Disruption of Wnt/b-Catenin Exerts Antileukemia Activity ... · mutations (FLT3-TKD), are...
Transcript of Disruption of Wnt/b-Catenin Exerts Antileukemia Activity ... · mutations (FLT3-TKD), are...

Cancer Therapy: Preclinical
Disruption of Wnt/b-Catenin Exerts AntileukemiaActivity and Synergizes with FLT3 Inhibition inFLT3-Mutant Acute Myeloid LeukemiaXuejie Jiang1,2, Po Yee Mak1, Hong Mu1,Wenjing Tao1, Duncan H. Mak1,Steven Kornblau1, Qi Zhang1, Peter Ruvolo1, Jared K. Burks1,Weiguo Zhang1,Teresa McQueen1, Rongqing Pan1, Hongsheng Zhou1,2, Marina Konopleva1,Jorge Cortes3, Qifa Liu2, Michael Andreeff1, and Bing Z. Carter1
Abstract
Purpose:Wnt/b-catenin signaling is required for leukemic stemcell function. FLT3 mutations are frequently observed in acutemyeloid leukemia (AML). Anomalous FLT3 signaling increasesb-catenin nuclear localization and transcriptional activity. FLT3tyrosine kinase inhibitors (TKI) are used clinically to treat FLT3-mutated AML patients, but with limited efficacy. We investigatedthe antileukemia activity of combined Wnt/b-catenin and FLT3inhibition in FLT3-mutant AML.
Experimental Design: Wnt/b-catenin signaling was inhibitedby the b-catenin/CBP antagonist C-82/PRI-724 or siRNAs, andFLT3 signaling by sorafenib or quizartinib. Treatments on apo-ptosis, cell growth, and cell signaling were assessed in cell lines,patient samples, and in vivo in immunodeficient mice by flowcytometry, Western blot, RT-PCR, and CyTOF.
Results:We found significantly higher b-catenin expression incytogenetically unfavorable and relapsed AML patient samplesand in the bone marrow–resident leukemic cells compared with
circulating blasts. Disrupting Wnt/b-catenin signaling suppressedAML cell growth, induced apoptosis, abrogated stromal protec-tion, and synergized with TKIs in FLT3-mutated AML cells andstem/progenitor cells in vitro. The aforementioned combinatorialtreatment improved survival of AML-xenografted mice in twoin vivo models and impaired leukemia cell engraftment. Mech-anistically, the combined inhibition of Wnt/b-catenin and FLT3cooperatively decreased nuclear b-catenin and the levels of c-Mycand other Wnt/b-catenin and FLT3 signaling proteins. Impor-tantly, b-catenin inhibition abrogated the microenvironmentalprotection afforded the leukemic stem/progenitor cells.
Conclusions:DisruptingWnt/b-catenin signaling exerts potentactivities against AML stem/progenitor cells and synergizes withFLT3 inhibition in FLT3-mutant AML. These findings provide arationale for clinical development of this strategy for treatingFLT3-mutated AML patients. Clin Cancer Res; 24(10); 2417–29.�2018AACR.
IntroductionWnt signaling plays essential roles in regulating cell prolifer-
ation, survival, and differentiation. Activation of canonical Wntsignaling stabilizes b-catenin, resulting in its nuclear translocationand increased interactions with cotranscriptional regulator T-cellfactor (TCF) 4/lymphoid enhancer factor 1 (1). Deregulation ofWnt/b-catenin signaling is linked to acute myeloid leukemia(AML) initiation and progression (2) and is required for leukemiastem cells' (LSC) self-renewal and survival (3). Overexpression of
b-catenin was reported to be an independent adverse prognosticfactor for AML (4). In fact, b-catenin was found to be over-expressed in most AML samples and localized more frequentlyin the nucleus of bone marrow (BM) LSC compared with normalCD34þ cells (5). Thus, inhibition of b-catenin signaling repre-sents a promising therapeutic strategy in AML (6, 7).
FMS-like tyrosine kinse-3 (FLT3) mutations, including inter-nal tandem duplication (FLT3-ITD) and tyrosine kinase domainmutations (FLT3-TKD), are frequently observed in AML (8).These mutations cause ligand-independent activation of thetyrosine kinase and downstream signaling pathways, includingMAPK/ERK, JAK/STAT5, and PI3K/AKT, which in turn activatecanonical Wnt signaling by stabilizing and increasing nuclearlocalization and transcriptional activity of b-catenin (9). Fur-thermore, aberrant b-catenin signaling contributes to FLT3-ITD–
related myeloid transformation by TCF-dependent transcription-al activity, and FLT3 mutations also directly cooperate with Wntsignaling in AML (10).
FLT3mutations are associatedwith poor prognosis in AML (11,12). Consequently, FLT3 tyrosine kinase inhibitors (TKI) havebeen developed to treat AML patients with FLT3 mutations.Unfortunately, their effects are often limited because of acquiredFLT3 mutations, TKI-induced alternative signaling activation,microenvironment-mediated resistance, and their inability to
1Section of Molecular Hematology and Therapy, Department of Leukemia, TheUniversity of Texas MD Anderson Cancer Center, Houston, Texas. 2Departmentof Hematology, Nanfang Hospital, Southern Medical University, Guangzhou,Guangdong, China. 3Department of Leukemia, The University of Texas MDAnderson Cancer Center, Houston, Texas.
Note: Supplementary data for this article are available at Clinical CancerResearch Online (http://clincancerres.aacrjournals.org/).
Corresponding Authors: Michael Andreeff and Bing Carter, The University ofTexas MD Anderson Cancer Center, 1515 Holcombe Boulevard, Unit 448, Hous-ton, TX 77030-4009. Phone: 713-792-7261 and 713-794-4014; Fax: 713-794-1903; E-mail: [email protected]; and [email protected]
doi: 10.1158/1078-0432.CCR-17-1556
�2018 American Association for Cancer Research.
