Evaluation of squint
-
Upload
drsiddharth-gautam -
Category
Health & Medicine
-
view
1.794 -
download
0
Transcript of Evaluation of squint
Evaluation of squint
EXAMINATIONof A CASE OF squintPRESENTER-DR. SIDDHARTH GAUTAM
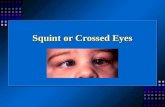
Squint is misalignment of the visual axes.It is a failure of the co-ordination of binocular alignment. It leads inevitably loss of binocular single vision. Fusion of the two images is replaced either by diplopia or suppression of one image. Strabismus may be caused by orbit, muscle, motor nerve, or brainstem pathology.
Classification
Apparent / Pseudo-strabismusThe visual axes are parallel, but the eyes seem to have a squint.This term is applied to a false appearance of squint in the absence of any deviation and it may occur under different condition.Any abnormality of lids, canthi or orbit may lead to pseudo strabismus
Latent Strabismus / Heterophoria It is a condition in which the tendency of the eyes to deviate is kept latent by fusion. Therefore, when the influence of fusion is removed the visual axis of one eye deviates away.Types1. Esophoria- It is a tendency to converge. 2. Exophoria- It is a tendency to diverge.3. Hyperphoria- It is a tendency to deviate upwards, while hypophoria is a tendency to deviate downwards. 4. Cyclophoria- It is a tendency to rotate around the anteroposterior axis. When the 12 Oclock meridian of cornea rotates nasally, it is called incyclophoria and when it rotates temporally it is called excyclophoria.
Manifest Strabismus / Heterotropia Concomitant squintIt is a type of manifest squint in which the amount of deviation in the squinting eye remains constant (unaltered) in all the directions of gaze; and there is no associated limitation of ocular movements.Types 1. Esotropia- inward turning of the eyes
2. Exotropia- outwards turning of the eyes
3. Hypertropia- upwards turning of eyes4. Hypotropia- downwards turning of eyes
Incomitant squintIt is a type of heterotropia in which the amount of deviation varies in different directions of gaze. 1. Paralytic squint2. A and V pattern heterotropias3. Restrictive squint
EVALUATION History:A careful history is important in the diagnosis Age of onset of deviationIs the deviation constant or intermittent?Is the deviation present for distance, near or both?Is it unilateral or alternating?Is it present only when the patient is inattentive or fatigued?
Is it associated with trauma or physical stress?Old photographsBirth historyIs there a family history of strabismus?.Are there any other medical problems? Headaches, diplopia, vertigo
Ocular examination
Visual acuity adapted for ageFor school children and adults-Snellens test typeLandolts test typeFor 3-5 years-Illiterate E-count testTumbling E-testIsolated hand figure testSheridan- Gardiner HOTV testPictorial vision chartsBroken wheel testBork candy bead test
For 2-3 yearsDot visual acuity testCoin testMiniature toy testFor 1-2 years Marble game testSheridans ball testWorths ivory ball testFor infantsOptokinetic nystagmus testPreferential looking testVisually evoked responseCatford drum testIndirect assessment Blink reflex, Menace reflex
Determination of Refractive ErrorIt is most important, because a refractive error may be responsible for the symptoms of the patient or for the deviation itself. Preferably, refraction should be performed under full cycloplegia, especially in children.
REFRACTION AND FUNDOSCOPY
It should be emphasized that dilated fundoscopy is mandatory in the context of strabismus, to exclude any underlying ocular pathology such as macular scarring, optic disc hypoplasia or retinoblastoma.Strabismus is often secondary to refractive error.Hypermetropia, astigmatism, anisometropia and myopia may all be associated with strabismus.
CYCLOPLEGIA
The commonest refractive error causing strabismus is hypermetropia. Accurate measurements of hypermetropia necessitate effective paralysis of the ciliary muscle (cycloplegia), in order to neutralize the effect of accommodation, which masks the true degree of this refractive error.
1.CYCLOPENTOLATEIt affords cycloplegia in most children. The concentration employed is 0.5% under the age of 6 months and 1 % thereafter. One drop, repeated after 5 minutes, usually results in maximal cycloplegia within 30 minutes, with recovery of accommodation within 2-3 hours and of mydriasis within 24 hours.The adequacy of cycloplegia can be determined by comparing retinoscopy readings with the patient fixating for distance and then for near.If cycloplegia is adequate, there will be little or no difference. If cycloplegia is incomplete there will be a difference between the two readings and it may be necessary to wait another 15 minutes or to instil another drop.
