Female Genital Tract Malignancies
-
Upload
youan-bi-beniet-marius -
Category
Health & Medicine
-
view
3.114 -
download
3
description
Transcript of Female Genital Tract Malignancies

Marius Beniet YouanBi, Pharm D,
Master of Clinical Pharmacy
University of Nairobi.
Female Genital tract malignancies

OUTLINES
1. VULVAR CANCER
3. CERVICAL CANCER
2. VAGINAL CANCER
4. WOMB CANCER
6. OVARIAN CANCER
5. FALLOPIAN CANCER

Human Female genital system

1. VULVAR CANCER


The vulva is
the external
genitalia of
the female
reproductive
tract
Vulva


Vulvar cancer
Vulvar cancer is a
cancer that
starts in the
external female
sex organs –
inner edges of
the labia majora
or labia minora

Vulvar cancer epidemiology
• 4th most common gynecologic cancer
(following uterus, ovary and cervix)
• Comprises 5% of gynecologic
malignancies
• Mean age at diagnosis is 65y, but is
decreasing


• Cigarette smoking
• Human Papilloma Virus (HPV)
infection
• Immunosuppression
• Chronic vulvar conditions such as
lichen sclerosus
• VIN/CIN
• Prior history of cervical cancer
Causes & Risk Factor

Pathogenesis
1. HPV infection (60%)
Two pathways of vulvar carcinogenesis:
2. Chronic inflammatory (vulvar
dystrophy) or autoimmune
processes

THE CLINICAL
MANIFESTATIONS
OF VULVAR
CANCER

Clinical Manifestations
• Most patients present with a single vulvar
plaque, ulcer or mass
• Labia major is the most common site
• Lesions are multifocal in 5% of cases A
synchronous second malignancy is found
in 22% of cases, usually CIN/cervical cancer

Clinical Manifestations

Clinical Manifestations

Clinical Manifestations

Clinical Manifestations

Clinical Manifestations
• Pruritus is the most common presenting
symptom (especially if associated with
vulvar dystrophy such as lichen
sclerosus)
• Vulvar bleeding or discharge
• Dysuria
• Enlarged groin lymph node


Diagnosis
• Biopsy of gross lesions
• If no gross lesion present but high
clinical suspicion, perform colposcopy

Types of Vulvar Cancer
• Squamous cell carcinoma SCCA (>90% of cases)
• Melanoma
• Sarcoma
• Basal cell carcinoma
• Verrucous carcinoma
• Adenocarcinoma (Bartholin gland)

Vulvar Cancer Staging (Surgical)Stage Description
IA Lesion <2 cm with <1 mm stromal invasion, no nodal
metastases
IB Lesion >2 cm with >1 mm stromal invasion, no nodal
metastases
II Lesion any size, extension to adjacent structures, no
nodal metastases
III Lesion of any size with involvement of the lower urethra,
vagina or anus OR groin lymph node metastases
IVA Tumor invading upper urethra, bladder mucosa, rectal
mucosa, pelvic bone
IVB Any distant metastases, including pelvic lymph nodes

Treatment of SCCA VulvarStage Treatment
IA Wide local excision (WLE)
IB WRE and inguinal-femoral lymphadenectomy
II WRE and inguinal-femoral lymphadenectomy
III WRE and inguinal-femoral lymphadenectomy
OR chemoradiation +/- surgery to resect
residual disease as needed
IVA chemoradiation +/- surgery to resect residual
disease as needed
IVB Chemotherapy

Treatment of SCCA Vulvar : Surgery
Wide Radical Excision (WRE):
• Excision of vulvar lesion down to the
fascia of the urogenital diaphragm
• 2 cm tumor-free margin
Inguinal-Femoral Lymphadenectomy:
• Removal of the superficial inguinal
and deep femoral lymph nodes

• Radiation in combination with chemotherapy
is an alternative to surgery in women with
stage III/IVA disease
• Indicated if positive inguinal/pelvic nodes
• Indicated if positive margins after WRE if
re-excision not possible or desirable (i.e.
around the clitoris or anal sphincter)
Treatment of SCCA Vulvar : Radiation therapy

Treatment of SCCA Vulvar : Chemotherapy
• Indicated for metastatic disease (stage
IVB)
• Platinum-based
• Treatment is palliative

