Does platelet-rich plasma promote remodeling of autologous …coimplante.odo.br/Biblioteca/Enxertos...
Transcript of Does platelet-rich plasma promote remodeling of autologous …coimplante.odo.br/Biblioteca/Enxertos...

Does platelet-rich plasma promoteremodeling of autologous bone graftsused for augmentation of the maxillarysinus floor?
Gerry M. RaghoebarJurjen SchortinghuisRobert S. B. LiemJan L. RubenJacqueline E. van der WalArjan Vissink
Authors’ affiliations:Gerry M. Raghoebar, Jurjen Schortinghuis, ArjanVissink, Department of Oral and MaxillofacialSurgery and Maxillofacial Prosthetics, UniversityHospital Groningen, Groningen, the NetherlandsRobert S. B. Liem, Section of Electron Microscopy,Department of Cell Biology, University ofGroningen, Groningen, the NetherlandsJan L. Ruben, Department of Oral Function andProsthetic Dentistry, Dental School, Faculty ofMedical Sciences, University of Groningen,Groningen, the NetherlandsJacqueline E. van der Wal, Department ofPathology, University Hospital Groningen,Groningen, the Netherlands
Correspondence to:G. M. RaghoebarDepartment of Oral and MaxillofacialSurgery and Maxillofacial ProstheticsUniversity Hospital GroningenPO Box 30.0019700 RB GroningenThe NetherlandsTel.: þ31 50 3613840Fax: þ31 50 3611161e-mail: [email protected]
Key words: autologous bone, edentulous maxilla, endosseous implants, platelet-rich
plasma, sinus floor elevation surgery
Abstract: The aim of this study was to evaluate the effect of platelet-rich plasma (PRP) on
remodeling of autologous bone grafts used for augmentation of the floor of the maxillary
sinus. In five edentulous patients suffering from insufficient retention of their upper
denture related to a severely resorbed maxilla, the floor of both maxillary sinus was
augmented with an autologous bone graft from the iliac crest. Randomly, PRP was added to
the bone graft used to augment the floor of the left or right sinus (split-mouth design).
Three months after the reconstruction, bone biopsies were taken with a trephine from the
planned implant sites (N¼30). Subsequently, three implants were placed in the left and
right posterior maxilla. Microradiograms were made of all biopsies (N¼30), whereafter the
biopsies were processed for light microscopic examination. In addition, clinical parameters
were scored. Wound healing was uneventful, clinically no difference was observed between
the side treated with PRP or not. Also microradiographical and histomorphological
examination of the biopsies revealed no statistical difference between the PRP- and non-
PRP side. One implant placed in the PRP side of the graft was lost during the healing phase.
Implant-retained overdentures were fabricated 6 months after implantation. All patients
functioned well (follow-up 20.2 � 4.3 months). In this study, no beneficial effect of PRP on
wound healing and bone remodeling was observed. It is posed that PRP has no additional
value in promoting healing of grafted non-critical size defects.
Implant dentistry is a dynamic field, both
from a scientific and clinical point of view.
Many clinicians are in search for rather
simple pre-implant surgical procedures
that are less inconvenient to the patient,
but possess the ability to create optimal
circumstances for implant placement. Vari-
ous augmentation techniques are in use to
create sufficient bone volume for reliable
insertion of endosseous implants in the
severely resorbed maxilla (Raghoebar
et al. 2001).
Today, reconstruction of the jaws re-
quires transplantation of osteocompetent
cells. These cells are expected to survive,
produce bone, and finally mature into
a functioning bony mandible or maxilla.
Although elevation surgery of the maxil-
lary sinus floor has proven to be a reliable
method with good results, bone healing is
not always predictable and occasionally the
bone volume at the time of placement of
the implants is not sufficient for predict-
able implant placement.
To improve soft-tissue healing and bone
remodeling, platelet-rich plasma (PRP) has
been introduced as a new and potentially
useful adjunct in oral and maxillofacial
bone reconstructive surgery. Platelets play
an important role in wound healing. TheyCopyright r Blackwell Munksgaard 2005
Date:Accepted 20 June 2004
To cite this article:Raghoebar GM, Schortinghuis J, Liem RSB, Ruben JL,van der Wal JE, Vissink A. Does platelet-rich plasmapromote remodeling of autologous bone grafts used foraugmentation of the maxillary sinus floor?Clin. Oral Impl. Res. 16, 2005; 349–356doi: 10.1111/j.1600-0501.2005.01115.x
349

arrive quickly at the wound site and begin
coagulation. They release multiple growth
factors and cytokines involved in wound
healing, including platelet-derived growth
factor, transforming growth factors, vascu-
lar endothelial growth factor, platelet-
derived endothelial cell growth factor, in-
terleukin-1, basic fibroblast growth factor,
and platelet activating factor-4 (Aghaloo et
al. 2002; Weibrich et al. 2002). These
growth factors are thought to contribute
to bone regeneration and to increase vascu-
larity, both of which are considered vital
features of a healing bone graft.
Up to now, only one study has been
reported in the literature evaluating the
effect of PRP on bone density and healing
time following reconstruction of mandibu-
lar continuity defects with autogenous
bone. The authors claimed a 1.62–2.16-
fold increase in bone density when PRP
was added to an autogenous bone graft
(Marx et al. 1998). Although this beneficial
effect has not been proven in other clinical
studies yet, it already has been proposed to
utilize PRP in combination with alloplasts,
xenografts or other non-autogenous mater-
ials, even without combination with a
bone graft (Furst et al. 2003).