2. ATROPINEIt may be necessary in some children with either high hypermetropia or heavily pigmented irides, in which cyclopentolate may be inadequate.Atropine may be used as drops or ointment. Drops are easier for an untrained person to instil, but there is less risk of overdose with ointment. The concentration is 0.5% under the age of 12 months and 1% thereafter.Maximal cycloplegia occurs at 3 hours: recovery of accommodation starts after about 3 days and is usually complete by 10 days.Atropine is instilled (by the parents) b.d. for 3 days before retinoscopy, but not on the day of examination. The parents should be warned to discontinue medication if there are signs of systemic toxicity, such as flushing, fever or restlessness and seek immediate medical attention.
CHANGE OF REFRACTIONBecause refraction changes with age, it is important to check atleast every year and more frequently in smaller children and if acuity is reduced.At birth most babies are hypermetropic.After the age of 2 years there may be an increase in hypermetropia and decrease in astigmatism.Hypermetropia may continue to increase until the age of about 6 years and then between the ages of 6 and 8 year levels off subsequently decreasing until the early teenage years.
WHEN TO PRESCRIBE
1. HYPERMETROPIAIn general up to 4D of hypermetropia should not be corrected in a child without a squint unless they are having problems with near vision.With degrees of hypermetropia greater than this a two-thirds correction is usually given.However,in the presence of esotropia the full cycloplegic correction should be prescribed, even under the age of 2 years.
WHEN TO PRESCRIBE2. ASTIGMATISMA cylinder of 1.50D or more should be prescribed, especially in cases of anisometropia after the age of 18 months.
WHEN TO PRESCRIBE3. MYOPIAThe necessity for correction depends on the age of the child. Under the age of 2 years,-5.00D or more of myopia should be corrected: between the ages of 2 and 4 the amount is -3.00D.Older children should have correction of even milder degrees of myopia to allow clear distance vision.
WHEN TO PRESCRIBE4. ANISOMETROPIAAfter the age of 3 the full difference in refraction between the eyes should be prescribed if it is more than 1D.If there is no squint then any associated hypermetropic correction may be equally reduced for each eye.
Examination of anterior and posterior segmentExamination of associated lid problems, ptosis or media opacities in anterior segment are of direct importance. Examination of pupillary reflexes may reveal the underlying optic nerve or retinal pathologies which are responsible for poor vision. Examination of fundus has assumed more importance, recently, in light of objectively observing torsion of the eyes.
Measurement of deviation1. Hirschberg testIt gives rough objective estimate of the angle of a manifest squintUseful in young or uncooperative patients or when fixation in deviating eye is poor.Procedure - Here the patient is asked to fixate at point light held at a distance of 33 cm and the deviation of the corneal light reflex from the centre of pupil is noted in the squinting eye.
Each mm of deviation is approximately equal to 7 degree. (1 degree = 2 prism dioptre)The angle of squint is 15 degrees and 45 degrees when the corneal light reflex falls on the border of pupil and limbus, respectively
2. Krimsky and Prism reflection tests-In this test the patient is asked to fixate on a point light and prisms of increasing power (with apex towards the direction of manifest squint) are placed in front of the normal fixating eye till the corneal light reflex is centred in the squinting eye. The power of prism required to centre the light reflex in the squinting eye equals the amount of squint in prism dioptres.
Prism reflection tests- involves the placement of prisms in front of deviating eye until the corneal light reflections are symmetrical.
3. Cover Uncover testTest consists of two parts-Cover test- to detect heterotropia.Procedure - To perform it, the patient is asked to fixate on a point light. Then, the normal looking / fixating eye is covered while observing the movement of the uncovered eye.
In the presence of squint the uncovered eye will move in opposite direction to take fixation, while in apparent squint there will be no movement. This test should be performed for near fixation (i.e., at 33 cm) distance fixation(i.e., at 6 metres).
Uncover test- to detect heterophoria.Procedure - To perform it, one eye is covered with an occluder and the other is made to fix an object.
In the presence of heterophoria, the eye under cover will deviate. After a few seconds the cover is quickly removed and the movement of the eye (which was under cover) is observed. Direction of movement of the eyeball tells the type of heterophoria (e.g., the eye will move outward in the presence of esophoria).
4. Alternate cover test It is a dissociation test which reveals the total deviation when fusion is suspended.Procedure - Suppose Rt eye is covered for several seconds. The occluder is quickly shifted to opposite eye for 2 seconds, then back and forth several times. After the cover is removed, the examiner notes the speed and smoothness of recovery as the return to their pre-dissociated state.
A patient with a well compensated heterophoria will have straight eyes before and after the test has been performed whereas a patient with poor control may decompensate to a manifest deviation.It reveals whether the squint is unilateral or alternate and also differentiates concomitant squint from paralytic squint.