Chemotherapy regimens SCCA Vulvar
First-Line Combination Therapy
REGIMEN DOSING
Paclitaxel (Taxol) + cisplatin
(Platinol; CDDP)
Day 1: Paclitaxel 135mg/m2 IV, admi over
24 hr plus
Day 2: Cisplatin 50mg/m2 IV at a rate of
1mg/min.
Repeat cycle every 3 weeks for 6
cycles.
Carboplatin (Paraplatin) +
paclitaxel
Day 1: Carboplatin AUC=5mg/mL/min
administered over 1 hr, followed
by paclitaxel 175mg/m2 administered
over 3 hrs.
Repeat cycle every 3 weeks for 6–9
cycles or until disease progression or
unacceptable toxicity

Chemotherapy regimens SCCA Vulvar
First-Line Combination Therapy cont’d
REGIMEN DOSING
Cisplatin + topotecan
(Hycamtin)
Days 1–3: Topotecan 0.75mg/m2 IV
administered over 30 min plus
Day 1: Cisplatin 50mg/m2 IV.
Repeat cycle every 3 weeks.
Cisplatin + gemcitabine
(Gemzar)
Days 1 and 8: Cisplatin
30mg/m2 + gemcitabine 800mg/m2.
Repeat cycle every 4 weeks.

Chemotherapy regimens SCCA Vulvar
First-Line Monotherapy
REGIMEN DOSING
Cisplatin (preferred as a
single agent)
Day 1: Cisplatin 50mg/m2.
Repeat cycle every 3 weeks
for a total of 6 cycles.

Chemotherapy regimens SCCA Vulvar
Second-Line Therapy
REGIMEN DOSING
Bevacizumab (Avastin)
Day 1: Bevacizumab 15mg/kg
IV.
Repeat cycle every 3 weeks.
Docetaxel (Taxotere)Day 1: Docetaxel 100mg/m2 IV,
administered over 1 hr.
Repeat cycle every 3 weeks

OTHERS TYPES OF
VULVAR CANCER

Melanoma of the Vulva
• 2nd most common type of vulvar cancer (5-6%)
• Occurs more frequently in white women
• Mean age at diagnosis is 68y
• Treatment is wide local excision with 2
cm margins and sentinel lymph node
biopsy

Melanoma of the Vulva

Basal Cell Carcinoma
• 2% of vulvar cancers
• Usually occur in white, postmenopausal women
• May be locally invasive but usually do not metastasize
• Slow-growing
• Treatment is wide local excision

Basal Cell Carcinoma

Paget Disease of the Vulva
• <1% of vulvar malignancies
• Most common presenting symptom is pruritus
• Lesion is usually well demarcated slightly raised edges and a red background
• Most patients are postmenopausal and Caucasian
• Treatment is wide local excision

Paget Disease of the Vulva

Summary – Vulvar Cancer
• Comprises 5% of gynecologic malignancies
• 2 pathways of vulvar carcinogenesis:
– HPV infection (60%)
– Chronic inflammatory (vulvar dystrophy)
• Most common histology is squamous cell carcinoma
• Treatment includes surgery, radiation and/or chemotherapy depending on stage

2. VAGINAL CANCER

Vagina
the muscular
passage that
leads from the
cervix to the
vulva


Vaginal cancer
• Vaginal cancer,
sometimes referred
to as primary
vaginal cancer.
• Cancer that starts in
the vagina.

Vaginal cancer
There are two main kinds of vaginal cancer:
primary
vaginal cancer
secondary
vaginal cancer
the cancer originates in the vagina
cancer spreads to
the vagina from
another organ
Represents 2-3% of Pelvic Cancers

Primary vaginal cancer
• Squamous cell
carcinoma::80-85% , 50 yrs. and up
.
• Clear cell
adenocarcinoma
:10%, teenagers and young women[14 – 20 yrs. ]
• Melanoma :2-3%, women over 50

Secondary vaginal cancer
84% of cancers in vaginal area are secondary
• Cervical
• Uterine
• Colorectal
• Ovary


Causes & Risk Factor
• Cigarette smoking
• Human Papilloma Virus (HPV 16 and 18) infection
• Immunosuppression
• VIN/CIN
• Prior history of cervical cancer
• Treatment for womb cancer by radiotherapy


Clinical Manifestations
• Painless vaginal bleeding, between periods,
after menopause, or after sex
Symptoms appear , often in later stages.
They can include:
• Vaginal discharge (may smell or be bloody)pain
during sex
• A lump in the vagina that you can feel
• A persistent itch in the vagina

Clinical Manifestations
Advanced vaginal cancer can also cause:
• constipation
• pain when peeing
• swelling in the legs (oedema)
• persistent pelvic pain


Diagnosis
• Biopsy to look for either precancerous
(VAIN) or cancerous cells
• Scans and x-rays to see if the cancer
has spread to other parts of your body.

