Envoy Clearinghouse User’s Guide - MDsuite - Electronic Medical
Transcript of Envoy Clearinghouse User’s Guide - MDsuite - Electronic Medical

ENVOY Users Guide for elligence.doc
Envoy Clearinghouse User’s Guide For Use with the elligence Practice Management System
Clearinghouse: WebMD Envoy (800) 845-6592 File Format: National Standard Format
Revision Date: May 19, 2003
9645 Granite Ridge Drive, Suite 230 San Diego, CA 92123
Technical Support (858) 514-0311 l Fax (858) 514-0322 E-mail: [email protected] l web: www.elligence.net

Data Strategies, Inc. Envoy User’s Guide ’
Revision Date: May 19, 2003 Page 2
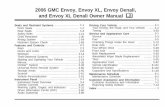
Table of Contents
Introduction...........................................................................................3 Chapter One..........................................................................................5
ENROLLMENT WITH ENVOY..............................................................................................5 SETTING UP YOUR SYSTEM FOR EMC TO ENVOY...........................................................5
Define > Primary Tables > EDI Destinations ......................................................................5 Define > Secondary Tables > Insurance Plans ...................................................................6 Define > Secondary Tables > Procedures ..........................................................................7 Define Secondary Tables > Providers................................................................................7 Define > Other Tables > Billing Entities..............................................................................8 Transactions > Post Charges ............................................................................................8
Chapter Two..........................................................................................9
BILLING CLAIMS TO ENVOY ..............................................................................................9
Step One: Pre-Processing and File Generation..................................................................9 Step Two: File Transmission ...........................................................................................12 Step Three: Post Processing ..........................................................................................13
Appendix One – Manually Transmitting Files to Envoy.............. 14 Appendix Two – Sample Envoy Reports....................................... 15 Appendix Three - Understanding the Flow of the Envoy Billing Process............................................................................................... 16

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 3
Introduction
Envoy is a company that acts as a clearinghouse for insurance claims. They accept insurance claims for a few hundred different insurance carriers, called Participating Payers. These companies are subsidizing Envoy’s processing of their claims because it is in their best interest. Claims billed electronically can be transferred from the provider’s office, to the clearinghouse, and then to the carriers’ offices entirely without human intervention. Automated processes handle all transactions – from delivering the claims to the proper destination to reporting back to the sender on any warnings, errors, and claim adjudication messages.
ü Benefit to the Insurance Carrier: They do not have to hire people to enter or look over claims manually.
ü Benefit to the Medical Office: Claims can be processed faster and more efficiently. Payment arrives sooner and so cash-flow is greatly improved.
The Envoy clearinghouse works this way:
1. Your office uses the system to build claims files according to Envoy’s specifications
2. You transmit them to the clearinghouse via telephone lines and a modem through the elligence EDI Manager.
3. The clearinghouse processes your claims and sends you a “Post-Processing” report to let you know what they found – how many claims were received, accepted and rejected plus many other valuable pieces of information. All rejections explained in detail in these reports.
4. All claims accepted by the clearinghouse are forwarded to their destination carrier.
5. That carrier process the claims they receive from the clearinghouse and either begins the payment process, or returns a report to the clearinghouse letting them know why they could not pay for the claims. This information is returned to you electronically via the Post Processing reports.
Envoy will not send you any information through the mail. All of the communication you will have with them will be through electronically transmitted reports and messages. This is a little different from most of the carriers you may be used to working with, so it is imperative to your success in working with Envoy that you stay aware of the online messages and reports they send you. This procedure will be explained later in this document.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 4
Envoy has a technical support staff that is capable of answering any questions you have about your post-processing reports or claims that have been denied. The phone number for Envoy technical support is (800) 845-6592. When you call them for help, please try to have the following information available:
• Your submitter ID # (also known as your TSO #)
• Your Provider’s or Group’s billing ID – (either a Tax ID # or a Social Security #)
• Patient information (name, policy #, primary insurance coverage)
• The claim’s detail information (date billed, date of service, procedure code, fee)
• Data Strategies’ Tax ID – 953613969 – since we are considered your “submitter” or “vendor”.
