Silk fibroin/nanohydroxyapatite porous scaffolds for bone ...
formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
-
Upload
changen-pan -
Category
Documents
-
view
217 -
download
0
Transcript of formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
-
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
1/12
-
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
2/12
-
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
3/12
for healthy bone formation. However, how exposure to nano-
particles (NPs) by osteoblasts affects the deposition and
organization of such ECM proteins is poorly understood.
Previous studies of natural bone suggest that the mineral
component of bone is composed of apatite platelets with
a thickness of 27 nm, length of 15200 nm and width
of 1080 nm. These particles have also been described as
being needle-shaped [3]. CaP NPs, such as hydroxyapatite
(Ca10(PO4)6(OH)2, HA), can be artificially synthesized to be
as small as the nanosized-HA plates found in native bone
tissue (approx. 50 nm) [8]. These NPs potentially have an
important role in bone tissue engineering, forming nanosized
building blocks for bone tissue repair and/or replacement.
Thian et al. evaluated the bioactivity of electrohydrodynamic
atomized nanoapatite [9], as well as studying nanostructured
HA coatings produced using magnetron sputtering and elec-
trohydrodynamic spraying [1013]. Nanoapatite has also
been observed to form in various shapes, and with different
aspect ratios, when synthetic HA has been incubated in simu-
lated body fluid that contains similar ion levels to blood
plasma [14]. The aspect ratio of the particles may also influ-
ence the dissolution of a degradable ceramic such as HA.However, the stimulatory effect of differently shaped CaP
NPs on active osteoblasts, and the effect of uptake on intra-
cellular ion levels has not previously been studied. In
addition, a thorough, ultrastructural investigation into the
response of osteoblasts to HA NPs of different shapes, as
well as their influence on subsequent ECM formation, is
also lacking. The idea that different NP shapes may differen-
tially influence cell behaviour has been measured using
apoptosis and proliferation assays [15], as well as protein
expression analysis [16] and stains for NP uptake in a macro-
phage cell line [1619]. An experiment testing two differently
sized rod-shaped HA NPs on an osteoblast-like (osteosar-coma) cell line found that although the smaller particles
caused a significant amount of cells to apoptose, there was
no difference in alkaline phosphatase activity [20]. Another
study found that rod-shaped particles caused primary osteo-
blasts to decrease their proliferation after 3 days of culture
compared with spherical-shaped. A change of morphology
was also visible under scanning electron microscopy (SEM)
[21]. The effect of different-shaped NPs on the intracellular
ion content of primary osteoblasts, as measured using
TEM-based microanalysis, as well as ultrastructural and
ECM changes other than NP internalization [22] have not,
to the authors knowledge, been previously investigated
[18]. Whether NP treatment enhances MV formation and
release is currently unknown. With bone regeneration being
the ultimate goal of using HA NPs, our hypothesis was
that the osteoblast proliferation, function and ECM pro-
duction would respond to HA NPs, and that this response
would be sensitive to HA NPs having two different shapes
and aspect ratios. In addition to traditional biochemical
assays for measuring cell proliferation, we also used a
highly sensitive, TEM-based microanalysis technique that
measures cytoplasmic ion concentrations, including
potassium/sodium (K/Na) ratio [23,24]. To gain further
information of the effects of HA NP exposure on osteoblast
physiology and differentiation, microanalysis was also usedto measure intracellular calcium (Ca) and phosphorus (P)
levels, as a complement to other measures such as alkaline
phosphatase (ALP) activity. The effects of HA NPs on the
ultrastructural composition of osteoblasts (MVs and other
intracellular compartments), and early matrix and MV release
was studied.
2. Material and methods
2.1. Nanoparticle productionHA NPs were synthesized using the precipitation method. A
total of 200 ml 0.3 M phosphoric acid (Aldrich) was slowly
dripped into in 200 ml 0.5 M Ca hydroxide suspension under
shear stress (250 and 4500 r.p.m.). The pH was adjusted to
above 11 by adding ammonium hydroxide. The resultant
precipitate was then left at room temperature and aged for
7 days [25].
2.2. Nanoparticle characterization and analysis2.2.1. Fourier-transformed infrared spectroscopyFourier-transformed infrared spectroscopy was carried out on a
Perkin Elmer Spectrum One FTIR spectrometer, with a Perkin
Elmer Universal ATR sampling accessory. Perkin Elmer Imaging
Suite version 4.1 was used to collect the data, between the range
of 6000250 cm21, and the background signal was subtractedfrom sample data.
2.2.2. Inductively coupled plasma mass spectroscopyQuantification of media ion concentrations (Na, K, Ca and P),
using inductively coupled plasma mass spectroscopy (ICP-MS),
was carried out to obtain an approximate measure of the concen-
tration of ions released by HA NPs of different shapes, which
osteoblasts would be exposed to during in vitro tests. For this,
10 mg HA NPs (rice- and round-shaped, abbreviated as AR2 and
AR4) were incubated in 10 ml supplemented osteoblast media
(see below) at room temperature for 24, 48, 96 and 144 h
(7 days), in polypropylene tubes. Samples were kept rotating for
the entire incubation time (Denley Spiramix 10 roller system).
The supernatant media was removed to fresh tubes and diluted
1/20 with distilled water and analysed using ICP-MS. The ICP-
MS instrument used was a Perkin Elmer/Sciex Elan 6100DRC,
with a Perkin Elmer AS93 autosampler using Perkin Elmer
Elan v. 3.3 software. Argon was used as the plasma gas. The
elements and isotopes monitored were: 39K, 23Na, 44Ca and 31P.
For all elements except Ca, the most abundant isotope was moni-
tored, and standard curves made up with the same isotope. For
Ca, the most abundant isotope, 40Ca matches the mass of the
plasma gas, argon (40Ar). In order to distinguish between Ca
and Ar, the 44Ca isotope was monitored instead. A reaction cell
was used for Ca, with ammonia flowing at 0.7 ml min21. Each iso-
tope was monitored for 4 s, and five such replicates were averagedto produce the measured intensity reading quoted in the results.
Standards were prepared by spiking the cell culture medium with
the elements to be measured at concentrations of 0.1, 1, 10, 100,
1000 and 10 000 mg l21.
