Emmaculate Fields, APRN -CNP
Transcript of Emmaculate Fields, APRN -CNP

OU NeurologyOU Neurology
Emmaculate Fields, APRN-CNPClinical Instructor
Department of NeurologyThe University of Oklahoma Health Sciences Center

OU Neurology
DISCLOSURES’ FINANCIAL DISCLOSURE
’ Nothing to disclose’ UNLABELED/UNAPPROVED USES DISCLOSURE
’ Nothing to disclose
’ Some of the slides have been adapted from teaching materials used at the University of Oklahoma Health Sciences Center
’ Some slides are from the National Stroke Association (denoted NSA)

OU Neurology
LEARNING OBJECTIVESUpon completion of this course, participants will be able to:’ Understand the basics of CT & MR imaging’ Establish an approach to CT interpretation (ABBBC) & MR
interpretation’ Identify differences of pathologic lesions as seen on CT vs MRI

OU Neurology
Poll #1
’ How many Advance Practice Providers( APP’s) are here today?

OU Neurology
Poll #2
How many people in the room work with Advance Practice Providers( APPs) ?

OU Neurology
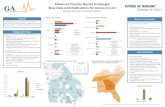
Why incorporate APPs ’Shortage of Neurologist (2012 (11%
shortfall), by 2025 (19% shortfall) ’Outpatient: Decrease waiting times for new
patients & follow-ups visits’ Inpatient: Reduce time burden of hospital
rounding & relieve residents to have protected educational time.

OU Neurology
CT BASICS-densityBlack
Hypodensity Hyperdensity
Fluid/Edema Bone
Air Bullets
Fat Blood
CSF Calcification
Contrast
White

OU Neurology
Isodense things on CT Brain parenchyma
• Brain parenchyma is light gray
• White matter is darkerthan gray matter
Gray matter (cerebral cortex)
Gray matter (basal ganglia)
White matter

OU Neurology
Hypodense things on Ct scan- CSF is very dark, sulci, cisterns & ventricles- Air , nasal cavity, sinuses, mastoid air cells
fat
air
CSF = water

OU Neurology
Hyperdense things on CT- Bone, calcium, acute hemorrhage & contrast
acute blood
ocular lenses
calcifications
contrast (dye)bone
metal (bullets w/streak artifact)

OU Neurology
Approach to reading a CT scan- ABBBC’ A- Air-filled structures (nasal cavity, sinuses,
mastoid air cells)’ B- Bones (fractures)’ B- Blood (subarachnoid, intracerebral, subdural,
epidural hematoma)’ B- Brain tissue (infarction, edema, masses, brain
shift’ C- CSF spaces (sulci, ventricles, cisterns,
hydrocephalus, atrophy)

OU Neurology
Air-filled Structures’ Normal air spaces are black both on bone and brain
window.’ Frontal, maxillary, ethmoid, and sphenoid are air-filled
with no thickening of the mucosa or air fluid level.’ Mastoids are spongy bone filled with tiny pockets of air.
When these pockets are opacified you will see a (gray or white) shade.
’ Air-fluid levels in the setting of trauma suspect a fracture’ Mastoid opacification without trauma indicates
mastoiditis.

OU Neurology
Left maxillary sinus opacification

OU Neurology
B- Bones’ Useful when trauma is suspected’ Window your image for bone reading’ Recognize normal suture structures (usually available
on both sides)’ If fracture suspected, inspect the opposite side for
similar finding. If not present then look for abnormalities associated with the fracture (air/pneumocephalus, black spots with the hemorrhage)

OU Neurology
Fracture
J.F. Talbott, A. Gean, E.L. Yuh, S.I. StiverAmerican Journal of Neuroradiology Oct
2014, 35 (10) 1930-1935; DOI: 10.3174/ajnr.A4001
A, Axial noncontrast CT at the level of the internal capsules demonstrates a left-sided frontoparietal subdural hematoma (arrow). There is also bilateral subarachnoid hemorrhage, diffuse sulcal effacement, left to right midline shift, and near complete effacement of the left lateral ventricle with early trapping of the right lateral ventricle. B, Nondisplaced right occipital calvarial fracture paralleling the ipsilateral lambdoid suture is also identified on the preoperative head CT. A right sided parietal calvarialfracture was also present (not shown). C, Following left-sided decompressive craniectomy, postoperative head CT reveals a large right-sided occipital DEDH in the posterior fossa, adjacent to right-sided occipital bone fracture, with severe mass effect on
the cerebellum and brain stem and effacement of the fourth ventricle.