Preliminary case reports claim formation
of some osteoid material or bone using
such a technique, but the preliminary re-
sults are not equivocal and sometimes
conflicting (Anitua et al. 1999; Kassolis
et al. 2000; Rosenberg & Torosian 2000;
Shanaman et al. 2001; Vanassche & De-
francq 2001; Froum et al. 2002; Wiltfang
et al. 2003). No scientific conclusions can
be drawn from these preliminary reports.
Additional studies are needed. Therefore,
the aim of this study was to evaluate the
effect of PRP on remodeling of autologous
bone grafts used for augmentation of the
floor of the maxillary sinus.
Patient and methods
Patients
Five consecutive patients referred to the
Department of Oral and Maxillofacial Sur-
gery of the University Hospital, Groningen
because of insufficient retention of their
upper denture related to a severely resorbed
maxilla were selected on basis of the fol-
lowing inclusion criteria:
� severely resorbedmaxilla (classes V–VI,
Cawood & Howell 1991) with reduced
stability and retention of the upper
denture;
� comparable bone height between the
maxillary sinus and top of the maxilla
on both sides;
� class IV bone quality (Lekholm & Zarb
1985);
� edentulous period of at least 1 year;
� no history of radiotherapy in the head
and neck region;
� no history of reconstructive, pre-pros-
thetic surgery or previous oral implant-
ology.
In all patients, two superstructures were
planned supported by three implants to
obtain an optimal aesthetic and phonetic
result (Fig. 1).
Informed written consent to participate
in this study was obtained from all patients
(three women, two men; mean age
58.4 � 1.9 years at time of surgery, range
57–62 years). The patients had been edent-
ulous in the maxilla for 5–12 years. Ortho-
pantomograms, lateral cephalograms, and
postero-anterior oblique radiographs were
made to assess the height of the maxillary
alveolar bone, the dimensions of the max-
illary sinus, and the antero-posterior rela-
tionship of the maxilla to the mandible.
The radiographs were also screened for
sinus pathology. The mean vertical height
of the alveolar bone on the orthopantomo-
gram between the most caudal part of the
maxillary sinus and the oral cavity was in
the premolar and molar 3 � 2mm (range
1–4mm) and 2 � 1 (range 1–3mm), re-
spectively.
Platelet-rich plasma
During the time needed for harvesting bone
from the iliac crest, PRP was made using a
commercially available Platelet Concen-
tration Collection System kit (PCCS kit,
3i Implant Innovations Inc., Palm Beach
Gardens, FL, USA). Before the surgical
procedure, 6ml of anticoagulant citrate
dextrose-A was collected in a 60ml syr-
inge. From the venipuncture the syringe
was filled with whole blood up to 60ml.
Immediately following the whole blood
collection, the blood-filled syringe was in-
verted six times to ensure the anticoagulant
has been evenly dispersed. Using the plate-
let concentration system, the 60ml of
whole blood mixed with coagulant was
processed to a PRP solution. As a control
for the effectiveness of the work-up of PRP,
the transforming growth factor (TGF)-bconcentration of each PRP sample was
measured according to the method de-
scribed by Waarde et al. (1997).
To promote the release of growth factors
from the platelets, 10% calcium chloride
solution and the patient’s serum, as source
of autologous thrombin, were added before
actual reconstruction of the defects with
the bone graft. The resulting gel was mixed
with the bone graft and some gel was
applied at the closure of the wound at the
side reconstructed with the bone graft
mixed with PRP.
To check whether applying a bone graft
mixed with PRP does not result in a sys-
temic rise of the concentration of growth
factors released by platelets making a split-
mouth design less applicable in patients
locally treated with PRP, whole-blood
samples were collected just before applica-
tion of the bone graft mixed with PRP,
immediately after placement of the bone
grafts mixed with PRP and 24h after
surgery.
Surgical protocol
The maxilla of the patients was recon-
structed with autologous anterior medial
iliac crest bone grafts under general an-
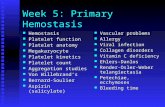
Fig. 1. A 56-year-old female with severe resorption
of the maxilla and mandible. The floor of the
maxillary sinus was augmented with autologous
bone grafts derived from the anterior iliac crest. On
the left side the bone graft was mixed with platelet-
rich plasma. (a) Orthopantomogram showing severe
resorption of the maxilla and mandible. (b) Ortho-
pantomogram 1 year after fabrication of the prosthe-
tic construction. No differences were observed
between the left and the right side.
