Flow Chart Summarising Policy - WordPress.com · 2015-09-16 · Flow Chart Summarising Policy...
Transcript of Flow Chart Summarising Policy - WordPress.com · 2015-09-16 · Flow Chart Summarising Policy...

Page 4 of 35
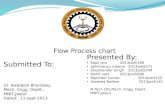
Flow Chart Summarising Policy
Pressure ulcer risk assessment completed within 2 hours of hospital admission or at first home visit
St George’s Hospital patients Community patients
Patient identified as AT RISK of pressure ulcer commence Part 2 of PUP Bundle:
- Adult hospital inpatients - Appendix C(1 or 6 as appropriate) - Paediatric hospital inpatients – Appendix C(2) - Patients at home appendix – Appendix C(4) - Interim Care Facilities - Appendix C(5) - QMUH appendix – Appendix C(3) - HMP Wandsworth (Jones Unit) - Appendix C(5)
For wound management of the pressure ulcer refer to Wound Management (Intranet) Policy
ALL patients with diabetes and a wound/pressure ulcer on the foot to be
referred to Diabetic Foot Team, ext 1859
A&E - use flow chart Appendix E Maternity – use flow chart Appendix F and Pressure Ulcer Prevention (PUP) bundle Appendix C(6) Paediatrics – use Pressure Ulcer Prevention (PUP) bundle Appendix C(2) All other adult inpatients – use Pressure Ulcer Prevention (PUP) bundle Appendix C(1) paed
All Grade 3 & 4 pressure ulcers to be referred to:
SGH - CNS in Pressure Ulcer Prevention on Bleep 6152 CSW – Community Tissue Viability Team 0208 812 4050
Use Pressure Ulcer Prevention (PUP) Bundle
Patients at home - Appendix C(4) Interim Care Facilities – Appendix C(5) QMUH - Appendix C(3) HMP Wandsworth (Jones Unit)– Appendix C(5)
Patient has a pressure ulcer: commence Part 3 of PUP Bundle including grading and DATIX report:
- Adult hospital inpatients - Appendix C(1 or 6 as appropriate) - Paediatric hospital inpatients – Appendix C(2) - Patients at home appendix – Appendix C(4) - Interim Care Facilities - Appendix C(5) - QMUH appendix – Appendix C(3) - HMP Wandsworth (Jones Unit) - Appendix C(5) -
Commence Part 4 of PUP bundle when transferring AT RISK or patients with a pressure ulcer between care environments in and outside of the hospital
Responsibility of healthcare professional
Referral pathways and contacts
Urgent referral pathway
SGH- St George’s Hospital QMUH – Queen Mary’s University Hospital HMP – Her Majesty’s Prison CSW – Community Services Wandsworth

Page 5 of 35
1. Introduction
This policy has been developed to assist staff in the provision of optimal care for all patients in pressure area care, in line with, safeguarding guidance (Social Care Institute for Excellence, Pan London Safeguarding Editorial Board 2011), National Institute for Health and Clinical Excellence (NICE) guidelines on pressure ulcer prevention (NICE 2005) and wound management, European Pressure Ulcer Advisory Panel (EPUAP) and National Pressure Ulcer Advisory Panel (NPUAP) guidance (EPUAP & NPUAP 2009), National Patient Safety Agency (NPSA) guidance (NPSA 2010) and Essence of Care guidance (Department of Health 2011).
2. Purpose
The policy aims to ensure that, whilst under the care of the Trust:
• no preventable pressure ulcers occur; • all pressure ulcers are managed optimally and safely; • pressure ulcer prevention and management is cost-effective.
3. Definitions
Grade Refers to the classification of a pressure ulcer on the basis of tissue layers involved. The EPUAP 2009 classification system is used. The definitions and a pictorial guide to grades of pressure ulcer are to be found in Part 3 of the PUP Bundle (Appendix C). Grade 1: (Formally referred to as Category/Stage I) Non-blanchable redness of intact skin Intact skin with non-blanchable erythema of a localized area usually over a bony prominence. Discoloration of the skin, warmth, edema, hardness or pain may also be present. Darkly pigmented skin may not have visible blanching. Grade 2: (Formally referred to as Category/Stage II) Partial thickness skin loss or blister Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled or sero-sanguinous filled blister Grade 3: (Formally referred to as Category/Stage III) Full thickness skin loss (fat visible) Full thickness skin loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Some slough may be present. May include undermining and tunnelling. Grade 4: (Formally referred to as Category/Stage IV) Full thickness tissue loss (muscle/bone visible) Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. Often include undermining and tunnelling

