Financial risk and hospital cost for elderly patients in non-age stratified urology DRGS
-
Upload
eric-munoz -
Category
Documents
-
view
215 -
download
2
Transcript of Financial risk and hospital cost for elderly patients in non-age stratified urology DRGS

FINANCIAL RISK AND HOSPITAL COST FOR
ELDERLY PATIENTS IN NON-AGE
STRATIFIED UROLOGY DRGS
ERIC MUNOZ, M.D., M.B.A. JONATHAN GOLDSTEIN, M.P.A. STEVEN WILKINS, M.D. HARRIS STERMAN, M.D. ERROL MALLET, M.D. LESLIE WISE, M.D.
From the Division of Urology, Department of Surgery, Queens Hospital Center, Jamaica; The Long Island Jewish Medical Center, New Hyde Park; State University of New York, Stonybrook; and City University of New York School of Medicine, New York, New York
ABSTRACT- The Diagnostic Related Group (DRG) hospital payment system may be inequitable for certain groups of Medicare patients. This study of 216 Medicare urology patients in the ten non- age stratified urology DRGs demonstrated that patients seventy years of age and older (70 +) had higher resource consumption than patients under seventy years of age (70 - ). Findings were: (1) older patients (70 +) had higher total hospital costs ($12,022 per patient) than younger patients (70 -) ($9,872 per patiem); (2) a longer hospital length of stay (14.2 days vs 11.6 days); (3)financial risk of $1,756 loss per (70-t) patient vs $1,309 profit per (70 -) patient (p < 0.05); (4) more diagnoses and procedures per patient, and (5) a higher mortality (4.0 % vs 3.3 % ). These findings suggest that the current DRG scheme may be inequitable vis-a-vis the older urology patient in non- age stratified DRGs, and thus could limit access and quality of care for these patients in the future.
The equity of the Medicare Diagnostic Related Group (DRG) prospective hospital payment system is being questioned by various con- sumers of American hospital care.1~2 The DRG system is supposed to reimburse for hospital services needed, but not necessarily hospital services delivered. Thus, certain groups of pa- tients may generate financial risk to hospitals under the current DRG payment scheme. The DRG classification system sometimes accounts for differences in the patient’s age.3 For exam- ple, of the thirty-six urology DRGs, twenty-six (68.4%) are stratified by the patient’s age (either O-17 years of age, 18-69 years of age, or above 69 years of age).4 The remainder of urol- ogy DRGs have no resource stratification by age.
The Federal Medicare DRG prospective hos- pital payment system has been on line for five years.5 So far there appear to be no major ad-
verse effects for American health care on either access or quality of care from DRGs.~ However, the hospital industry contends that the DRG program has caused a significant worsening of the fiscal health of American hospitals, and that certain groups of patients may suffer in the fu- ture.7 The purpose of this project was to test the hypothesis that financial risk would be gener- ated by older urology patients in the non-age stratified urology DRGs.
Material and Methods
All Medicare urology patients (N = 216) ad- mitted from January 1, 1985, to December 31, 1986, to the Long Island Jewish Medical Center (an 805-bed teaching hospital in suburban New York City) in any of the ten non-age stratified urology DRGs were studied (Table I). Our hospital is categorized as an urban teaching
UROLOGY ’ MAY 1989 / VOLUME XxX111, ItUMBER 5 445

DRG
303 315 334 335 341 344 345 350 351 352
TABLE I. Ten non-age stratified urology DRGs
Description
Kidney, ureter, and major bladder procedure for neoplasm Other kidney and urinary tract OR procedures Major male pelvic procedures with CC Major male pelvic procedures w/o CC Penis procedures Other male reproductive system OR procedures for malignancy Other male reproductive system OR procedures except for MA Inflammation of male reproductive system Sterilization male Other male reproductive system diagnoses
DRG Weight Index
2.5133 2.4625 1.5450 1.3449 0.9879 1.1088 0.8247 0.6033 0.2627 0.6319
hospital by the DRG reimbursement scheme; standard New York State DRG methodology was used for this analysis. Patients were grouped into two age categories; those under seventy years of age, and those seventy years of age and older.
Hospital costs in each age group (exclusive of physicians’ fees) were computed for each pa- tient by hospital service area to include: room and board, laboratory (urinalysis, hematology, coagulation, biochemistry, and microbiology), radiology, blood and blood products, operating room-recovery room, central supply-pharmacy, and other (EKG, pathology, respiratory therapy, etc). A number of characteristics were analyzed for each patient including: mean total hospital cost per patient, mean hospital cost per patient for each hospital service, mean DRG reimbursement per patient, mean profit/loss per patient, mean hospital length of stay (LOS) per patient, the mean number of diagnostic codes (ICD-g-CM) per patient, mean number
70 t 1
SO-
50 -
I- 40 - 3
k30-
20-
10 -
Of-
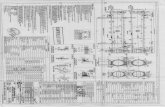
??70 YEARS AND ABOUE COSTS
??UNDER 70 YEARS
FIGURE 1. Patients seventy years of age and older consumed disproportionately larger share of hospi- tal resources than patients seventy years of age and under.
of procedure codes (ICD-g-CM) per patient, the percent outliers, and mortality. The Stu- dent’s t distribution was used to test for statisti- cal significance between groups of patients.