Vagina cancer Staging
• Stage I : Confined to Vaginal Wall
• Stage II : Subvaginal tissue but not
to pelvic sidewall
• Stage III : Extended to pelvic sidewall
• Stage IVA: Bowel or Bladder
• Stage IVB: Distant metastasis

Treatment of vaginal cancer
• Surgery with Radical Hysterectomy and
pelvic lymph dissection in selected
stage I tumors high in Vagina
• All others treated with radiation with
chemosensitization

Treatment of vaginal cancer cont’d
radiotherapy concurrently with
weekly intravenous Cis-platinum
chemotherapy (40 mg/m2)
• Radiation with chemosensitization

5 year Survival
• Stage I 70%
• Stage II 51%
• Stage III 33%
• Stage IV 17%


Prevention
The few things known to help, though,
are avoiding smoking, and getting
regular smear tests to detect
precancerous or cancerous cells early:
VAIN VIN ; HPV CIN

Pap smear test

Summary – Vagina Cancer
• Represents 2-3% of Pelvic Cancers
• 84% of cancers in vaginal area are secondary
• Clear cell adenocarcinoma most occurs
teenagers and young women
• Treatment includes most surgery, radiation
• Chemosensitization with cisplatin

3. CERVICAL CANCER

Cervix


Cervical cancer
Cervical cancer
begins in the cervix
(the neck of the
womb), which is a
strong muscle that
forms the passage
between the womb
and the vagina.

Cervical cancer epidemiology
• Approximately 570,000 cases
expected worldwide each year
• 275,000 deaths
• Number one cancer killer of women
worldwide
• With the advent of the Pap smear, the
incidence of cervical cancer has declined


Cervical Cancer Etiology
• Cervical cancer is a sexually transmitted disease.
• HPV is the primary cause of cervical cancer.
• Some strains of HPV have a predilection to
the genital tract and transmission is usually
through sexual contact (16, 18 High Risk).

Cervical Cancer Risk Factors
• smoking
• giving birth to more than 7 children
having your first child before 17yrs
• Number of sexual partners
• Early age of intercourse

Cervical Cancer Risk Factors
• High-risk male partner
• Taking the pill
• Having a weakened immune system

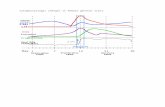
Pathogenesis


Clinical Manifestations
• May be silent until advanced disease develops
• Symptoms of Invasion :
Post-coital bleeding
Foul vaginal discharge
Abnormal bleeding

Clinical Manifestations cont’d
Unilateral leg swelling or pain
Pelvic mass
Pelvic pain
Gross cervical lesion

the stages of cancer progression
The pre-cancerous
stage before the
cells turn cancerous
is called Cervical
Intra-epithelial
Neoplasia commonly
in short called CIN

Clinical Manifestations cont’d


Diagnosis
• A cone or hysterectomy specimen
• MRI, a CT or PET-CT scan, blood
tests or a chest X-ray
• Colposcopy,
• Biopsy

Cold cone biopsy

Colposcopy Medical Test
a procedure that
allows doctor to
look at the
surface of your
cervix and biopsy
any abnormal
areas

Staging of cervical cancer

Treatment of Early Disease
• Conization or simple hysterectomy -
microinvasive cancer
• Radical hysterectomy - removal of the uterus
with its associated connective tissues, the
upper vagina, and pelvic lymph nodes..
• Chemoradiation therapy

Radical hysterectomy - removal of the
uterus

Advanced Staging
• Chemoradiation is the mainstay of treatment
• 4-5 weeks of external radiation treats the primary
tumor and adjacent tissues and lymph nodes
• Chemotherapy acts as a radiation sensitizer
and may also control distant disease

Locally advanced cervical cancer regimens
First-Line Therapy with Radiotherapy
REGIMEN DOSING
Cisplatin
40mg/m2 IV on days 1, 8, 15, 22, 29, and
36 (total dose not to exceed 70mg per
week).
Cisplatin + 5-FU
Days 1 and 29: 4 hrs prior to external-
beam radiotherapy: Cisplatin
50mgDinfusion /m2 IV at 1mg/min with
standard hydration, plus
Days 2–5, and 30–33: 5-FU
1000mg/m2 IV continuous infusion over
24 hrs (total dose 4000mg/m2 each
course).

