Enamel presentation. prepared by mohammed yahia
-
Upload
maher-aziz -
Category
Documents
-
view
695 -
download
2
Transcript of Enamel presentation. prepared by mohammed yahia
1- Introduction2- Formation of enamel3- Physical characteristics 4- Chemical composition5- Structure of enamel 6- Histological features of enamel7- Defects of enamel8- Treatment
objectives
Definition:
* Tooth enamel, along with dentin, cementum, and
dental pulp is one of the four major tissues that make
up the tooth in vertebrates. It is the hardest and most
highly mineralized substance in the human body. . It is
the normally visible dental tissue of a tooth because it
covers the anatomical crown and must be supported
by underlying dentin.
* Also define as “Acellular hard mineralized tissue that
forms the protective covering of variable thickness
over the entire surface of the crown”
Introduction
Odontogenesis “ tooth development”
1- initiation stage - 6th to 7th week
2- Bud stage – 8th week
3- Cap stage- 9th to 10th week
4- Bell stage – 11th to12th week
5- apposition stage – varies per tooth
6- maturation stage – varies per tooth
Amelogenesis “Enamel formation”
1- secretory phase.
2 – maturation phase.
Formation of enamel
Cap stageThe proliferation and growth are
unequal in the different parts of the
tooth bud, leading to formation of
cap shaped structure with deep
central depression attached to dental
lamina termed enamel organ. Dental sac
Bell stageThis stage characterize by
continuation of the proliferation and
further morphodifferentiation and
histodifferentiation. That’s lead to
formation of four well differentiated
cells types within the enamel organ.
The enamel organ consist of four layer :• Outer enamel epithelium
• Stellate reticulum
• Stratum intermedium
• Inner enamel epithelium
amelogenesis
• Secretory Phase
• Partially mineralized
enamel (30%)
• Full thickness of
enamel is formed
• Maturation Phase
• Influx of minerals
• Efflux of organic
material and water
amelogenesisTo understand the amelogenesis (formation of enamel) we must understand the life cycle of ameloblast (cells that forming the enamel).
Life cycle of amelobalst
• Morphogenic Stage
• Differentiation Stage
• Secretory Stage
• Maturation Stage
• Protective Stage
• Desmolytic Stage
Morphogenetic Stage
• Occurs during early Bell Stage of tooth
development
• Inner Enamel Epithelium
– Low columnar to cuboidal cells
– Centrally placed nucleus
– Golgi bodies placed proximally.
– Mitochondria and other cytoplasmic bodies are
scattered.
Differentiation Stage• Occurs during late Bell stage
• IEE Ameloblasts
• Ameloblasts (Histological changes)
• Elongates
• Nucleus shifts proximally.
• Golgi complex increases in volume
& migrate to central core of cell.
• Increase in ER
• Mitochondria shift proximally.
Basal lamina
Secretory Stage
• Synthesis of enamel proteinsEndoplasmic Golgi apparatus Reticulum
• Immediate mineralization of enamel matrix
Condensed and packaged membrane bound secretory granules
Contents released over newly formed dentin from distal end of ameloblast
Maturative Stage
• Ruffle-ended ameloblast
– Release of inorganic material
– Proximal junctions are leaky and
distal junctions are tight.
• Smooth ended ameloblast
– Removal of proteins and water
– Distal junctions are leaky while
proximal junctions are tight.
Water and organic material is selectively
removed from enamel with addition of
inorganic material.
Protective Stage
• Ameloblasts + SI + SR + OEE together form
stratified epithelium – Reduced Enamel
Epithelium.
• Function – Protect mature enamel till
eruption by separation from the connective
tissue.
Protective Stage
• Anomalies may develop in case connective
tissue comes in contact with enamel surface.
• At CEJ, ameloblasts may retract resulting in
deposition of afibrillar cementum on the
enamel surface.
Desmolytic Stage
• Epithelium induces atrophy of connective tissue, thus facilitating fusion of oral epithelium and REE.
• Epithelial cells release enzymes to destroy connective tissue by desmolysis.
• Premature degeneration may prevent the eruption of tooth. (impaction of teeth)
• Thickness
• Color
• Hardness
• Tensile strength
• Permeability
• Solubility
Physical characteristics
ThicknessThe thickness of enamel varies in different areas of the same tooth and
from one type of tooth to another type.
Thickness of enamel decrease gradually from cusps or incisal edges to CEJ.
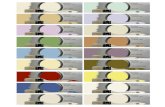
ColorThe color of enamel is usually gray and translucent in nature.But the color of tooth mainly depends upon three factors:1- color of underlying dentin. 2- thickness of enamel.3 – amount of stains in enamel.
HardnessEnamel is the hardest calcified tissue in the bodyBecause of its high content of minerals.( 96% )Enamel can withstand load of mastication and resist wear process
Tooth type thickness
Anterior tooth (incisal edge) 2 mm
Premolar tooth (cusp) 2.3 to 2.5 mm
Molar tooth (cusp) 2.5 to 3 mm
Tensile strengthAlthough it is hard , enamel is extremely brittle thus it has low tensile
strength and depends on the strength of the underlying dentin.Significance Because of high compressive strength of dentin than enamel, the
dentin acts as a cushion for enamel when masticatory forces are applied on it. For this reason, during tooth preparation, for maximal strength of underlying remaining tooth structure all enamel rods should be supported by healthy dentin base.
PermeabilityEnamel is selectively permeable, permitting partial or complete
passage of ions due to the presence of microscopic poresSolubility
Enamel dissolves in acid media. Its surface is less soluble than deep enamel.
Significance Acid etching of enamel which is very important technique for
conditioning enamel for many clinical procedures such as fissure sealants, restoration, cementing or orthodontic bands..etc.