ClinicalCancerResearch
www.aacrjournals.org 2417
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

eradicate LSC (13, 14). Thus, strategies to improve the efficacy ofTKIs are needed for the therapy of FLT3-mutated AML.
Disrupting Wnt/b-catenin signaling may target AML and LSC/progenitor cells and has the potential to enhance the activity ofTKIs in FLT3-mutated AML. C-82 is a b-catenin specific inhibitorthat binds to CBP, inhibits b-catenin/CBP interaction, andimpedes Wnt/b-catenin–mediated cell proliferation, self-renew-al, and survival in several hematologic malignancies, includingALL and CML (15–17). However, the antileukemia activity of C-82 in AML, including the effects on AML stem/progenitor cellsand the combinations of C-82 with TKIs in FLT3-mutated AML,has not been investigated. In this study, we investigated theeffects of C-82 on AML and LSC/progenitor cells and its com-binatorial activity when paired with the FLT3-ITD–directed TKIsorafenib or quizartinib. We demonstrate that C-82 exertedpotent activity against AML cells and LSC and synergized withTKIs in FLT3-mutated AML in vitro and in vivo.
Materials and MethodsProtein determination by reverse-phase protein array
Expression of b-catenin protein in samples from newly diag-nosed AML patients and paired newly diagnosed and relapsed orpaired peripheral blood (PB) and BM samples in AML patientswere determined by reverse-phase protein array (RPPA) as previ-ously described (18). The patient populations, clinical character-istics, and sample preparation for RPPAwere described previously(19). Antibody against b-catenin (#8480)was fromCell SignalingTechnology.
Cells and cell cultureMolm13 cells were purchased from the German Collection of
Microorganisms and Cell Cultures, and MV4-11 and KG-1 cellsfrom the American Type Culture Collection. OCI-AML3 cells wereprovided byDr.M.Minden (OntarioCancer Institute). Ba/F3 (Ba/F3-WT) or Ba/F3 cells stably transfected with human FLT3-ITD
(Ba/F3-ITD), FLT3-D835G (Ba/F3-D835G), or D835Y (Ba/F3-D835Y) point mutations as previously described (20) were pro-vided by Dr. D. Small (Johns Hopkins University School ofMedicine, Baltimore, MD). Ba/F3 cells with FLT3-ITD plusN676D (Ba/F3-ITDþ676) or Y842C mutation (Ba/F3-ITDþ842)were generated as previously described (21). Cell lines werevalidated by STR DNA fingerprinting using the AmpF_STR Iden-tifier Kit according to the manufacturer's instructions (AppliedBiosystems, Cat #4322288). The STR profiles were comparedwithknown ATCC fingerprints, and to the Cell Line Integrated Molec-ular Authentication database (CLIMA) version 0.1.200808(http://bioinformatics.hsanmartino.it/clima/; ref. 22). The STRprofiles matched known DNA fingerprints or were identified asunique (OCI-AML3).Mycoplasma testingwas performed using thePCRMycoplasmaDetectionKit fromAppliedBiologicalMaterialsper manufacturer's instructions. Authenticated and mycoplasma-free cells are stored under liquid nitrogen and are never kept inculture formore than4months. Cellswere cultured inRPMI-1640supplemented with 10% heat-inactivated fetal calf serum,2 mmol/L L-glutamine, 100 U/mL penicillin, and 100 mg/mLstreptomycin. Ba/F3-WT cells were supplemented with 2 ng/mLmurine interleukin-3 (PeproTech, Inc.).
Primary samples were obtained after informed consent follow-ing the MD Anderson Cancer Center Institution Review Boardapproved protocols in accordance with Declaration of Helsinki.Mononuclear cells were purified by Ficoll–Hypaque (Sigma-Aldrich) density-gradient centrifugation and cultured in a-MEMsupplemented with 10% fetal calf serum. Table 1 summarizespatient clinical characteristics.
Gene silencing by siRNAMolm13 and MV4-11 cells were electroporated with 750
nmol/L of 4 individual or SMARTpool ON-TARGET plusCTNNB1 siRNAs of the four (Dharmacon) using an Amaxaapparatus (Solution L, program Q-001; Lonza) following themanufacturer's instructions. b-Catenin silencing was confirmedby Western blot analysis.
Cell viability and apoptosis assayBa/F3 cells (1 � 105 cells/mL), AML cell lines (2 � 105 cells/
mL), and primary samples (5 � 105 cells/mL) were plated in 96-well plates with or without BM-derived mesenchymal stem cell(MSC) coculture and treated with C-82, sorafenib (AmericanCustom Chemicals Corporation), or quizartinib (Selleck Chemi-cals), or their combination. Cell viability was determined by theTrypan blue exclusion using a Vi-Cell XR Cell Counter (BeckmanCoulter). Apoptosis was estimated by flow cytometry afterannexin V–Cy5.5 staining in the presence of 7-amino-actinomy-cin D (7-AAD). Apoptosis in primary samples was assessed inCD45þ andCD34þCD38� cells after the cellswere incubatedwithCD34-PC5.5, CD38-PE Cy7, and CD45-APC H7 antibodies (BDBiosciences). Specific apoptosis was defined as:
%of apoptosis in treated cells�%of apoptosis in untreated cells%of visible untreated cells
� 100%
Cell-cycle distributionCells (1� 106) were exposed to 10 mmol/L EdUrd (Invitrogen)
in a culture medium for 2 hours, fixed in 4% formaldehyde, andprocessed with the Click-iT EdU Alexa Fluor 647 flow cytometry
Translational Relevance
Aberrant Wnt/b-catenin signaling is associated with AMLpathogenesis and required for leukemic stem cell survival andfunction. FLT3 is frequently mutated in AML and associatedwith poor prognosis. Anomalous FLT3 signaling furtherincreases b-catenin signaling activity. FLT3 TKIs have beendeveloped to treat AML patients with FLT3 mutations, butacquired FLT3 mutations, TKI-induced alternative signalingactivation, microenvironment-mediated resistance, and inac-tivity against leukemia stem cells limit their efficacy. This studydemonstrates that inhibition of Wnt/b-catenin signaling tar-gets AML cells, including stem/progenitor cells. Combinedinhibition ofWnt/b-catenin and FLT3 cooperatively decreasednuclear b-catenin and the levels of Wnt/b-catenin, and FLT3signaling proteins, and synergistically induced cell death invitro and in vivo in twomurine models andmarkedly impairedleukemia cell engraftment. These findings provide a mecha-nistic rationale for the clinical development of this combina-torial strategy for treating FLT3-mutated AML patients, aprocess that also targets successfully bone marrow microen-vironment protected leukemia stem/progenitor cells.