Page 6 of 35
Alternating Pressure Air Mattress (APAM) Overlay The standard equipment for pressure ulcer prevention. Suitable for patients up to a weight of 100 kg (approx 16 st). A mattress overlay is placed on top of a standard hospital or domestic mattress to prevent pressure damage to vulnerable patients. Alternating Pressure Air Mattress (APAM) Replacemen t System Pressure relieving mattress which replaces a standard hospital or domestic mattress and can be used for patients up to 190kg Alternating Pressure Air Mattress (APAM) Replacemen t System for very heavy patients Pressure relieving mattress which replaces a standard hospital or domestic mattress and can be used for patients up to 500kg. Care must be taken to ensure that the bed frame is of adequate carrying capacity to support the patient.
Pressure Ulcer
For the purposes of this policy, a pressure ulcer is defined as a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear. A number of contributing or confounding factors are also associated with pressure ulcers; the significance of these factors is yet to be elucidated (EPUAP & NPUAP 2009).
Pressure Ulcer Prevention (PUP) Bundle
A collection of documents (Appendix C) designed to assist clinicians with assessing pressure ulcer risk, prevention, management and communication between clinicians about pressure area care.
Avoidable Pressure Ulcer “Avoidable” means that the person receiving care developed a pressure ulcer and the provider of care did not do one of the following: evaluate the person’s clinical condition and pressure ulcer risk factors; plan and implement interventions that are consistent with the persons needs and goals, and recognised standards of practice; monitor and evaluate the impact of the interventions; or revise the interventions as appropriate. Unavoidable Pressure Ulcer “Unavoidable” means that the person receiving care developed a pressure ulcer even though the provider of the care had evaluated the person’s clinical condition and pressure ulcer risk factors; planned and implemented interventions that are consistent with the persons needs and goals; and recognised standards of practice; monitored and evaluated the impact of the interventions; and revised the approaches as appropriate; or the

Page 7 of 35
individual person refused to adhere to prevention strategies in spite of education of the consequences of non-adherence.
4. Scope
This policy applies to all clinical staff and all staff who handle or manage patients and/or pressure relieving equipment (temporary and permanent) working in any of the locations registered by St. George’s Healthcare NHS Trust (SGH) with the Care Quality Commission (CQC) to provide regulated activities. Locations are not necessarily geographically based or determined. Therefore, the term locations does not just refer to Trust buildings; it is the term used by the CQC to describe the hub of operations for a service or range of services and so includes all activities being performed in the course of performing one’s role.
All patients under the care of SGH, who are at risk of or with existing pressure damage will be managed in line with this policy, where clinically appropriate. Where, for individual reasons, it is not possible or clinically appropriate to manage patients in line with this policy, the reasons will be clearly documented. Adherence to this policy and its related procedures is the responsibility of all staff employed by the Trust.
5. Roles and Responsibilities
5.1 Executive
The Medical Director and Chief Nurse and Director of Operations have a responsibility for patient safety and therefore for pressure ulcer prevention.
5.2 Clinical staff
Clinical staff making decisions about the delivery of care must:
• follow the procedures outlined in the Pressure Ulcer Prevention (PUP) bundle (Appendix C);
• involve the patient and/or their relatives in the decision processes where possible; • report any adverse incidents or near misses involving pressure ulcer prevention
following the Trust’s Adverse Incident Reporting Policy and Procedures.
It is the responsibility of the admitting registered nurse and medical practitioner to carry out pressure ulcer risk assessment, pressure area assessment and wound assessment(s) if any.
5.3 Clinical Nurse Specialists
It is the responsibility of the Clinical Nurse Specialist in Pressure Ulcer Prevention (St George’s Hospital) and the Tissue Viability Team (Community Services) and Community Team Leader with equipment remit to:
• advise on formulation of Trust policy which is evidence based and reflects national and international guidance;
• facilitate the purchase of clinically effective equipment and consumables;

