final thesis
-
Upload
hadaitullah-baqri-baltistani -
Category
Health & Medicine
-
view
1.249 -
download
0
Transcript of final thesis

Assessment of Prescribing Practice of Antibiotics in common cold
(ARI) in children under the age of 5 years in PIMS Islamabad
Submitted To:
Najmuddin Bakrey
Submitted By:
Hadaitullah
Program:
Msc.IR
Semester:
2ND
Registration no:
1443_311007
PRESTON UNIVERSITY, Islamabad campus
1

ACKNOWLEDGEMENTS
All praise and thanks to Allah all mighty, the most merciful and beneficent. He has
always helped us out whenever we are in need.
First of all, our greatest gratitude to Sir.Nujmuddin, our research supervisor, who has
been a source of inspiration for us. He always listened to us and guided us in a very
empathetic way. His constant guidance, criticism and encouragements have enabled us to
accomplish this task. We would like to thanks our parents for their love prayers and
opportunities they provided. We would also like to thanks the chief pharmacist of the
PIMS who allowed me for data collection in PIMS Islamabad.
In the last I would thank specially Sir.Nujmuddin who helped me a lot and spared their
precious time for us.
Hadaitullah
2

Table of contents Table of contents
Sr. No Contents Page No
1. Title Page01
2. Acknowledgments 05
3. Abstract 07
4. Chapter # 1Introduction 08
5. Chapter # 2Objectives 18
6. Chapter # 3Methodology 20
7. Chapter # 4Results 22
3

Abstract:
Background: The spread of antibiotic-resistant bacteria is associated with antibiotic use.
Children receive a significant proportion of the antibiotics prescribed each year and
represent an important target group for efforts aimed at reducing unnecessary antibiotic
use. The judicious prescription of antibiotics has become a central focus of professional
and public health measures to combat the spread of resistant organisms.
Objective: To assess the prescribing practice of Antibiotics in common cold (ARI) in
children under the age of 5 years in PIMS Islamabad and to compare it with standard
treatment guideline.
Significance: Descriptive cross sectional study: A total of 100 prescriptions of children
under the age of 5 years were obtained from the hospital. Prospective method was used to
collect the prescriptions.
Antibiotics were prescribed to 70% of children presenting with symptoms of common
cold in different combination. About 53% of patients were given Antiobiotic +
Antipyretic + Antihistamine combination. About 30% of patients were given Antipyretic
and Antihistamine combination. About 7% of patients were given Antibiotic+ Antipyretic
combination. About 5% of patients were given antibiotic and antihistamines combination
and about 5% of patients were using Antiobiotic +Antipyretic+ Antihistamine
+Multivitamins combination. There was only one class of antibiotic was prescribed by
the physicians and that was penicillin. The number of drugs prescribed per patient varies
considerably for treatment of common cold in childerns. About 55 % of prescription
contains 3 numbers of drugs. 40% of prescription contains 2 numbers of drugs and only 5
% of prescription contains 4 numbers of drugs.
Conclusion: Antibiotics are commonly used in common cold in children under the age of
5 years. The outcome of such irrational practices was loss of these limited resources and
emergence of antibiotic resistance and result poor quality of health.
4

Chapter 1:
Introduction
5

INTRODUCTION:-
The common cold is not a single infectious disease, but rather a group of self-limiting
viral upper respiratory infections (URIs) producing a similar clinical syndrome.[1] The
average preschool child contracts approximately 6 to 10 colds per year, and the average
adult has 2 to 4 colds annually. Roughly 23 million lost work days and 26 million missed
school days are the result of the common cold each year. Many more persons continue
their usual activities with lower productivity and uncomfortable symptoms. Furthermore
expenditures for products used to treat cold symptoms exceed $2.5 billion annually after
adjusting for inflation[2] The common cold is generally regarded as a mild condition that
rarely causes significant morbidity. However, serious exacerbations of underlying disease
may occur in patients with asthma or pre-existing obstructive lung disease. Patients with
the common cold are also more susceptible to acquiring otitis media and sinusitis. [3]
Pediatric populations are important targets for efforts aimed at reducing unnecessary
antibiotic use. Environments unique to children, such as day care and school, enhance the
transmission and spread of drug-resistant S pneumoniae.[4] The frequency and duration of
prior antibiotic exposure are strongly associated with the spread of drug-resistant S
pneumoniae, and children receive a significant proportion of the total antibiotics
prescribed each year. [5]
The common cold is associated with considerable costs in terms of decreased
productivity; time lost from work or school; visits to healthcare providers; and the
volume and cost of drugs prescribed. [6] Despite the lack of effectiveness of antibiotics for
treating common cold symptoms (rhinorrhoea, stuffiness, acute cough, sore throat,
pharyngitis, and laryngitis), general practitioners (GPs) frequently prescribe antibiotics
for patients with such symptoms in response to patients expectation or doctors
perceptions of these expectations.
The over use of antibiotics for primarily viral respiratory tract infections has been
suggested as a contributing factor in the rise of antibiotic pathogens like Streptococcus
6