Locally advanced cervical cancer
regimens cont’d
First-Line Therapy with Radiotherapy
REGIMEN DOSING
Cisplatin + 5-FU
Days 1–5 of radiotherapy: Cisplatin
75mg/m2 IV over 4 hrs followed by 5-FU
4000mg/m2 IV over 96 hrs.
Repeat cycle every 3 weeks for 2
additional cycles.
Cisplatin + 5-
FU +hydroxyurea
Days 1 and 29: Cisplatin
50mg/m2 IV followed by 4000mg/m2 5-
FU over 96 hrs; hydroxyurea 2g orally
twice weekly for 6 weeks.

Locally advanced cervical cancer
regimens cont’d
First-Line Therapy with Radiotherapy
REGIMEN DOSING
Cisplatin + gemcitabine +
radiotherapy +brachytherapy
Induction therapy
Days 1, 8, 15, 22, 29 and 36: Cisplatin
40mg/m2 + gemcitabine
125mg/m2 + concurrent external-
beam radiotherapy 50.4Gy in 28
fractions, followed by brachytherapy
30–35Gy in 96 hrs.
Adjuvant therapy
Day 1: Cisplatin 50mg/m2, plus
Days 1 and 8: Gemcitabine
1,000mg/m2.
Repeat every 3 weeks for 2 cycles.

Metastatic or Recurrent
Cervical Cancer Regimens
Similar regimens as those used for
metastatic vulvar cancer


Reduce the risk
• reduce the risk of contracting the virus, which
in turn can reduce the risk of getting cervical
cancer
• start having sex when mature , and less sexual
partners because more you have higher your
chances are of developing cervical cancer

Summary – Vagina Cancer
• Number one cancer killer of women worldwide
• HPV is the primary cause of cervical
cancer
• Number of sexual partners
• Treatment includes surgery, and chemotherapy asso radiotherapy
• Prevent by a frequent Pap smear test

4. UTERINE CANCER

wall of Uterus


Womb cancer
• Also known
as, cancer of the
uterus, uterine cancer
or endometrial
cancer(++)
• begins in the lining
or walls of the
uterus.

Epidemiology
• Most common gynecologic malignancy
• Eighth leading cause of female mortality from cancer
• 97% arise from the endometrium (endometrial carcinoma)
• 3% arise from the mesenchymal components (sarcoma)

Types of womb cancer
• Uterine :
sarcoma
There are two main types of womb cancer:
95% of womb cancers
“starts in the womb’s lining, or endometrium
often caught early, and treated
successfully.
both less common and harder to treat.
starts in the muscle wall of the womb
• Endometrial:
cancer

Sub-types
• Leiomyosarcoma : Cancer of the muscle wall - the most
common sarcoma of the womb
• Papillary serous :
carcinomaAround 5% of womb cancers
• Clear cell carcinoma: Extremely rare, 1 to 2% of
womb cancers
• Adenocanthomas: combine both glandular and
cervical types of malignant cells

Two main types of womb cancer
Endometrial
carcinoma Uterine
sarcoma

THE FIRST TYPE OF
WOMB CANCER:
ENDOMETRIAL
CARCINOMA (95%)

Endometrial carcinoma

Epidemiology
• Median age of diagnosis: 60 years
• Most common in women > age 50 years
• Incidence is highly dependent on age
• 75% of uterine cancers occur in post-
menopausal women

Endometrial carcinoma Risk factors
RISK
FACTORS
OESTROGEN
OTHERS
OBESITY
DIABETES
HYPERTENSION
HNPCC

Estrogen exposure
EXOGENOUS
HORMONE
REPLACEMENT
THERAPY
TAMOXIFEN FOR
BREAST CANCER
ENDOGENOUSEARLY
MENARCHE
LATE
MENOPAUSE
PCOS
OBESITY
FUNCTIONING
OVARIAN TUMORS

• NULLIPAROUS WOMEN & WOMEN
WITH PCOD
NON OVULATION
HIGH OESTROGEN
ENDOMETRIAL HYPERPLASIA
NULLIPAROUS WOMEN
ENDOMETRIAL CANCER