OU Neurology
B- Brain tissue: Infarction, edema, masses, brain shift’ Evaluate brain for symmetry, neoplasms, infarction
and edema.’ Neoplasms: though hard to visualize on a non contrast CT, mostly
hypodense but can be hyperdense or isodense depending on type and stage, usually with edema surrounding the lesion.
’ Infarction: Hypodense, Look for a hyperdense MCA sign’ Edema: evaluate if associated with a lesion, sulcal effacement. Loss
of gray white differentiation, vasogenic edema usually does not follow vascular territories.

OU Neurology
B- Blood’ Density/age of blood
’ Hyperdense: Acute hemorrhage which is bright white usually < 4 days old’ Isodense: Sub acute Hemorrhage will be same density as the brain usually 4 days to
2 weeks old’ Hypodense: Old hemorrhage will be darker than brain tissue usually > 2-3 weeks
’ Look for any evidence of bleeding:’ Epidural hematoma: over brain convexity, not crossing suture line, lens shaped
(biconvex).’ Subdural hematoma: over brain convexity, interhemispheric, along the tentorium,
SDH will cross suture lines & it’s crescent shaped.’ Intraparenchymal/Intracerebral hemorrhage: within the brain matter, sizes/shape
varies dependent on etiology can be regular or irregular.’ Interventricular hemorrhage- inside ventricles, can be isolated and or secondary to
SAH, ICH.’ Subarachnoid hemorrhage- blood within the subarachnoid spaces (sulci, sylvian
fissure, cisterns). Usually assumes shape of the surrounding cerebral structure.

OU Neurology
C-CSF structures’ C- CSF spaces (sulci, ventricles, cisterns,
hydrocephalus, atrophy)’ Is there any sulcal effacement?’ Are all the cisterns present? ’ Any blood in the cisterns?’ Evaluate size of ventricles, any blood in the ventricles,
compression, shift, and bleeding

OU Neurology
MR BASICS’ Combination of static and dynamic magnetic
fields in conjunction with radiofrequency pulses to create cross-sectional pictures between external magnetic fields and tissues within the patient
’ MRI is an intensity based study vs CT scan which is density (hyperintense vs hyperdense lesion, respectively)’ Hyperintense = increased signal = white’ Hypointense = decreased signal = black

OU Neurology
MRI -advantages’ Quick detection of ischemic changes w/in minutes
(diffusion-weighted MRI sequence)’ MRI is more sensitive for parenchymal lesions, including
infarcts , subacute blood, m’ Superior visualization of posterior fossa (esp. brainstem),
and inferior temporal lobes’ Preferred over CT in children, as there is no use ionizing
radiation’ MRI contrast (gadolinium) less allergic reaction’ Susceptibility-weighted imaging (SWI) MRI sequence, is
most sensitive in detecting small amounts of hemorrhage

OU Neurology
MRI -disadvantages’ Claustrophobia limitations – option open MRI’ Weight limitations’ Critical patients on multiple infusions’ Slower, less accessible- difficult for the very young to be
still for imaging may require sedation’ Fair bone imaging’ Presence of metallic objects(pacemaker, prosthetic heart
valves, aneurysm clips, TENS units, hearing aids/cochlear implants)

OU Neurology
MR with contrast’ Gadolinium useful for evaluation of
’ Tumors’ Infection’ Abscess’ Demyelination disease processes
’ Look for ring enhancing lesions then proceed as follows’ Full/Complete ring- Abscess’ C/Incomplete ring-Opportunistic infections like toxoplasmosis,
Demyelination disease processes’ Look for meningeal enhancement
’ CSF leak’ SAH’ Intracranial hypotension’ Meningitis

OU Neurology
CT/MRI with contrast
http://casemed.case.edu/clerkships/neurology/Web%20Neurorad/brainabscess.htm

OU Neurology
MRI sequences’ DWI acute stroke’ T1 anatomy’ T2 pathology’ FLAIR Like T2 but now CSF is dark’ GRE blood, calcium’ ADCDWI with more diffusion/complement DWI

OU Neurology
VISUALIZING PARENCYMAL EDEMA & BLOOD ON DIFFERENT MRI SEQUENCES
T1 T2 FLAIR DWI
VASOGENIC EDEMA
CYTOTOXIC EDEMA
ACUTE HEME (deoxyHb)
SUBACUTE HEME (metHb)
CHRONIC HEME (hemosiderin)
x 14d
WM
WMGM
WM
WMGM

OU Neurology
DWI- diffusion weighted imaging ’ Dark-CSF’ Bright-cytotoxic edema, necrosis,
abscess’ Ischemic lesions
’ Acute infarctions are white’ Compare to T2 or FLAIR to
distinguish new & old lesions’ Compare to ADC to ensure
infarction is real’ DWI may show lesions due to other
conditions such as seizure or “T2-shine-through” phenomenon