Chemical composition
Mature enamel consists of:• Mainly(96%) inorganic substances, Mainly calcium
phosphate crystals (calcium hydroxyapatite crystals).
• Small (3%) amount of organic substances,Mainly non collagenous proteins:
A- amelogenins. B- non-amelogenins- ameloblastin- enamelin- tuftelin
• (1%) water
Enamel rod The basic unit of enamel
Number: 5 – 12 millions.
Direction: Run in oblique direction and wavy course.
Length: greater than the thickness of E.
Diameter average: 4 µm.
Appearance: Have a clear crystalline appearance.
Cross-section: hexagonal, round
Inter rod substance
•Cementing E. rods together.
•More calcified than the rod sheath.
•Less calcified than the rod itself.
•Appears to be minimum in human teeth.
Rod sheath
The boundary between rod and interrod enamel is marked by a narrow space filled with organic materials known as rod sheath
GNARLED ENAMEL
Gnarled enamel is found at the cusps of teeth. Its twisted appearance results from the orientation of enamel rods and the rows in which they lie…Significance: This part of enamel is resistant to cutting
while tooth preparation.
D
Twisted course of enamel rods
Gnarled enamel
Histological features of enamel
Stria of Retzius
• During development of enamel, variations in the metabolism of the organism cause variations in the amount of organic material deposited in the enamel. This causes changes in the coloration of the enamel that is layedown at that time so that alternating dark (higher organic material) and light (less organic material) banding occurs. These bands are called Stria of Retzius. The stria of retzius usually intercept the dentino-enamel junction.
Perikymata
Striae of Retzuis often extend from the DEJ
to the outer surface of the enamel, where
they end in shallow furrows know as perikymata (or imbrication line )
Neonatal line:
* It is an enlarged stria of Retzius which present in all deciduous teeth and 1st permanent molar.
* This line separates between enamel formed before birth and enamel formed after birth.
* This line is due to the sudden change of nutrition and environment due to birth.
* The quality of enamel formed before birth is better than that formed after birth, because of the more protected conditions and constant nutrition of the fetus.
Enamel Lamellae
* Enamel lamellae extend from the surface to varying depths of the enamel
* They are faults that develop as a result of failure of maturation processes. They are filled with organic material and water
* Some studies say the lamellae is the pathway of bacteria
Enamel spindles ENAMEL
* It originate from the DEJ
* Before enamel forms, some developing odontoblastsprocess extend into the ameloblast layer, and when enamel formation begins become trapped to form enamel spindles.
Significance: Spindles serve as pain receptors, that is why, when we cut in the enamel patient complains of pain.
ENAMEL TUFTS
* It originate from the DEJ, run a short distance in the enamel or sometimes to one half of the thickness.
* They are considered to be ‘faults’ by some researchers while others consider them to be necessary to anchor dentine to enamel...
Significance: Enamel tufts are hypomineralizedstructure in the enamel, thus play role in spread of dental infection.
Hunter-Schreger bands
* Hunter Schreger bands are seen here with special illumination in longitudinal ground sections of enamel as light and dark bands
* The dark bands (Diazones) absorb the light where the light bands (Parazones) reflect the light.. Significance: They are considered to resist and disperse the strong forces.
Dentino-enamel junction
* It is a border between the Enamel and Dentin (composed from both).
* DEJ is pitted/scalloped in which crests are toward enamel and shallow depressions are in dentin.
* This helps in better interlocking between enamel and dentin.
Defects of enamel
Genetic Non Genetic 1- Amelogenesis imperfctaA - Hypoplastic (type 1) B- Hypomaturation (type 2)C- Hypocalcified (type3).
1- caries 2 – attrition 3 – abrasion 4- erosion5- localized nonhereditary enamel hypoplasia 6- localized nonhereditary enamel hypocalcification7-fluorosis
Amelogenesis imperfecta is a group of
conditions caused by defects in the genes encoding
enamel matrix proteins.
Type 1: hypoplastic amelogenesis imperfecta• The main defect is in formation of the matrix (protein).
• Enamel is not formed to full thickness because
ameloblasts fail to lay down sufficient matrix.
• Enamel is randomly pitted, grooved or very thin, but
hard and translucent.
• Affected teeth appear small with open contacts due to
very thin or nonexistent enamel causing thermal
sensitivity.
• Teeth are not susceptible to caries unless the enamel is
scanty and easily damaged.
• Commonly in men.
Type 2: hypomaturation amelogenesis imperfecta
• Occurs during matrix apposition.
• Enamel is softer and chips from the underlying
dentin.
• Enamel has a mottled brown-yellow-white color.
• Contact points present as enamel is of normal
thickness.
• Radiographically enamel approaches the
radiodensity of dentin.
Type 3: hypocalcified amelogenesis imperfecta
• Occurs during the calcification stage.
• Most common type.
• Enamel is of normal thickness but soft, friable,
and easily lost by attrition.
• Enamel appears dull, lustrous, honey colored
and stains easily.
Non Genetic
attrition: defined as physiological
continous, process resulting in loss of tooth structure from direct frictional forces between contacting teeth. • It occur both on occlusal and
approximal surfaces. • Attrition is accelerated by
parafunctional mandibular movements, especially bruxism.
Abrasion:It refers to the loss of tooth substance induced by mechanical wear other than of mastication.
Localized nonhereditary enamel hypoplasia:Refers to the localized defects in the crown of the portion tooth caused by to injury to ameloblasts during the enamel matrix formation stage.
Localized nonhereditary enamel hypocalcification:Refers to localized defects in the crown of a tooth due to
injury to the ameloblasts during the mineralization stage.
• In these defects, the enamel is normal in structure
but its mineralization is defective.
• The color of lesion varies from chalky to yellow,
brown, dark brown or grayish.