pneumoniae because of selective pressure, particularly that exerted by broad-spectrum
antibiotics. [7]
INCIDENCE AND PREVALANCE OF COMMON COLD:-
The incidence of infection peaks in the early spring (April and May) and fall, reaching
the highest incidence in the fall. The incidence of infection from coronavirus, the second
most common viral agent, peaks in the early summer and again in the autumn to early
winter. Coronavirus has been detected in up to 30% of upper respiratory infections. [1] The
pattern of RSV infection is similar to that for rhinovirus; however, the peak incidence is
slightly later in the spring (April through June) and fall (October through November). [2]The isolation of influenza A virus from patients with cold-like symptoms is indicative
of a mild influenza illness, and the incidence is expected to follow trends in influenza
illness within a community. Parainfluenza virus type 3 is present in summer months and
is associated with annual outbreaks or epidemics Isolation of adenovirus is fairly constant
throughout the year." [2]
EPIDEMIOLOGY:-
Transmission of the common cold may occur by direct contact with nasopharyngeal
secretions or by inhalation of small and large airborne particles. Viruses can be isolated
from the hands of patients with the common cold. Transmission may occur with a simple
touch or hand¬shake. [3] In addition, viruses can remain viable in nasal secretions for
several hours after being deposited on inanimate objects (e.g., door handles or faucets).
The uninfected individual acquires the virus on his or her hands, and then inoculates the
mucosal surfaces by touching the face, nose, or eyes. IS Prevention of transmission is
possible by washing hands frequently with disinfectants, by using of virucidal tissues,
and perhaps by avoiding facial and eye contact with the hands. However, these methods
are not very practical. One study suggested that aerosol transmission is the chief mode of
transmission in adults. [8]
7

Acute respiratory infections (ARI) are among the most prevalent factors of morbidity in
the world. ARI related mortality is a major issue in children under five years of age in
developing countries.[8] According to WHO, estimated morbidity averages bronchiolitis,
and obstructive laryngitis. [9] One million deaths due to measles, 350,000 to pertussis, and
8,000 to diphtheria are to be added. Infectious agents are first, S. pneumoniae, H.
influenzae and respiratory syncytial virus, second, S. aureus, influenza, and para
influenzae viruses, adenovirus. [8,9] Control programs of ARI are based upon adequate
medical care in primary health care centers, training of health workers, maternal
education, and immunizations. Such programs set up in some developing countries
enabled a 20% decrease of infant mortality and a 25% decrease in children under five
years of age. [10]
Acute respiratory infections (ARI) are a leading cause of childhood morbidity in
Pakistan. The National ARI Control Programme was launched in 1989 in order to reduce
the morbidity attributed to ARI and rationalize the use of drugs in the management of
patients with ARI. [11] WHO standard ARI case management guidelines were adopted to
achieve these objectives. The medical staff at Children’s Hospital, Islamabad were
trained in such management in early 1990; further training sessions were conducted when
new staff arrived. [10,11]
Among under-5-year-olds in Pakistan, acute respiratory infections (ARI) are responsible
for more than one quarter of deaths in the community and one-third of deaths occurring
in hospitals. [12] ARI is also the leading cause of morbidity in childhood. Factors
contributing to complications and mortality due to ARI include delays in talking the child
to a health care provider. Misdiagnosis or delay in diagnosis by the health professional
and inappropriate use of antibiotics for treatment of ARI. [8,9]
Seven countries have established national task forces for ARI control, four have prepared
documents for implementation of the programme and six have specific budget lines for
the ARI Control Programme in the 1988-1989 biennium. [9,10]
CONDITIONS AND ETIOLOGY:-
8

