Effect of Storage on Levels of Nitric Oxide Metabolites in Platelet Preparation
-
Upload
ji-won-park -
Category
Documents
-
view
213 -
download
1
Transcript of Effect of Storage on Levels of Nitric Oxide Metabolites in Platelet Preparation
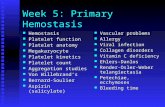
312 Chronic Intermittent Hypoxia Increases 3nitrotyrosine Formation and Enhances the Hypoxic Chemosensory Response of the Rat Carotid Body Esteban A Moya1, Rodrigo Del Rio1, and Rodrigo Iturriaga1 1P Universidad Catolica de Chile. Santiago, Chile. The obstructive sleep apnea syndrome, characterized by chronic intermittent hypoxia (CIH) is recognized as a risk factor for hypertension. A key step in the CIH-induced hypertension is the potentiation of the carotid body (CB) chemosensory responses to acute hypoxia, attributed to an increased level of O2
– in the CB. Since O2
– may react with NO to generate ONOO–, which in turn nitrates tyrosine residues forming 3-nitrotyrosine (3-NT), we studied if the temporal course of the CB chemosensory potentiation correlates with the immunoreactivity levels of 3-NT, endothelial and inducible nitric oxide synthase (eNOS and iNOS) in the rat CB exposed to CIH. The CB chemosensory responses to acute hypoxia were recorded in male Sprague-Dawley rats exposed to CIH (5% O2 for 20 s, 12 times/hr, 8 hrs/day) for 7, 14 and 21 days. The CBs from CIH and sham-rats were fixed in paraformaldehyde 4%, included in paraffin and cut in 5 μm sections for immunohistochemical detection of 3-NT, eNOS and iNOS. We found that 7 days of CIH potentiated the CB chemosensory responses to hypoxia and increased the 3-NT levels in the CB, effects that persisted until 21 days of CIH. In addition, we found a decrease in the eNOS immunoreactivity at 7 days of exposure to CIH, which tended to recover at 21 days of CIH. By contrast, the iNOS immunoreactivity increased at the day 21 of CIH exposure. Our results showed a marked increase of 3-NT in the rat CB, which correlates with the enhanced carotid chemosensory responses to hypoxia, suggesting that 3-NT may contribute to the potentiation through the nitration of tyrosine residues of proteins involved in the chemosensory process. Supported by FONDECYT 1100405 doi: 313 Effect of Storage on Levels of Nitric Oxide Metabolites in Platelet Preparation Ji Won Park1, Barbora Piknova1, and Alan N Schechter1 1NIDDK/NIH, Bethesda Platelets are discoid non-nucleated cells that circulate freely in the plasma and are highly reactive cells that play a pivotal role in hemostasis and thrombosis. Platelet transfusion can be a life-saving therapy when low platelet number or malfunction is a main contributor to bleeding in serious hemorrhagic situations. Due to changes in structure and function, known as the platelet storage lesion (PSL), and possible bacterial contamination, platelet storage is restricted to 5 days. We wish to understand platelet physiology and biochemical changes during storage to improve post-transfusion efficacy and availability of human platelet preparation. Nitric oxide (NO) plays an important role in a number of physiological and pathological processes including anti-platelet activities due to inhibition of platelet adhesion to the vascular endothelium and also direct inhibition of platelet aggregation as a result of increased cGMP production. It has recently been found that NO can be generated by reduction of nitrite as well as by nitric oxide synthase, thus it is reasonable to examine the NO metabolites formed during platelet storage to get information related to transfusion efficacy. In the present study, we monitored three NO metabolites (nitrite, nitrate, and SNO) during storage from day 0 to 8 in platelet rich plasma (PRP), concurrent platelet poor plasma (PPP) and platelet cells obtained by centrifugation of PRP. To examine the effects of oxygen levels on NO metabolites during storage, we compared two types of storage bags which have different gas permeability. Unexpectedly, nitrite leaked into
the stored plasma from both types of bags. The CLX bag, which has higher gas permeability, showed twice as much nitrite at day 6 as the PL1813 bag, which has lower gas permeability. This effect does not seem related to gas exchange or metabolism of the component level. Interestingly nitrate decreased over time in both bags. There was no detectable amount of nitrosylated proteins (SNO) in any group. We hypothesize that changes in the level of nitrite and nitrate during storage might affect post-transfusion activity of platelets and other blood components. doi: 314 Role of Nitrite in Neurovascular Coupling: Possible Nitric Oxiderelated and independent Mechanisms Barbora Piknova1, Ara Kocharyan2, Afonso Silva2, and Alan N Schechter1 1NIH/NIDDK, 2NIH/NINDS Nitric oxide (NO), the most potent vasodilator, also acts as a nontraditional neurotransmitter in the brain. The coupling of blood flow and neuronal activity in the brain in response to various stimuli – so called “neurovascular coupling” - and the exact role of NO is still largely unexplored. It is known that inhibition of neuronal nitric oxide synthase (nNOS) causes uncoupling between neuronal and hemodynamic responses to functional activation of the somatosensory pathway. In our study, using Laser Doppler flowmetry, we followed neurovascular coupling in the somatosensory cortex of rat subjected to forepaw stimulation. We investigated whether topical administration of NO in form of sodium nitroprusside (SNP) or nitrite, by now known to be an NO precursor, restores neurovascular coupling abolished by the nNOS inhibitor 7NI. We found that, after initial decoupling of neuronal and hemodynamic responses to rat forepaw stimulation, SNP, added at physiological concentration, did significantly increase, but not fully restore neurovascular coupling. In contrast, nitrite at its physiological concentration recovered neurovascular coupling to its original level. We tested the nitrite dose response and we found that sub-physiological concentrations were not enough to restore neurovascular coupling, but that supra-physiological concentrations acted mostly as massive local vasodilator without a clear functional response return observed. We are testing several possible mechanisms for how nitrite can affect neurovascular coupling. A possibility is directly through generated NO, either via reaction with heme-containing proteins or with ascorbic acid. A second possibility is that nitrite acts via NO-independent mechanism, such as altering ATP release from erythrocytes. doi: 315 LName and LArginine Differentiatally Ameliorate Cigarette SmokeInduced Emphysema in Mice Karla Maria Pires1, Carlos Rueff-Barroso2, Wagner Pimenta1, Adriana Melo1, Renata Nesi3, Marco Aurelio Silva1, Luis Crsitovao Porto1, and Samuel Santos Valenca3 1Rio de Janeiro State University, 2Fluminense Federal University, 3Rio de Janeiro Federal University Nitric oxide (NO) represents one of the most important intra- and extracellular mediators and takes part in both biologic and pathologic processes. This study aimed to verify the role of NO in pulmonary emphysema induced by cigarette smoke (CS) in a murine model. We compared N-acetylcysteine (NAC), a precursor of glutathione, to G-nitro-L-Arginine-Methyl Ester or L-NAME (LN), which is a NO inhibitor, and to L-arginine (LA), which is a substrate for NO formation. Mice were divided into several
SFRBM/SFRRI 2010S118
10.1016/j.freeradbiomed.2010.10.320
10.1016/j.freeradbiomed.2010.10.321
10.1016/j.freeradbiomed.2010.10.322