Hospital Costing Methodology
Hospital cost per patient was obtained by uti- lizing per patient charge specific data and con- verting these charges to hospital costs. Cost-to- charge ratios utilized by our hospital’s accounting division were used to convert charges to costs. The following ratios were used for each hospital service category.
Room and board 0.75 Laboratory 0.40 Blood (storage, processing,
transfusion, and products) 1.15 Pathology 2.42 Diagnostic radiology 0.94 Therapeutic radiology 1.71 Operating room 1.10 Recovery room 1.15 Respiratory therapy 0.76 Electrocardiology 0.25 Electroencephalography 1.40 Medical supplies 1.00 Pharmacy 1.00 Diagnostic ultrasound 0.46 Computed tomographic scan 0.53 Emergency department 0.91 Pulmonary function 0.08
Thus to obtain the hospital cost for labora- tory charge of $100, the following calculation was performed ($100 x 0.40 = $40); medical supplies ($100 x 1.00 = $100); therapeutic ra- diology ($100 x 1.71 = $171); and so on.
Results The 216 patients in the ten non-age stratified
urology DRGs generated an aggregate hospital cost of $2,392,882 vs a DRG reimbursement of $2,292,486 yielding an aggregate loss of $100,396. However, patients seventy years of
UROLOGY / MAY 1989 / VOLUME XXXIII, NUMBER 5

TABLE II. Urology: cost for hospital service by age
Age (Yrs.) Sample
Size R&B7 Lab$ Blood X-ray OR-RR5 Pharm Other Total
Under 70
70 and older
All
91 $5,480 $1,122 $31 $464 $1,213 $757 $716 $9,872 f 5,739 f 1,566 f 51 + 1,024 + 1,128 f 1,146 zt 1,381 f 10,386
125 6,950 1,388 37 530 1,350 772 993 12,022 f 6,173 f 2,044 f 54 f 800 + 848 + 1,458 + 1,685 + 11,775
216 $6,331 $1,276 $35 $502 $1,292 $766 $876 $11,078
*Mean per patient, + standard deviation. fRoom and board. $Laboratory (urinalysis, hematology, coagulation, biochemistry and microbiology). §Operating room-recovery room.
age and older consumed a disproportionately larger share of hospital resources than patients under seventy years of age. For example, pa- tients under seventy accounted for 42.1 percent of total hospital admissions, but generated only 37.2 percent of total hospital costs; whereas pa- tients seventy years of age and older accounted for 57.9 percent of total hospital admissions, but generated 62.8 percent of total hospital costs (Fig. 1).
Mean total hospital cost per patient was higher for patients seventy years old and older ($12,022) vs p t t a ien s under seventy years of age ($9,872) (Table II). M ean hospital cost per pa- tient was higher in every hospital service cate- gory for older patients. Mean DRG reimburse- ment per patient generated losses for patients seventy years of age and older ($1,756 loss per patient) versus profits for patients under seventy years old ($1,309 profit per patient), p < 0.05 (Table III). Although older patients had a slightly lower DRG case-mix index, they had a much longer hospital stay, and higher mortal- ity rate. In addition, older patients had more diagnoses and procedure codes per patient.
Comment The purpose of this study was to test the hy-
pothesis that financial risk would be different by age for Medicare patients in the non-age
stratified urology DRGs. We found that pa- tients seventy years of age and older in these DRGs generated significant financial risk under DRGs, in addition to having a longer total hos- pital stay, more diagnoses and procedures per patient, and a higher mortality than patients under seventy years old. These findings raise questions about the equity of the DRG scheme vis-a-vis older urology patients in these DRGs and whether or not this system may affect both the access and quality of care for these patients.