Raghoebar et al . Platelet-rich plasma and remodeling of bone grafts
350 | Clin. Oral Impl. Res. 16, 2005 / 349–356

esthesia. In all cases, bilaterally a two-stage
procedure (first stage, bone grafting; second
stage, placement of implants) was per-
formed because the height of the maxillary
bone and/or the width of the alveolar crest
were less than 5mm. A bone height of
5mm or more is a prerequisite for implant
placement with sufficient primary stability
(Raghoebar et al. 2001). In addition to
elevation of the floor of the maxillary
sinus, the width of the alveolar crest was
reconstructed too. An osteotomy was pre-
pared in the lateral wall of the maxillary
sinus using the surgical procedure de-
scribed by Raghoebar et al. (2001). After
harvesting of the bone grafts from the iliac
crest, the bone was split into two equal
parts. Randomly, one side was recon-
structed with autologous bone mixed with
PRP gel and one side with autologous bone
only. The floor of the maxillary sinus was
augmented with bone blocks and the re-
maining space occupied by cancellous bone
particles that were obtained by grounding
the graft in a bone mill (Leibingers, Frei-
burg, Germany). Subsequently, placing
monocortico-cancellous bone blocks buc-
cally of the cortex of the alveolar defect
increased the width of the superior alveolar
process. The cancellous side of the bone
graft was in contact with the jawbone and
again cancellous bone particles were used
to fill the small gaps between the bone graft
and the alveolar crest. The grafts were fixed
with titanium screws to the alveolar bone.
PRP gel was applied over the graft at the
PRP side. No membranes were used to
cover the lateral wall defect after the bone
graft was placed. PRP gel was also applied
over the wound after closure with sutures
at the PRP side.
Before harvesting bone grafts, the pa-
tients received broad spectrum antibiotics,
starting 1h preoperatively (intravenously)
and continued orally for 2 days after sur-
gery. Postoperatively, the patients received
a 0.2% chlorhexidine mouth rinse (1min,
five times daily) for 2 weeks. One month
postoperatively, the edentulous patients
were allowed to wear dentures if possible,
after relining them in the operated areas
with a soft liner.
After a healing period of at least 3
months, the implant placement procedure
was performed. A surgical template was
used. Using the template and a trephine
bur (+ 2mm) biopsies were taken in the
region of the canine, the first premolar and
first molar on the same spot as the endoss-
eous implants will be placed (Fig. 2a, c).
The length of the biopsy was the same as
the length of the implant (at least 13mm).
The implants were inserted at the biopsy
locations after widening these holes to
the required dimensions using the standard
burs for the implant system chosen. In all
cases, the bone volume was sufficient. Six
months after insertion, the implants were
uncovered, the oral mucosa was thinned
where applicable and the abutments con-
nected and the prosthetic construction was
fabricated.
Evaluation
The investigators were blinded for both the
clinical and laboratory investigations with
regard to the PRP-treated side. Clinically,
all patients were evaluated according to a
standardized protocol 1, 3, 6 and 12 weeks
after surgery. The clinical protocol in-
cluded assessment of complications during
surgery and postoperative healing (inflam-
mation, wound dehiscence, sequestration,
and loss of bone particles). In addition,
TGF-b concentration of PRP and blood
were measured and the bone biopsies
were studied by microradiography and light
microscopy.
Microradiography
An X-ray source (Philips PW 1730, Eind-
hoven, the Netherlands) was used that
produced monochromatous radiation with
a specific wavelength of 1.537 A. The X-
ray radiation used is Cuka radiation with a
Cu (copper) X-ray tube and a nickel filter.
The wavelength produced is especially
sensitive to be absorbed by calcium. The
biopsies were placed between the 35mm
film (Fuji B&W POS/71337, Rotterdam,
the Netherlands) and the X-ray source and
exposed for 25 s, with a tube charge of
Fig. 2. Bone biopsies and microradiographs of the premolar region 3 months after grafting. (a) Bone biopsy of the platelet-rich plasma (PRP) side. (b) Microradiograph of
the biopsy of the PRP side. (c) Bone biopsy of the non-PRP side. (d) Microradiograph of the biopsy of the non-PRP side.
Raghoebar et al . Platelet-rich plasma and remodeling of bone grafts
351 | Clin. Oral Impl. Res. 16, 2005 / 349–356

25kVand 25mA. Tominimizemagnifica-
tion effects, the distance was kept small
(0.3mm) between the specimen and the
film and large (300mm) between the X-ray
source and the specimen. Film was used
instead of radiographic plates because of a
much higher resolution of the film. After
development of the film with a D-19
developer (Kodak, Amsterdam, the Nether-
lands) for 10min, fixating, rinsing, and
drying, the film was placed on a light
box. A digital image of the biopsy on film
was recorded with a stereo microscope
(Wild/Leitz M7 S, Heerburg, Switzerland)
with a magnification � 10 and a CCD
camera (Teli CS 8310, Tokyo, Japan).
The camera was linked to a personal com-
puter equipped with a framegrabber. The
magnified microradiographs were stored as
images with a size of 640 � 480 pixels
and with a resolution of 256 gray values
ranging from 0 (white) to 256 (black).
Histological examination
Immediately after taking, the biopsies were
fixed in 2% glutardialdehyde in 0.1M
sodium cacodylate buffer, pH 7.4, at 41C
for at least 2 days. During this period,
microradiography of the biopsies was
performed. Subsequently, after rinsing in
0.1M sodium cacodylate buffer, the sam-
ples were dehydrated in a graded con-
centration of ethanol and embedded
in glycolmethacrylate. Two micrometer-
thick serial sections were obtained using a
Jung 1140 autocut microtome with a D-
hard metal knife (Shandon, Life Sciences
International Ltd, Cheshire, UK). The
sections were mounted on glass slide and
stained with toluidine blue and alkaline
fuchsin (Merck, Darmstadt, Germany).
