EKG Findings and Arrhythmias
-
Upload
basmah-al-dhafar -
Category
Documents
-
view
219 -
download
0
Transcript of EKG Findings and Arrhythmias
8/6/2019 EKG Findings and Arrhythmias
http://slidepdf.com/reader/full/ekg-findings-and-arrhythmias 1/4
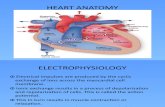
EKG findings and Arrhythmias
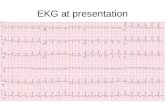
Heart Blocks:
First-degree AV block – normal sinus rhythm with PR interval ³ 0.2ms
Second-degree, type 1 (Weckenbach) block – PR interval elongates from beat to beat until a PR is dropped
Second-degree, type 2 (Mobitz) block – PR interval fixed but there are regular non-conducted P-waves leading
to dropped beats
Third-degree block – no relationship between P waves and QRS complexes. Presents with junctional escape
rhythms or ventricular escape rhythm
Atrial Fibrillation
• The most common chronic arrhythmia
• From ischemia, atrial dilatation, surgical history, pulmonary diseases, toxic syndromes
• Classically, the pulse is irregularly irregular
Signs and Symptoms:
•
Chest discomfort• Palpitations
• Tachycardia,
• Hypotension + syncope
8/6/2019 EKG Findings and Arrhythmias
http://slidepdf.com/reader/full/ekg-findings-and-arrhythmias 2/4
Treatment :
• Control rate with b-blockers, CCB’s, and digoxin (not acutely)
• If fibrillations last >24hr then should anticoagulate with warfarin for at least 3 weeks before
cardioversion (prevents embolisms)
• If you cannot convert to normal sinus rhythm, the patient will require long-term anticoagulation.1st line is warfarin, 2nd line is aspirin
Cardioversion to convert to normal rhythm:
1st line – IV procainamide, sotalol, amiodarone
Electrical à shock of 100-200J followed by 360J
Atrial Flutter
• Less stable than Afib • The rate is slower than that of atrial fibrillation (approximately 250-350bpm)
• Ventricular rate in atrial flutter is at risk of going too fast, thus atrial flutter is considered to be moredangerous (medically slowing this rate can cause a paradoxical increase in ventricular rates)
• Classic rhythm is an atrial flutter rate of 300bpm with a 2:1 block resulting in a ventricular rate of 150bpm
• Signs and symptoms similar to those of atrial fibrillation
• Complications include syncope, embolization, ischemia, heart failure
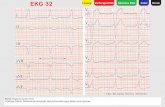
Classic EKG finding is a “sawtooth” pattern:
Treatment :
• If patient is stable, slow the ventricular rate with CCB’s or b-blockers (avoid procainamide because itcan result in increased ventricular rate as the atrial rate slows down)
• If cardioversion is going to take place be sure to anticoagulate for 3 weeks
• If patient is unstable must cardiovert à start at only 50J because is easier to convert to normal sinusrhythm than atrial fibrillation
8/6/2019 EKG Findings and Arrhythmias
http://slidepdf.com/reader/full/ekg-findings-and-arrhythmias 3/4
Multifocal Atrial Tachycardia (MFAT)
• An irregularly irregular rhythm where there are multiple concurrent pacemakers in the atria.
• Commonly found in pts with COPD
EKG shows tachycardia with ³ 3 distinct P waves
Treatment :
• Verapamil
• Treat any underlying condition
Supraventricular Tachycardia
• Many tachyarrhythmias originating above the ventricle
• Pacemaker may be in atrium or AV junction, having multiple pacemakers active at any one time
• Differentiating from ventricular arrhythmia may be difficult if there is also the presence of a bundlebranch block
Treatment :
• Very dependent on etiology
• May need to correct electrolyte imbalance
• May need to correct ventricular rate [digoxin, CCB, b-blockers, adenosine (breaks 90% of SVT)]
• If unstable requires cardioversion
• Carotid massage if patient has paroxysmal SVT
8/6/2019 EKG Findings and Arrhythmias
http://slidepdf.com/reader/full/ekg-findings-and-arrhythmias 4/4
Ventricular Tachycardia
• VTach is defined as ³ 3 consecutive premature ventricular contractions
• If sustained, the tachycardic periods last a minimum of 30s.
• Sustained tachycardia requires immediate cardioversion due to risk of going into ventricular fibrillation
Treatment :
• If hypotensive or no pulse existent do emergency defibrillation (200, then 300, then 360J)
• If patient is asymptomatic and not hypotensive, the first line treatment is amiodarone or lidocainebecause it can convert rhythm back to normal
Ventricular Fibrillation
• Erratic ventricular rhythm is a fatal condition.
• Has no rhyme or rhythm
Signs and Symptoms:
• Syncope
• Severe hypotension
• Sudden death
Treatment :• 1st line – Emergent cardioversion is the primary therapy (200-300-360J), which converts to normalrhythm almost 95% of the time
• Chest compressions rarely work
• 2nd line – Amiodarone or lidocaine
If treatment isn’t given in a timely matter, patient experiences failure of cardiac output and this progresses to
death.