Dural Arteriovenous Fistula Treated by Combined Surgical… · 2014. 12. 26. · Loh CT, Almekhlafi...
Transcript of Dural Arteriovenous Fistula Treated by Combined Surgical… · 2014. 12. 26. · Loh CT, Almekhlafi...

Central JSM Neurosurgery and Spine
Cite this article: Loh CT, Almekhlafi MA, Eesa M, Dolati P, Mitha AP (2014) Dural Arteriovenous Fistula Treated by Combined Surgical/Endovascular Ap-proach. JSM Neurosurg Spine 2(6): 1045.
*Corresponding authorAlim P. Mitha, Cerebrovascular/Endovascular/Skull Base Neurosurgeon, Assistant Professor of Clinical Neurosciences and Radiology, Foothills Medical Centre, University of Calgary, 12th Floor, Foothills Medical Centre, 1403-29th Street NW, Calgary Alberta T2N 2T9 Canada, Tel: 403-944-4550; Fax: 403-944-8712; Email:
Submitted: 17 November 2014
Accepted: 20 November 2014
Published: 22 December 2014
Copyright© 2014 Mitha et al.
OPEN ACCESS
Keywords•Brain•Malformation•Angiography•Treatment•Cerebral
Case Report
Dural Arteriovenous Fistula Treated by Combined Surgical/Endovascular ApproachChristopher T. Loh1, Mohammed A. Almekhlafi1,2, Muneer Eesa1,3, Parviz Dolati1,4 and Alim P. Mitha1,3*1Department of Clinical Neurosciences, University of Calgary, Canada 2King Abdulaziz University, Saudi Arabia3Department of Radiology, University of Calgary, Canada 4Brigham and Women’s Hospital, Harvard Medical School, USA
Abstract
Dural arteriovenous fistulas (dAVFs) are unusual vascular lesions that may form because of trauma or sinus thrombosis, but are idiopathic in most cases [1]. Connections between the dural artery and the cortical veins result in the veins being exposed to high pressures, leading to venous hypertension and subarachnoid hemorrhage [2]. Patients may present with pulsatile tinnitus (or pulse-synchronous cephalic bruit), non-specific headaches, vision loss or mental status change [3]. One or several major arteries can supply a dAVF, including the vertebral, basilar, and external (ECA) or internal carotid arteries (ICA) through their dural branches [2]. Given the high risk of bleeding in dAVFs with cortical venous hypertension, treatment of such lesions is indicated. This can be achieved via endovascular occlusion of the fistulous pouch or via open microsurgical disconnection.
In this report, a case is presented in which a patient with a transient speech difficulty was found to have a left sided dAVF with a blind-ending venous sinus pouch and retrograde cortical venous drainage. A combined surgical/endovascular approach resulted in successful and complete embolization.
ABBREVIATIONSdAVFs: Dural Arteriovenous Fistulas; CTA: Computerized
Tomography Angiography; ECA/ICA: External/Internal Carotid Arteries
CASE PRESENTATIONA 74-year-old man presented after a transient episode
of expressive aphasia and dysarthria. Clinically, he was neurologically intact. His workup with CT angiogram (CTA) showed prominent veins in the area of the left transverse sinus suggestive of a left transverse sinus dAVF. A six-vessel digital subtraction angiography (DSA) revealed a high grade left hemispheric fistula, which was supplied by the posterior auricular and occipital branches of the left external carotid artery as well as the tentorial artery of Bernasconi & Cassinari from the left internal carotid artery. It drained into an isolated and dilated venous pouch with significant cortical venous reflux.
At completion of the DSA procedure, he developed Wernicke’s aphasia and left facial twitching. He was felt to have had a focal seizure secondary to cerebral edema of the left hemisphere and potentially triggered by the contrast agent used for the DSA.
He was loaded with phenytoin with gradual resolution of his symptoms.
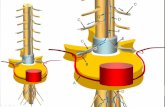
The management options were limited due to the isolated drainage of the fistula precluding transvenous access to the pouch. Transarterial embolization was felt to have a low likelihood of achieving full occlusion of the venous pouch given the large size of the venous pouch, and was also felt to be unsafe because of supply to the dAVF from the ICA. Our preferred method was a combined approach through direct exposure of the ectatic venous pouch surgically followed by direct puncture and coil embolization of the dAVF. Microsurgical disconnection was considered an option, but thought to require a more extensive craniotomy with higher risk complications compared to the combined approach.
A preoperative MRI was done for frameless stereotactic intraoperative navigation. An M33 drill bit was used to create a burr hole right over the venous pouch with the help of the neuronavigation system. A 16-gauge angiocatheter was used for vascular access under direct visualization. Afterwards, a micro catheter was advanced through the angiocatheter and coil occlusion of the venous pouch was achieved using a single

