Fatty Liver Pesentation
-
Upload
mohamed-naguib -
Category
Documents
-
view
238 -
download
0
Transcript of Fatty Liver Pesentation
-
8/3/2019 Fatty Liver Pesentation
1/31
Nonalcoholic fatty liver disease
(NAFLD)Challenge to Diagnosis
Dr.Mona Hegazy,MD.
Assistant Prof. of Internal Medicine
Cairo University
-
8/3/2019 Fatty Liver Pesentation
2/31
Non-alcoholic fatty liver disease (NAFLD) isnow recognized as one of the most commonliver disorders in the USA, with a prevalenceof 10-24%. A similar trend is also found in
Europe and Japan.Defined as a fataccumulation in the liver (triglyceride thataccumulates in tiny sacs within thehepatocytes ) exceeding 5-10% by weight in
the absence of alcohol abuse, contributingmedications and viral hepatitis
-
8/3/2019 Fatty Liver Pesentation
3/31
Nonalcoholic fatty liver disease (NAFLD)
refers to a wide spectrum of liverdiseases,ranging from simple fatty liver
(steatosis), to nonalcoholic steatohepatitis
(NASH), to cirrhosis. All of the stages of NAFLD have in common
the accumulation of fat (fatty infiltration) in
the hepatocytes. In NASH, the fat
accumulation is associated with varying
degrees of inflammation (hepatitis) and
scarring (fibrosis) of the liver.
-
8/3/2019 Fatty Liver Pesentation
4/31
How long have we knownabout NAFLD and NASH?
Hepatologists actually recognized what is now called NASH in the
1970's, but it was described under different names. In 1980, Dr. J.
Ludwig from the Mayo Clinic made an astute observation. He noted
that certain individuals who share common features (obesity,
diabetes, and elevated cholesterol) had a liver disease that closely
resembled alcoholic liver disease (ALD). So, Dr. Ludwig was the
first to coin the term nonalcoholic steatohepatitis (NASH).
For many years, however, NASH was thought by most doctors to bea totally harmless condition. Or, it was considered an innocent
bystander that was associated with other liver diseases (especially
viral hepatitis). In fact, during those years, simple fatty liver
(steatosis) and NASH were considered to be equivalent processes
-
8/3/2019 Fatty Liver Pesentation
5/31
A direct correlation between the severity of fatty liver
and BMI was clearly demonstrated for both genders.
It was found that, a male subject with a BMI
characterized as overweight (25-29.9 kg/m2) had a69.8 times greater chance of developing severe fatty
liver than a male with a normal BMI, and the odds
soared to 805.6 times when the BMI was obese (>30
kg/m2).
J Gastroenterol Hepatol. 2007
-
8/3/2019 Fatty Liver Pesentation
6/31
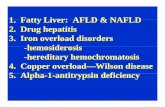
Are there other causes of fat accumulation in the liver?
Indeed, there are many other causes of fat accumulation in the liver besides
NAFLD. However, NAFLD and NASH are considered theprimary fatty liverdiseases. The secondary fatty liver diseases include those that occur in other
types of liver disease.
1. Macro vesicular
Obesity
Type 2 DM
Intestinal bypass
Prolonged parenteral nutrition
Viral infectionHyperlipidaemias
Galactosaemia
Corticosteroids
High dose estrogens
Amiodrone
2.Micro vesicular
Acute fatty liver of pregnancy
Genetic defect of mitochondrial fatty
acid oxidation
Tetracycline
Salicylate
Cholesterol ester storage disease
-
8/3/2019 Fatty Liver Pesentation
7/31
The prevalence of simple fatty liver in obese persons can be estimated to
be approximately 90% and that of NASH in obese persons to be 20%
Hepatology 2005
Projecting the prevalence of NAFLD and NASH in the obese
subpopulation to the entire population would suggest that upwards of 29
million Americans have NAFLD and 6.4 million of these persons have
NASH
Among obese patients, the prevalence of type 1 NAFLD (simple steatosis)
is about 60%. True NASH is found in 20-25%, and 2-3% has cirrhosis.
Hepatology 2003.
During a follow up period of 1-7 years, the progression to cirrhosis
occurred in approximately 8-17% of patients with NAFLD.
Hepatology 2005.
-
8/3/2019 Fatty Liver Pesentation
8/31
Theoretically fat in the liver cells could accumulate
through at least 4 mechanisms:
Increase delivery of dietary fat or fatty acids to the liver.
Increase mitochondrial synthesis of fatty acids or reduced
oxidation.(hyperinsulinemia in insulin resistance promote
lipogenesis and increase triglycerides uptake by the liver)
Impaired export of triglyceride out of the liver cell.
Excess carbohydrate delivered to the liver may be converted to fatty
acids.
In fact, it has been shown that as the BMI increases, so does theamount of fat in the liver.