All sections were studied lightmicroscop-
ically on the following items: quality of
bone biopsy, ratio bone–bonemarrow, type
of bone marrow (loose connective tissue,
fibrous, fat), presence of hematopoietic
tissue, presence of bone formation, osteo-
blastic rimming, and presence of bone
resorption.
Histomorphometric analysis of the bi-
opsies was performed using Leica Qwins
image analysis software (Leica Microsys-
tems Image Solutions, Leica, Switzerland).
Under a magnification of � 100 (Leica
DM RA microscope, Leica, Switzerland),
every image field of the histological section
was digitized by a Leica DC 200 digital
camera. Subsequently, the percentage of
bone area was determined in each image
field using the Leica Qwins image analy-
sis software and then averaged. The bone
area in an image field was determined by
setting a threshold to the color of the pixels
of the bone, whose area then could be
measured.
Statistical analysis
The data were analyzed using t-test. A
significance level of 0.05 was chosen.
Results
Clinical assessments
One sinus membrane was perforated dur-
ing surgery. Healing was uneventful and
loss of bone particles through the nose was
not observed. A small incision breakdown
occurred in the first week in one patient in
the non-PRP side. This patient was put on
a regimen of rinsing with a chlorhexidine
mouth rinse four times daily. The dehis-
cence healed within 2 weeks.
A total of 30 implants (length 13 or
15mm, Branemarks, Nobel Biocare, Go-
teborg, Sweden) was placed in augmented
maxillae (Fig. 1). Before the prosthetic
phase, one implant was mobile on the
PRP side and was removed. No other im-
plants were lost during the follow-up
(20.2 � 4.3 months).
Comparison of the clinical features at the
PRP and non-PRP sides revealed no differ-
ences with regard to wound healing, com-
plications during or postsurgery and loss of
implants.
PRP
The procedure for working up whole blood
to PRP resulted in a significant increase in
TGF-b concentration (60.6 � 23.6mg/ml)
when compared with the TGF-b concen-
tration of plasma. The level of TGF-b in
the plasma of the patients before apply-
ing PRP, immediately after applying PRP
and 24h after surgery were 3.4 � 1.5,
3.3 � 1.7 and 3.6 � 2.1 mg/ml, respect-
ively. Thus, the procedure applied did not
result in an increase in the TGF-b concen-
tration in serum.
Microradiography
The microradiographs revealed no statis-
tical difference between the PRP and non-
PRP side (P40.05, t-test) (Fig. 2). The
average density on the microradiographs
(arbitrary gray values) at the first premolar
and first molar region was at the PRP side
91 � 23.1 and 71.8 � 23.8, and at the
non-PRP side 84.6 � 19.6 and 90.7 �13.5, respectively. No density data for
bone biopsies derived from the implant
sites in canine region are given because
light microscopic evaluation had revealed
that these biopsies, in contrast to the biop-
sies taken from the (pre)molar region, lar-
gely consisted of pre-existing bone.
Light microscopy
All except one biopsies were of excellent
quality. In all cases, the bony tissue was
predominantly vital, with just a few small
non-vital parts. No differences were ob-
served between the PRP and the non-PRP
group. The bone–bone marrow ratio ranged
from 50–50% to 40–60%, again not show-
ing a difference between the PRP and the
non-PRP group. The same holds true for
the aspect of the bone marrow, which
contained loose or fibrous connective tis-
sue, or consisted of fat cells. Focally, hema-
topoietic tissue was found. Around the
grafted bone particles, active bone forma-
tion with osteoblastic rimming was seen in
both the PRP and the non-PRP group (Figs
3 and 4). Histomorphometric analysis re-
vealed no differences in areas occupiedwith
bone between PRP- and non-PRP-treated
sides. Again because of the fact that biop-
sies derived from the canine region largely
consisted of pre-existing bone no histomor-
phometric data are given for this region.
The average area occupied by bone in
the augmented (pre)molar region was
41.1 � 8.3% at the non-PRP treated
and 38.4 � 11.3% at the PRP-treated
side (Table 1).
Discussion
Researchers in oral and maxillofacial sur-
gery continuously strive to improve bone-
grafting techniques and to providemeans to
obtain a faster and denser bony regenerate.
This study did not show a significant
increase in bone formation by adding PRP
to an autogenous bone transplant used to
augment the floor of a maxillary sinus and
to increase the width of the alveolar pro-
cess. Although the sample size is small and
Raghoebar et al . Platelet-rich plasma and remodeling of bone grafts
352 | Clin. Oral Impl. Res. 16, 2005 / 349–356

biopsies were taken at insertion of the
implants only (all placed in a grafted area),
some conclusions may be drawn from this
study. The small sample size might have
contributed to the fact that no differences
in remodeling of the grafts between the
PRP- and non-PRP-treated sides were ob-
served, but even no tendency of improved
healing could be shown. An explanation for
the lack of difference between the PRP- and
non-PRP sides might be that the majority
of the bony regeneration takes place within
the first month of healing. This would be
in line with the mode of action of platelet
growth factors. Degranulation and release
of growth factors occurs within 3–5 days
and the growth factor activity may end in
as soon as 7–10 days (Marx 2001; Froum
et al. 2002).
Consistent with the outcome of our
human study, also in animal experiments
no significant differences in wound healing
between autogenous bone and autogenous
bone mixed with PRP were observed 1, 2,
and 4 months after grafting (Aghaloo et al.