5. Prism cover testIt measures angle of deviation on near or distance fixation and in any gaze position.It combines alternate cover test with prisms.Procedure - Prisms of increasing strength with apex towards the deviation are placed in front of one eye and the patient is asked to fixate an object with the other. The cover-uncover test is performed till there is no recovery movement of the eye under cover.
It gives the amount of deviation in prism dioptres. Both heterophoria as well as heterotropia can be measured by this test.
6. Maddox wingMaddox wing is an instrument by which the amount of phoria for near (at a distance of 33 cm) can be measured. Based on the basic principle of dissociation of fusion by dissimilar objects.It measures heterophoria.The instrument is designed in such a way that, through its two slits, right eye sees a vertical white arrow and a horizontal red arrow and the left eye sees a vertical and a horizontal line of numbers.
Procedure - The patient is asked to tell the number on the horizontal line which the vertical white arrow is pointing (this will give amount of horizontal phoria) and the number on the vertical line at which the red arrow is pointing (this will measure the vertical phoria). The cyclophoria is measured by asking the patient to align the red arrow with the horizontal line of numbers.
7. Maddox rod A Maddox rod consists of many cylindrical glass rods of red colour set together in a metallic disc which converts the appearance of a white spot of light into a red streak. Procedure - Patient is asked to fix on a point light in the centre of Maddox tangent scale at a distance of 6 metres. A Maddox rod is placed in front of one eye with axis of the rod parallel to the axis of deviation.
The Maddox rod converts the point light image into a line. Thus, the patient will see a point light with one eye and a red line with the other. Due to dissimilar images of the two eyes, fusion is broken and heterophoria becomes manifest. The number on Maddox tangent scale where the red line falls will be the amount of heterophoria in degrees. In the absence of Maddox tangent scale, the dissociation between the point light and red line is measured by the superimposition of the two images by means of prisms placed in front of one eye with apex towards the phoria.
Tests for grade of binocular vision and sensory functions.Grades of BSV-Simultaneous perception
Fusion
Steriopsis
1. Worth four dot test-This is a dissociation test which can be used with both distance and near fixation & differentiates between BSV, ARC and suppression. Procedure- For this test patient wears goggles with red lens in front of the left and green lens in front of the right eye and views a box with four lights one red, two green and one white.
Interpretation:All the four lights in the absence of manifest squint normal BSVIn abnormal retinal correspondence (ARC) patient sees four lights even in the presence of a manifest squint.Only three green lights--left suppression.Only two red lights-- right suppression.Three green lights and two red lights, alternately-- alternating suppression.five lights (2 red and 3 green)-- diplopia
2. Test for fixationIt can be tested with the help of a visuoscope or fixation star of the ophthalmoscope. Patient is asked to cover one eye and fix the star with the other eye. Fixation may be centric (normal on the fovea) or eccentric (which may be unsteady, parafoveal, macular, paramacular, or peripheral.
3. After-image testIn this test the right fovea is stimulated with a vertical and left with a horizontal bright light and the patient is asked to draw the position of after-images.Interpretation: A patient with normal RC will draw a cross An esotropic patient with abnormal retinal correspondence (ARC) will draw vertical image to the left of horizontal An exotropic patient with ARC will draw vertical image to the right of horizontal
4. Bagolini Striated GlassesIt detects BSV, ARC or suppression.Each lens of Bagolini glass lens has fine striations which convert a point source of light into a line.Procedure -two lenses are placed at 45 and 135 degree in front of each eye and patient fixates a small light source. Each eye perceives an oblique line of light, perpendicular to that perceived by fellow eye. Dissimilar images are thus presented to each eye under binocular viewing conditions.
Results-Two streaks intersect at their centers in the form of a oblique cross BSVTwo lines but not forming crossDiplopiaOnly one streakno simultaneous perception and suppression Small gap in one of the streak Central suppression scotoma
DiplopiaSuppressionCentral suppression scotoma Normal or ARC
5. Sensory function tests with Synoptophore.Synoptophore compensates for the angle of squint and allows stimuli to be presented to both eyes simultaneously.Synoptophore (major amblyoscope) consists of two tubes, having a right-angled bend, mounted on a base. Each tube contains a light source for illumination of slides and a slide carrier at the outer end, a reflecting mirror at the right-angled bend and an eyepiece of +6.5 D at the inner end. The two tubes can be moved separately or together by means of knobs around a semi-circular scale.
Synoptophore is used for many diagnostic and therapeutic indications in orthoptics.Synoptophore tests for sensory functions include: Estimation of grades of binocular visionDetection of normal/abnormal retinal correspondence(ARC). It is done by determining the subjective and objective angles of the squint.