2.3. Osteoblast cell culturePrimary human osteoblasts (HOBs) were isolated from bone
discarded during elective orthopaedic surgery, and cells grown
using an explant outgrowth technique, as described previously
[26]. Cells were plated onto tissue culture plastic and passaged
when confluent. For proliferation, alkaline phosphatase (ALP)
activity and lactose dehydrogenase (LDH) assays, cells were seeded
onto tissue culture plastic according to standard culture protocolsin osteogenic media (1027 M water-soluble dexamethasone, 10 mM
b-glycerophosphate and 0.02 mM ascorbic acid (all Sigma)). Briefly,
40 000 HOBs were seeded per plate and flushed with 2 ml media
per well, either control media (no NPs) or with AR2 or AR4 NPs
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
2
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/ -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
4/12
(0.1 mg ml21). For electron and fluorescence microscopy, cells were
seeded on glass coverslips for 1 h in a 100 ml droplet, before flushing
with 2 mlmedia, which eithercontained HANPs or noHA NPs. For
cell assays, cells were grown for 3 and 7 days, after which they were
lysed with DNase/RNase-free water (Sigma, UK). For TEM, cells
were cultured on glass coverslips for 7 and 28 days, after which
cells were fixed and processed for transmission electron microscopy
(TEM) as described below.
2.4. Cell proliferation: DNA (Hoescht) assayTotal cellular DNA was measured using the Hoechst 33258 dye
(B2883, Sigma-Aldrich, Dorset, UK). Briefly, this was diluted
from 1 to 1.0 mg ml21 in saline sodium citrate (SSC) buffer added
to each standard or sample well in the Fluoronunc plate at a 1 : 1
ratio with sample volume. Samples were read in an Opsys
MR plate reader (Dynex Technologies, UK) at 460 nm, using
REVELATION QUICKLINK software (v. 4.24). Adenine thymidine
Hoechst 33258-specific fluorescence was read at 460 nm.
2.5. Alkaline phosphatase activityThe ALPactivity was used as a phenotypic marker of osteogenesis
[26]. For the assay, 10 ml of substrate reagent was mixed (40 mgp-nitrophenyl phosphate, 34 mg MgCl2.H2O, 80 ml Triton X-100
12.5% v/v (Sigma, UK) in 0.1 M glycine (pH 10.3) and a
p-nitrophenyl standard (Sigma, UK, 100 mg ml21). After 3 and
7 days of culture, samples were washed in phosphate-buffered
saline (PBS), and cells lysed by adding DNase/RNase-free water
followed by three freezethaw cycles, then transferred to Eppen-
dorf tubes and spun in an ultracentrifuge at 10 000 r.p.m. for
10 min. Samples were reacted with substrate reagent in 1 : 1 ratio
in black 96-well plates (Cliniplate, Thermo Fisher Scientific),
sealed (pre-cut transparent microplate sealers, Greiner Bio-One,
Stonhouse, Glous, UK) and shaken for 2 min (Titertek, Flow
Laboratories, UK) and measured at 410 nm (reference wavelength
630 nm) on a Hidex Plate Chameleon multilabel detection plat-
form (Hidex, UK) with Mikrowin 2000 software (MikrotekLaborsysteme GmbH). A standard curve using p-nitrophenyl
(the cleavage product ofp-nitrophenyl phosphate detected using
the assay) was used to determine ALP activity. To compare results
within groups, ALP activity readings were normalized for the
numberof cells, by measuring the amount of DNAin each sample.
2.6. Preparation of cells for transmission electron
microscopy and immuno-transmission electron
microscopyFor imaging, microanalysis and immune-TEM of HOB cultures,
cells on coverslips were fixed in 2.5% glutaraldehyde in phosphatebuffer, rinsed several times and then treated with 1% (w/v)
osmium tetroxide in phosphate buffer. The coverslips were
rinsed and dehydrated in a graded ethanol series. The coverslips
were then infiltrated with epoxy resin (TAAB, UK) and then sec-
tioned. Sections in the plane of the monolayers, as well as cross
sections through the sample (profile view of the cell culture
layers) were made. Ultrathin sections (7090 nm) were cut using
a Reichert-Jung Ultracut E ultramicrotome, mounted on mesh
copper grids and contrasted using uranyl acetate and lead citrate.
For TEM immunogold labelling, cells grown on coverslips
were fixed in 0.05% glutaraldehyde in phosphate buffer, washed
in 50 mM glycine in phosphate buffer, rinsed briefly in phosphate
buffer and water, and dehydrated through a graded series of etha-
nol. The coverslips were flooded with resin and left to infiltrateovernight at room temperature. Resin embedding was carried
and resin polymerized at 508C. Ultrathin resin sections were cut
(7090 nm) and mounted onto nickel grids. To block non-specific
reactions grids were floated on drops of 1% BSA in PBS. After the
blocking step, grids were incubated in primary antibody in 1%
BSA-PBS for 2 h, 1 : 100 for rabbit anti-human matrilin-3
(Abcam, UK), or 1 : 400 for rabbit anti-human FN (Dako, UK).
Grids were washed with 1% BSA-PBS, incubated on drops of
12 nm gold NP-conjugated secondary antibody (Jackson Immu-
noResearch Europe, UK) in 1% BSA-PBS for 1 h at a 1 : 40
dilution. Grids were then washed in 1% BSA-PBS and then PBS.
After rinsing in distilled water, the grids were allowed to air dry,
and finally stained for contrast with uranyl acetate and lead citrate
as previously described.
2.7. Transmission electron microscopy, immuno-
transmission electron microscopy and electron
dispersion of X-rays spectroscopyHA NPs were imaged using an FEI Tecnai T20 electron micro-
scope, and images captured using a Gatan ultrascan camera. For
TEM and immuno-TEM imaging, sections were examined on a
FEI Tecnai 12 transmission microscope operated at 120 kV and
images acquired with an AMT 16 000 M digital camera. For
elemental analysis (electron dispersion of X-rays spectroscopy
(EDS)), a Tecnai T12 microscope equipped with an EDAX X-raydetector and GENESIS software was used. HA NP aspect ratios
were calculated based upon measurements of length versus
width of a minimum of 25 samples pergroup. For both side (trans-
verse) and top views of HOB TEM sections, MVs were quantified
for each group (n 510). MVs released by cells at the top of cell
cultures or between cell layers were quantified and averaged for
each group (control, AR2 and AR4). MVs which had clustered at
the plasma membrane of cells were also quantified ( figure 8a).
Intracellular ion concentrations can be measured using TEM-
EDS microanalysis [23]. In this study, the use of the microanalysis
technique was applied as a novel measure of osteoblast response
to HA NPs, over a time course. Intracellular concentration of
sodium and potassium were estimated using TEM X-ray microana-
lysis. Cells were grown on gold TEM grids as described in Warleyet al.[27]. At each time point (24 h, 48 h and 7 days), the grids were
removed from the culture and washed briefly by dipping into ice
cold distilled water, then cryofixed by plunging into liquid nitro-
gen. The grids were then freeze-dried and coated with a thin
layer of carbon before analysis. Point analysis of Na, K, Ca and P
in the cell cytoplasm was carried out, avoiding internalized HA
NPs. Quantification was carried out using the Hall method.