The Common Cold is not a single infectious disease, but rather a group of self-limiting
viral upper respiratory infection (URIs) producing a similar clinical syndrome [1]. URIs
are the most common infectious diseases. They include rhinitis (common cold), sinusitis,
ear infections, acute pharyngitis or tonsillopharyngitis, epiglottitis, and laryngitis—of
which ear infections and pharyngitis cause the more severe complications (deafness and
acute rheumatic fever, respectively) [1,2]
There are many viral pathogens which can cause the symptoms of the common cold; the
most common are the more than 100 serotypes of rhinoviruses.[11] The type of virus
responsible for the greatest number of colds. Other viruses that cause colds include
enteroviruses (echovirus and coxsackie viruses) and coronavirus. In most cases, a specific
virus causes a person to be ill only once, after which they are immune to that virus [11,12].
An estimated 25 million individuals seek medical care for uncomplicated upper
respiratory tract infections (URI) annually in the United States. [13]
TREATMENT OPTIONS AVAILABLE FOR ARI:-
There is no widely accepted specific therapy for the common cold. Use of interferon
nasal spray.[14] zinc gluconate lozenges.i" high-dose vitamin C [15] and investigational
antiviral drugs[14,15] has shown limited or no benefit in shortening the duration of
symptoms and/or reducing viral shedding. High-dose vitamin C (at least 1 gI day) may
provide a small benefit; however, this benefit is controversial. [14] In addition, several of
the treatments (interferon, zinc gluconate, and antiviral drugs) are associated with
significant side effects. Zinc gluconate lozenges are unpalatable. A nasal spray
containing soluble intercellular adhesion molecule 1 (ICAM-l) was shown to reduce cold
symptoms by almost 50% when used before or within 12 hours after experimental
rhinovirus infection. ICAM-l is responsible for binding of rhinovirus to susceptible
nasopharyngeal cells, permitting virus entry. Soluble ICAM-1 is a competitive inhibitor
of this binding. It is likely that this therapy will be expensive if it becomes available.
Moreover, it is not clear if treatment given beyond 12 hours after exposure to rhinovirus
would be effective. [15]
9

CUR R E N T TH E R APY CARRIED OUT FOR COMMON C OL D:-
Current therapy for the common cold focuses on symptomatic relief and includes
analgesics, systemic and topical decongestants, and antihistamines. Aspirin and
acetaminophen suppress the development of antibodies and prolong the duration of viral
shedding. [16] These agents reduce fever that may be a protective response to infection.
However, fever is only present in a small minority of patients. Aspirin and
acetaminophen may be useful to reduce headache, malaise, and muscle aches if they are
present. These agents should not be used routinely for the common cold. The association
of aspirin use and Reye's syndrome in children with influenza warrants further caution in
the routine use of aspirin. [16,17] This association has not been described in association
with the common cold. However, influenza can sometimes mimic the common cold and
Reye's syndrome has been reported, although rarely, with adenoviruses and parainfluenza
viruses. Ibuprofen and naproxen have no detrimental effect on serum antibody response
and virus shedding and appear effective for relieving some cold symptoms. [18]
The use of antihistamines to relieve cold symptoms is controversial. Histamine does not
appear to play a significant role in the pathogenesis of the common cold. Some
antihistamines possess anticholinergic action, which may reduce nasal secretions. [19] The
use of a sustained release formulation of brompheniramine was effective for reducing
sneezing, rhinorrhea, and cough after experimentally induced rhinovirus colds. [20] In
patients with natural colds, clemastine provided some symptomatic relief of rhinorrhea
ana sneezing, but the effects appeared less prominent. [21] A review of studies before
1996 concluded that antihistamines do not have major effects on overall cold symptoms,
although some attenuation of sneezing and rhinorrhea may occur. [22] These minor
benefits must be weighed against the potential for side effects, primarily somnolence and
dry mouth and throat. Intranasal ipratropium bromide, an anticholinergic agent, is
efficacious for reducing rhinorrhea and sneezing. [23]
Systemic and topical decongestants have been widely used to relieve nasal congestion.
Topical solutions of oxymetazoline, xylometazoline, and phenylpropanolamine are
10