2002). The grafting material used in latter
study was cortical membranous bone from
the rabbit cranium, which differs from the
bone used in this study, the latter being
cancellous endochondral bone from the
iliac crest. More recently, Jakse et al.
(2003) published a study in which they
augmented the floor of the maxillary sinus
with autologous bone in sheep, either with
or without PRP. These authors also con-
cluded that the regenerative capacity of
PRP is of quite low potency. Finally Furst
et al. (2004) failed to show an effect of
platelet-released growth factors on bone
regeneration of cortical mandibular defects
in rats. Based on their and our results, we
like to pose that addition of PRP to a bone
transplant used for sinus floor elevation
surgery has apparently no adjuvant clinical
value.
In contrast to the above-mentioned re-
ports, other authors proposed that adding
PRP to bone grafts will result in an increase
the bone density of the reconstructed defect
(Marx et al. 1998; Vanassche & Defrancq
2001). Furthermore, it has been claimed
that platelets can act as local regulators of
fracture repair and bone regeneration (Gru-
ber et al. 2002). Vanassche & Defrancq
included no controls in their study, how-
ever, Marx et al. (1998) showed the bene-
ficial effect of adding PRP in mandibular
continuity defects of 5 cm or greater. Our
study as well as the studies by Aghaloo
et al. (2002) and Jakse et al. (2003) did not
confirm the observation of Marx et al.
(1998) in defects of a lower magnitude.
Therefore, we like to pose that PRP, be-
cause of its effect as local regulators of bone
regeneration, may have a beneficial effect
on bone healing in critical size defects and
defects with compromised vascularization,
while it has no adjuvant value in smaller
defects like in sinus floor elevation surgery.
In the current study, using a very sensi-
tive microradiography method assessing
the density of bone at the implant side,
no differences between the PRP- and non-
PRP sides were observed. Quantitative mi-
croradiography is a commonly used tech-
nique to measure mineral distributions
(calcium, phosphate) and mineral amounts
of carious lesions in enamel and dentin
(Ruben & Arends 1993; de Josselin de
Fig. 3. Histologic examination of the bone biopsy of
Fig. 2a (platelet-rich plasma side). (a) Overview.
Magnification, � 20. (b) Detail of (a) showing
remodeling of bone. Both osteoclast and osteoblast
activity was present around the grafted bone particle.
Osteoblastic rimming is clearly visible on the left
side of the bone particle. Magnification, � 200.
Fig. 4. Histologic examination of the bone biopsy of
Fig. 2c (non- platelet-rich plasma side). (a) Over-
view. Magnification, � 20. (b) Detail of (a) show-
ing remodeling of bone. Osteoblastic rimming is
clearly visible on the right side of the bone particle.
Magnification, � 200.
Table 1. Histomorphometrical analysis ofthe specimen
Patient Non-PRP side PRP side
#1P1 47.8 � 14.5 53.9 � 12.9M1 45.9 � 20.6 52.2 � 5.5
#2P1 57.3 � 11.8 34.7 � 8.8M1 29.6 � 14.4 49.3 � 11.1
#3P1 42.2 � 17.6 33.8 � 22.7M1 36.2 � 13.7 32.3 � 12.6
#4P1 33.1 � 7.5 29.6 � 11.4M1 37.5 � 7.7 46.6 � 15.9
#5P1 47.7 � 21.5 23.8 � 11.4M1 36.7 � 10.5 25.1 � 6
Overall 41.1 � 8.3 38.4 � 11.3
The relative area occupied with bone in the
first premolar (P1) and first molar (M1) region
(%; mean � SD) is given.
PRP, platelet-rich plasma.
Raghoebar et al . Platelet-rich plasma and remodeling of bone grafts
353 | Clin. Oral Impl. Res. 16, 2005 / 349–356

Jong et al. 1987). The technique has also
been used to measure mineral distributions
in bone (Hobson & Beynon 1997; Hobson
1998; Biovin & Meunier 2002). Microradio-
graphy has the advantage over histology that
an image is obtained from the entire speci-
men, making it possible to both locate and
measure areas of bone growth (Schortinghuis
et al. 2003). Although the study by Marx
et al. (1998) reported a 1.62–2.16 times
greater radiographic maturation rate in PRP-
treated reconstruction sites as measured on
panoramic radiographs, in the current study,
using a much more sensitive method no
difference in bone density was observed
between the PRP- and non-PRP sides. This
again supports our hypothesis that PRP has
no adjuvant value in sinus floor elevation
surgery, while it still may have an adjuvant
value in major reconstructive surgery.
With regard to grafting with bone sub-
stitutes, Kassolis et al. (2000) reported
some beneficial effects of the use of PRP.
They used PRP in combination with free-
dried bone allografts in maxillary sinus
floor elevation surgery. Histologic sections
revealed numerous areas of osteoid and
bone formation around freeze-dried bone
allograft particles. Histomorphometry was
not performed and there were no controls.