Elements were quantified as mmol/kg by reference to previously
prepared internal calibration standards [23]. A minimum of
10 cells per group were analysed at each time point.
2.8. StatisticsA minimum of four samples were tested per group for all assays
unless otherwise stated, apart from microanalysis where a mini-
mum of 10 cells were analysed per group for each time point. For
statistical analyses, SPSS v. 17.0 was used. The MannWhitney U
non-parametric test was used to compare between two sam-
ples, and the KruskallWallis non-parametric test was used to
compare groups of more than two samples.
3. Results
3.1. Nanoparticle characterization and analysis3.1.1. Fourier-transformed infrared spectroscopyFTIR showed that both AR2 and AR4 NPs had similar spectra
(figure 1). The peaks at 1023 cm21 (AR4) or 1024 cm21 (AR2)
are most likely PO43
n3, confirming the presence of HA. The
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
3
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/ -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
5/12
bands at 874 cm21 (both groups), and at 1416 cm21 (AR4) or
1421 cm21 (AR2) suggest the presence of CO32 [28].
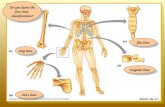
3.1.2. Transmission electron microscopy and electron dispersiveX-ray spectroscopyTEM of the HA NPs showed a size of approximately 50
20 nm for AR4, and a rice-grain morphology ( figure 2a,b),
and an approximately 20 nm diameter and spherical shape
for AR2 (figure 2c,d). Aspect ratios are listed intable 1. High-
angle annular dark-field-scanning TEM (HAADF STEM)
showed the presence of elements of high atomic number (for
example, higher than H, O or C) within the HA NPs. EDS
was then used to confirm the presence of Ca and P ( figure 3).
3.1.3. Inductively coupled plasma mass spectroscopyMeasurement of Ca, P, Na and K concentrations in cell culture
media, using ICP-MS, showed that following incubation with
0.9
0.8
0.7
0.6
0.5
0.4ab
sorbance
0.3
0.2
0.1
01700 1500 1300
wavenumber (cm1)
1100 900 700
Figure 1. FTIR showing similarity of AR4 and AR2 HA NPs. Grey line, AR4; black line, AR2.
100 nm 50 nm
20 nm 20 nm
(a) (b)
(c) (d)
Figure 2.TEM of (a,b) rice-shaped (AR4) HA NPs and (c,d) round-shaped (AR2) HA NPs. (a,c) Show NPs in clusters (100 and 20 nm scale bar, respectively); (b,d)
show singular HA NPs (20 and 50 nm scale bar, respectively). One side of AR4 was similar in length to the diameter of the AR2 (20 nm), the long side of the AR4
was larger (approx. 50 nm).
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
4
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/ -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
6/12
HA NPs, Ca, P, Na and K ion levels decreasedat all time points,
for both AR2 and AR4 (figure 4). The decrease in Ca and P
concentration was the highest in AR2 samples, whereas for
Na and K, although after 24 h in the AR2 group had a lower
concentration of both elements than AR4, there was less of a
notable difference in Na and K levels between the two
groups at the other time points. However for both NPs, the
levels of all elements measured were lower at every time
point than in the control (NP-free) media.
3.2. Proliferation assayCell proliferation, as measured by total DNA, was lower
than controls in the presence of both groups of HA NPs, at
3 and 7 days compared with controls ( figure 5), although
this was only statistically significant for AR2, when compa-
red to the control group ( p
0.043 and p
0.034 at 3 and7 days, respectively).
3.3. Alkaline phosphatase activityALP activity increased in the presence of NPs at 3 days, and
in the AR2 group at 7 days (figure 6). This was found to be
statistically significant ( p 0.034) for both AR2 and AR4 at
3 days, and for AR2 at 7 days ( p 0.034).
3.4. Transmission electron microscopy-based ultrastructural
observations and matrix vesicle release, microanalysis
of cytoplasmic ion concentrations and immuno-transmission electron microscopy
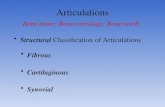
Transverse sections, looking at a side view of monolayer
cultures revealed a 5 10 cell thick cell layer. Osteoblasts
appeared to self-organize in culture. In all groups, cells at the
top of the 5 10 cell-layer structure (media-facing side, asopposed to tissue culture plastic-facing)contained higher num-
bers of vesicles and higher MV release was observed (figure 7),
suggesting that these cells may have a greater potential for
promoting bone/matrix mineralization. After 7 and 28 days,
cells displayed normal morphology. NP-stimulated cell cul-
tures appeared more active, containing a greater number of
Golgi bodies, mitochondria and MVs (figure 7b), compa-
red with controls (figure 7a). In some cells, NP-like clusters
were observed at the plasma membrane, especially at the
top layer of cultures (figure 8a). In addition, intra-
cellular osmium-stained vesicles were observed to a greater
extent in NP-stimulated samples following 7 days culture(figure 8b,c), especially at the top layer of cells. Counting of
the released MVs, at the top of the cell layers or between cell
layers, found an overall decrease in vesicles released post-HA
NP stimulation, although this was not statistically significant
(figure 8c,p 0.10). There were more MVs observed in AR2-
stimulated HOB cultures than in the AR4 group, although
there was no statistically significant difference observed
between the two groups ( p 0.12).
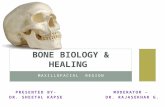
Random, disorganized fine threads, which did not show
typicalcollagen banding patterns (figure 7c), were observed fre-
quently within the extracellular space of control cultures, but
not in either type of HA NP cultures (figure 7d). There were
also fewer gaps visible between cells following NP stimu-lation. Immuno-TEM identified the thread-like fibrils as FN
(see arrows,figure 9a). FN-positive staining fibrils were not as
apparent in the HA NP-treated groups and did not show the
banding pattern associated with collagen (figure 9b). Following
rice-shaped HA NP exposure, matrilin-3 was found to form
larger polymeric units [7] as identified by clusters of the
immunogold secondary antibody ( figure 9d ). These large clus-
ters were not visualized in the control HOB samples (figure 9c).
Measuring cytoplasmic Ca and P concentrations showed
highly elevated levels in both AR2 and AR4 groups at 24 h.
This was statistically significant for AR4 ( p 0.05 for Ca and
P, table 2). The Ca and P concentration in AR4 seemed todecrease between 24 and 48 h, whereas it increased in AR2.
The reverse was observed at 7 days, with the AR4 group
having the highest Ca and P levels (although Ca levels were
still elevated in the AR2 group).
500 nm
1
30
25
20
counts
15P
Ca
CaCu
Cu
EDX HAADF detector area 1
10
5
02 4 6 8
energy (keV)
10 12
(a) (b)
Figure 3. (a) HAADF STEM image and (b) EDS of agglomerated AR4 NPs, confirming the presence of Ca and P in the sample.