• Obesity reduces level of serum
hormone binding protein
free estrogen circulates in body
OBESITY
• Peripheral fat : conversion of
epiandrostenedione to
oestrone

RISK FACTORS
NULLIPARITY
PCOS
EARLY MENARCHE
LATE MENOPAUSE
OBESITY
DIABETES
HYPERTENSION
LYNCH 2 / HNPCC
TAMOXIFEN
HRT

Clinical manifestations
• Bleeding
– Present in 90% of all cases
– 15% of patients with postmenopausal
bleeding will have endometrial cancer

Clinical manifestations
• Other Signs/Symptoms
– Vaginal Discharge(80-90%)
– Pelvic Pain, Pressure
– Referred Leg Pain
– Change in Bowel Habits
– Pyometria/Hematometria

Diagnosis
• Pap Smear
– Only 30-50% patients with cancer will have
an abnormal result
• Endometrial Biopsy
– False negative rate of 5-10%

Diagnosis
• Transvaginal Ultrasound
– Not for routine screening or diagnosis
• Fractional Dilation and Curettage
– Use in cases of cervical stenosis,
patient intolerance to exam, recurrent
bleeding after negative biopsy

Endometrial Cancer Grade
• The grade is based on the percentage of the
solid component.
– Well Differentiated (Grade 1): <5%
– Moderately Differentiated (Grade 2): 5-50%
– Poorly Differentiated (Grade 3): > 50%

Endometrial carcinoma type
• There are two major pathogenic types of
endometrial carcinoma :
Type II
Type I

Type I Endometrial Carcinoma
• Well differentiated endometrioid
• Better prognosis
• Superficial myometrial invasion
• Infrequent lymph node metastases
• Associated with hyperplasia
• Younger/peri-menopausal women

Type II Endometrial Carcinoma
• Older/post-menopausal women
• Thin
• Poorly differentiated carcinoma
– Papillary Serous
– Clear Cell
• Deep myometrial invasion
• Frequent lymph node metastases
• Associated with atrophy

Endometrial Carcinoma Treatment
• Surgery is the mainstay of treatment
followed by adjuvant radiation and/or
chemotherapy based on stage of disease.
• Primary radiotherapy or hormonal therapy
may be employed in patients who have
contraindications to surgery.

Hormone Therapy
• Appropriate in patients that desire fertility
preservation
• ONLY-G1 tumors!!
• High dose progestins
– Young patient
– Well differentiated
cancer

Endometrial Cancer hormonal regimens
Hormonal Regimens (for Endometrioid Only)
Tamoxifen (Nolvadex) Tamoxifen 20mg orally twice daily.
Medroxyprogesterone
acetate(MPA)Medroxyprogesterone acetate 200mg
orally once daily.
Tamoxifen +medroxyprog
esterone acetate
Medroxyprogesterone acetate 80mg
orally twice daily for 3 weeks
alternating with tamoxifen 20mg orally
twice daily.
Repeat cycle every 3 weeks.
Combination is associated with grade 4
thromboembolic events in a few
patients.1

Endometrial Cancer chemotherapy regimensChemotherapy Regimens and other Treatment Regimens
REGIMEN DOSING
Cisplatin (Platinol;
CDDP) +doxorubicin (Adria
mycin) (for adjuvant use)
Day 1: Doxorubicin
45mg/m2 IV + cisplatin
50mg/m2 IV, followed by
Days 2–11: Optional filgrastim
5mcg/kg/day.
Repeat cycle every 3 weeks; maximum 6
cycles.
Cisplatin + doxorubicin +p
aclitaxel (Taxol)
Day 1: Doxorubicin
45mg/m2 IV + cisplatin
50mg/m2 IV followed by
Day 2: Paclitaxel 160mg/m2 3-hr IV
infusion, followed by
Days 3–12: Filgrastim 5mcg/kg SC.
Repeat cycle every 3 weeks for max 7
cycles.
Maximum BSA of 2.0 was used for
calculations.