When you call Envoy with questions it is likely they may give you technical information as part of their answer. Please keep in mind that this information is valuable and you may need to contact Data Strategies technical support for help using it to your benefit. Be sure to write down any information they give like record names, dates, or any instructions they give you.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 5
Chapter One ENROLLMENT WITH ENVOY The enrollment process with Envoy should be simple and straightforward, no matter which types of claims you choose to send through the clearinghouse. Commercial claims can be submitted after one enrollment form is filled in and returned to Data Strategies. I f you choose to send claims for what are known as “Non Participating” carriers, the enrollment process will take a little longer.
Along with this booklet, you should have received an EDI Submitter Information sheet that includes your Electronic Billing Options and a EDI Checklist which you can use to be sure your enrollment is being handled correctly. Please refer to these documents for detailed information about Envoy enrollment procedures.
SETTING UP YOUR SYSTEM FOR EMC TO ENVOY In order to bill your commercial insurance claims to the Envoy clearinghouse, you must have your system setup correctly. These screens within the system require careful attention:
Define > Primary Tables > EDI Destinations
Define > Secondary Tables > Insurance Plans
Define > Secondary Tables > Procedures
Define > Secondary Tables > Providers
Define > Other Tables > Billing Entities
Transactions > Post Charges
Billing > Electronic
Define > Primary Tables > EDI Destinations Define these fields once for the Envoy clearinghouse:
Field Usage / Description
Receiver Number Please enter “envoy” into this field.
ANSI Delimiters Leave these as their default values.
Claims –
Modem Phone Number Must be 888-696-7869
File Spec Must be NSF 3.1 (Adjusted for Envoy)

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 6
Submitter – (Identifies the submitter doing the billing – not necessarily the Provider)
Provider Type Select the most appropriate choice.
Submitter Type Select Person if you need to enter a First and Last Name. Select Non-Person Entity if you have only one name to enter (as for a business).
Submitter Number Enter the Submitter Number, or TSO assigned to you by DSI. Do not enter the letters, “TSO”.
Contact EDI Access Number Leave blank for Envoy.
Claims – Mode Set to Production unless you are instructed to do otherwise by DSI.
Username Enter Site ID assigned to you on your Submitter Information sheet. Usually, “0001”.
Password Enter the password assigned to you on your Submitter Information sheet.
Define > Secondary Tables > Insurance Plans Define these fields for each Insurance Plan you will be billing though Envoy:
Field Usage / Description
Name and Address Each company must have a valid street address, including the city state and ZIP code.
Payer Type Choose the appropriate entry from the list (Commercial Insurance Co, Blue Cross/Blue Shield, Medicare or Medicaid)
Payer ID The 5-character code for this carrier from the current Envoy Payer Lists. These lists are always available from www.envoy.com.
EDI Destination Set to Envoy.
Capitated Plan Must be unchecked.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 7
Define > Secondary Tables > Procedures Define these fields for each procedure you will be sending to Envoy:
Field Usage / Description
AMA Code Every procedure billed to Envoy must have a AMA Procedure code.
Type of Service Must be selected. ‘A-Medical Service’ is a safe choice if you are unsure.
Bill via Electronic Billing Both must be checked
Defaults, Place of Service It is a good idea to select a default Place of Service here.
Define Secondary Tables > Providers Define these fields for every provider you will be billing to Envoy:
Field Usage / Description
Location Choose a billing location (address) to assign to this provider
Specialty Code Choose a specialty from the list of available options.
Employer ID The Tax ID # or Social Security # that this particular provider will be billing to Envoy with.
Medicare, Medicaid, BC/BS, Commercial Identifiers Enter these numbers for this Provider as required for the types of claims you will be billing through Envoy.