In normal retinal correspondence, these two angles are equal. In ARC, objective angle is greater than the subjective angle and the difference between these is called the angle of anomaly. When the angle of anomaly is equal to the objective angle, the ARC is harmonious. In unharmonious ARC angle of anomaly is smaller than the objective angle.
6. Neutral density filter testIn this test, visual acuity is measured without and with neutral density filter placed in front of the eye. In cases with functional amblyopia visual acuity slightly improves while in organic amblyopia it is markedly reduced when seen through the filter.
7. Tests for StereopsisTests on stereopsis can be based on two principles-Using targets which lie in two planes, but are so constructed that they stimulate disparate retinal elements and give a three dimensional effect, for example:Circular perspective diagram such as the concentric ringsTitmus fly test, TNO test, Random dot stereograms, Polaroid testLangs stereo testStereoscopic targets presented haploscopically in major amblyoscopeUsing 3 dimensional targets (e.g. Langs two pencil test).
Stereopsis is measured in seconds of arc.Qualitative tests for Stereopsis:Langs 2 pencil testSynaptophoreQuantitative tests for Stereopsis:Random dot testTNO TestLangs stereo testMethods using Polarization:Targets are provided as vectographs and images seen by one eye is polarized at 90 degree using polarized glasses.Titmus stereo fly testPolaroid testRandom dot stereogramsTNO test
1. Synoptophore / Stereoscope tests / Stereograms:Stereogram with three concentric circles and a check dot for each eye is to be seen with both eyes together. Stereograms with three eccentric circles are to be seen with each eye separately. If the patient reports seeing concentric circles, it means stereopsis is present. If they are seen eccentrically one may ask whether the inner circles are closer to the right or left of the outer circle. It determines whether the disparate elements are suppressed in the right or the left eye.
2. Vectographs:Consists of Polaroid material on which the two targets are imprinted so that each target is polarized at 90 degrees with respect to the other. Patient is provided with Polaroid spectacles so that each target is seen separately with the two eyes.Titmus stereo testThe three-dimensional polaroid vectograph which constitutes the Titmus test is basically made up of two plates in the form of a booklet.To perform the test the plates are reviewed with polaroid glasses. The Titmus stereo test consists of three parts:
Fly test- The right side of the test booklet contains a large housefly to test gross stereopsis (threshold 3000 sec of arc). It is especially useful in young children. The subject is asked to pick up one of the wings of the fly, If the subject sees stereoscopically, he will reach above the plate. In the absence of gross stereopsis the fly will appear as an ordinary flat photogrpah.
Fig. Titmus test using fly for gross stereopsis A- no stereopsis B-Stereopsis present
Animal test- It is performed if the gross stereopsis is present. This test consists of three rows of five animals each; one animal from each row is imaged disparately (thresholds 10, 200 and 400 see of arc. respectively) And, in each row, one of the animals correspondingly imaged in two eyes is printed heavily black (serves as a misleading clue). The subject is asked which one of the animals stands out. A subject without stereopsis will name the animal printed heavily (misleading clue); while in the presence of stereopsis he will name the disparately imaged animal.
Circle test - It consists of nine squares, each containing four circles arranged in the form of a lozenge . Only one of the circles in each square is disparately imaged at random with threshold ranging from 800 to 40 sec of arc. If the subject has passed other two tests, he is asked to 'push-down' the circle that stands out, beginning with the first set, When he makes mistakes or finds no circle to push down, the limit of his stereopsis is presumably reached,Circle No. 5, equivalent to 1(X) sec of arc is considered to he lowest limit of fine central stercoacuity and is designated as the lowest limit of good stereoacuity.
3. Random dot stereogram tests- The random dot stereogram tests are devoid of monocular clues and the patients cannot guess what the stereo figure is and where it is located on the test plate. So, this test provides truer measurement of stereopsis than the Titmus test .
Other tests- Frisby test -Stereoscopic contours induced optokinetic nystagmus test and Television random dot stereotest
4. Simple motor task test based on stereopsis- Two pencil test- It is very simple primitive bin an effective test for detecting presence or absence of gross stereopsis (threshold value 3000 - 5000 sec of arc). To perform this test, examiner holds a pencil vertically in front of the patient, who is asked to touch its upper tip with the tip of the pencil held ill his hand by one swill movement from above. Patient having stereopsis passes the test with both eyes open. Patients fail the test with one eye closed or when both eyes are open but stereopsis is absent
DiplopiaThe simultaneous appreciation of two images of the same object in different positions and result from images of the same object falling on non-corresponding retinal points. Types - Binocular - Uniocular
Binocular diplopia- It occurs due to formation of image on dissimilar points of the two retinae.Causes- Paralysis or paresis of the extraocular musclesDisplacement of one eye ballMechanical restriction of ocular movements as caused by thick pterygium, symblepharon and thyroid ophthalmopathy. Deviation of ray of light in one eye as caused by decentred spectacles. Anisometropia
Types- Uncrossed diplopia- In uncrossed (harmonious) diplopia the false image is on the same side as deviation. It occurs in convergent squint. Crossed diplopia- In crossed (unharmonious) diplopia the false image is seen on the opposite side. It occurs in divergent squint.
