using homogenates of autologous cells ratherthan whole cells, and this fact might explain inpart the difference from our results. It can onlybe re-emphasized, therefore, that under the par-ticular circumstances of our experiment, the 51control patients showed negative reactions to theintradermal injection of homologous leukocytes.
This work appears to confirm in humans the re-sults Brent and associates obtained in the guineapig (2). In our work, however, only the "directreaction" was tested. The number of positive re-actions with nondonor homologous cells suggeststhat the reaction is not entirely specific for donortissue. This finding is contrary to the results inthe single human reported by Martin. Waite and
633

MERRILL, FRIEDMAN, WILSON AND MARSHALL
McCullough (7). These authors produced a de-layed cutaneous reaction of hypersensitivity toviable donor leukocytes by their intradermal ad-ministration to a patient with hypogammaglobu-linemia, 250 and 266 days after transplantationof lymph nodes from the donor. In their case,injection of autologous leukocytes caused no reac-tion, and a similar result was obtained with anequal number of leukocytes derived from threenormal nondonors. The number of leukocytesemployed, however, was only one-third of thenumber used in our experiments. Brent and co-workers (2) mention in the discussion of theirwork with guinea pigs that the reaction "dependsupon the sensitization toward antigens present inanimals whose tissues provoke the state of sen-sitivity in the first instance." They go on to saythat the presence of these antigens in the donordoes not imply that they are absent from anyother guinea pig chosen at random from a hetero-geneous stock. Since our human patients werecertainly "heterogeneous stock," it is not surpris-ing that this reaction is not entirely "individualspecific." Actually, in the work reported byBrent and associates, the intradermal reaction wasuniformly positive for the donor strain but was nottested against leukocytes from other strains ofguinea pigs from which a cross reaction mighthave been obtained (2). The lack of individualspecificity for the homograft donor is of particularinterest as it relates to the rejection of homograftsby man. The actual rejection of cutaneous homo-grafts appears to be a highly individual, specificphenomenon in both purebred strains of mice andin man. The previous rejection of a skin graftin both species will result in an immunity whichcauses the accelerated rejection of a second graftfrom the same donor. However, preliminary re-sults from our laboratory suggest that previousimmunization of humans by the intradermal in-jection of donor leukocytes results not only in ac-celerated rejection of skin from the specific donorbut of skin from nondonors. This fact, plus theresults mentioned above, suggests that immuniza-tion with peripheral leukocytes is not as specificas immunization by transplantation of skin. Thisfact may be due perhaps to a difference in anti-genic structure between skin and leukocytes orpossibly to the degradation of their antigenicstructure by processing of the leukocytes. The
lack of consistency in our results might also beexplained by the fact that the antigens in ourstudies were peripheral leukocytes, a heterogene-ous cell population, probably of more varyingantigenicity when compared with the more homo-geneous cell population of the lymph nodes andspleen preparations of Brent and co-workers.Our preliminary results with extracted antigendiffer from Brent's in that the reactions wereconsiderably weaker and less specific. Brentstates that "extracted splenic antigen gives moreregular results in the direct reaction than livingdonor cells and is to be preferred on all countsexcept speed and convenience of preparation"(2). In Brent's experiments with guinea pigs,the cell-free antigen extracted from 50 mg ofsplenic tissue elicited a result comparable to thatof 12 million living cells. In our experiments,however, with a much larger subject (man) onlytwo million cells were used. In the work ofBillingham and associates, the antigenicity of thecell-free extract was only 1/100 as potent per mil-ligram of nitrogen as that of living cells (3).The antigenic material in our lysate preparationmust have been considerably less potent for therecipient than that used in Brent's experiments.In part, therefore, our divergent results with alimited number of injections of lysate may be ac-counted for by differences in dosage and by theeffect of the method of the preparation upon thepotency of the material. This idea is supportedby our observations that, where injection of ly-sate gave a positive reaction, the injection of liv-ing cells was invariably positive and that, in twoinstances in which the injection of lysate was fol-lowed by a negative reaction, the living cells gavea positive reaction.