Table 1. Length and width measurements of rice- and round-shaped HA
NPs, as well as corresponding aspect ratios (n 25).
HA NP
shape length (nm) width (nm)
aspect
ratio
rice (AR4) 107.8+ 27.0 28.4+ 9.1 3.79
round (AR2) 39.7+ 6.6 18.7+ 5.0 2.12
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
5
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/ -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
7/12
K/Na ratios measured with TEM microanalysis have been
used as a sensitive indicator of cell viability and proliferation
[29]. Following treatment with HA NPs for 24 and 48 h, both
types of HA NPs had lowered K/Na ratios compared with con-
trols, suggesting that they had lower viability. The change in
K/Na ratio was significantly lower for AR4 group ( p 0.05),
indicating lower cell viability. These data did not correlate
with the DNA assay results, which showed that the AR2
group had the lowest cell proliferation.
4. DiscussionPrevious work in the literature has described initial NP
uptake by cells and their effects on cell proliferation and
protein expression [16]. However, a thorough ultrastructural
investigation into the effects of HA NPs on osteoblasts,especially of different NP shapes, and MV release has not
previously been carried out, to the authors knowledge. Simi-
larly, the use of microanalysis to understand how exposure to
NPs alters the intracellular ion balance has not previously
been tested in osteoblasts, which we have shown here. Fur-
thermore, we have been able to demonstrate that exposure
to NPs may be influenced by NP shape, in terms of changes
to osteoblast proliferation, ALP activity and intracellular ion
levels. A previous study compared ALP activity following
NP exposure to two rod-shaped NPs of different sizes and
did not find any significant difference between them
[19,21]. Another study looking at an osteosarcoma-derived
cell line found that cell proliferation was decreased in the
presence of spherical-shaped HA NPs [21]. The group also
reported a change in cell morphology, as observed via
SEM, although this was not based on ultrastructural analysis
of ECM proteins or intracellular ion concentration. This study
provides additional in-depth information to these initial
reports that tested HA NPs of different shapes. Two ECM
proteins, which were affected by the exposure of cells to
NPs, FN and matrilin-3, were identified using immuno-
TEM. This work has shown that osteoblast cell layersappear to self-organize, such that the top layer of cells is
highly active and contains numerous MVs. MV release
by HOBs into the extracellular space was altered in the
NP-stimulated groups.
3000
2500
2000
1500
1000
24 48time (h) time (h)
control AR4 AR2
96 144
mgl1
mgl1
mgl1
mgl1
14000
13000
12000
11000
10000
9000
8000
140000
150000
160000
170000
130000
120000
3000
2500
2000
1500
1000
24 48 96 144
24 48
time (h) time (h)
96 144 24 48 96 144
(b)(a)
(c) (d)
Figure 4. Graphs comparing release of (a) Ca, (b) P, (c) K and (d) Na by HA NPs following 24, 48, 96 and 144 h (7 days) incubation in cell culture media, as
measured using ICP-MS. Note that the media ion concentrations decreasedafter incubation with HA NPs at all time points.
0
3 days
*
*
7 daystime (days)
control AR4 AR2
0.2
0.4
0.6
0.8
1.0
1.2
mgDNA
Figure 5.Graph representing results of DNA (Hoescht) assay at 3 and 7 days
post-incubation of HOBs with HA NPs (AR4 and AR2). Cells exposed to AR2
showed the lowest proliferation over the 7-day period. Statistical significance
is shown with an asterisk (*) where p 0.05.
0
3 days
**
*
7 daystime (days)
control AR4 AR2
1
2
3
4
5
6
ALP/DNA
Figure 6.Results of ALP assay, showing a change to ALP levels following 3
and 7 days treatment with AR4 and AR2. Statistical significance is shown
with an asterisk (*) where p 0.05.
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
6
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/ -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
8/12
1mm 1mm
500 nm 500 nm
(a) (b)
(c) (d)
Figure 7.Images from TEM, showing in (a) and (b) a transverse view of HOB cell layers following 7 days culture, ( a) controls (no NPs) and (b) with AR2, which
showed higher levels of MVs towards the top of the culture, compared with controls (see arrow); ( c) thin threads in the extracellular space of control osteoblast
cultures (see arrow); (d) a lack of such ECM structures in the round HA NP-stimulated group. The scale bars in ( a) and (b) are 1mm; in (c) and (d) they are 500 nm.
(a) (b)
120
100
80
60
40
no.vesiclesreleasedpercell
20
0control AR4
group
AR2
(c)
Figure 8.TEM images of MVs release by round-shaped HA NP-stimulated osteoblasts, including (a) a growing cluster of MVs at the cell surface and (b) chains of
MVs being released into the extracellular space (scale bar, 100 nm for all images). ( c) Number of MVs released by primary HOBs under control conditions and after
stimulation with rice- or round-shaped HA NPs. There was no significant difference between groups, although AR2 had higher MV release than AR4.
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
7
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/ -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
9/12
Despite extensive research into ceramic NPs and their
in vitro biocompatibility, as well as the effect of HA NPs
on other cell types [18,30], this is the first work to speci-
fically document the changes in osteoblast ultrastructure
and ECM following HA NP exposure. Furthermore, it
attempts to quantify cytoplasmic Ca and P, based on a micro-
analysis technique which has not been used with cultured
osteoblasts. In terms of cultured cells, microanalysis hasbeen limited to use in other cell types, such as red blood
cells and monocytes [15,24]. In the first description of MVs,
Anderson [4] used TEM, EDS and XRD techniques to detect
Ca and phosphate within sections of cartilage and bone. Mot-
skinet al.[15,30] used microanalysis to measure the Ca and P
content of HA NPs engulfed within monocyte-macrophages
in vitroand to study NP dissolution, as opposed to the specific
measurement of cytoplasmic Ca and P concentrations. Relating
the increase in ALPactivity to the different intracellular Ca and
P levels, we suggest that a moderate increase in Ca and P levels
for 24 h, as experienced following AR2 HA NP exposure, may
be stimulatory for increasing osteoblast function, for example,
via increased MV CaP accumulation and release. Xuet al.[16]showed an increase in expression of Ca-regulating proteins
after stimulation with needle-shaped or round-shaped HA
NPs. By contrast, higher Ca and P ion levels may not be as
effective, or indeed detrimental, as observed with AR4 HA
NPs. The decrease in cell proliferation in the AR2 group, as
detected using DNA quantification, may be a result of
increased cell differentiation, as suggested in an osteoblast
study by Robinson et al. [31]. A similar result was observed
by Xuet al. [16] except between sharper, needle-shaped HA
NPs and round-shaped HA NPs.