This makes their results questionable as
in our study; using autogenous bone,
however, we also see proper ostoid and
bone formation in the non-PRP-treated
areas grafted with iliac crest bone. Kassolis
et al. (2000) recognized this flaw in their
experimental setup, as they did not draw
firm conclusions from their study. They
mentioned a need for studies to determine
whether PRP enhances new bone forma-
tion or maturation with allogenic grafts or
not. A recent study indeed indicated that
addition of PRP to grafts of anorganic
bovine bone used for sinus floor elevation
surgery that contained minimal or no auto-
logous bone did not make a significant
difference either in vital bone or in inter-
facial bone contact on the test implants
(Froum et al. 2002). Also, combination of
PRP with bovine hydroxyapatite was not
demonstrably superior to hydroxyapatite
alone (Furst et al. 2003). These are not
surprising observations as PRP acts on
healing capable cells to increase their num-
bers (mitogenesis) and stimulate vascular
ingrowth (angiogenesis) (Marx 2001) that
are not present in acellular bone substi-
tutes. PRP is not osteo-inductive and
must be used in combination with living
bone cells. Therefore, it is unlikely to sig-
nificantly promote bone substitutes and
other non-cellular graft materials.
An effective way to evaluate the effects
of PRP on the formation of bone is to study
the effect in bilateral sinus grafts, with the
addition of PRP being the only controlled
variable. This is the first study to be
performed in this manner with autologous
bone. In our study a beneficial effect of
PRP on bone healing and remodeling could
not be shown. In critical size defects, in
compromised bone after radiotherapy and
in large bony defects, PRP still might have
some value, as has been observed by some
authors in the treatment of such a category
of patients (Marx et al. 1998; Fennis et al.
2002). Furthermore, in the current study
the non-PRP-supported bone graft and
PRP-supported bone graft were left unfunc-
tioned. Implants were placed 3 months
after reconstruction. At that time the grafts
showed comparable signs of remodeling.
This does not exclude a possible beneficial
effect of PRP on early bone healing making
earlier placement of implants after grafting
possible. In such a case, the possible early
enhancing effects of PRP on bone healing
might play a role.
Controlled clinical trials are necessary to
determine whether addition of PRP signifi-
cantly enhances bone formation and ma-
turation or not. Up to now, we like to pose
that PRP has no additional value in pro-
moting healing of grafted non-critical size
defects. As there is a strong clinical poten-
tial associated with supplementing growth
factors in healing wounds, there is a great
need for well-designed studies.
Acknowledgements: Mrs I. R. Zerbo,
Department of Oral Cell Biology, ACTA,
Free University of Amsterdam,
is gratefully acknowledged for her
assistance in the histomorphometry
measurements and Mrs M. A. W. H. van
Waarde is gratefully acknowledged for
measuring the TGF-b concentrations in
blood and PRP.
Resume
Le but de cette etude a ete d’evaluer l’effet du plasma
riche en plaquettes sur le remodelage de greffons
osseux autogenes utilises pour l’epaississement du
plancher sinusal. Chez cinq patients edentes souffr-
ant d’une retention insuffisante de leur prothese
superieure en relation avec unmaxillaire severement
resorbe, les planchers sinusaux des deux maxillaires
ont ete epaissis avec un greffon d’os autogene pro-
venant de la crete iliaque. Au hasard, du plasma
riche en plaquettes (PRP) a ete ajoute au greffon
osseux utilise pour epaissir le plancher du sinus
gauche ou droit (modele de bouche divisee). Trois
mois apres la reconstruction, des biopsies osseuses
ont ete obtenues avec un trepan des sites planifies
pour placer des implants (N¼ 30). Ensuite, trois
implants ont ete places dans les parties maxillaires
gauches et droites. Des microradiogrammes des 30
biopsies ont ete effectuees, ces dernieres ont ensuite
ete utilisees pour l’examen au microscope optique.
De plus, des parametres cliniques ont ete enregis-
tres. La guerison a ete parfaite, cliniquement aucune
difference n’a ete observee entre les sites traites avec
PRP ou sans. L’examen microradiographique et
histomorphologique des biopsies n’a revele aucune
difference significative entre les sites PRP et non-
PRP. Un implant place dans le site PRP du greffon a
ete perdu durant la phase de guerison. Des protheses
retenues sur implants ont ete fabriquees six mois
apres l’insertion des implants. Tous les patients ont
une mise en fonction excellente apres un suivi de
20 � 4,3 mois. Dans cette etude, aucun effet ben-
efique additionnel du PRP sur la guerison et le
remodelage osseux n’a ete observe. Le PRP n’aurait
aucune valeur supplementaire a promouvoir la guer-
ison dans ce type d’operation.
Zusammenfassung
Fordert plattchenreiches Plasma die Remodellier-
ung von autologen Knochentransplantaten, welche
fur die Augmentation des Sinusbodens vom Sinus
maxillaris verwendet werden?
Das Ziel dieser Studie war, den Einfluss von
plattchenreichem Plasma auf die Remodellierung
von autologen Knochentransplantaten, welche fur
die Augmentation des Sinusbodens vom Sinus max-
illaris verwendet wurden, auszuwerten.
Bei 5 zahnlosen Patienten, welche aufgrund einer
stark resorbierten Maxilla uber einen ungenugenden
Halt der Oberkieferprothese klagten, wurde der
Sinusmaxillaris mit autologem Knochen vom Beck-
enkamm augmentiert. Zufallig wurde dem Kno-
chen, der zur Augmentation des rechten oder
linken Sinusbodens verwendet wurde, plattchen-
reiches Plasma (PRP) hinzugefugt (unterschiedlich
behandelte Seiten). Drei Monate nach der Aug-
mentation wurden mittels Hohlfrasen Biopsien an
den geplanten Implantatlokalisationen entnommen
(N¼ 30). Danach wurden je drei Implantate in die
rechte und linke posteriore Maxilla eingesetzt.