Page 8 of 35
• actively promote pressure ulcer prevention policy in their respective fields and facilitate/provide education programmes enabling staff to give best care in pressure ulcer prevention and management;
• provide the nursing, medical and finance directors with the information and data necessary to fulfil their roles with regard to pressure ulcer prevention and management.
5.4 Medical Physics & Bioengineering
Will ensure Trust-owned equipment necessary for pressure ulcer prevention and management is delivered in a timely manner, is safe, of adequate quality, maintained to high standards and that there is a mechanism for effecting repairs as required.
5.5 Pressure Ulcer Prevention Team/Equipment Supply Contractors
Will deliver, monitor, maintain and decontaminate equipment necessary for pressure ulcer prevention and management to agreed timescales and standards of quality.
5.6 Administrative and Information Technology Staff
Administrative staff will:
• provide management data as required;
• ensure risk management processes are followed;
• pressure ulcer data is collated and reported as required.
6. Pressure Ulcer Prevention and Management 6.1 The Pressure Ulcer Prevention (PUP) Bundle The pressure ulcer prevention bundle consists of five documents which are designed to assist staff in the delivery of pressure area care. They are obtainable through the Procurement Department using codes detailed in Appendix C. The bundle consists of:
• Covering sheet and prevention guidance (laminated, in each patient’s nursing folder)

Page 9 of 35
• Part 1. Risk assessment chart (double-sided, every admitted patient will have one in their nursing folder and will have assessment on admission and twice-weekly).
• Part 2. Repositioning chart (double-sided, every patient at risk of pressure damage will have one in their nursing folder). Chart to be completed daily.

Page 10 of 35
• Part 3. Pressure ulcer management chart and grading guide (laminated, in each patient’s nursing folder). Provides a flow diagram for managing newly identified pressure ulcers and illustrated guidance on pressure ulcer grading.
• Part 4. Communication sheet. To be used whenever a patient with or at risk of pressure ulcer is transferred from one area of the Trust to another or to outside the Trust. When completed it provides information on the history of the ulcer(s), clinical and administrative actions already taken, wound care and equipment needs and provides a record of other communication between areas.
There are variations in the PUP Bundle to cater for the specifics of locale (contacts, procurement of equipment) and patient group (adults, children, special needs etc). It is therefore important that each area is supplied with the appropriate Bundle. The content of the bundles for each area is outlined in Appendix C.

Page 11 of 35
6.2 Part 1: Risk and Skin Assessment
In the community:
Patients in their own homes, in interim care facilities and Queen Mary’s University Hospital with be assessed utilising the relevant PUP Part 1 sheet (Appendix C (4) (3) and (5) respectively).
• Patients in their own home will be assessed on the first assessment visit and subsequently whenever their condition changes, no less than monthly if they are classified as ‘at risk’ and three-monthly if they are not.
• All inpatients will be assessed within 2 hours of admission. Reassessment will take place whenever the patient’s condition changes, whenever transfers between areas occur and otherwise no less frequently than twice-weekly.
In St George’s Hospital:
With the exception of the cases outlined below, all patients admitted to St George’s Hospital will be assessed for presence and risk of pressure ulcer using Part 1 of the PUP Bundle (Appendix C (1) and (2)) within 2 hours of admission.
A&E department. Patients will be assessed within 2 hours of admission using an assessment flowchart initially (Appendix E). The outcome of the assessment will be documented in the Casualty Card. A full assessment utilising the appropriate inpatient PUP Bundle (Appendix C (1) and (2) will be carried out if the flowchart assessment reveals the patient has a pressure ulcer or suggests they are at risk of pressure damage.
Maternity department. Pregnant women will be assessed within 2 hours of admission using an assessment flowchart initially (Appendix F). A full assessment utilising the appropriate inpatient PUP Bundle (Appendix C (1)) will be carried out if the flowchart assessment reveals the patient has a pressure ulcer or suggests they are at risk of pressure damage.
Theatres. Patients will be assessed using the Protocol for positioning of patients in theatres (St George’s Healthcare Intranet; T:\Theatre Protocols 2011). The results of assessment will be documented in the Peri-operative Care Pathway.
Reassessment for all patients will take place whenever the patient’s condition changes, whenever transfers between areas occur and otherwise no less frequently than twice-weekly.
The principal tool for the assessment of pressure ulcer risk for adults is modified Waterlow and for children Glamorgan. In principle, adult patients with a score of 15 or more and children with a score of 10 or more will be considered ‘at risk’. In addition risk factors such as paralysis; loss of consciousness, epidural or existing pressure ulcer will automatically identify the patient as being ‘at risk’.
This policy emphasises that clinical judgement must be used in conjunction with the risk assessment tool in line with NICE (2005) r ecommendations.
Where patients are classified ‘at risk’ their skin will be assessed for pressure damage each time they are repositioned. Skin assessment involves visual inspection of the body for redness or evidence of tissue breakdown (ulceration, induration, temperature changes, colour changes, pain) where it comes in contact with the supporting surfaces, medical