Jiang et al.
Clin Cancer Res; 24(10) May 15, 2018 Clinical Cancer Research2418
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

assay kit (Thermo Fisher Scientific) following the manufacturer'sinstructions. After cells were treated with RNase and counter-stained with 10 mg/mL propidium iodide (Sigma-Aldrich), DNAcontent was determined by flow cytometry (Beckman Coulter).Cell-cycle distribution was analyzed using the Kaluza software(Beckman Coulter).
Western blot analysisProtein levels were determined by Western blot as described
previously (23) using the Odyssey Infrared Imaging System andthe signals quantified by Odyssey software version 3.0 (LI-CORBiosciences). Protein expression was normalized to the loadingcontrol. Cytoplasmic and nuclear fractions were isolated as pre-viously described (24). Antibodies against b-catenin (#8480),phospho (p)-FLT3 (Tyr589/591; #3464), p-ERK (Thr202/Tyr204;#4376), p-AKT (Ser473; #4058), AKT (#4685), c-Myc (#5605),STAT5 (#94205), and CD44 (#5640) were from Cell SignalingTechnology; ERK2 (#sc-154) and FLT3 (#sc-479) from Santa CruzBiotechnology; survivin (#AF886) from R&D Systems; p-STAT5(pY694; #611965) from BDBiosciences. b-Actin,a-tubulin (bothfrom Sigma-Aldrich), or Lamin B1 (Cell Signaling Technology)was used as a loading control.
Protein determination by flow cytometryCells were incubated with LIVE/DEAD Fixable Yellow Dead
Cell Stains (Thermo Fisher Scientific) for 30 minutes in the dark,fixed with 4% paraformaldehyde, and permeabilized with0.115% Triton X-100 in PBS. Cells were then stained with Fc-blocker (Miltenyi Biotec) at 4�C for 10 minutes, followed withCD34-PC5.5, CD38-APC (BD Biosciences), CD44-BV421 (Bio-Legend) and survivin-FITC (R&D Systems) antibodies and resus-pended in 0.1% paraformaldehyde in PBS and analyzed using aGallios flow cytometer (Beckman Coulter). Survivin and CD44levels were expressed as the mean fluorescence intensity (MFI)difference of cells stained with the target antibodies and stainedwith IgG.
Confocal immunofluorescence microscopyCells were mounted onto slides, fixed with 4% paraformalde-
hyde, and permeabilized with 100% methanol. After cells wereincubated with blocking solution (1% BSA/PBS), mouse anti-human CD44 and rabbit anti-human b-catenin monoclonal
antibodies (Cell Signaling Technology) were added (1:200). Cellswere washed, and secondary antibodies (Alexa 594-tagged don-key anti-mouse and Alexa 488-tagged donkey anti-rabbit; LifeTechnologies) were added. Cells were stained with 406-diami-dino-2-phenylindole (DAPI, Thermo Fisher Scientific). Single,central cellular plane, confocal images were collected using anOlympus FV1000 laser confocal microscope. Images were cap-tured using the Olympus TIRF 100 � 1.45 NA objective at thecentral plane of the cell as determined by the DAPI label. Imageswere loaded into 3I's Slidebook Software (v5.5, Intelligent Imag-ing Innovations). In Slidebook, cellular masking was performedto identify the nuclear and cytoplasmic space. All collected chan-nels were used to create the whole cell mask and the DAPI markerwas used to create the nuclear mask with the focal z resolution at�0.3 mm.While multiple z-planes were not captured, any proteincoexpressing (colocalizing)withDAPIwould be determined to belocated in the nucleus. By subtracting the nuclear mask from thewhole cell mask, the cytoplasmic mask was created. The meanintensity for each marker was quantified in each mask (nuclear,cytoplasmic, and whole cell) by SlideBook imaging software andcompared to determine the amount of nuclear accumulation.
Real-time RT-PCRRNA isolation and RT-PCR were performed as previously
described (25) with minor modifications. The PCR amplificationmixture (20 mL) contained cDNA, a primer pair of human Wntsignaling primer library for pathway PCR array (Real Time Primer,LLC), and SYBR Green PCR fast master mix (Thermo FisherScientific). The abundance of each transcript relative to that ofB2M was calculated using the 2�DCt method, where DCt is themeanCt of the transcript of interestminus themeanCt of the B2Mtranscript.
AdhesionAdhesion of leukemia cells to MSCs was determined as previ-
ously described (25). Briefly, leukemia cells were added to MSCsthat were plated the night before and cultured for 24 hours.Floating and attached leukemia cells were counted by flow cyto-metry after staining the cells with human CD45 antibody in thepresence of counting beads (Life Technologies). Adhesion ofleukemia cells was defined as attached viable CD45þ cells/totalviable leukemia cells.