Intracellular Ca levels have an important role in osteoblast
homeostasis, regulation and apoptosis [3234]. Interestingly,a time-dependent change in Ca2 levels was observed over
7 days, when cells were exposed to HA NPs. Whether this
change was due to HA NPs entering into the cell cytoplasm
followed by NP dissolution is yet to be determined. Motskin
et al. [15] showed that microparticles and NPs made via
different materials synthesis techniques had different effects
on human monocyte-derived macrophages, with some show-
ing significantly greater uptake and/or toxicity. TEM images
demonstrated that HA NPs were dissolved by cells over time,
whereas microparticles broke into NPs before they were dis-
solved by cells [15]. Using two complimentary methods of
assessing cell viability and/or proliferation (DNA quantifi-cation and Na/K microanalysis), we have shown that cell
viability was affected by treatment with HA NP over 24 h,
48 h and 7 days, and that HA NPs with two different
shapes resulted in different microanalysis results. The effects
of four differently shaped NPs (needle, spherical, long rod-
like and short rod-like) on the proliferation, ALP activity,
intracellular reactive oxygen species and apoptosis, has also
been carried out by Xuet al. [18].
Although extracellular phosphate is essential to the regu-
lation of mineralization [35], in this experiment we have
actually observed adecrease in phosphate-media levels follow-
ing incubation with HA NPs, rather than increase. Differences
in,or changes to surface chemistry, with or without ionadsorp-tion/de novo apatite formation, may have contributed to
changes in NP toxicity [15], uptake, intracellular distribution
and dissolution. Differences in protein and/or ion adsorption
and apatite formation on NP surfaces, which have been
linked to NP morphology [36,37], may have also contributed
to the microanalysis results.
Another observation in this study was the apparent self-
organization of osteoblasts following cell culture for 7 days,
as demonstrated by transverse TEM sections showing that
HOBs formed a four- to five-cell thick layer on tissue culture
plastic. MVs, which were visualized using TEM, were much
more prevalent in the top osteoblast layer than at thebottom of the cell-layer structure. Budding and release of
MVs into the extracellular space were also located at the
top layer of the culture. These TEM images show some evi-
dence that osteoblasts are able to self-organize in vitro, such
(a) (b)
(c) (d)
Figure 9.Immuno-TEM of HOBs for (a) FN (control group), (b) FN (AR4), (c) matrilin-3 (control group) and (d) matrilin-3 (AR4). Gold labelling showed that FN was
shown to co-localize with the fine fibrils that were decreased in the presence of HA NPs (fibrils with no apparent collagen double-banding pattern). Matrilin-3,
which is important for normal endochondral ossification during skeletal development, was found to have different staining patterns following HOB treatment with
HA NPs, showing increased oligomerization and/or polymerization. Arrows indicate positive immunogold labelling.
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
8
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/ -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
10/12
that the most active cells are located at the top layer of the
culture. In this five-cell thick in vitro culture, we have
shown that by self-organizing, the HOBs have exposed their
MV-releasing region of the outer membrane to the extracellular
environment, especially at the top of the culture where
MV release is most apparent. By observing cryo-electron
microscopy of developing mouse calvaria and long bones,
and using elemental analysis (EDS), Mahamid et al.[5] hypo-
thesized that phosphate first concentrates within MVs,
followed by the sequestration of Ca, forming an amorphous
CaP. We have also shown the deposition of osteoid/MVs
by these cells from the top of the cultures and within the
extracellular space, similar to that imaged by Ecarot-Charrier
et al. [38], and that their release into the extracellular space
appeared to be altered by HA NPs of either morphology. The
statistically significant increase in ALP activity in the round-
shaped HA NP (AR2) group suggests that osteoblasts in this
group may be more active compared to those stimulated
with AR4 [39].
In terms of changes observed in the ECM, which plays a
crucial role in bone formation, we have shown that thin fibrils
observed via TEM stain positively with anti-FN antibody, andappear to be altered in the presence of HA NPs. FN is required
for collagen assembly and maintenance, as well as bone devel-
opment and repair [4042]. HA has been shown to avidly bind
proteins and other ions and molecules, including FN [4345].
It may be that the FN-binding ability of HA may have inter-
fered with thein vitroformation of normal FN networks. It is
also not known whether the changes to the ECM are linked
to matrilin-3 oligomerization. Matrilins-1 and 3 have been
shown to be expressed temporally within the growth plate
and also have been observed to formextended filamentous net-
works [7]. Matrilin-3 expression has not previously been
observed in cultured osteoblasts [7] and is reported here forthe first time. The role of biomaterials in regulating such
ECM proteins is an area of current investigation.
5. ConclusionIn conclusion, HA NPs of two different shapes, rice-shaped
(AR4) and round-shaped (AR2), were shown to influence
HOB proliferation, cytoplasmic ion levels, ultrastructure
and ECM assembly. AR2 and AR4 were shown to adsorb
Ca, P, Na and K at different levels, from cell culture media.
A sensitive TEM-based microanalysis technique was used to
detect subtle changes in cell viability and cytoplasmic ion
levels, by measuring the K/Na ratio and Ca and P concen-
trations. ECM proteins FN and matrilin-3 were shown to
change in organization following culture with HA NPs, and
expression of matrilin-3 in primary HOBs was confirmed
using immuno-TEM. AR2 had a greater osteogenic effect
when compared with AR4, as measured, suggesting that HA
NPs of this shape and/or aspect ratio may have a positive
effect upon new bone formation. AR2 caused a moderate
increase in intracellular Ca and P levels, while AR4 caused a
larger increase in ion levels. Interestingly, when primary
HOBs were cultured in vitro, they were observed to self-
organize into a layered structure four to five cells thick, withthe most active cells located at the top of the culture. The rel-
evance and consequences of changes to cell viability,
cytoplasmic ion levels, cell self-organization to new bone for-
mation in vivo requires further investigation. In addition,Table
2.
CytoplasmicHOBCa,
P,
NaandKconcentrationsfollo
wing3and7daysculture,withandwithout
HA
NPs(AR4andAR2).DifferencesinionlevelswerefoundfollowingHA
NPtreatment,whichcorrespondedtoassaysforcell
proliferation(DN
A)andosteoblastfunction(ALP).