The DRG payment system is undergoing con- stant examination regarding equity, access, clinical research, and technology diffusion8 As in any large aggregate grouping scheme, there will be inequities and inaccuracies in payment. At present, the main determinants of hospital DRG payment are based on whether or not they are urban or rural, teaching or non-teach- ing, disproportionate share (i.e., treat more poor patients), and which region of the country they are in (the level of standard reimburse- ment, one component of DRG payment, varies by region for now), Some attention has focused on the fact that differences in severity of illness ( i.e., degree and type of patient’s illness) may affect the cost per patient within each DRGSg Certain types of hospitals, mainly teaching and public, are thought to be at risk from treating more severely ill patients. Both the Health Care
TABLE III. Urology: resource characteristics by age*
Age (Yrs.) DRG Weight Index Profit/Loss Hospital LOST No. of Dx$ No. of Proc$ % Outliers % Mortality
Under 70 1.8507 $1,309§ 11.6 3.3 f 0.7510 f 9,431 k 11.8 + 2.5
70 and older 1.6790 ($1,756) 14.2 3.5 f 0.7163 f 9,601 f 11.7 f 2.4
All 1.7513 ($465) 13.1 3.4
‘Mean per patient, f standard deviation. ILength of stay (days). $(ICD-g-CM) diagnosis and/or procedure codes per patient. $Statistically different at p < 0.05 from seventy years of age and older category.
3.0 8.8 3.3 *2.1 zt 28.5 f 18.0
3.5 7.2 4.0 k2.1 f 26.0 f 19.7
3.3 7.9 3.7
UROLOGY / MAY 1989 / VOLUME XxX111, NUMBER 5 447

Financing Administration (HCFA) and the Pro- spective Payment Assessment Commission (Pro- PAC) are studying the costs and benefits of vari- ous DRG severity adjusters and the redistributive effects of same. As of the most re- cent Federal regulations, no modification of DRGs regarding severity of illness has been im- plemented. lo
The question of vulnerability of various age groups of Medicare patients (especially very elderly Americans) from DRGs has been ad- dressed by HCFA. A large recent analysis by HCFA demonstrated that hospital charges were not substantially different from average charges per DRG for Medicare patients eighty years of age and older. l1 However, our study demon- strates that a hospital-specific analysis (such as we performed) may generate contradictory findings regarding this assumption.
We have generated data to suggest that our hospital may face financial risk from older sur- gical patients in general.12 Our hospital now appears to face some degree of risk from older urology patients in the ten non-age stratified DRGs we studied. Although there are many components to hospital strategic planning, this analysis suggests that this population of elderly urology patients may be unattractive to our hospital; thus DRGs may reduce both the access and quality of care for these patients. Urologists must continue to analyze the changes underway in surgical health care financing to assure the best possible urologic care in the future. It is important that payment changes underway in American health care be as equitable as possible to optimize hospital care in the future.
Conclusions
Prospective payment systems using DRGs are changing the financial incentives offered to hos- pitals. This study of 216 Medicare patients treated in the ten non-age stratified urology DRGs demonstrated that patients seventy years
of age and older had greater resource consump- tion and generated financial risk under DRGs compared with patients under seventy years old. This study suggests that the current DRG system may be inequitable to certain groups of older urology patients, and thus could limit both their access to and quality of care in the future.
Department of Surgery Long Island Jewish Medical Center
New Hyde Park, New York 1_1042 (DR. MUNOZ)
ACKNOWLEDGMENT. To James Moyer, Seth Warren, and Gordan Doletto, Divisions of Management Information Systems and the DRG Task Force of the Long Island Jew- ish Medical Center; Katherine Mulloy for data computa- tion, and to Christina Weiss for manuscript assistance.
References
1. Horn S, et al: Interhospital differences in severity of illness, N Engl J Med 313: 20 (1985).
2. Muiioz E, et al: Mode of admission and cost: public hospi- tals face financial risk, Am J Pub Health 76: 696 (1986).
3. Fetter RB: Diagnosis Related Groups, Clin Res 32: 336 (1984).
4. Healthcare Financing Management Association: Descrip- tion and analysis of Medicare Prospective Price Setting, Oak Brook, Illinois, Healthcare Financing Management Association, 1984.
5. Schramm CJ, and Gabel J: Sounding board: prospective payment: some retrospective observations, N Engl J Med 318: 1681 (1988).
6. Medicare Prospective Payment and the American Health Care System. Prospective Payment Assessment Commission. Re- port to Congress, Washington, D.C., June 1988.
7. McCarthy CM: DRGs-five years later, N Engl J Med 318: 1683 (1988).
8. Office of Technology Assessment, Congress of the United States: Medicare’s Prospective Payment System, New York, Springer, 1986, pp 59-131.
9. Jencks JF, Dobson A, and Willis P: Evaluating and improv- ing the measurement of hospital case mix, Health Care Fin Rev (Ann Suppl): 1 (1987).
10. Federal Register, United States Government Printing Of- fice, Washington, D.C. 53:103: 19497 (1988).
11. Jencks SF, and Kay T: Do frail disabled, poor and very old Medicare beneficiaries have higher hospital charges, JAMA 257: 198 (1987).
12. Muiioz E, et al: Age, resource consumption, and outcome for surgical patients at an academic medical center, Surgery 103: 335 (1988).
448 UROLOGY / MAY 1989 i VOLUME XxX111. NUMBER 5