Table 1. Characteristics of AML patients and experiments
Pt No Source % Blasts Disease status FLT3 status Cytogenetic Experiments
1 PB 90 New diagnosis WT 46,XY C-822 PB 70 New diagnosis ITD 46,XY C-823 PB 93 Relapse/refractory WT Complex karyotype C-824 PB 74 Relapse/refractory WT Complex karyotype C-825 PB 84 Relapse/refractory WT Complex karyotype C-826 BM 74 Relapse/refractory WT Complex karyotype C-827 PB 78 Relapse/refractory WT Complex karyotype C-8214 BM 52 Primary refractory ITD þ D835 47,XY, þ9 C-82 þ TKI15 BM 74 New diagnosis D835 47,XY,inv(16),þ22,del(7) C-82 þ TKI16 PB 56 Relapse/refractory ITD 46,XY C-82 þ TKI17 BM 83 Relapse D835 46,XY C-82 þ TKI18 PB 52 New diagnosis D835 46,XY C-82 þ TKI19 PB 72 Relapse/refractory D835 46,XY C-82 þ TKI20 BM 61 Relapse WT 46,XX C-82 þ TKI21 BM 60 New diagnosis WT 46,XX C-82 þ TKI22 BM 97 Relapse WT 46,XY, t(1;3), del(7) C-82 þ TKI23 BM 78 Relapse/refractory ITD 46,XY Mouse experiments
Abbreviation: Pt No, patient number.
Wnt/b-Catenin Signaling Inhibition in AML
www.aacrjournals.org Clin Cancer Res; 24(10) May 15, 2018 2419
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

In vivo studiesAnimal experiments were performed in accordance with the
MD Anderson Cancer Center Institutional Animal Care and UseCommittee approved protocols. Molm13 cells (5 � 105) stablyexpressing a dual luciferase-GFP reporter (Molm13-GFP/Luc)were injected into NOD/SCIDIL2RgNull (NSG) mice, and cellsfrom a FLT3-ITD–mutated AML patient (no. 23, Table 1; 2� 106)collected from spleen of second generation patient-derived xeno-graft (PDX) inNOD/SCIDIL2RgNull-3/GM/SF (NSGS)micewereinjected into NSGS mice via tail vein (both 6–8-week-old,females; The Jackson Laboratory). After confirming engraftmenteither by imaging using the IVIS-200 noninvasive biolumines-cence in vivo imaging system (Xenogen) or by flow cytometrymeasuring human CD45þ cells in mouse PB, mice were random-ized to the following treatment groups (n ¼ 10/group): vehiclecontrol, PRI-724 (C-82 prodrug; 40 mg/kg) by subcutaneousminipump, sorafenib (5 mg/kg for NSG and 10 mg/kg for NSGSmice) by daily oral gavage, or PRI-724 plus sorafenib for 4 weeks.Three mice/group were killed 2 hours after dosing on 15th forNSGand25th forNSGSmice of treatment days. Leukemia burdenwas assessed by flow cytometry, CyTOF mass cytometry, or H&Estaining. Mice were monitored daily and survival time wasrecorded.
NSGSmice (7- to 8-week-old, females; The Jackson Laboratory)were also injected via tail veinwith the PDX cells (no. 23, Table S1;2� 106) untreated or after ex vivo treatment with C-82 (1.0 mmol/L), sorafenib (2.5 mmol/L), or both for 48 hours (n ¼ 6/group).Leukemia cell engraftment and progression were assessed by flowcytometry, and survival was monitored.
CyTOFBM cells from mice were labeled with metal-tagged antibo-
dies for cell surface and intracellular proteins (SupplementaryTable S1) and analyzed using a CyTOF Helios mass cytometer(Fluidigm; refs. 25, 26). The viable cells were gated with FlowJosoftware (TreeStar Inc.) and exported. The exported FCS fileswere transferred into the spanning-tree progression analysis ofdensity-normalized events (SPADE) software and analyzed asreported previously (27, 28).
Statistical analysesCell line experiments were conducted in triplicates. Results
were expressed as means � SEM unless otherwise stated. Thecombination index (CI) was determined by the Chou–Talalaymethod and expressed as the mean of CI values obtained at the50%, 75%, and 90% effective doses (29). CI<1.0 was consideredsynergistic; 1.0, additive; >1.0, antagonistic. Statistical analyseswere performed using a two-tailed Student t test or one-wayanalysis of variance (ANOVA) for multiple group comparisons.Mouse survival was estimated by the Kaplan–Meier method andanalyzed using log-rank statistics. P < 0.05 was defined as statis-tically significant.
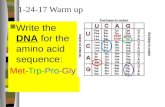
ResultsHigh b-catenin expression is associated with unfavorablepatient characteristics in AML and induced by the BMmicroenvironment
Using RPPA, we determined the expression of b-catenin in 511newly diagnosed AML patient samples. We found that high levelswere associated with unfavorable cytogenetics (P < 0.01), and the
b-catenin level was significantly higher in relapsed comparedwithpaired newly diagnosed samples (n ¼ 47, P ¼ 0.043; Supple-mentary Fig. S1A). Higher b-catenin expression was observed inBM than in paired PB samples (n ¼ 140, P ¼ 0.0006; Supple-mentary Fig. S1B), suggesting that the BM microenvironmentmodulates b-catenin expression in AML cells. Consistent withthis observation, coculturing OCI-AML3 cells with MSCs (48hours) induced the expression of b-catenin and its target, theadhesion protein CD44 in leukemia cells, while inhibition ofb-catenin with Wnt/b-catenin signaling antagonist C-82 sup-pressed the MSC-induced CD44 expression and the adhesion ofOCI-AML3 cells to MSCs (Supplementary Fig. S1C). The BMstroma induction of b-catenin levels in AML cells was furtherdemonstrated by coculturing Molm13 and PB cells from primarypatients (n ¼ 3) with MSCs (48 hours; Supplementary Fig. S1D).