K/Na
Ca
P
control
AR4
AR2
control
A
R4
AR2
control
AR4
AR2
24h
16.4
7+
4.5
0
2.8
1+
1.4
1
6.7
6+
4.5
0
22.5
4+
11.1
8
287.2
2+
119.4
1
156.2
5+
179.1
2
846.0
5+
68.6
1
1350.6
1+
147.3
0
908.3
0+
129.8
8
48h
5.9
4+
0.0
7
1.2
0+
1.1
4
3.8
1+
3.2
4
62.3
0+
88.2
0
50.9
5+
26.4
8
137.5
1+
125.2
1
962.0
7+
141.7
2
928.3
3+
183.8
5
1051.9
3+
365.7
1
7days
5.3
3+
3.0
2
6.6
0+
4.9
3
4.8
2+
1.0
5
19.6
0+
17.9
4
135.1
9+
151.0
4
53.7
2+
61.5
5
966.1
6+
416.5
3
912.2
4+
253.5
5
803.3
6+
161.0
3
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
9
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/ -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
11/12
further analysis of NP effects on osteoblast ultrastructure and
ECM production is an important and critical biological
consideration for future work.
Acknowledgements. The authors would like to thank OrthopaedicResearch UK (ORUK) for their generous support and Dr GiuseppeCama for assistance with FTIR analysis of HA NPs.
References
1. Lanyon LE. 1984 Functional strain as a determinant
for bone remodeling.Calcif. Tissue Int. 36(Suppl. 1),S56S61. (doi:10.1007/BF02406134)
2. Goodship AE, Lanyon LE, McFie H. 1979 Functional
adaptation of bone to increased stress. An
experimental study. J. Bone Joint Surg. Am.
61, 539546.
3. Fratzl P, Gupta HS, Paschalis EP, Roschger P. 2004
Structure and mechanical quality of the collagen
mineral nano-composite in bone. J. Mater. Chem.
14, 21152123. (doi:10.1039/b402005g)
4. Anderson HC. 1969 Vesicles associated with
calcification in the matrix of epiphyseal cartilage.
J. Cell Biol. 41, 5972. (doi:10.1083/jcb.41.1.59)5. Mahamid J, Sharir A, Gur D, Zelzer E, Addadi L,
Weiner S. 2011 Bone mineralization proceeds
through intracellular calcium phosphate loaded
vesicles: a cryo-electron microscopy study.
J. Struct. Biol. 174, 527535. (doi:10.1016/j.jsb.
2011.03.014)
6. Boonrungsiman SGE, Carzaniga R, Evans ND,
McComb DW, Porter AE, Stevens MM. 2012 The role
of intracellular calcium phosphate in osteoblast-
mediated bone apatite formation. Proc. Natl Acad.
Sci. USA 109, 13 170 13 175. (doi:10.1073/pnas.
1208916109)
7. Klatt AR, Nitsche DP, Kobbe B, Morgelin M,
Paulsson M, Wagener R. 2000 Molecular structure
and tissue distribution of matrilin-3, a filament-
forming extracellular matrix protein expressed
during skeletal development. J. Biol. Chem. 275,
3999 4006. (doi:10.1074/jbc.275.6.3999)
8. Huang J, Best SM, Brooks RA, Rushton N,
Bonfield W. 2008 In vitro evaluation of nanosized
carbonate-substituted hydroxyapatite and its
polyhydroxyethylmethacrylate nanocomposite.
J. Biomed. Mater. Res. A 87 , 598607. (doi:10.
1002/jbm.a.31815)
9. Thian ESA et al. 2007 Bioactivity of nanoapatiteproduced by electrohydrodynamic atomization.
J. Bionanosci.1 , 6063. (doi:10.1166/jbns.
2007.004)
10. Thian ES, Huang J, Best SM, Barber ZH, Bonfield W.
2006 Nanostructured apatite coatings for rapid bone
repair. Bioceramics 309311, 519522.
11. Thian ESet al. 2008 Influence of
nanohydroxyapatite patterns deposited by
electrohydrodynamic spraying on osteoblast
response. J. Biomed. Mater. Res. A 85, 188194.
(doi:10.1002/jbm.a.31564)
12. Munir G, Koller G, Di Silvio L, Edirisinghe MJ,
Bonfield W, Huang J. 2011 The pathway to
intelligent implants: osteoblast response to nano
silicon-doped hydroxyapatite patterning. J. R. Soc.
Interface8 , 678688. (doi:10.1098/rsif.2010.0548)
13. Li X, Koller G, Huang J, Di Silvio L, Renton T, Esat M,
Bonfield W, Edirisinghe M. 2010 A novel jet-basednano-hydroxyapatite patterning technique for
osteoblast guidance. J. R. Soc. Interface 7 ,
189197. (doi:10.1098/rsif.2009.0101)
14. Vandiver J, Patel N, Bonfield W, Ortiz C. 2005
Nanoscale morphology of apatite precipitated onto
synthetic hydroxyapatite from simulated body fluid.
Bioceramics284286, 497500.
15. Motskin M, Wright DM, Muller K, Kyle N, Gard TG,
Porter AE, Skepper JN. 2009 Hydroxyapatite nano
and microparticles: correlation of particle properties
with cytotoxicity and biostability. Biomaterials 30,
3307 3317. (doi:10.1016/j.biomaterials.2009.02.044)
16. Xu JL, Khor KA, Sui JJ, Zhang JH, Chen WN. 2009
Protein expression profiles in osteoblasts in response
to differentially shaped hydroxyapatite
nanoparticles.Biomaterials30, 53855391. (doi:10.
1016/j.biomaterials.2009.07.002)
17. Zhao X, Heng BC, Xiong S, Guo J, Tan TT, Boey FY,
Ng KW, Loo JS. 2011 In vitro assessment of
cellular responses to rod-shaped hydroxyapatite
nanoparticles of varying lengths and surface
areas. Nanotoxicology5 , 182194. (doi:10.3109/
17435390.2010.503943)
18. Xu Z, Liu C, Wei J, Sun J. 2012 Effects of four types
of hydroxyapatite nanoparticles with different
nanocrystal morphologies and sizes on apoptosis in
rat osteoblasts. J. Appl. Toxicol. 32, 429435.
(doi:10.1002/jat.1745)
19. Zhao X, Ng S, Heng BC, Guo J, Ma L, Tan TTY, Ng
KW, Loo SCJ. 2013 Cytotoxicity of hydroxyapatite
nanoparticles is shape and cell dependent. Arch.
Toxicol.87, 10371052. (doi:10.1007/s00204-
012-0827-1)
20. Liu X, Zhao M, Lu J, Ma J, Wei J, Wei S. 2012 Cell
responses to two kinds of nanohydroxyapatite with
different sizes and crystallinities. Int. J. Nanomed. 7,1239 1250. (doi:10.2147/IJN.S28098)
21. Zhao Y, Zhang Y, Ning F, Guo D, Xu Z. 2007
Synthesis and cellular biocompatibility of two kinds
of HAP with different nanocrystal morphology.
J. Biomed. Mater. Res. B. Appl. Biomater.83,
121126. (doi:10.1002/jbm.b.30774)
22. Gratton SE, Ropp PA, Pohlhaus PD, Luft JC, Madden
VJ, Napier ME, DeSimone JM. 2008 The effect of
particle design on cellular internalization pathways.