Oxidative stress and endotoxin cytokine-mediatedinjury follow this fat accumulation, leading to hepatic
fibrosis.
-
8/3/2019 Fatty Liver Pesentation
9/31
Importance of early diagnosis
The risk of developing cirrhosis in a patient with NASH is still
uncertain and varies perhaps from 8% to 17%. Up to now, very few
studies have followed patients over sufficient periods of time to
actually document the progression of NASH to cirrhosis
Furthermore, more and more reports indicate that at least 50% of
cases ofcryptogenic cirrhosis occur in the setting of previous long-
standing obesity and/or DM2. These observations suggest thatinsulin-resistance, hence NASH, was often the basis of what was
called cryptogenic cirrhosis.
-
8/3/2019 Fatty Liver Pesentation
10/31
In fact, the number of liver transplantations for presumed
NASH-related cirrhosis is on the rise. The high rate of
recurrent NASH developing in the new livers of patientsreceiving liver transplants for cryptogenic cirrhosis further
confirms the causal role of NASH.
Finally, a study from France 2009 suggests that patients with
NASH have a similar risk of developing cirrhosis as do
patients with HCV.
However, the progression to cirrhosis in NASH is thought to be
slow and the cirrhosis diagnosis is typically made in patients in
their sixties
-
8/3/2019 Fatty Liver Pesentation
11/31
Severity of NAFLD can be measured by several
methods:
Liver biopsy represents the best diagnostic test for staging liver steatosis,inflammation and fibrosis (Medical and ethical considerations limit its usein subject with non-progressive fatty liver condition).
Liver enzymes (ALT, AST, and -GT).
Liver ultrasonography, although not sufficiently sensitive to detect liverinflammation and fibrosis, demonstrates a good correlation withhistological findings of fatty infiltration. The international guidelines havebeen proposed for the diagnosis of different degree of steatosis with a
sensitivity of 83% and specificity of 100% *
Clin Radiol 2001& J Hepatol 2007
Magnetic resonance imaging (MRI) is the overall best imaging exam forfatty liver, but remains the most expensive.
-
8/3/2019 Fatty Liver Pesentation
12/31
This is a normal liver.The right lobe is largerthan the left lobe. The falciform ligament isthe rough dividing line between the two lobes
This liver is slightly enlarged and has a paleyellow appearance, seen both on the capsuleand cut surface. This uniform change isconsistent with fatty metamorphosis (fattychange).
-
8/3/2019 Fatty Liver Pesentation
13/31
Liver biopsy represents the best diagnostic test for staging liversteatosis, inflammation and fibrosis (Medical and ethical considerationslimit its use in subject with non-progressive fatty liver condition).
Functionally, the liver can be divided intothree zones, based upon oxygen supply.Zone 1 encircles the portal tracts . Zone 3 islocated around central veins. Zone 2 islocated in between
This is the histologic appearance of hepaticfatty change. The lipid accumulates in thehepatocytes as vacuoles. These vacuoleshave a clear appearance with H&E staining.
-
8/3/2019 Fatty Liver Pesentation
14/31
Liver ultrasound
Liver ultrasonography, although not sufficiently sensitive to detectliver inflammation and fibrosis, demonstrates a good correlationwith histological findings of fatty infiltration. The internationalguidelines have been proposed for the diagnosis of different degreeof steatosis with a sensitivity of 83% and specificity of 100% *
J Clin Radiol 2001& J Hepatol 2006
US has proved to be a sensitive, accurate and convenient diagnostic
tool in detecting steatosis: its sensitivity ranges from 60-94% andits specificity from 84-95%. When the hepatic steatosis reaches33%, the detection sensitivity is nearly 100%. Sonographicrankings have been documented to be compatible with the severityof histological hepatic steatosis
J Gastroenterol Hepatol. 2007
-
8/3/2019 Fatty Liver Pesentation
15/31
-
8/3/2019 Fatty Liver Pesentation
16/31
-
8/3/2019 Fatty Liver Pesentation
17/31
-
8/3/2019 Fatty Liver Pesentation
18/31
Liver enzymes
(ALT, AST, and -GT)
-
8/3/2019 Fatty Liver Pesentation
19/31
Several published series have provided detailed information on
the histological and clinical spectrum of hepatic affection in
patients with NAFLD. The majority of subjects in these studies
were identified by the presence of elevated liver enzymes.Between 1990-1999.
It is, however known that; a low normal alanineaminotransferase (ALT) value does not guarantee freedomfrom underlying steatohepatitis with advanced cirrhosis.
J gastroenterology 2002& Ann Intern Med 2002
-
8/3/2019 Fatty Liver Pesentation
20/31
The fatty changes associated with obesity are
macro vesicular (large droplet fat deposition) withintact mitochondria. And with the fact that; alanineaminotransaminase (ALT) is a cytoslic enzyme,while aspartate aminotransaminase (AST) is a
mitochondrial enzyme.