Disrupting Wnt/b-catenin signaling induces apoptosis,suppresses cell growth, and inhibits b-catenin downstreamtargets in AML bulk and stem/progenitor cells
We treated several AML cell lines with C-82 (48 hours)and observed marked apoptosis induction (EC50 ¼ 0.82 �0.04 mmol/L and 0.79 � 0.02 mmol/L) and cell growth suppres-sion (IC50¼ 0.42�0.06mmol/L and0.39�0.02mmol/L) inOCI-AML3andMolm13 cells (Fig. 1A), respectively. Althoughpartiallysuppressing cell growth, C-82 only slightly induced apoptosis inKG1 cells at the doses used (Fig. 1A). Cell-cycle analysis showedthat the treatment decreased S-phase cells, while increasing cells insub-G1 phase in OCI-AML3 andMolm13, consistent with growthsuppression and apoptosis induction in these cells (Fig. 1A). C-82also induced apoptosis (72 hours) in AML blasts (n ¼ 7; EC50 ¼1.90 � 0.28 mmol/L and IC50 ¼ 1.17 � 0.26 mmol/L) andCD34þCD38� stem/progenitor cells (n ¼ 6; EC50 ¼ 4.25 �0.69 mmol/L and IC50 ¼ 2.11� 0.04 mmol/L) from AML patients(Table 1), and had minimal toxicity to normal BM CD34þ cells(Fig. 1B). C-82 treatment decreased the b-catenin/CBP down-stream targets, including survivin, c-Myc, and CD44, in Molm13,OCI-AML3, AML bulk, and CD34þCD38� stem/progenitor cellsfrom patients, as determined by either Western blot or flowcytometry in available samples (Fig. 1C). Representative FACSplots of survivin and CD44 are shown in Supplementary Fig. S2.
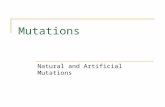
Combined inhibition of b-catenin and FLT3 signalingsynergistically induces apoptosis in FLT3-mutated AML cellsand CD34þCD38� AML stem/progenitor cells
In agreement with the finding that constitutive activation ofFLT3 stimulates the b-catenin pathway (9), we observed thatMolm13 cells were very sensitive to C-82 treatment (Fig. 1A). Todemonstrate that FLT3 mutations were indeed associated withb-catenin, we determined b-catenin expression and C-82 sensi-tivity in Ba/F3 cells without or with FLT3 mutations. We foundthat cells with FLT3 mutations expressed higher b-catenin andwere generallymore sensitive toC-82 than cell lineswithout FLT3-mutation (Fig. 2A).We then treated Ba/F3 cells and AML cell lineswith C-82, sorafenib, and their combination. The combinationsynergistically induced apoptosis (CI < 1) in Ba/F3-ITD, Ba/F3-D835G, Ba/F3-ITDþ676, and even in the sorafenib-resistant Ba/F3-ITDþ842 cells (Fig. 2B). The synergy was also observed inMolm13 and MV4-11 cells with FLT3-ITD mutation, even whenthey were cocultured with human BM-derived MSCs (Fig. 2C).Similar results were obtained in Molm13 and MV4-11 cellstreated with C-82 and the novel FLT3 inhibitor quizartinib
Jiang et al.
Clin Cancer Res; 24(10) May 15, 2018 Clinical Cancer Research2420
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

(Supplementary Fig. S3). To further demonstrate that C-82–induced b-catenin inhibition contributes to the synergy in thecombination, we inhibited b-catenin expression using 4 specificandpooled siRNAs inMolm13 andMV4-11 cells. Each siRNAwas
able to reduce b-catenin expression and the pool (SMARTpool)was slightly more effective (Supplementary Fig. S4). We nexttreated the cells with the SMARTpool siRNA (24 hours) and thenwith sorafenib for additional 48 hours. Figure 2D shows that
Figure 1.
C-82 induces apoptosis, suppresses growth, and inhibits b-catenin targets in AML cells and stem/progenitor cells. A, AML cell lines were treated with C-82 for 48hours. Apoptosis was measured by flow cytometry. Viable cell count was assessed by the Trypan blue exclusion method. Cell-cycle status was determinedby flow cytometry. B, AML patient and normal BM (NBM) samples were treated with C-82. Apoptosis in bulk and CD34þCD38� AML (72 hours) and normal CD34þ
(48 hours) cells was measured by flow cytometry. C, Molm13 and OCI-AML3 cells were treated for 24, 48, or 72 hours and AML patient samples for 72 hourswith C-82. Survivin, CD44, and c-Myc expressions were determined by Western blot or flow cytometry. For Molm13 and OCI-AML3 cells, the top panel shows arepresentative Western blot and the bottom panel the quantitative Western blots of three independent experiments. � , P < 0.05; ��, P < 0.01.
Wnt/b-Catenin Signaling Inhibition in AML
www.aacrjournals.org Clin Cancer Res; 24(10) May 15, 2018 2421
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

Figure 2.