Provider Plan Network Identification Number Enter your Provider’s License #.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 8
Define > Other Tables > Billing Entities Complete the Billing Entities screen according to the Data Strategies’ provided instructions. If you need help with this, please contact your Data Strategies Technical Support team.
Transactions > Post Charges Be sure to keep these things in mind as you Post Charges :
Field Usage / Description
Provider Select the performing physician.
Location Select the location that describes where the work was performed.
Billing Entity Select the appropriate Billing Entity for each Charge.
Ins Memo Enter any comments for this particular charge that should accompany this claim

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 9
Chapter Two
BILLING CLAIMS TO ENVOY
The following list explains the Envoy billing life-cycle. These steps are followed in a circle as you bill new claims and respond to problems identified in older claims and then begin billing again.
Step One: Pre-Processing and File Generation
Step Two: File Transmission
Step Three: Post-Processing
Step One: Pre-Processing and File Generation In elligence, go to Billing > Electronic. As with all related features in elligence, you should setup a Profile that will make this process work just the way that you want it to.
Billing Date This is the date that your charges will show as having been billed on. We recommend that you leave this date as “today’s date” unless you have a really good reason to change it.
Bill the following Destinations
You may select to generate claims for other Destinations at the same time as Envoy, or you may choose to create each Destination’s files separately.
Bill Primary Coverages for Charges that:
Have not been billed to the current responsibility
Check this option to bill new charges for the first time, or to bill charges which have been “reset”.
Were Previously Billed From…
Check this option to enable automatic rebilling of charges that were originally billed in the selected date range. Recommended.
Advanced Selections
Make any selections here for Patients and/or Charges if you do not wish to allow all billable charges to be sent out at this time. Normally, recommended only in special cases.
Page Setup Choose how you want elligence to output your Exceptions and Pre-Processing reports.
Use Performing Provider as Referring Doctor…
Please a check in this box if you wish to see elligence insert your Performing Provider’s names/UPIN whenever a Referring Doctor is required but none was provided in the Patient’s Illness.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 10
Previewing the Exception Report
When you click Next, you will either be taken to a Preview of the Exception Report (if problems are found) or the Pre-Processing report. The Exception report lists any problems that elligence identified with the claims you wanted to bill at that time. The system cannot locate every possible problem with your claims but it can catch most of them. Here is a sample of what the Exception Report can look like:
Each Exception (or problem) discovered by the system is shown as a hyper-link on the preview of this report. While you are looking at the preview, you can click on each hyper-link to jump to the screen where you can make whatever correction is needed. For instance, in the sample report above, you could click on the words Insurance Company – Aetna to jump to the Define > Secondary Tables > Insurance Companies screen in order to enter the company’s Payer ID. Normally, you should click on each link and enter whatever data was found to be missing or invalid until all of the problems that elligence found have been taken care of. You may print this report and deal with the errors out side of this screen if you would rather as well.
Previewing the Pre-Processing Report
When you click Next from the Exception Report, you will be taken to the Pre-Processing Report. This report gives you a list of the charges that were found to be ready for billing by elligence, excluding any charges that are still listed on the Exception Report. You always have the choice to correct your Exceptions or not but Patients or Claims with Exceptions will not be billed by elligence.
Select the Print button at the bottom of the Pre-Processing Report window in order to receive a printed copy of the report. If you are going to allow the system to create a file with these charges, you will definitely want to print the report before clicking Next again. This report is your proof of which claims were billed electronically today.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 11
File Generation
When you are finished printing the Pre-Processing Report, select the Next button to begin the File Generation. The system will gather together all of the claims that were accepted by the system and build one or more files for each EDI Destination you selected for this batch. Any claims that you left listed on the Exception Report will not be included in these files. Normally, elligence will create one file for each type of claim in this batch, according to the included Payer Types. So, for instance, you may receive two files – one that includes your Commercial claims and one that includes your Blue Cross/Blue Shield claims.
Ø Important Note
As the system builds this file with the accepted Envoy claims, those claims will be marked as “Billed” to Envoy. This is important because the system does this before you ever try to transmit the claims to Envoy. If you were to go through the File Generation step, but never transmitted the claims to Envoy, the system would still show them as having been billed.