Von allen Biopsien wurde Mikrorontgenbilder ange-
fertigt (N¼30), danach wurden die Biopsien fur
die lichtmikroskopische Untersuchung aufgearbei-
tet. Zusatzlich wurden klinische Parameter
aufgenommen.
Die Wundheilung war unauffallig. Klinisch konnten
keine Unterschiede zwischen den mit und ohne
PRP behandelten Seiten beobachtet werden. Ebenso
ergab die mikroradiographische und histomorpho-
Raghoebar et al . Platelet-rich plasma and remodeling of bone grafts
354 | Clin. Oral Impl. Res. 16, 2005 / 349–356

metrische Untersuchung der Biopsien keine
statistisch signifikanten zwischen der PRP und
nicht-PRP Seite. Ein Implantat, welches in eine
PRP Seite eingesetzt worden war, ging wahrend
der Einheilphase verloren. Die implantatgetragenen
Hybridprothesen wurden 6 Monate nach Im-
plantation angefertigt. Alle Patienten funktionierten
problemlos (Beobachtungszeit bis 20.2 � 4.3
Monate).
In dieser Studie konnte kein positiver Einfluss des
PRP auf die Wundheilung und die Knochenremo-
dellierung beobachtet werden. Es wird vermutet,
dass PRP keinen zusatzlichen Effekt bei der Forder-
ung der Heilung von Transplantaten in Defekten
mit nicht-kritischer Grosse hat.
Resumen
La intencion de este estudio fue evaluar el efecto del
plasma rico en plaquetas en el remodelado de injertos
de hueso autologo usado para aumento del suelo del
seno maxilar.
Se aumento el suelo de ambos senos maxilares con
injertos de hueso autologo de la cresta iliaca en 5
pacientes edentulos que padecıan de insuficiente
retencion de su dentadura superior relacionada con
un maxilar severamente reabsorbido. Aleatoria-
mente, se anadio plasma rico en plaquetas (PRP)
al injerto oseo usado para aumentar el suelo del
seno derecho o izquierdo (diseno de boca partida).
Tres meses tras la reconstruccion, se tomaron
biopsias de hueso con un trepano de los lugares
de implantes planificados (N¼30). Subsecu-
entemente se colocaron tres implantes en el
maxilar posterior derecho e izquierdo. Se hicieron
microrradiogramas de todas las biopsias (N¼ 30),
posteriormente las biopsias se procesaron para mi-
croscopıa optica. Ademas se tomaron parametros
clınicos.
La cicatrizacion de la herida tuvo lugar sin
incidentes. Clınicamente no se observo diferencia
alguna entre el lado tratado con PRP o no. Tampoco
el examen microrradiografico e histomorfologico
de las biopsias revelaron diferencias estadıstica-
mente significativas entre los lados con o
sin PRP. Un implante colocado en el lado del
PRP se perdio durante la cicatrizacion. Las
dentaduras implantorretenidas se fabricaron a
los seis meses de la implantacion. Todos los pa-
cientes funcionaron bien (seguimiento de 20.2 �4.3 meses).
En este estudio no se observo ningun efecto bene-
ficioso del PRP sobre la cicatrizacion y sobre el
remodelado oseo. Se plantea que el PRP no tiene
ningun valor adicional en promover la cicatrizacion
de defectos no crıticos injertados.
References
Aghaloo, T.L., Moy, P.K. & Freymiller, E.G. (2002)
Investigation of platelet-rich plasma in rabbit
cranial defects: a pilot study. Journal of Oral
and Maxillofacial Surgery 60: 1176–1181.
Anitua, E. (1999) Plasma rich in growth factors:
preliminary results of use in the preparation of
future sites for implants. International Journal of
Oral & Maxillofacial Implants 14: 529–535.
Biovin, G. & Meunier, P.J. (2002) The degree of
mineralization of bone tissue measured by
computerized quantitative contact microra-
diography. Calcified Tissue International 70:
503–511.
Cawood, J.I. & Howell, R.A. (1991) Reconstructive
preprosthetic surgery. I. Anatomical considera-
tions. International Journal of Oral and Maxillo-
facial Surgery 20: 75–82.
de Josselin de Jong, J.E., ten Bosch, J.J. & Noord-
mans, J. (1987) Optimised microcomputer-guided
quantitative microradiography on dental mineral-
ised tissue slices. Physics in Medicine and Biol-
ogy 32: 887–899.
Fennis, J.P.M., Stoelinga, P.J.W. & Jansen, J.A.
(2002) Mandibular reconstruction: a clinical and
radiographic animal study on the use of auto-
genous scaffolds and platelet-rich plasma. Inter-
national Journal of Oral and Maxillofacial
Surgery 31: 281–286.
Froum, S.J., Wallace, S.S., Tarnow, D.P. & Cho,
S.C. (2002) Effect of platelet-rich plasma on bone
growth and osseointegration in human maxillary
sinus grafts: three bilateral case reports. Interna-
tional Journal of Periodontics & Restorative
Dentistry 22: 45–53.