Combined inhibition of b-catenin and FLT3 synergistically induces apoptosis in cell lines, AML blasts, and CD34þCD38� AML stem/progenitor cells with FLT3mutations. A, Expression of b-catenin in Ba/F3 cells without or with FLT3 mutations determined by Western blot and apoptosis in these cells treatedwith C-82 detected (24 hours) by flow cytometry. B, Apoptosis in FLT3-mutated Ba/F3 cells treated with C-82, sorafenib, or both (24 hours). C, Apoptosis in Molm13and MV4-11 cells without (top) or with (bottom) MSC coculture treated with C-82, sorafenib, or both (48 hours). D, Molm13 and MV4-11 cells were treated withCTNNB1 SMARTpool ON-TARGET plus siRNAs for 24 hours, then with sorafenib. b-Catenin silencing was confirmed byWestern blot. Apoptosis was measured aftercells were treated with sorafenib for 48 hours. E, AML patient samples with or without FLT3 mutations were treated with C-82 (1.0 mmol/L), sorafenib(2.5 mmol/L), or both (48 hours). Apoptosis was determined in bulk and CD34þCD38� cells. Apoptotic cells were assessed by flow cytometry. CI values werecalculated. CI < 1.0 indicated synergistic effect. cocx, coculture; Ctrl, control; Sor, sorafenib; Comb, combination.
Jiang et al.
Clin Cancer Res; 24(10) May 15, 2018 Clinical Cancer Research2422
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

siRNA silencing of b-catenin enhanced sorafenib-induced celldeath in these cells. No synergy was detected when C-82 wascombined with sorafenib in FLT3-WT Ba/F3 or OCI-AML3 cells,while the synergy was observed when C-82 was combined withchemotherapeutic agent Ara-C in both Molm13 and OCI-AML3cells (Supplementary Fig. S5). Importantly, synergy was alsoobserved in bulk and CD34þCD38� AML cells from FLT3-mutat-ed patients treated with C-82 and sorafenib with or without MSCcoculture (48 hours; even in a patient with ITDþD835 mutation,#14, Table 1), while cells from FLT3-WT AML patients were ingeneral less sensitive to C-82, and resistant to sorafenib, and nosynergy was observed in these cells with the combination treat-ment (Fig. 2E). Furthermore, either agent alone, or their combi-nation, had limited cytotoxicity on normal BM cells (Supplemen-tary Fig. S6).
Combinations of C-82 and TKIs inhibit both b-catenin/CBPand FLT3 signaling and decreaseb-catenin nuclear localizationin AML cells
FLT3-ITD AML cells were treated with C-82, sorafenib, or both.Wnt signal pathway PCR array analysis revealed that both C-82and sorafenib markedly suppressed the expression of multiplegenes involved in theWnt/b-catenin signaling pathway, includingb-catenin (CTNNB1), CD44, survivin (BIRC5), cyclin D1(CCND1), and c-Myc, and several frizzled family receptors/cor-eceptors andWnt ligands, such as FZD1, FZD3, FZD5, FZD6, low-density lipoprotein receptor (LDLR), WNT10B, andWNT3A (�2-fold decreases; indicated by arrows), but C-82 or the combinationwas more effective than sorafenib alone for most target inhibi-tions (Fig. 3A). Western blot confirmed that C-82, sorafenib, orthe combination suppressed the expression of Wnt/b-catenin/CBP downstream targets such as c-Myc, survivin, and CD44 inMolm13 andMV4-11 cells (Fig. 3B). Sorafenib or quizartinib andthe combination, but not C-82 alone, effectively inhibited FLT3signaling molecules including p-FLT3, p-STAT5, p-ERK, and p-AKT (Fig. 3B and C). Optimal inhibition of both b-catenin andFLT3 signaling was observed only when C-82 and TKIs werecombined (Fig. 3A–C). As expected, sorafenib did not affectsignaling pathways in OCI-AML3 cells (Fig. 3D).
Because c-Myc is a b-catenin target, it was not surprising thatC-82 reduced c-Myc levels in Molm13, MV4-11, and OCI-AML3cells independent of their FLT3 mutational status (Fig. 3A–D).Interestingly, TKIs potently decreased c-Myc levels in FLT3-ITD–mutated AML cells, coinciding with potent inhibitions ofp-ERK and p-STAT5 (Fig. 3B and C). This would suggest that, inaddition to modulating c-Myc through regulation of Wnt/b-catenin, FLT3 may also regulate c-Myc level through p-ERKor p-STAT5 signaling.
To test this, we treated Molm13 cells with the STAT5 inhib-itor AG490 or an ERK inhibitor PD0325901 (both from SelleckChemicals), and found that AG490, but not PD0325901,suppressed c-Myc expression (Fig. 3E), suggesting that theTKI-induced c-Myc inhibition is mediated, in part, throughFLT3/STAT5 signaling. Furthermore, C-82 and sorafenib incombination inhibited the expression of total b-catenin andCD44, and also reduced the nuclear localization of b-catenin inMolm13 and MV4-11 cells by confocal analysis, and thedecreased b-catenin nuclear localization was further confirmedby Western blot (Fig. 3F; images of each single staining areshown in Supplementary Fig. S7). These data indicated that thecombination could disrupt both b-catenin/CBP and FLT3 sig-
naling, and induce cell death more effectively in FLT3-mutatedAML cells.