When the File Generation step is completed, you will be shown a link to the EDI Manager, which is where you want to go to transmit your claims. You may either click this link now, or go to Billing > EDI Manager whenever you are ready to submit these claims.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 12
Step Two: File Transmission Go to Billing > EDI Manager > Outbox. Your newly generated Envoy files should appear in the list in your Outbox by default. This indicates that they are ready to be transmitted. Select the Send/Receive button to start your File Transmission. This will include all of the files in your Outbox at this time, except those that you have specifically asked the system to “HOLD”. You always have the option of selecting to transmit only those files created for the database you are currently logged into, or for all databases at once.
Data Strategies recommends that you normally assign the EDI Send/Receive process to one person in your office and that they perform this process just once per day, when they are ready to work with all of your EDI Destinations at once. This will simplify both that person’s workload and the job of any technical support personnel who wish to help them with this process.
The EDI Send/Receive process will automatically call every EDI Destination for every database in order to upload any new claims files for that Destination and to download any new reports that have become available since the last time the system logged on using your information. The EDI Manager will call out to every destination whether you have new files for it at this time or not, so please be patient.
Each call to Envoy will include these steps:
• Your elligence application server calls Envoy’s computers using a toll-free phone number.
• It logs in, sending Envoy your submitter code and password to identify you.
• Envoy sends us the latest Post-Processing report they have available. This is always a report that tells you about your previous file submission.
• Elligence sends Envoy your new claim file(s).
• We log-off of Envoy’s computer and disconnect.
When the Send/Receive button is first selected, a window will pop-up letting you know that the EDI Manager file transmission process will be running in the background for some time and that you are now free to go and complete any other work in the system that you wish to. When that background File Transmission is complete, you will receive a pop-up Tickler message indicating whether this transmission was successful or not. These Ticklers will remain active in your Ticklers window (Utility > Ticklers) until you choose to delete them.
All claims files will automatically be moved from the Outbox folder to the Sent Items folder when they have been successfully transmitted to their EDI Destination. A Log file will be created for each combination of database/EDI Destination and those Logs can be viewed in the Logs folder of the EDI manager. Any reports that were received from Envoy during this process will be placed into the InBox folder for your review. See below for more on this.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 13
A Note About Script Files
A script file is a set of instructions for your computer, like a small program. We create script files that tell your computer how to transmit your EMC files to every EDI Destination that is supported in elligence. This saves you from having to enter all the transmission specific information that would normally be required. If, for any reason, you have chosen not to use the built-in Send/Receive process for your Envoy claims files, see Appendix One for information and instructions on logging into Envoy’s computers manually.
Step Three: Post Processing Each time you transmit a new claim file to the Envoy clearinghouse, they also send you a Post-Processing report. Each Post-Processing report informs you of the results from your previous file transmission. For example, if you submit your files every Wednesday, the report you get this week will inform you about the previous Wednesday’s submission. See Appendix Two for a list of the types of reports that will be available to you through Envoy.
To review these reports after a successful Send/Receive process, go to Billing > Electronic > InBox. The reports will be sorted by Destination and then database and then filename/date. Select the newest Envoy report you have not yet looked and click View to read its contents.
You will be shown a Preview of the report, and you may select the Print button at the bottom of that screen to begin printing the report. This is recommended so that you have a copy of each report for your files.
Look carefully at the report. It will show you whether your previous batch of claims was accepted by the clearinghouse or rejected for some reason.
Look for sections called, “Batch and Claim Level Rejections” – these describe in detail the problems that Envoy found with these claims, if any.
Look for the sections called, “Acceptance Report” – these list the names of patients whose claims were Accepted by Envoy.
See Appendix Two for further information about the Envoy Post-Processing reports.