Page 12 of 35
appliances and other parts of the body (e.g. where ankles come in contact with one another). The result of the inspection will be documented on the Repositioning Chart (PUP Bundle Part 2, Appendix C)
In addition to general risk of pressure damage, the local risks to tissue viability of clothing, surgical appliances and medical equipment will be considered. Examples include:
• Plaster of Paris and other casts
• Braces, splints and traction
• Oxygen masks, nasal cannulae, endotracheal tubes and other breathing apparatus with associated strapping
• Clothing with heavy seams, pockets (and content), elasticised cuffs and hard edges and poorly fitted footwear
• Anti-embolic stockings and compression bandaging
• Urinary catheters.
The patient’s skin where it comes into contact with appliances etc will also be considered a pressure area and monitored at the same time as all other pressure areas.
6.3 Part 2: Pressure Ulcer Prevention
All patients who are assessed as being at risk of pressure ulcer will be managed in line with the guidelines set out in Part 2 of the PUP Bundle (Appendix C).
Fundamental Equipment:
All patients at risk of pressure ulcer will be nursed on a pressure relieving mattress. The standard equipment for pressure ulcer prevention is an alternating pressure air mattress. However, air mattresses must never be used for pati ents with unstable spinal fractures.
It is important to provide the patient with a mattress suitable for their size and weight (see Appendix G). When assessing weight it is essential to consider body mass index and body morphology. Patients with high body mass index and unusual morphology (for example lower limb amputees) may require higher weight class equipment as they exert a higher unit pressure on the mattress for the same weight. The following is therefore a guide and manufacturer’s instructions should also be considered before a final decision is made:
• For patients up to a weight of 100 kg (approx 16 st) - a mattress overlay • For patients 100kg - 190 kg a standard mattress replacement system • For patients 190 kg+ a heavy duty mattress replacement system • For younger paediatric patients nursed in bed a smaller-celled overlay • For paediatric patients nursed in cots – a cot overlay • For patients in bassinets – a bassinet overlay
The processes for obtaining equipment are to be found in the Flow charts and Prevention Guidance of the PUP Bundle (Appendix C) for each respective area.

Page 13 of 35
• St George’s Hospital – Bleep 6681. If not provided within two hours escalate to bleep 6152 between 9am and 5pm on working days and bleep 6007 out of hours.
• Queen Mary’s University Hospital - Bleep 200 or 263
• In the patient’s home, Dawes House and HMP Wandsworth – complete WICES (Wandsworth Integrated Community Equipment Services) form and order from Mediquip via www.equipmentforyou.org.uk
Pressure relieving equipment will be monitored regularly when in use to ensure it is set up in line with manufacturers’ instructions, is functioning correctly, that all alarms are switched on and not muted and that the patient is not ‘bottoming through’ the mattress.
To check for ‘bottoming’ insert hand under the pressure relieving mattress underneath the patients centre of gravity (usually the sacral area). There should be a clear space between patient and underlying mattress (overlays) or bed frame (replacement systems). These checks will be recorded on the repositioning chart (PUP Bundle – Appendix C).
If a malfunction is suspected in powered pressure relieving devices, the ‘trouble-shooting’ guide (Appendix D) should be followed. If the fault cannot be resolved, the team providing the mattress will be contacted for a repair or replacement (see Appendix D for contact details).
Additional Equipment
In the patient’s home, patients at low but chronic risk of pressure damage may be nursed on a high-specification foam mattress.
In theatres, pressure areas will be protected as indicated by the Protocol for positioning patients in theatre (St George’s Healthcare Intranet; T:\Theatre Protocols 2011). All protective applications will be documented in the Peri-operative Care Pathway.
Additional protection may be indicated for heels of patients with diabetes as indicated by the diabetic podiatrist.
Soft pillows can be used to keep limbs from rubbing together
Repositioning
With the exception of cases outlined below, all patients at risk of pressure ulcer will be repositioned not less than four hourly when in bed if they are on a pressure relieving mattress and not less than two hourly if in bed without a pressure relieving mattress. Chair nursing will be limited to not more than 2 hours per session.
• Patients in the community and/or their carers will be advised of appropriate repositioning regimes (in line with Flow chart and Part 2 guidance – Appendix C (4)).
• Patients who are or will be normally chair-mobile, will be permitted to sit out longer than for two hours provided their tissue tolerance to the periods of time proposed has been established and is regularly monitored.
• Patients in theatres will be positioned and repositioned using the Protocol for positioning of patients in theatres (St George’s Healthcare Intranet; T:\Theatre