So simple NAFLD must be always associated withvarying degree of ALT elevation with or without
mild elevation of AST.
-
8/3/2019 Fatty Liver Pesentation
21/31
BUT
The entire histological spectrum of NAFLD canbe seen in individuals with normal ALT values.
The histological spectrum in these individuals isnot significantly different from those withelevated ALT levels.
A low normal ALT value does not guarantee
freedom from underlying steatohepatitis withadvanced fibrosis.
J Hepatology 2003
-
8/3/2019 Fatty Liver Pesentation
22/31
An important question is !!
How does one identify subjects withclinically significant NAFLD in the absence
of symptoms, signs, or abnormal ALTvalues?
It is clearly both unreasonable andimpractical to perform routine liverbiopsies for this purpose.
-
8/3/2019 Fatty Liver Pesentation
23/31
What might be the answer!
-
8/3/2019 Fatty Liver Pesentation
24/31
Lowering of the upper limit of normal ALTactivity to < or= 30 IU/L in men, and < or= 19IU/L in women.
J Hepatology 2005.
Fatty Liver Index or FLI.
The ratio between ALT and AST.
-
8/3/2019 Fatty Liver Pesentation
25/31
The ratio between ALT and AST
A cross-sectional study was performed on 107 obese patients; they weredivided into two groups after assessing the liver by ultrasonography (67
patients with ultrasongraphic liver steatosis).
Application of lower levels of ALT normal values on the results, it was
found that; ALT levels were above normal range in 55 patients (82%)instead of 41 patients (61%) with our reference value of up to 41 IU/L in
both sexes.
ALT and AST was higher than 1 in 63 patients (94%) out of 67 patients
with fatty liver
Results showed that, ALT: AST ratio above one in patients with
ultrasongraphic liver steatosis has a sensitivity of 94% and a specificity of
62.5% in diagnosis of fatty liver associated with obesity, with 86% as
positive predictive value, and 72.5% as negative predictive value.
Egyptian Journal Of Inter Med, 2006.
-
8/3/2019 Fatty Liver Pesentation
26/31
FATTY LIVER INDEXThis score was developed on a representative sample of the general
population of a town of Northern Italy.
FLI could be used to determine who requires a confirmatory ultrasound
and/or counseling to reduce weight or improve other clinical risk factors
for complications.
An algorithm based on BMI, waist circumference, triglycerides and GGThad an accuracy of 84%in detecting FL. They used this algorithm to
develop the "fatty liver index" (FLI), which varies between 0 and 100. A
FLI < 30 rules out and a FLI 60 rules in fatty liver.
Among liver enzymes, only GGT was an independent predictor of FLwhile AST was not associated with FL in any of the models and ALT was
not an independent predictor of FL. We have previously shown that ALT
is not a surrogate marker of NAFLD and the present study extends this
consideration to the entire spectrum of FL disease.
Gastroenterol . J . 2006
-
8/3/2019 Fatty Liver Pesentation
27/31
NAFLD and NASH At A Glance
Accumulation of fat in the liver (fatty liver) is common to all
stages of nonalcoholic fatty liver disease (NAFLD). The initialstage in the spectrum of NAFLD is simple fatty liver (steatosis).
The basic cause of NAFLD is insulin resistance. The most
frequent risk factor for insulin resistance is obesity, especiallyabdominal obesity.
Simple fatty liver is in itself quite harmless, disappears rapidly
with weight loss, and 20-25%of those affected progress to NASH,which is the next stage of NAFLD,
The time-line ,and exact risk factors for progression through the
stages of NAFLD are still unknown.
-
8/3/2019 Fatty Liver Pesentation
28/31
Estimates of the number of cases of NAFLD among the obeseand patients with diabetes mellitus type 2 (DM2) suggest that
90% have simple fatty liver, 20% have NASH, and 10% havecirrhosis. Among those with cirrhosis, primary liver cancer
develops at a rate of approximately 1% to 2% per year.
If weight loss results in a decrease or normalization of theliver enzymes, the diagnosis of NAFLD is practically assured.
Only a liver biopsy, however, can confirm the diagnosis of
NAFLD and NASH and determine the severity of the disease.
Weight loss, if overweight, and correcting elevatedcholesterol, triglycerides, and blood sugar should be beneficial
in NAFLD
-
8/3/2019 Fatty Liver Pesentation
29/31
How can fatty liver syndrome be avoided?
To avoid fatty liver adopt and follow these guidelines:
Follow a low fat and a low-cholesterol diet Exercise regularly to maintain an ideal weight Establish a regimen to insure your body is receiving
the necessary and essential vitamins and minerals Avoid alcohol Review medications to ensure that they aren't toxic to
your liver Have blood sugar, cholesterol and triglyceride levels
regularly checked.
-
8/3/2019 Fatty Liver Pesentation
30/31
-
8/3/2019 Fatty Liver Pesentation
31/31