THE SECOND TYPE OF
WOMB CANCER:
UTERINE SARCOMA( 3%)

Uterine Sarcoma
• 3% of all uterine cancers
• 15% of all deaths from uterine
cancer
• Types Carcinosarcoma
Leiomyosarcoma
Endometrial Stromal Tumors

Carcinosarcoma
• Post-menopausal- median age of 62 years
• Associated with diabetes, hypertension, and obesity
• 7-37% of patients have prior pelvic irradiation
• Poor prognosis

Leiomyosarcoma
• Median age 52 years
• Premenopausal have a better prognosis
• Leiomyosarcoma:
1. Mitotic count: > 10 mitosis per HPF
2. Cellular atypia
3. Coagulative necrosis

Uterine Sarcoma Treatment: Surgery
3. Bilateral salpingo-ophorectomy
NOT in premenopausal women
1. Stage I/II sarcomas should be treated with
hysterectomy
2. Lymphadenectomy is indicated in all
sarcomas except leiomyosarcoma

Uterine Sarcoma Treatment: Recurrence
• Isolated lesions
-surgical excision
• Recurrent carcinosarcoma
-paclitaxel, platinum or ifosfamide
• Recurrent leiomyosarcoma
-doxorubicin, ifosfamide, docetaxel and
gemcitabine

Uterine Sarcoma Chemotherapy regimens
Chemotherapy
REGIMEN DOSING
Doxorubicin (Adriamycin)
Day 1: 75mg/m2 IV bolus.
Repeat cycle every 31 days OR
60mg/m2–70mg/m2 IV typically dosed every
3 weeks.
Gemcitabine (Gemzar) +do
cetaxel (Taxotere) +granulo
cyte-colony-stimulating
factor (G-CSF)
Days 1 and 8: Gemcitabine 900mg/m2 IV
over 90 min, followed by
Day 8: Docetaxel 100mg/m2 IV over 60
min, followed by
Days 9–15: G-CSF
150mcg/m2 SC OR on Day 9 or
10: Pegfilgrastim 6mg SC.
Repeat cycle every 3 weeks until disease
progression or toxicity occurs.
Gemcitabine
Days 1, 8 and 15: Gemcitabine
1,000mg/m2 IV.
Repeat cycle every 4 weeks.

5. FALLOPIAN TUBES CANCER

The Fallopian tubes
The Fallopian tubes, also
known as oviducts, uterine
tubes, and salpinges are
two very fine tubes leading
from the ovaries into
the uterus, via the utero-
tubal junction

WHAT IS
FALLOPIAN TUBE
CANCER

Fallopian tube cancer
• Fallopian tube cancer begins in a
woman’s fallopian tubes
• Adenocarcinoma
• sarcoma
• chorisarcoma
• others
• Secondary + + +

Epidemiology
• 5 years survival 56%
0.3% of all gynecology malignancies
3.6 / million women
• One of the most rare malignancy of the female
genital tract
• Mean age of diagnosis 50 yrs.
2/3 menauposal

Risk factors
• Nulliparity
• Chronic salpingistis
• Infertility 70% cases
• inflammatory disease (such as TB)

Pathogenesis
• Similar to endometrial and ovarian cancer
Oncogene :
crb
Tumeurs suppressors genes :
p53

Clinical manifestations of FTC
•A pelvic mass or lump
•Vaginal bleeding, especially after menopause
•Abdominal or pelvic pain or feeling of pressure
•Vaginal discharge, which may be clear, white,
or tinged with blood

Diagnosis of FTC
• Preoperative diagnosis very rare
• Sonography
• Serum ca 125

Staging of FTC
• Stage I : confined to fallopian
• Stage II : confined to pelvis
• Stage III: extra pelvic disease
• Stage IV: distant Metastasis

Treatment of FTC
• For early disease
• As an adjuvant therapy
• Reassessment laparotomy
Surgery
• Platinum based combination
chemotherapy
Chemotherapy

Summary
• Very rare genecology malignancy
• 5 years Survival is 56 %
• Staging and treatment similar to
ovarian cancer


6. OVARIAN CANCER

Ovary
ovary is an ovum-
producing reproductive
organ, in pairs
they are both gonads
and endocrine
glands

WHAT IS
OVARIAN CANCER

Ovarian cancer
Ovarian Cancer
is cancer that
forms in the tissue
of the ovary

Epidemiology
• It causes more deaths than any other
gynecologic cancer.
• 80 percent will survive one year and about
50% will survive five years.
• Ovarian cancer is the second most common
gynecologic cancer after uterine cancer.