Inhibition of b-catenin enhances the antileukemia activity ofTKIs against FLT3-mutated AML xenografts and impairsengraftment in immunodeficient mice
To test the effect of the combinatorial strategy in FLT3-mutated AML in vivo, we used two xenograft murine models.For the Molm13-GFP/Luc cell xenograft in the NSG murinemodel (Fig. 4A), treatment with PRI-724 (C-82 prodrug) orsorafenib inhibited leukemia growth, and the combination wasthe most effective in this regard, as determined by in vivoimaging analysis (Fig. 4B and C) and flow cytometric measure-ment of human CD45þ cells in mouse PB (Fig. 4D). Micetreated with PRI-724 (19 days, P ¼ 0.025) or sorafenib (28days, P ¼ 0.0002) had a statistically significantly longer mediansurvival compared with controls (17 days), and the combinedtreatment further prolonged the survival (30.5 days; P¼ 0.0005vs. PRI-724; P ¼ 0.0056 vs. sorafenib) in this aggressive xeno-graft AML model (Fig. 4E). Tissues were collected (n¼ 3/group)2 hours after the 15-day treatments. The combination markedlydecreased leukemia cells in the BM and spleen, as determinedby flow cytometry, H&E staining, and reduced spleen sizes (Fig.4F and G). Using CyTOF mass cytometry that can simulta-neously measure cell surface and intracellular proteins, wedetermined the number of human CD45þ cells and proteinexpression in these cells in 15-day-treated BM samples. SPADEtree analysis showed that the combination greatly decreasedhuman CD45þ populations (Fig. 4H) and the expression ofb-catenin, CD44, c-Myc, p-FLT3, p-ERK, p-AKT, and p-STAT5 inthese cells (Fig. 4I). Although reduction of survivin in Molm13cells upon the combinatorial treatment was observed in vitro(Fig. 3B), we observed only slightly lower survivin levels, whichdid not reach statistical significance in vivo at the time sampleswere collected (2 hours after treatments on day 15). There areseveral reasons why we did not see the same level of targetreduction of the combination treatment in vitro and in vivo, suchas (i) the doses for in vivo and in vitro do not exactly translate,(ii) it is much easier to perform a time course in vitro than invivo, and (iii) leukemia cells collected from mice lived in a verydifferent microenvironment compared with cells in culture, aswe have shown that the BM microenvironment induces b-cate-nin and its downstream targets. Of note, the survivin decreasewas observed in BM samples collected from AML patients whohad underwent phase I dose escalation with PRI-724 (30).
For the PDX xenograft in theNSGSmurinemodel (Fig. 5A), thecombination treatment also showed the strongest antileukemiaactivity as demonstrated by flow cytometric measurement ofhuman CD45þ cells in mouse PB (n ¼ 10/group) after a 3-weektreatment (Fig. 5B) and inBMand spleen cells collected frommice(n¼3/group) after a 25-day treatment (Fig. 5C).Mice treatedwithPRI-724 or sorafenib had a significantly longer median survival(31 days, P ¼ 0.008 or 48 days, P ¼ 0.0003; respectively)compared with controls (29 days), and the combination furtherprolonged the survival (54 days; P ¼ 0.0005 vs. PRI-724; P ¼0.0067 vs. sorafenib; Fig. 5D). An attempt to determine leukemiacell populations and the target protein expression by CyTOF incollected BM cells failed due to insufficient cells in sorafenib andthe combination treatment groups. Results indicate that PRI-724enhanced sorafenib activity in vivo against FLT3-mutated AML.Except for an initial slight body weight loss in sorafenib and the
Wnt/b-Catenin Signaling Inhibition in AML
www.aacrjournals.org Clin Cancer Res; 24(10) May 15, 2018 2423
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

Figure 3.
C-82 and TKI combination inhibits b-catenin/CBP and FLT3 signaling and reduces b-catenin nuclear localization in AML cells. A, Molm13 cells were treated with C-82(0.5 mmol/L), sorafenib (20 nmol/L), or both for 48 hours, and RNA levels were determined by the Wnt signaling pathway PCR array (arrows indicate genesdiscussed in the text). B, Expression of b-catenin/CBP and FLT3 signaling and downstream targets were analyzed by Western blotting in Molm13 andMV4-11 cells treated with C-82 and sorafenib for 6, 24, and 48 hours. C-82 and sorafenib were 0.5 mmol/L and 20 nmol/L for Molm13 and 0.56 mmol/L and 75 nmol/Lfor MV4-11, respectively. C, Molm13 cells were treated with C-82 (0.5 mmol/L) and quizartinib (1.6 nmol/L), and (D) OCI-AML3 cells were treated with C-82(0.5 mmol/L) and sorafenib (20 nmol/L) for 6, 24, and 48 hours. E, Molm13 cells were treated with JAK/STAT inhibitor AG490 (100 mmol/L) or MEK/ERKinhibitor PD0325901 (200 nmol/L) for 6 and 24 hours. Protein expressions were determined by Western blot analysis. F, Confocal image (1,000 �) andquantifications illustrating expressions of b-catenin and CD44, and the nuclear localization of b-catenin (top) and b-catenin levels in total, cytoplasmic, and nuclearfractions by Western blot analysis (bottom) in Molm13 or MV4-11 cells treated with C-82 (0.5 or 0.56 mmol/L), sorafenib (20 or 75 nmol/L), or both for48 hours. Ctrl, control; Sor, sorafenib; Comb, combination. � , P < 0.05; �� , P < 0.01.
Jiang et al.
Clin Cancer Res; 24(10) May 15, 2018 Clinical Cancer Research2424
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

Figure 4.
PRI-724 enhances sorafenib activity in Molm13-GFP/Luc xenograft NSG mice. A, Experimental scheme. After confirmed engraftment of Molm13-GFP/Luc cells byimaging, mice were treated with RPI-724, sorafenib, or the combination for 4 weeks. B, Weekly images of mice from the IVIS-200 imaging system. X, noalive mice. C, Imaging quantification by the IVIS-200 software. D, Leukemia cells (human CD45þ) in mouse PB determined by flow cytometry. E, Survival curves.F, Leukemia cells (human CD45þ) in mouse BM and spleen detected by flow cytometry. G, Mouse BM and spleen H&E staining (200�) and spleen sizes.H, CyTOF/SPADE analysis of leukemia cells (human CD45þ) in mouse BM samples after 15-day treatments. I, The expression of b-catenin targets and FLT3downstream signal proteins in human CD45þ cells in BM of control mice presented in SPADE tree (left) and the quantitation of these proteins in various treatmentgroups (right). � , P < 0.05; ��, P < 0.01.
