Flashers, Floaters and Double Vision. Objectives Develop a safe approach to the disposition of...
-
Upload
chase-regan -
Category
Documents
-
view
219 -
download
0
Transcript of Flashers, Floaters and Double Vision. Objectives Develop a safe approach to the disposition of...

Flashers, Floaters and Double Vision

Objectives
•Develop a safe approach to the disposition of patients complaining of both...
•sudden onset of unilateral flashers and floaters
•double vision

Case 1•62 y.o. female with hypertension and no
ocular history
•1 week of a large floater in her left eye
•Believes her vision on the left has deteriorated
• In this same week she had an episode of “light flashes” in the left periphery
•Assessed by optometry 6/12 ago and says “everything was normal”

Case 1
•corrected right 20/20, left 20/50
•pupil exam, field testing normal
•no RAPD
•dilated direct ophthalmoscopy normal
•U/S not done

• Ocular
• Floaters and/or flashers
• PVD - 24% (50-59) 87% (80-89)
• RD - 0.3% (lifetime), 14% (if complaining of flashes/floaters)
• Predominate Floaters
• vitreous hemorrhage - usually proliferative diabetic retinopathy
• Predominate Flashers
• oculodigital stimulation
• rapid eye movements
• age related macular degeneration
• Non-ocular
• migraine with aura - binocular visual problem
• occipital lobe disorder - binocular visual problem
• postural hypotension- binocular visual problem


Disposition ?
•What would you do in this case at 1pm on Monday?
•What would you do in the case at 1am on Saturday?
•Is this case an “emergency” or “urgency”

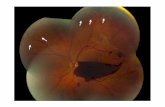
Does this patient have retinal
detachment? •Flashes/Floaters (one/both) LR of 0.79-2.1
•Subjective OR objective visual loss with flashes / floaters LR of 5.0
•Vitreous Hemorrhage or Pigment on slit lamp exam LR 10 - 44
•No data for “sudden grey curtain obstructing vision”

Can bedside U/S safely rule out retinal
detachment?•prospective study of U/S scan by ED physicians in patients with sx/sx of RD yielded a 97% sensitivity, 92% specificity (Shinar Z. Chan L. Orlinsky
M. Use of Ocular Ultrasound for the Evaluation of Retinal Detachment. J Emerg Med. Jul 20 2009.)
•another study with similar methodology demonstrated a 100% sensitivity and 83% specificity (Yoonessi R. Hussain A. Jang TB. Bedside Ocular Ultrasound for the Detection of Retinal
Detachment in the emergency Department. Acad Emerg Med. Sep 2010.)

Is RD a true emergency?• MORD pilot study identified no R.F. other than distance of the
tear from the fovea for progression of MORD to macula-off RD (a finding not done in the ED). In this study 26% of patients were treated out-of hours.
• The 1995 AAO stance is that MORD be treated within 24 hours (American Academy of Ophthalmology. Ophthalmic procedure assessment. The repair of rhegmatogenous retinal detachment. Ophthalmology 1995; 103:1313-1324.).
• A growing body of literature suggests no long term difference providing that repair occurs within 3 days of symptom onset. (Anatomic and visual outcomes in early versus late macular-on primary retinal detachment repair. Retina. 2011 jan; 31(1):93-8.)
• “best evidence practice for MORD would indicate that surgery be scheduled no later than 7 days of symptom onset.” (Letter in Eye (2006),
1105-1106)
• Macula-off Detachment - a recent study found that repair of macula-off detachment in the first three days after the event results in equivalent outcomes to repair in 24 hours, but repair of greater than one week had significantly worse outcomes.

Case 1- Resolution•62 y.o. female with OS flashers /
floaters, objective visual loss, an normal eye exam.
•Referred that day for opthalmology assessment
• Found to have PVD with a supra-temporal retinal tear.
•Referred to a retinal surgeon at a tertiary centre for definitive management.


Disposition ?
•What would you do in this case at 1pm on Monday?
•What would you do in the case at 1am on Saturday?
•Is this case an “emergency” or “urgency”

RD Summary
•Patients with acute onset of either flashers &/or floaters with subjective/objective visual loss, and signs of vitreous hemorrhage need a same day referral.
•RD likely represents an urgency vs. emergency based on available literature.

Case 2• 75 y.o. male with double vision and left
eyelid ptosis, previously completely well.
• Awoke in the AM c/o he was seeing double esp. when looking up.
• Denies any visual blurring, headache, fever, neck pain or “b symptoms.”
• Remainder of R.O.S is normal.
• PMHx: HTN, lipids, GERD, CAD, AF - therapeutic INR, Pacemaker - SSS

Physical Findings• obvious droopy left eyelid
• right 20/25, left 20/40
• PERL, no RAPD
• right normal EOM
• left cannot elevate, depress or adduct
• IOP 13 mmHg bilaterally
• SLE normal anterior chamber & cornea
• Fundi exam attempted - but limited (not dilated)


Differential? • Binocular Diplopia
• Cranial Nerve - idiopathic (microvascular), stroke, compressive lesion, infectious (sinus thrombosis), alcohol related (WE)
• Mechanical - typically assc. with proptosis and pain - i.e. Grave’s dx, orbital myositis, base of skull tumors
• Neuromuscular - typicall assc. with systemic illness - i.e. botulism, GBS (Miller Fisher Variant), MG, MS
The can’t miss diagnosis have more than just CN findings.


Disposition? •Should I order a CT/MRI, what type?
•Can I safely send this patient to the family physician for follow up in 4-6 weeks?
•Can I safely send this patient for opthalmology f/u tomorrow?
•Do I need to call the opthalmogist now?
•Do I need to call the stroke MD now?

Red Flags - Admit/Image
•More than one cranial nerve deficit
•Pupillary involvement of any degree
•Any neurologic symptoms besides diplopia
•Pain
•Proptosis

Who Can I d/c without any imaging?
•Unilateral
•Single Cranial Nerve Palsy
•Normal pupillary light response
•No other signs or symptoms

Case 2
• Patient was f/u by opthalmology 2 days post d/c.
• Visit 1 - 80% ptosis, pupil sparing, no adduction, elevation, depression of L eye
• Visit 2 (2/52) - near 100% ptosis, pupil sparing, no adduction, elevation, depression L eye
• Visit 3 (4/52) - 30% ptosis, able to adduct past midline, slight elevation and depression
• Visit 4 (8/52) - no ptosis, normal EOM, no double vision

Diploplia Summary•Patients with isolated pupil sparing 3rd,
4th and 6th CN palsies likely have idiopathic or microvascular disease.
•EXTREMELY CAREFUL NEURO EXAM
•In the above cases emergent management is not often necessary, although urgent opthalmology referral, with a call from the ER physician should be encouraged.