Risk factors
• Family history of the disease is one of the most
significant risk factors
• The risk of ovarian cancer increases with age
• Rates are highest where diets tend to be
high in fat. Animal fats (red meats, whole
milk or cheese)

Types of ovarian cancer
• There are many different types, but the most
common are three:
Ovarian Epithelial Carcinoma; begins in
the cells of the surface of the ovaries.(90%)
Malignant Germ Cell Tumor; Cancer
that begins in the egg cells.

Types of ovarian cancer cont’d
Stromal; Cancer that develops on the
connective tissue that holds the ovary
together and produces most of the
female hormones.
• malignant and stromal make up about 10%

Pathogenesis
1. Genetic Mutation: Inherited 5 to 10% of Ovarian
Cancer
2. Genetic Mutation: Environmental
Infertility & infertility drugs
Estrogen & Hormone Replacement Therapy
Obesity in adulthood
Talcum Powder

Pathogenesis cont’d
3. Oncogenes and Tumor-suppressors
The genes most affected in families with
a history of Ovarian Cancer are BRCA1
and BRCA2
The suppressor Gene p53

Clinical manifestations
• Abdominal pressure, swelling, or bloating
• Urinary urgency or burning with no infection
• Pelvic discomfort or pain
• Persistent indigestion, gas, or nausea

Clinical manifestations cont’d
• Changes in bladder and bowel habits
• Persistent lack of energy
• Low back pain
• Changes in menstruation.

Diagnosis
• Physical
Malignancy: irregular, solid consistency, is
fixed, nodular, or bilateral, is associated
with ascites
• Ultrasound
Low positive predictive value for cancer

Diagnosis cont’d
• Tumor markers
Epithelial: CA 125, elevated in 80%
35 U/mL is upper limit of normal
Also elevated in many benign conditions

Stage of ovarian cancer

Ovarian Cancer Treatments
There are many different kinds of treatments
available, depends on certain factors, like:
• the stage and size of the tumors,
• your age,
• general health,
• Desire to have kids

Ovarian Cancer Treatments cont’d
• Surgery -Is the most common. The surgeon
tries to remove as much of the tumor as possible
• Chemotherapy-. Chemo is commonly
used after surgery to kills cancer cells that
weren’t removed

Ovarian Cancer Treatments cont’d
• Radiation Therapy- The main goal is to
reduce pain symptoms
Biotherapy/Immunotherapy- Boosts the
body’s immune system to fight the disease.

Ovarian cancer chemotherapy regimensIntravenous First-Line Primary Chemotherapy/Primary Adjuvant
Therapy (Stage II–IV)
REGIMEN DOSING
Paclitaxel (Taxol) + carboplatin(Pa
raplatin)
Day 1: Paclitaxel 175mg/m2 IV
administered over 3 hrs + carboplatin
AUC=5–7.5mg/mL/min IV administered
over 1 hr.
Repeat every 3 weeks for 6 cycles.
Docetaxel (Taxotere) +carboplatin
Day 1: Docetaxel 60–75mg/m2 IV followed
by
carboplatin AUC=5–6mg/mL/min IV.
Repeat every 3 weeks for 6 cycles.
Dose-dense
paclitaxel +carboplatin
Day 1: Carboplatin AUC=6mg/mL/min IV
administered over 1 hr, plus
Days 1, 8, and 15: Paclitaxel 80mg/m2 IV
administered over 1 hr.
Repeat every 3 weeks for 6 cycles.

Ovarian cancer chemotherapy regimens
Intraperitoneal First-Line Therapy for
Advanced Disease
REGIMEN DOSING
Paclitaxel + cisplatin (Platinol;
CDDP)
Day 1: Paclitaxel 135mg/m2 continuous
IV infusion over 24 hrs,followed by
Day 2: Cisplatin 75–
100mg/m2 IP, followed by
Day 8: Paclitaxel 60mg/m2 IP
(maximum body surface area 2m2).
Repeat every 3 weeks for 6 cycles.

General Conclusion
FGTM occur in each of the know anatomical segment :
vulvar, vagina, cervix, uterus, fallopian and ovary
FGTM is common and cervical cancer is responsible
for more deaths following by ovarian cancer then
womb cancer
Option exist now for prevention, detection and treatment ,
Abnormal bleeding and discharge is the most
common clinical manifestation
Surgery and chemotherapy are the main treatment
option , hence the need for us to master the adverse
effects of cytotoxic drugs