Proc. Natl Acad. Sci. USA 105, 11 61311 618.
(doi:10.1073/pnas.0801763105)
23. Warley A, Cracknell KP, Cammish HB,
Twort CH, Ward JP, Hirst SJ. 1994 Preparation
of cultured airway smooth muscle for study
of intracellular element concentrations by
X-ray microanalysis: comparison of whole
cells with cryosections. J. Microsc. 175,
143153. (doi:10.1111/j.1365-2818.1994.tb03477.x)
24. Mauritz JMAet al. 2010 Biophotonic techniques for
the study of malaria-infected red blood cells.Med.
Biol. Eng. Comput. 48, 10551063. (doi:10.1007/
s11517-010-0668-0)
25. Akao M, Aoki H, Kato K. 1981 Mechanical properties
of sintered hydroxyapatite for prosthetic
applications.J. Mater. Sci. 16, 809812. (doi:10.
1007/BF02402799)
26. Di Silvio L, Gurav N. 2002 Osteoblasts. InHuman
cell culture (eds FP Koller, BO Masters), p. 242.
The Netherlands: Springer.27. Warley A. 1994 The preparation of cultured cells for
X-ray microanalysis. Scanning Microsc. Suppl. 8 ,
129137 (discussion 378).
28. Thamaraiselvi TV, Prabakaran K, Rajeswari S. 2006
Synthesis of hydroxyapatite that mimic bone
minerology. Trends Biomater. Artif. Organs 19,
8183.
29. Alaminos M, Sanchez-Quevedo MC, Munoz-Avila JI,
Garcia JM, Crespo PV, Gonzalez-Andrades M,
Campos A. 2007 Evaluation of the viability of
cultured corneal endothelial cells by quantitative
electron probe X-ray microanalysis. J. Cell Physiol.
211, 692698. (doi:10.1002/jcp.20976)
30. Motskin M, Muller KH, Genoud C, Monteith AG,
Skepper JN. 2011 The sequestration of
hydroxyapatite nanoparticles by human monocyte-
macrophages in a compartment that allows free
diffusion with the extracellular environment.
Biomaterials32 , 94709482. (doi:10.1016/j.
biomaterials.2011.08.060)
31. Robinson JA, Harris SA, Riggs BL, Spelsberg TC.
1997 Estrogen regulation of human osteoblastic cell
proliferation and differentiation. Endocrinology138,
29192927.
32. Barry ELR. 2000 Expression of mRNAs for thealpha(1) subunit of voltage-gated calcium channels
in human osteoblast-like cell lines and in normal
human osteoblasts.Calcif. Tissue Int. 66, 145150.
(doi:10.1007/s002230010029)
33. Zayzafoon M. 2006 Calcium/calmodulin signaling
controls osteoblast growth and differentiation.
J. Cell. Biochem. 97, 5670. (doi:10.1002/
jcb.20675)
34. Francis MJO, Lees RL, Trujillo E, Martin-Vasallo P,
Heersche JNM, Mobasheri A. 2002 ATPase pumps
in osteoclasts and osteoblasts. Int. J. Biochem.
Cell Biol. 34 , 459476. (doi:10.1016/S1357-
2725(01)00142-X)
35. Sapir-Koren R, Livshits G. 2011 Bone mineralization
and regulation of phosphate homeostasis. IBMS
BoneKEy8 , 286300. (doi:10.1138/20110516)
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
10
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://dx.doi.org/10.1007/BF02406134http://dx.doi.org/10.1039/b402005ghttp://dx.doi.org/10.1083/jcb.41.1.59http://dx.doi.org/10.1016/j.jsb.2011.03.014http://dx.doi.org/10.1016/j.jsb.2011.03.014http://dx.doi.org/10.1073/pnas.1208916109http://dx.doi.org/10.1073/pnas.1208916109http://dx.doi.org/10.1074/jbc.275.6.3999http://dx.doi.org/10.1002/jbm.a.31815http://dx.doi.org/10.1002/jbm.a.31815http://dx.doi.org/10.1166/jbns.2007.004http://dx.doi.org/10.1166/jbns.2007.004http://dx.doi.org/10.1002/jbm.a.31564http://dx.doi.org/10.1098/rsif.2010.0548http://dx.doi.org/10.1098/rsif.2009.0101http://dx.doi.org/10.1016/j.biomaterials.2009.02.044http://dx.doi.org/10.1016/j.biomaterials.2009.02.044http://dx.doi.org/10.1016/j.biomaterials.2009.07.002http://dx.doi.org/10.1016/j.biomaterials.2009.07.002http://dx.doi.org/10.3109/17435390.2010.503943http://dx.doi.org/10.3109/17435390.2010.503943http://dx.doi.org/10.1002/jat.1745http://dx.doi.org/10.1007/s00204-012-0827-1http://dx.doi.org/10.1007/s00204-012-0827-1http://dx.doi.org/10.2147/IJN.S28098http://dx.doi.org/10.1002/jbm.b.30774http://dx.doi.org/10.1073/pnas.0801763105http://dx.doi.org/10.1111/j.1365-2818.1994.tb03477.xhttp://dx.doi.org/10.1111/j.1365-2818.1994.tb03477.xhttp://dx.doi.org/10.1007/s11517-010-0668-0http://dx.doi.org/10.1007/s11517-010-0668-0http://dx.doi.org/10.1007/BF02402799http://dx.doi.org/10.1007/BF02402799http://dx.doi.org/10.1002/jcp.20976http://dx.doi.org/10.1016/j.biomaterials.2011.08.060http://dx.doi.org/10.1016/j.biomaterials.2011.08.060http://dx.doi.org/10.1007/s002230010029http://dx.doi.org/10.1002/jcb.20675http://dx.doi.org/10.1002/jcb.20675http://dx.doi.org/10.1016/S1357-2725(01)00142-Xhttp://dx.doi.org/10.1016/S1357-2725(01)00142-Xhttp://dx.doi.org/10.1138/20110516http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://dx.doi.org/10.1138/20110516http://dx.doi.org/10.1016/S1357-2725(01)00142-Xhttp://dx.doi.org/10.1016/S1357-2725(01)00142-Xhttp://dx.doi.org/10.1002/jcb.20675http://dx.doi.org/10.1002/jcb.20675http://dx.doi.org/10.1007/s002230010029http://dx.doi.org/10.1016/j.biomaterials.2011.08.060http://dx.doi.org/10.1016/j.biomaterials.2011.08.060http://dx.doi.org/10.1002/jcp.20976http://dx.doi.org/10.1007/BF02402799http://dx