rapidly effective in relieving congestion and improving nasal airflow. [24] With
xylometazoline, this effect persists for 6 hours. These agents are only indicated for short-
term use «3 days) because rebound congestion can occur with more prolonged use.
Systemic decongestants including pseudoephedrine and phenylpropanolamine also are
effective for symptomatic relief. A recent study showed that oral pseudoephedrine is
more effective than placebo for relieving nasal congestion. [25]
Intranasal and inhalation formulations of sodium cromoglycate (cromolyn sodium), used
every 2 hours for the first 2 days, then four times daily thereafter, provide symptomatic
relief of cold symptoms compared to placebo. The duration of cold symptoms was
significantly shortened and symptoms decreased in final 3 days. [26]
Cough associated with the common cold is usually related to postnasal drainage and
throat irritation and is under voluntary control. Antitussive agents such as codeine are not
effective for this type of cough. [27],40 Codeine may be useful for chronic cough based on
a reflex mechanism that occurs in some patients after resolution of the cold.
Antihistamines and decongestants may be effective in relieving cough associated with
acute upper respiratory infection. [28]
Considerable interest in the effectiveness of echinacea for prevention and treatment of
the common cold has evolved in recent years. A double-blind placebo-controlled study
showed no benefit of using echinacea for preventing the common cold or respiratory
infection. [29] The relative risk of acquiring an URI was 0.88 (95% confidence interval
[CI] of 0.60 to 1.22) with treatment. Once a cold occurred, the median duration of
symptoms was 4.5 days in the echinacea group and 6.5 days in the placebo group (not
significant). It remains possible that a very small effect would be detected in a larger
trial; however, the clinical significance remains questionable. Variations in the source
and chemical makeup of various echinacea products could explain why other sources
claim efficacy with echinacea for the treatment of the common cold. There is no role for
the use of antibacterial drugs in the treatment of the common cold. [30] Antibiotics may be
11

required only to manage complications such as acute otitis media or acute rhinosinusitis. [31]
IRRATIONAL PRESCRIBING PRACTICES IN COMMON COLD
TREATMENT:-
Although a cold is a viral illness, antibiotics often are inappropriately prescribed to
patients, even when bacterial complications (e.g., pneumonia, bacterial sinusitis) are not
present. Studies of antibiotics for the treatment of the common cold focus on cure rate,
symptom persistence, prevention of secondary bacterial complications, and adverse
effects. [32]
Over prescription and abuse of antibiotics in the treatment of acute respiratory infections
and is a worldwide problem, potentially leading to widespread antibiotic resistance. [33]
The use of antimicrobials is especially prevalent in the very young and the elderly. In one
study, 37 and 70 percent of children, by three and six months of age respectively, had
received at least one antibiotic prescription. [34]
Most antibiotic prescriptions in the ambulatory setting are for respiratory infections.
Studies evaluating physicians' prescribing patterns have found that almost 50 percent of
office visits for colds and upper respiratory tract infections (URIs), and 80 percent of
visits for acute bronchitis are treated with antibacterial agents. [35]
The majority of antibiotics prescribed to adults in ambulatory practice in the United
States are for acute sinusitis, acute pharyngitis, acute bronchitis, and nonspecific upper
respiratory tract infections (including the common cold). For each of these conditions
especially colds, nonspecific upper respiratory tract infections, and acute bronchitis (for
which routine antibiotic treatment is not recommended) [36]
12

IRRATIONAL TREATMENT PRACTICES OF COMMON COLD IN
PAKISTAN:-
A knowledge, attitude and practices (K.A.P.) survey was conducted among doctors
working as general practitioners (GP) in Multan, for diagnosis and management of acute
respiratory infections (ARI) in children under five years of age. GPs in Multan were not
familiar with national ARI control Program and rational drug use guidelines. They rarely
asked about symptoms describing severity of disease while taking patient histories and
did not look for signs of severe pneumonia during physical examinations. Most patients
diagnosed as URTI (upper respiratory tract infection) received oral antibiotics and those
with pneumonia received inject able antibiotics. Other drugs prescribed included cough
syrups, antihistamines and antipyretics. The average number of drugs prescribed per
patient was 3.4. The doctors were deficient in providing home care advice for sick
children to the caretakers. Average time spent by doctors on each patient was two
minutes and twenty-three seconds. A combination of biomedical and social factors help
to perpetuate this irrational prescribing behavior of the GPs. Continuing education
programs for doctors in general practice about ARI management in children and rational
use of drugs and health education of the public may improve the current prescribing
practices. The resolution adopted at the SEARC conference on South East Asian children
in October 1986 provided endorsement to the policy of ARI control at the highest official
level. [9]
SITUATION ANALYSIS IN CHILDREN UNDER 5:-
The highest rates of antibiotic prescribing in primary care are to children with respiratory
illness but surprisingly there have been few prospective controlled studies of the impact
of such prescribing on resistance in a community setting [37]In the 1980s Brook reported
isolation of lactam producing bacteria in 46% of children one week after antibiotic
treatment of otitis media or pharyngitis and 27% after three months compared with a
constant 11% in controls.21 A paper from Malawi in 2000 reported recovery of co-
13