Central
Mitha et al. (2014)Email:
JSM Neurosurg Spine 2(6): 1045 (2014) 2/3
plane fluoroscopy unit. Intraoperative angiography confirmed the complete occlusion of the dAVF. Postoperatively, and the patient demonstrated significant improvement in neurological function and with no further complications. He returned for out-patient follow-up six weeks following the procedure and had no focal neurological complaints at that time. If post-treatment angiography demonstrates complete cure, our typical practice is to perform further non-invasive follow-up studies; we generally reserve conventional angiography for any suggestion of recurrent dAVF. In this patient’s case, a one-year post-surgical MRI brain was performed that demonstrated no evidence of recurrence of his dAVF.
DISCUSSIONDural AVFs account for about 15% of all intracranial
vascular malformations [3]. Some researchers hypothesize that dAVFs can be created from a venous sinus thrombosis via
neovascularization when the dural wall becomes inflamed by the thrombus formation [4]. Others reported on dAVFs shrinking due to venous sinus thrombosis by sinus proliferation of the elastic lamina, intimal thickening or repeated thrombus formation due to turbulent flow form arteries [3]. The natural history of dAVFs is variable and depends on a number of factors. The presence of deep cortical venous drainage, especially those with venous ectasia poses significant risk of hemorrhage [5]. Among those with unruptured dAVFs, presentation with focal neurological deficits increases the annual risk of rupture to 10% [5]. Patients with these high risk features warrant expedited medical assessment and management.
With the recent developments in endovascular and surgical techniques, there are numerous options for treating dAVFs. Via a transarterial approach, embolic agents as Onyx Embolic Liquid System (LES) or n-butyl cyanoacrylate (NBCA) glue have been successfully used to obliterate the fistulous pouch. When
A B C DFigure 1 (A) - CT angiogram maximal intensity projection (MIP) images showing increased vascularity in the superior occipital and posterior auricular
branches of the left temporal region. (B) - Diagnostic catheter angiogram, lateral view showing the dural AVF (circle). (C) - 3D reconstruction of the cerebral angiogram showing the site of entry of the feeding artery.(D) Angiogram of the Left Internal Carotid Artery injections demonstrating the supply through the tentorial artery of Bernasconi & Cassinari.
A B C
Figure 2 Intra-operative angiogram images. (A) -The intravenous catheter in the fistulous pouch (circle).(B) - The coiling microcatheter through the venous catheter is shown with coils deployed into the fistula.(C) - The final angiogram of the left common carotid artery injection showed no residual filling of the fistula.

Central
Mitha et al. (2014)Email:
JSM Neurosurg Spine 2(6): 1045 (2014) 3/3
Loh CT, Almekhlafi MA, Eesa M, Dolati P, Mitha AP (2014) Dural Arteriovenous Fistula Treated by Combined Surgical/Endovascular Approach. JSM Neurosurg Spine 2(6): 1045.
Cite this article
the transarterial approach is not accessible, transvenous coil occlusion of the fistula can be entertained. In our case, all the above options were considered. Due to the fistulous pouch being inaccessible by the transfemoral venous route and because of high risk of embolization through an arterial injection, surgical exposure of the venous pouch through a burr hole using neuronavigation, followed by direct puncture and coil occlusion, was felt to be the most straightforward approach to treatment. There were noted two draining veins emerging from the venous pouch resulting in retrograde reflux. Clipping of these veins, or the venous pouch at the site of the fistula, was entertained as a possible option, but was thought to require a more extensive craniotomy with its associated risks of significant blood loss [6]. Obliterating the venous pouch through an endovascular approach was thought to provide a more direct and durable treatment.
Direct percutaneous puncture of vascular malformations to facilitate endovascular therapy has become a routine procedure. Operators use this approach to facilitate access to otherwise inaccessible carotid-cavernous fistulae or to reach tortuous vascular territories as for stroke thrombectomy. Our report is unique in that surgical exposure of the vascular lesion via a burr whole was used to facilitate the endovascular treatment.
In summary, we report on an unusual case where endovascular
embolization of an inaccessible dAVF was facilitated through burr hole with neuronavigation. This combined surgical-endovascular approach can be useful in selected cases.
REFERENCES1. Barnwell SL, Halbach VV, Dowd CF, Higashida RT, Hieshima GB, Wilson
CB. A variant of arteriovenous fistulas within the wall of dural sinuses. Results of combined surgical and endovascular therapy. J Neurosurg. 1991; 74: 199-204.
2. Spiotta AM, Sivapatham T, Hussain MS, Hui FK, Moskowitz SI, Gupta R. Combined surgical and endovascular approach to a complex dural arteriovenous fistula involving the superior sagittal sinus and torcula. J Stroke Cerebrovasc Dis. 2012; 21: 283-288.
3. Endo S, Kuwayama N, Takaku A, Nishijima M. Direct packing of the isolated sinus in patients with dural arteriovenous fistulas of the transverse-sigmoid sinus. J Neurosurg. 1998; 88: 449-456.
4. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995; 82: 166-179.
5. Gross BA, Du R. The natural history of cerebral dural arteriovenous fistulae. Neurosurgery. 2012; 71: 594-602.
6. Sundt TM Jr, Piepgras DG. The surgical approach to arteriovenous malformations of the lateral and sigmoid dural sinuses. J Neurosurg. 1983; 59: 32-39.