Furst, G., Gruber, R., Tangl, S., Sanroman, F. &
Watzek, G. (2004) Effects of fibrin sealant protein
concentrate with and without platelet-released
growth factors on bony healing of cortical man-
dibular defects. An experimental study in mini-
pigs. Clinical Oral Implants Research 15:
301–307.
Furst, G., Gruber, R., Tangl, S., Zechner, W., Haas,
R., Mailath, G., Sanroman, F. & Watzek, G.
(2003) Sinus grafting with autogenous platelet
rich plasma and bovine hydroxyapatite. Clinical
Oral Implants Research 14: 500–508.
Gruber, R., Varga, F., Fischer, M.B. & Watzek, G.
(2002) Platelets stimulate proliferation of bone
cells: involvement of platelet derived growth fac-
tor, microparticles and membranes. Clinical Oral
Implants Research 31: 529–535.
Hobson, R.S. (1998) A pilot study of mineraliza-
tion distribution in the cortical bone of the
human mandible. Archives of Oral Biology 43:
633–639.
Hobson, R.S. & Beynon, A.D. (1997) Preliminary
quantitative microradiography study into the dis-
tribution of bone mineralization within the basal
bone of the human edentulous mandible. Arch-
ives of Oral Biology 42: 497–503.
Jakse, N., Tangl, S., Gilli, R., Berghold, A., Loren-
zoni, M., Eskici, A., Haas, R. & Pertl, C. (2003)
Influence of PRP on autologous sinus grafts. An
experimental study on sheep. Clinical Oral Im-
plants Research 14: 578–583.
Kassolis, J.D., Rosen, P.S. & Reynolds, M.A. (2000)
Alveolar ridge and sinus augmentation utilizing
platelet-rich plasma in combination with freeze-
dried bone allograft: case series. Journal of Perio-
dontology 17: 1654–1661.
Lekholm, U. & Zarb, G.A. (1985) Patient selection
and preparation. In: Branemark, P.I., Zarb, G.A.
& Albrektsson, T., eds. Tissue-Integrated Pros-
theses: Osseointegration in Clinical Dentistry.
1st edition, 199–209. Chicago: Quintessence.
Marx, R.E. (2001) Platelet-rich plasma (PRP): what
is PRP and what is not PRP. Implant Dentistry
10: 225–228.
Marx, R.E., Carlson, E.R., Eichstaedt, R.M., Schim-
mele, S.R., Strauss, J.E. & Georgeff, K.R. (1998)
Platelet-rich plasma: growth factor enhancement
for bone grafts. Oral Surgery Oral Medicine Oral
Pathology Oral Radiology and Endodontics 85:
638–646.
Raghoebar, G.M., Timmenga, N.M., Reintsema,
H., Stegenga, B. & Vissink, A. (2001) Maxillary
bone grafting for the insertion of endosseous im-
plants: results after 12–124 months. Clinical Oral
Implants Research 12: 279–286.
Rosenberg, E.S. & Torosian, J. (2000) Sinus grafting
using platelet-rich plasma initial case presenta-
tion. Practical Periodontics and Aesthetic Den-
tistry 12: 843–850.
Ruben, J. & Arends, J. (1993) Shrinkage prevention
of in vitro demineralized human dentine in trans-
verse microradiography. Caries Research 27:
262–265.
Schortinghuis, J., Ruben, J.L., Meijer, H.J.A.,
Bronckers, A.L.J.J., Raghoebar, G.M. & Stegenga,
B. (2003) Microradiography to evaluate bone
growth into a rat mandibular defect. Archives of
Oral Biology 48: 155–160.
Raghoebar et al . Platelet-rich plasma and remodeling of bone grafts
355 | Clin. Oral Impl. Res. 16, 2005 / 349–356

Shanaman, R., Filstein, M.R. & Danes-Meyer, M.J.
(2001) Localized ridge augmentation using GBR
and platelet-rich plasma: case reports. Interna-
tional Journal of Periodontics & Restorative
Dentistry 21: 345–355.
Vanassche, B. & Defranq, J. (2001) Use of PRP
(platelet rich plasma) in bone volume aug-
mentation. Revue Belge de Medicine Dentaire
56: 125–133.
Waarde, M.A.W.H., van Assen, A.J., van Kampinga,
H.H., Konings, A.W.T. & Vujaskovic, Z. (1997)
Quantification of transforming growth factor-beta
in biological material using cells transfected with a
plasminogen activator inhibitor-1 promoter-lucifer-
ase construct. Analytical Biochemistry 247: 45–51.
Weibrich, G., Kleis, W.K.G., Hafner, G. & Hitzler,
W.E. (2002) Growth factor levels in platelet-rich
plasma and correlations with donor age, sex, and
platelet count. Journal of Cranio-Maxillofacial
Surgery 30: 97–102.
Wiltfang, J., Schlegel, K.A., Schultze-Mosgau, S.,
Nkenke, E., Zimmerman, R. & Kessler, P.
(2002) Sinus floor augmentation with b-trical-ciumphosphate (b-TCP): doed platelet-rich plasma
promote its osseous integration and degrada-
tion. Clinical Oral Implants Research 14:
213–218.
Raghoebar et al . Platelet-rich plasma and remodeling of bone grafts
356 | Clin. Oral Impl. Res. 16, 2005 / 349–356