OU Neurology
T1-Good for anatomy evaluation’ Dark-CSF, edema, water, acute
infarction ,gliosis’ Bright- fat, metals,’ Lesions poorly seen without
IV contrast (gadolinium)’ Best used for pre- & post-
gadolinium comparisons

OU Neurology
T2-good for pathology’ CSF is white’ Lesions are white
’ Edema’ Water’ Acute infarction ’ Gliosis
’ Lesions very well seen, but…’ May be difficult to
distinguish lesion and CSF’ Does not visualize very new
infarctions’ Cannot distinguish new and
old lesions

OU Neurology
FLAIR- Fluid-attenuated inversion recovery)- basically like T2 but CSF is dark’ T2-weighted image with
standing water turned black, therefore:’ CSF & old lacunes black
’ Lesions are white’ Edema’ Acute infarction ’ Gliosis
’ Lesions very well seen, but…’ Does not visualize very new
infarctions’ Cannot distinguish new & old
lesions’ Lesions may be inadvertently
erased—compare to T2

OU Neurology
GRE-Gradient Echo
’ Good for looking at brain tissue
’ Great for detecting intraparenchymal blood (black)
’ Parenchyma and nonblood lesions fuzzy

OU Neurology
ADC-Apparent diffusion coefficient’ Bright-CSF, gliosis’ Dark-Infarcts
’ New infarctions are black, confirm that white DWI lesion is truly infarction
’ Hemorrhage may also be black, so must compare to other MR images

OU Neurology
Appearance of intracerebral hemorrhage on non-contrast CT and MRI by stages

OU Neurology
Cerebral amyloid angiopathy as seen on CT/MRI
Image 1 Image 2
Image 3 Image 4 Image 5
• Images 1 and 2 with an acute spontaneous ICH. The CT and MRI images of an 84-year-old woman who presented with a left parietal intracerebral hemorrhage (cortical location). MRI images show the characteristic microbleeds suggestive of CAA as the underlying of spontaneous ICH.
• Image 3, 4, & 5 are MRI images from a 94 year old man who presented with a very small spontaneous left frontal hemorrhage. The gradient recall and susceptibility weighted MR images demonstrated significant microbleeds in bilateral cortical regions indicating CAA as the cause of spontaneous ICH.
Hakimi, R and Garg, A. Imaging of Hemorrhagic Stroke. Continuum, 2016.

OU Neurology
ICH secondary to cerebral venous thrombosis (CVT)
’ CVT is thrombosis of the venous sinuses’ CTB with ICH ’ MR and CT venogram can further aid in diagnosing CVT. ’ While the CT venogram involves administration of iodinated contrast medium, the MR venography
can be performed without the need for contrast using 2D/3D time of flight as well as 2D and 3D phase contrast techniques.
’ Cortical vein thrombosis refers to CVT involving only a small cortical vein vs CSVT to venous or lateral sinus thrombosis, which implies involvement of one of the large cerebral venous sinuses.
’ Pathology–hypercoagulable state(s), for example, postpartum women’ Pathophysiology –cerebral vein occlusions cause venous pressure with:
’ Intracranial hypertension ->ICP (intracranial pressure)’ Blood-brain-barrier disruption leakage of fluid (vasogenic edema) & (hemorrhage) –ICH, SAH
’ Symptoms –headache, seizures, focal deficits (esp. legs, visual fields, aphasia)’ Treatment–full-dose anticoagulation, even with intracranial hemorrhage ’ The appearance of the thrombus on MRI is time specific:
’ Isointense on T1 and hypointense on T2 in the acute phase’ Hyperintense on T1 and T2 in the subacute phase’ Isointense on T1 and hyperintense on T2 in the chronic phase
’

OU Neurology
CVT
https://doi.org/10.1161/CIRCULATIONAHA.111.067835Circulation. 2012;125:1704–1709

OU Neurology
CVT
Anatomy of intracerebral venous system. References: http://www.radiologyassistant.nl/en/p4befacb3e4691/cerebral-venous-thrombosis.html

OU Neurology
CVT ON MRI WITH CONTRAST:DELTA SIGNT1 WITHOUT & WITH GADOLINIUM
Parenchyma: often paramedian, gyral enhancementSinovenous system: G- no flow; G+ delta/empty triangle sign
Sagittal Coronal Coronal
T1 G- T1 G+

OU Neurology
T2
CVT: PARENCHYMAL LESIONS DWI
T1 FLAIR DWI
1. Lack of hyperintense area suggests vasogenic edema2. Hypointense area suggests acute hemorrhage (when
considered with T1 findings)