Page 14 of 35
Protocols 2011). Positioning will be documented on the Peri-operative Care Pathway.
With the exception of Theatres noted above, all repositioning will be documented using the PUP Repositioning Chart in Part 2 of the PUP Bundle (Appendix C)
Medical appliances
Patients who require the attachment of medical appliances will have skin contact areas carefully monitored and consideration will be given to applying additional protection. Plaster of Paris and other casts will be applied and managed in line with local Trust policy and NPSA recommendations (NPSA 2009).
Refusal of treatment: patients who have mental capa city
Patients who have mental capacity have the right to refuse treatment. To ensure the patient and their carers where appropriate, are able to make an informed choice, a multidisciplinary team approach will be adopted to ensure the risks and potential consequences of non-compliance and/or refusal of recommendations of care are understood. If patients and their carers where appropriate, decide against preventive treatment or demonstrate non compliance, this should be documented in the patient’s record.
Refusal of treatment: patients who do not have ment al capacity
Where patrients refuse necessary treatment and it is suspected that they lack ‘capacity’, the Mental Capacity Act (2005) in conjunction with the Trust Policy on Obtaining Valid Consent for Treatment should be utilised to ensure decisions are made in the patient’s best interests (see also Safeguarding Adults (Clin 5.21) and Safeguarding Children and Young People (Clin.5.6) policies).
At times relatives/informal carers/friends (who may or may not have lasting power of attorney with regard to health matters may object to necessary treatment being given (such as a pressure relieving mattress or repositioning). In such circumstances every effort should be made to reach agreement; however given pressure area care is time-sensitive it may be necessary for staff to act contrary to the wishes of relatives, carers and/or friends to ensure the patient receives appropriate pressure in the patient’s best interest as per the Mental Capacity Act (2005). Advice should be sought at the earliest earliest opportunity. Advice and support can be sought from the Safeguarding Lead (see Part 3 of PUP Bundle for contact details) and/or the Legal Services Manager
6.4 Part 3: Managing Pressure Ulcers
When patients develop or are admitted with pressure ulcers:
• the pathway outlined in Part 3 of the PUP Bundle will be followed (Appendix C);
• all pressure ulcers will be reported using the Trust’s Datix Web Adverse Incident reporting system and to local monitoring systems as appropriate;

Page 15 of 35
• pressure ulcers will be graded using the EPUAP (2009) grading system (see Part 3 of PUP Bundle – Appendix C);
• pressure ulcers will be photographed, with patient consent and in line with consent to medical photography policy;
• all diabetic patients with pressure damage of their feet will be referred to a diabetic podiatrist.
All pressure ulcers graded 3 or 4 will be declared as Serious Incidents (SIs). All pressure ulcers Grade 3 or 4 will be investigated using root cause analysis, with the exception of those pressure ulcer which are discovered on admission from elsewhere, which will be referred to the transferring organisation for investigation if appropriate. The findings and proposed actions to prevent recurrence of pressure damage will be presented monthly to the Nursing Board. Where there is suspicion that pressure damage occurred as a result of deliberate abuse or neglect, the patient should be referred to the appropriate Safeguarding Lead (Part 3 of PUP Bundle, Appendix C).
Wounds will be documented and managed in line with the Trust Wound Management Policy. Where the patient already has a preventative strategy in place, this will be evaluated in the light of ulcer development, reviewed and altered as appropriate to avoid further occurrence of pressure damage. Where causes and/or remedial action are not clear, the patient should be referred to CNS-Pressure Ulcer Prevention (bleep 6152) in St George’s Hospital and to the Tissue Viability Team (020 8812 4051) in the community.
6.5 Part 4: Communication
When patients at risk of or with pressure ulcers are transferred to another healthcare institution or discharged into the community, the team taking over their care will be provided with a completed Communication Sheet (Part 4 of the PUP Bundle – Appendix C). A copy of the Communication Sheet will be retained in the medical record.
7. Dissemination and implementation
7.1 Dissemination: Existing documents will be replaced on the Intranet with the new version. Physical copies of the old version will be removed from the ward areas by the Pressure Ulcer Prevention Team The new version will be made available via the Trust Intranet only. Awareness of the policy will be disseminated by the Pressure Ulcer Prevention (PUP) Task Group through Staff Induction programmes, PUP training sessions and all appropriate opportunities. 7.2. Implementation The policy will be embedded through training and monitoring provided by members of the PUP Task Group. All persons involved in the pressure ulcer prevention and management process will receive training appropriate to their role. In particular nurses and Health Care Assistants will receive training as part of their induction and mandatory training programmes.