trimoxazole resistant pneumococci in 52% of children one week after malaria treatment
with co-trimoxazole compared with 34% in controls but with no difference after four
weeks[38]. An Australian study in 2002 reported a twofold increase in the odds of recovery
of resistant pneumococci in children who had used lactam antibiotics in the two months
before swab collection.[39] We report a prospective study in children from UK general
practice with new methods for identifying a highly mobile integrative and conjugative
element (ICE) that encodes lactamase and circulates among nasopharyngeal
Haemophilus species.[40]
Studies showed that irrational prescribing practices of common cold is one of the most
critical issue that need to be global considerations. In Pakistan a small efforts is put on
this issue. Lot is to be done in this area therefore this study will have focus on to
document current treatment practices of ARI in selected facilities and try to find the
prevalence of ARI and reason of ARI and reason for prescribing antibiotics in ARI and
identify the problems that need to be sorted out. This work will add to existing literature
in will give you bases will be helpful in research.
14

Chapter 2:
Objectives
15

GENERAL OBJECTIVE:-
Assessment of prescribing practice of antibiotics in common cold under the age of
five years in PIMS Islamabad.
SPECIFIC OBJECTIVES;-
To document the current treatment practices of (ARI) in selected
hospital of Islamabad Pakistan
To identify the most common prescribing combination of drug in ARI .
To determine the %age of patients receiving antibiotics in children under 5
To determine the average number of drugs per patient
To determine the %age of patients receiving different dosage forms
To determine the %age of patients receiving drugs other than antibiotics
16

Chapter 3:
Methodology
17

Methodology:
A descriptive cross sectional study was conducted in Pakistan Institute of Medical
Sciences during the period of September to October. Standard Treatment Guideline was
used as a reference point to describe that antibiotics should not be prescribed in children
under the age of 5 years having common cold. These standard treatment guidelines were
developed from Davidson’s Principles and Practice of Medicine 20th Edition by Nicholas
A. Boon, Nicki R. Colledge, Brian R. Walker, John Hunter.
The data was collected by using data collection tools. In order to collect data from
Pakistan Institute of Medical Sciences an application was written to Director Hamdard
Institute of Pharmaceutical Sciences in order to issue a letter to hospital give
permission to carried out study easily in Pakistan Institute of Medical sciences . Then
this letter was submitted to the Hospital Administration .the letter was processed in
the hospital within three weeks .The permission letter was granted by hospital and also
issue a letter to the Children hospital for permission. After this the field visit for data
collection was planned. The data was collected from Out Patient department of Children
Hospital Pakistan Institute of Medical Sciences .We travel by our own car to reach
Hospital for data collection. We collected data between 10 am to 1pm because at this
time the sufficient patients visit to OPD hospital.
In order to collect quantities data, a data collection form was design by consulting
with teacher and WHO manual How to Investigate Drug use in Health Facility,
after designing the form was pilot tested to check its utility, after the success full
pilot testing the form was used for data collection. Then the permission letter was
shown to the chief pharmacist in Pakistan institute of medical sciences for
issuance of permission for the prescription observation on children OPD. After
collecting the required data, we thank a lot to dispenser for his cooperation. At the
end of the day, we move by car towards home and entered the collected data in
data collection form. . After the completion of data in data collection form, the data
18

was entered in Statistical Package for Social Sciences(SPSS 17) by creating
variables. Then the data was analyzed by applying different statistical test .and
then results were presented in graphical and tabular form.
Chapter 4:
Results
19

Results:
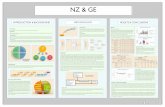
Out of the 100 prescriptions from Pakistan Institute of Medical Sciences to check
among the most commonly prescribe combination of drugs in ARI under 5. the
prescribed drug was antipyretic, antihistamine and antibiotic. From antipyretic
paracitamol, from antihistamine chlorpheneramine and from antibiotic Amoxil. The
percentages of these combinations were shown in Fig-1.
D r u g c o m b in a t io n u s e d
5 3
5 7
3 0
5
0
1 0
2 0
3 0
4 0
5 0
6 0
1
%ag
e
A n t io b io t i c + A n t ip y re t i c + A n t ih i s t a m in e
A n t io b io t i c + A n t ih i s ta m in e
A n t ib io t i c + A n t ip y r e ti c
A n t ih i s t a m in e + A n t ip y r e t i c
A n t io b io t i c + A n t ip y re t i c + A n t ih i s t a m in e +M u l t iv i t a m in
Fig-1
20

The presence of antibiotic in overall prescription was shown in Fig-2.
Fig-2
The no. of drugs per patient was shown in Fig-3.
21

Fig-3The class of antibiotic prescribed was shown in Fig-4.
Fig-4
The age of patient was shown in Fig-5.
22

Fig-5The number of antibiotic per prescribtion was shown in Fig-6.
Fig-6
23

24

25