OU Neurology
Intracranial hemorrhage secondary to cerebral venous thrombosis (CVT)29 year-old woman with a medical history of ulcerative colitis, on immunosuppressive therapy, presented to a referring hospital with new-onset persistent headaches. A non-contrast CT head at that time was unremarkable (Image 1).
Two days later, she was brought in encephalopathic with the same persistent headache. A head CT with and without contrast was performed this time which now showed a large right temporo-parietal intracerebral hemorrhage with significant cerebral edema and a midline shift of 10 mm (Image 2). The contrast enhanced images also showed absence of contrast opacification at the right sigmoid sinus suggestive of CVT as the underlying cause of hemorrhage (Image 3). Patient was transferred to our hospital . A head MRV was also obtained that revealed extensive CVT involving the right internal jugular vein and the right transverse and sigmoid sinuses (Image 4). The patient was treated with heparin despite the presence of ICH (standard treatment). Significant right sided mastoiditis was also noted on the MRI images (Image 5) and hence ENT consult was obtained. It was felt that the mastoiditis was a consequence of CVT in this case rather than the cause, which is more often the case. Despite IV heparin and hypertonic therapy, the cerebral edema failed to improve and her clinical exam deteriorated leading to hemicraniectectomy. Her clinical condition gradually improved and she was later discharged to rehab.
Image 1 Image 2
Image 3
Image 4 Image 5

OU Neurology
NeurocysticercosisA 45-year-old Brazilian man who had recently moved to Europe presented to the emergency department for a severe, drug-resistant headache. Physical, medical, and neurological examination results were unremarkable. A noncontrast head computed tomography scan detected small, scattered intracerebral cysts in the left basal ganglia with a punctate calcification eccentrically along the cyst wall (Figure, A), while other cysts showed no calcification (Figure, B). Brain magnetic resonance imaging (Figure, C and D) showed classic findings of parenchymal neurocysticercosis in the viable stage: small cysts with a mural nodule, representing the eccentrically located cysticercus larva and its scolex.1The cystic fluid appeared clear, cerebral spinal fluid–like, and there were no signs of inflammatory reaction. Diagnostic confirmation was obtained with serology
Cianfoni A, Cina A, Pravatà E, et al. Neurocysticercosis: Still Life in the Brain. Arch Neurol. 2009;66(10):1290–1291. doi:10.1001/archneurol.2009.202

OU Neurology
Neurocysticercosis’ 53 year old Hispanic man,
recently immigrated to US, transferred for SAH evaluation manifested as severe HA.
’ Neurocysticercosis is an intracranial parasitic infection caused by the pork tapeworm, Taenia solium from insufficiently cooked pork containing the encysted larvae or through fecal-oral route.

OU Neurology
References’ Broder J, Preston R. An evidence-based approach to imaging of acute neurological conditions. Emerg Med
Practice 2007; 12:1-28.’ Kremer, P. C., Jolink, W. T., Kappelle, L. J., Algra, A., Klijn, C. M., & null, n. (2015). Risk Factors for Lobar and
Non-Lobar Intracerebral Hemorrhage in Patients with Vascular Disease. Plos ONE, 10(10), 1-10. doi:10.1371/journal.pone.0142338
’ Hemphill, C. et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage. Stroke. 2015 July 46(7): 2032-60
’ van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurology. 2010 Feb; 9(2):167-76 2.
’ Blumenfeld, H. (2010). Neuroanatomy through clinical cases (2nd ed.). Sunderland, Mass.: Sinauer Associates.
’ Perron, A(2005). Blood Can Be Very Bad: CT interpretation for the EM Physician. Foundation for Education and Research in Neurological Emergencies. Retrieved March 1, 2020 from http://www.uic.edu/com/ferne/pdf/acep_2020_peds/perron_ich_acep_2005_peds
’ Perron AD, Huff JS, Ullrich CG, Heafner MD, Kline JA. A multicenter study to improve Emregency Medicine residents’ recognition of intracranial emergencies on computed tomography. Ann Emerg Med. 1998 Nov; 32(5):554-62
’ Ermak, D. M., Cox, L., & Ahmed, A. (2017). Advanced Practice Clinician Training for Neurology. Cureus, 9(4), e1196. doi:10.7759/cureus.1196’ Freeman, W. D., Vatz, K. A., Griggs, R. C., & Pedley, T. (2013). The Workforce Task Force Report. Clinical implications for neurology, 81(5),
479-486. doi:10.1212/WNL.0b013e31829d8783’ Head computed tomography interpretation in trauma: a primer. Broder JS’ Interpretation of Emergency Head CT: A Practical Handbook 1st Edition, Erskine J. Holmes Cambridge University
Press; 1 edition (June 9, 2008)

OU NeurologyOU Neurology