Uniocular diplopiaIn uniocular diplopia an object appears double from the affected eye even when the normal eye is closed.Causes-Subluxated clear lens (pupillary area is partially phakic and partially aphakic). Subluxated intraocular lens (pupillary area is partially aphakic and partially pseudophakic). Double pupil due to congenital anomaly, or large peripheral iridectomy or iridodialysis. Incipient cataract-Usually polyopia i.e., multiple images may be seen due to multiple water clefts within the lens. Keratoconus.
Evaluation of diplopia1. Diplopia charting. It is indicated in patients complaining of confusion or double vision. In it patient is asked to wear red and green diplopia charting glasses. Red glass being in front of the right eye and green in front of the left. Then in a semi-dark room, he is shown a fine linear light from a distance of 4 ft. and asked to comment on the images in primary position and in other positions of gaze. Patient tells about the position and the separation of the two images in different fields.
2. Hess screen test.
Hess screen plot the dissociated ocular position as a function of extraocular muscle action and enables differentiation of paralytic squint caused by neurological pathology from restrictive myopathyHess screen test tells about the paralysed muscles and the pathological sequelae of the paralysis, viz., overaction, contracture and secondary inhibitional palsy.
Electronic Hess screen contains a tangent pattern (2 D projection of a spherical surface) printed onto a dark grey background.Red lights that can be individually illuminated by a control panel indicate the cardinal positions of gaze within a central field (15 degree from primary position and a peripheral field 30 degree), each square represents 5 degree of ocular rotation.The two charts are compared. The smaller chart belongs to the eye with paretic muscle and the larger to the eye with overacting muscle.
Procedure- Patient is seated 50 cm from screen and wears red-green goggle ( red lens in front of right eye) and holds a green pointer.The examiner illuminated each point in turn which is used as the point of fixation. This can now be seen only with RE, which therefore becomes the fixating eye.The patient is asked to superimpose their green light on red light, so plotting the relative position of the left eye. All points are plotted in turn.In orthophoria the two lights should be more or less superimposed in all nine positions of gaze.The goggles are then reversed (red filter in front of left eye) and procedure is repeated.The relative positions are marked by the examiner on a Hess chart and connected with straight line.
Interpretation- Two charts are comparedSmaller chart indicates eye with paretic muscle (RE)Larger chart indicates eye with overacting yoke muscle (LE)Smaller chart will show its greatest restriction in main direction of action of paretic muscle (Rt LR)Larger chart will show its greatest expansion in main direction of action of yoke muscle (Lt MR)The degree of disparity between plotted point and template in any position of gaze gives an estimate of angle of deviation.
3. Field of binocular fixationIt should be tested in patients with paralytic squint where applicable, i.e., if patient has some field of single vision. This test is performed on the perimeter using a central chin rest.
4. Forced duction test (FDT) It is performed to differentiate between the incomitant squint due to paralysis of extraocular muscle and that due to mechanical restriction of the ocular movements.FDT is positive (resistance encountered during passive rotation) in cases of incomitant squint due to mechanical restriction and negative in cases of extraocular muscle palsy.
Squint Surgery-It is required in most of the cases to correct the deviation. However, it should always be instituted after the correction of refractive error, treatment of amblyopia and orthoptic exercises.Basic principles of squint surgery-To weaken the strong muscle by recession (shifting the insertion posteriorly) To strengthen the weak muscle by resection (shortening the muscle)
Types-Weakening procedures-RecessionDisinsertionPosterior fixation sutureStrengthening procedures-ResectionTuckingAdvancement of muscle near limbus
Type and amount of muscle surgery-depends upon the type and angle of squint, age of patient, duration of the squint and the visual status.
The maximum limit allowed - MR -resection - 8 mm - MR -recession - 5.5 mm------ LR -resection - 10 mm - LR -recession - 8 mm
Muscle ResectionRecessionMR1-1.5 degree2-2.5 degreeLR1-2 degree1-2 degree
THANK YOU