.doi.org/10.1007/BF02402799http://dx.doi.org/10.1007/s11517-010-0668-0http://dx.doi.org/10.1007/s11517-010-0668-0http://dx.doi.org/10.1111/j.1365-2818.1994.tb03477.xhttp://dx.doi.org/10.1111/j.1365-2818.1994.tb03477.xhttp://dx.doi.org/10.1073/pnas.0801763105http://dx.doi.org/10.1002/jbm.b.30774http://dx.doi.org/10.2147/IJN.S28098http://dx.doi.org/10.1007/s00204-012-0827-1http://dx.doi.org/10.1007/s00204-012-0827-1http://dx.doi.org/10.1002/jat.1745http://dx.doi.org/10.3109/17435390.2010.503943http://dx.doi.org/10.3109/17435390.2010.503943http://dx.doi.org/10.1016/j.biomaterials.2009.07.002http://dx.doi.org/10.1016/j.biomaterials.2009.07.002http://dx.doi.org/10.1016/j.biomaterials.2009.02.044http://dx.doi.org/10.1016/j.biomaterials.2009.02.044http://dx.doi.org/10.1098/rsif.2009.0101http://dx.doi.org/10.1098/rsif.2010.0548http://dx.doi.org/10.1002/jbm.a.31564http://dx.doi.org/10.1166/jbns.2007.004http://dx.doi.org/10.1166/jbns.2007.004http://dx.doi.org/10.1002/jbm.a.31815http://dx.doi.org/10.1002/jbm.a.31815http://dx.doi.org/10.1074/jbc.275.6.3999http://dx.doi.org/10.1073/pnas.1208916109http://dx.doi.org/10.1073/pnas.1208916109http://dx.doi.org/10.1016/j.jsb.2011.03.014http://dx.doi.org/10.1016/j.jsb.2011.03.014http://dx.doi.org/10.1083/jcb.41.1.59http://dx.doi.org/10.1039/b402005ghttp://dx.doi.org/10.1007/BF02406134 -
8/12/2019 formation: an analytical study Nanohydroxyapatite shape and its potential role in bone
12/12
36. Ribeiro N, Sousa SR, Monteiro FJ. 2010 Influence of
crystallite size of nanophased hydroxyapatite on
fibronectin and osteonectin adsorption and on
MC3T3-E1 osteoblast adhesion and morphology.
J. Colloid Interface Sci.351, 398 406. (doi:10.1016/
j.jcis.2010.08.013)
37. Guth K, Campion C, Buckland T, Hing KA. 2010
Surface physiochemistry affects protein adsorption
to stoichiometric and silicate-substitute microporous
hydroxyapatites. Adv. Eng. Mater. 12, B113 B121.
(doi:10.1002/adem.200980026)
38. Ecarot-Charrier B, Shepard N, Charette G, Grynpas
M, Glorieux FH. 1988 Mineralization in osteoblast
cultures: a light and electron microscopic study.
Bone9 , 147154. (doi:10.1016/8756-3282(88)
90004-X)
39. Anderson HC. 2003 Matrix vesicles and calcification.
Curr. Rheum. Rep. 5 , 222226. (doi:10.1007/
s11926-003-0071-z)
40. Stein GS, Lian JB. 1993 Molecular mechanisms
mediating proliferation differentiation
interrelationships during progressive development
of the osteoblast phenotype. Endocr. Rev. 14,
424442.
41. Sottile J, Hocking DC. 2002 Fibronectin
polymerization regulates the composition and
stability of extracellular matrix fibrils and cell
matrix adhesions. Mol. Biol. Cell13 , 35463559.
(doi:10.1091/mbc.E02-01-0048)
42. Huang GR, Zhang Y, Kim B, Ge GX, Annis DS,
Mosher DF, Greenspan DS. 2009 Fibronectin binds
and enhances the activity of bone morphogenetic
protein 1. J. Biol. Chem. 284, 25 87925 888.
(doi:10.1074/jbc.M109.024125)
43. Service RF. 2003 American chemical society meeting:
nanomaterials show signs of toxicity. Science300,
243. (doi:10.1126/science.300.5617.243a )
44. Sayes CM, Reed KL, Warheit DB. 2007 Assessing
toxicity of fine and nanoparticles: comparing in vitro
measurements toin vivopulmonary toxicity profiles.
Toxicol. Sci. 97 , 163180. (doi:10.1093/toxsci/
kfm018)
45. Guth K, Campion C, Buckland T, Hing KA. 2011
Effects of serum protein on ionic exchange between
culture medium and microporous hydroxyapatite
and silicate-substituted hydroxyapatite.J. Mater. Sci.
Mater. Med.22, 2155 2164. (doi:10.1007/s10856-
011-4409-1)
rsif.royalsocietypublishin
g.org
J.R.Soc.Interface
1
1
:
20140004
11
on April 2, 2014rsif.royalsocietypublishing.orgDownloaded from
http://dx.doi.org/10.1016/j.jcis.2010.08.013http://dx.doi.org/10.1016/j.jcis.2010.08.013http://dx.doi.org/10.1002/adem.200980026http://dx.doi.org/10.1016/8756-3282(88)90004-Xhttp://dx.doi.org/10.1016/8756-3282(88)90004-Xhttp://dx.doi.org/10.1007/s11926-003-0071-zhttp://dx.doi.org/10.1007/s11926-003-0071-zhttp://dx.doi.org/10.1091/mbc.E02-01-0048http://dx.doi.org/10.1074/jbc.M109.024125http://dx.doi.org/10.1126/science.300.5617.243ahttp://dx.doi.org/10.1093/toxsci/kfm018http://dx.doi.org/10.1093/toxsci/kfm018http://dx.doi.org/10.1007/s10856-011-4409-1http://dx.doi.org/10.1007/s10856-011-4409-1http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://rsif.royalsocietypublishing.org/http://dx.doi.org/10.1007/s10856-011-4409-1http://dx.doi.org/10.1007/s10856-011-4409-1http://dx.doi.org/10.1093/toxsci/kfm018http://dx.doi.org/10.1093/toxsci/kfm018http://dx.doi.org/10.1126/science.300.5617.243ahttp://dx.doi.org/10.1074/jbc.M109.024125http://dx.doi.org/10.1091/mbc.E02-01-0048http://dx.doi.org/10.1007/s11926-003-0071-zhttp://dx.doi.org/10.1007/s11926-003-0071-zhttp://dx.doi.org/10.1016/8756-3282(88)90004-Xhttp://dx.doi.org/10.1016/8756-3282(88)90004-Xhttp://dx.doi.org/10.1002/adem.200980026http://dx.doi.org/10.1016/j.jcis.2010.08.013http://dx.doi.org/10.1016/j.jcis.2010.08.013