The relation of the mechanism of the rejectionof the skin homograft and that of delayed hyper-sensitivity has been the subject of some specula-tion. It is possible that a weak state of immunityresults in the rejection of a first set homograftand in the production of a delayed type of intra-dermal sensitivity, whereas a hyperimmune stateassociated with circulating serum antibodies mayresult in the direct or "Arthus" phenomenon (1)and in the nonvascularized "white graft" in thecase of skin transplantation (8). It is possiblethat both these mechanisms may simply be vari-ants of the same immune response differing only
634

DELAYEDTYPE DERMALHYPERSENSITIVITY AFTER SKIN GRAFTING
in the quantitative aspect. If this is true and ifboth the classical homograft rejection and the de-layed type of cutaneous sensitivity depend uponcontact of antigen with a previously sensitizedlymphocyte, the delay in both instances may rep-resent time for liberation of antigen (in the caseof the injected intradermal leukocytes) plus theaccumulation of "sensitized" lymphocytes fromthe circulating lymphocyte population. One otherpoint might be included in comparing the presentresults to animal work insofar as an analogy be-tween homograft immunity and other types of"delayed sensitivity" is concerned. Intravenousinjection of antigen does not give rise to delayedhypersensitivity, whereas the intradermal or sub-cutaneous injection of antigen does. Similarly,the placing of a skin homograft, which is essen-tially a subcutaneous antigen, causes acceleratedrejection of a subsequent homograft from thesame donor; whereas prior intravenous injectionof epidermal cells causes, if anything, an increasein the survival time of subsequently transplantedskin (9). It is of interest in this regard thatamong our 51 controls were 10 patients who hadreceived multiple transfusions presumably con-taining white blood cells and that none of theserecipients of intravenous white cells had a sub-sequent positive cutaneous reaction to the in-tradermal injection of leukocytes.
Brent and associates have suggested that thedelayed type hypersensitivity reaction may becommon to the tuberculin test, to the homograftreaction, and to the autoimmune diseases. Sucha disease is disseminated lupus erythematosus inwhich circulating antibodies are found whichreact with the patient's own nuclear material.If such nuclear material were injected intrader-mally, therefore, one might expect a similar typeof delayed hypersensitivity. This finding hasproved to be the case (4).
SUMMARY
The immunity occasioned by the rejection of askin homograft in man is manifested by delayedintradermal sensitivity following injection of do-nor white blood cells. Unlike the immunity oc-casioned by the rejection of a previous skin homo-graft itself, under the conditions of our experi-ments, this reaction is not specific for donorleukocytes but may be elicited by the injection ofnondonor leukocytes into a sensitized recipient.
ACKNOWLEDGMENT
The authors gratefully acknowledge the invaluable as-sistance of Miss Audrey Jean Clemens in carrying outthis study.
REFERENCES
1. Lawrence, H. S. Homograft sensitivity. An expres-sion of the immunologic origins and consequencesof individuality. Physiol. Rev. 1959, 39, 811.
2. Brent, L., Brown, J., and Medawar, P. B. Skintransplantation immunity in relation to hyper-sensitivity. Lancet 1958, 2, 561.
3. Billingham, R. E., Brent, L., and Medawar, P. B.The antigenic stimulus in transplantation im-munity. Nature (Lond.) 1956, 178, 514.
4. Friedman, E. A., Bardawil, W. A., Merrill, J. P., andHanau, C. "Delayed" cutaneous hypersensitivityto leukocytes in disseminated lupus erythematosus.New Engl. J. Med. 1960, 262, 486.
5. Lawrence, H. S. Personal communication.6. Holman, H. Systemic lupus erythematosus. A re-
view of recent developments in the study of thisdisease. J. Pediat. 1960, 56, 109.
7. Martin, C. M., Waite, J. B., and McCullough, N. B.Antibody protein synthesis by lymph nodes homo-transplanted to a hypogammaglobulinemic adult.J. clin. Invest. 1957, 36, 405.
8. Stetson, C. A., Jr., and Demopoulos, R. Reactions ofskin homografts with specific immune sera. Ann.N. Y. Acad. Sci. 1958, 73, 687.
9. Billingham, R. E. Studies on epidermal cell sus-pension, with particular reference to problems oftransplantation immunity. Ann. N. Y. Acad. Sci.1957, 64, 799.
635