You should correct any claims listed as problems on these reports and then rebill them whenever this is convenient for you. This returns you to the top of this billing life-cycle and so you repeat this process with some new claims and some re-billed claims as necessary.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 14
Appendix One – Manually Transmitting Files to Envoy These instructions assume you will enter a third-party modem communication software being run outside of elligence rather than using our Send/Receive process. 1. Get into your third-party communications software. 2. Set it to E-7-1. 3. Set it to dial this number: 888-696-7869 4. When prompted with this: Type this: Please type terminal identifier A
Please log in: NEICTSO03 [EN]
Password MI CLAIMS [EN]
SELECT APPLICATION TSOK [EN]
ENTER USERID/PASSWORD(/NEWPASSWORD)+
TSO****/{your password} [EN]
IKJ*****I TSO**** LOGON IN PROGRESS...
Kermit ready to send... {The report should download automatically – do nothing} …The File Transfer progresses...
HAVE YOU RECEIVED A REPORT FILE? yes [EN]
Kermit ready to receive. {Begin the File Upload procedure in your software now}
Uploading file: XXXXXXXXXX.NSF
{The File Transfer progresses...} {wait}
Submitted. Press [EN]
Ready. LOGOFF [EN]
Please login: Disconnect from Envoy..
If you need to send another claim file Start this process from the beginning again.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 15
Appendix Two – Sample Envoy Reports You will receive a Post-Processing report each time you log in to the Envoy clearinghouse. When you begin each File Transmission, you will have the option to either receive your report concerning the previous file transmission and then submit a new claim file, or just log in and receive the report. If you would like, you may request that Data Strategies send you a complete set of sample reports with explanations of each piece of information they might contain.
The Post-Processing reports you receive from Envoy will fall into one of these categories:
DAILY REPORTS
Provider Daily Statistics – This report contains statistics for every batch of claims submitted for each provider. Rejected batches and claims are listed with detailed error explanations. It is imperative that this report be reviewed after each file transmission to prevent “lost” claims.
Provider Daily Summary – This is a summary of the number of accepted claims per batch submitted. This report also has a totals section which displays all input, accepted, and rejected daily, month-to-date (MTD), and year-to-date (YTD) statistics.
Daily Acceptance Report by Provider – This report lists only claims that have been accepted by NEIC. The report shows only the name and account number for each patient’s accepted claims.
MONTHLY REPORT
Provider Monthly Summary – This report displays the number of accepted claims sent to the destination insurance carriers including month-to-date (MTD) and year-to-date (YTD) totals. The second section of this report is a monthly summary and percentage listing of claim-level rejections and warnings. This is a good place to see what type of errors you are experiencing most frequently so that you can correct them.
EXCEPTION REPORTS
Unprocessed Claims Report – This report informs the provider that the following claims are unable to be processed by the payer (insurance carrier) and what corrective action should be taken. This is very important since it tells you that a claim was forwarded by the Envoy clearinghouse to the destination insurance company, but they found some problem and could not pay for the claim. Usually these types of problems can be fixed and then resubmitted electronically.
Claim Settlement Report – These reports provide information regarding adjudicated claims. When the destination insurance carrier has any qualifications to paying for the claims, they will be listed here. For instance, problems such as, dates of service billed after coverage was terminated will be shown here.

Data Strategies, Inc. Envoy User’s Guide
Revision Date: May 03 Page 16
Appendix Three - Understanding the Flow of the Envoy Billing Process
What You Do In The Office What Envoy and The Carriers Do
Generate new claim file(s).
Logon to Envoy and 1. receive your
report, if first call of the day
2. send the new file(s)
Logoff from Envoy, and read your Post-processing report and then make corrections to any claims listed there as rejected.
Begin by Pre-Processing and correcting any errors listed on the Pre-Processing report.
Envoy receives the claim from you and checks it for problems.
If problem(s) found, they’ll return the claim to you for correction and resubmission.
If no problem is found, claim is forwarded to carrier.
If the carrier finds a problem, they will report the problem to Envoy. Envoy will report the problem to you.
If the carrier accepts the claim as is, they will pay it or deny it within their usual period.