Wnt/b-Catenin Signaling Inhibition in AML
www.aacrjournals.org Clin Cancer Res; 24(10) May 15, 2018 2425
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

Figure 5.
Inhibition of b-catenin enhances sorafenib activity in FLT3-ITD PDX cell xenograft NSGS mice and suppresses engraftment potential of the PDX cells.A, Experimental scheme. After confirmed engraftment by flow cytometry of human CD45 positivity, NSGS mice were treated with RPI-724, sorafenib,and the combination for 4 weeks. B, Leukemia burden assessed by flow cytometry measuring human CD45þ cells in mouse PB after 3-week treatments.C, Leukemia burdens in mouse BM and spleen determined by flow cytometry after 25-day treatments. D, Survival curves. E, Engraftment of the ex vivotreated PDX cells and survival curve. The PDX cells (2 � 106) were untreated or treated with C-82 (1 mmol/L), sorafenib (2.5 mmol/L), or both for 48 hours andthen injected into NSGS mice. Engraftment was assessed by flow cytometric measurement of human CD45 positivity at 9 and 12 weeks after cellinjection. Ctrl, control; Sor, sorafenib; Comb, combination. � , P < 0.05; ��, P < 0.01.
Clin Cancer Res; 24(10) May 15, 2018 Clinical Cancer Research2426
Jiang et al.
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

combination treatment groups, no significant drug-related toxic-ity was observed.
To further assess the potential of inhibition of b-catenin and itscombination with TKIs on targeting FLT3-mutated AML stem/progenitor cells, we treated the above PDX cells with C-82,sorafenib, or both ex vivo, then injected the cells to NSGS mice.As shown in Fig. 5E,mice injectedwith cells prior exposed to C-82or the combination of C-82 and sorafenib, but not sorafenibalone, engrafted significantly slower, exhibited lower leukemiaburden than the untreated controls. These animals also livedlonger. At 120 days after cell injections, 5 of 6 or 3 of 6 miceinjectedwith untreated or sorafenib-treated cells died,while 5 of 6or 6 of 6 mice injected with C-82 or C-82 plus sorafenib-treatedcells were alive (Fig. 5E). The results support the notion thatinhibition of b-catenin, but not FLT3-ITD tyrosine kinase, targetsAML stem/progenitor cells.
DiscussionBesides its roles in AML initiation and progression, b-catenin
signaling plays an essential role in the BM microenvironmentsupporting minimal residual disease and LSC maintenance,which are responsible for leukemia relapse (31). Inhibition ofb-catenin is regarded as a promising strategy to eliminate LSC(32). Our finding of higher b-catenin expression in BM than inpaired PB AML samples supports an important role for Wnt/b-catenin signaling in the leukemia BM microenvironment.Disruption of Wnt/b-catenin signaling by C-82 suppressedgrowth, induced apoptosis, and overcame stromal protectionof AML cells and stem/progenitor cells. Moreover, the b-catenindownstream target CD44 is overexpressed in AML cells andreportedly plays an important role in chemoresistance (33).CD44 also regulates AML LSC homing to microenvironmentalniches and maintaining a primitive phenotype (34). Hence,targeting CD44 not only increases chemosensitivity but alsopotentially eradicates AML LSC in BM niche (33, 35). In thisregard, we showed that inhibition of Wnt/b-catenin signalingdecreased CD44 expression in AML blasts and LSCs, inhibitedadhesion of AML cells to MSCs, and induced death of AML cellscocultured with MSCs.
Although highly heterogeneous, approximately 30% of AMLpatients have FLT3 mutations that contribute to disease progres-sion and poor prognosis (36, 37). To overcome limitations andimprove efficacy of FLT3 TKIs, novel combinatorial strategies arerequired, including targeting multiple signaling pathways, dis-rupting BM microenvironment protection, and eliminating LSC(38, 39). FLT3 signaling is known to increase b-catenin nuclearlocalization and transcription activity (9, 40) and Wnt/b-cateninpathway to modulate the TKI sensitivity through GSK-3b–depen-dent mechanisms (41). Moreover, it was reported that FLT3mutations cooperate with Wnt/b-catenin signaling transductionin AML cells and primary AML blasts (10). Interestingly, a recentstudy demonstrated that the microenvironment can confer sor-afenib resistance in FLT3-mutated cells by activating integrinavb3/PI3K/AKT/GSKb/b-catenin signaling pathway (42), furthersupporting the induction of b-catenin by BM microenvironmentand suggesting the potential for combinatorial inhibition of FLT3and b-catenin in FLT3-mutated AML. We demonstrated thatinhibition of b-catenin by C-82 decreases the expression of CD44,an important LSC homing protein, which may contribute to thesynergistic effect of C-82 and sorafenib in FLT3-mutated cells
under in vitro leukemia-MSC coculture conditions, and in vivo inmouse models, by disrupting leukemia-microenvironmentalinteractions.
Our initial study focused on investigating the effect of targetingb-catenin onAMLcells and stem/progenitor cells andweobservedhigher sensitivity of FLT3-mutated cells to the b-catenin inhibitorC-82. After confirming higher levels of b-catenin in FLT3-mutatedcells, which corresponded to C-82 sensitivity, we demonstratedthat combined inhibition of b-catenin by C-82 and FLT3 by TKIsexerted synergistic antileukemic effects on FLT3-mutated AMLcells and LSC/progenitor cells, in agreement with a recent reportshowing that a novel dual FLT3 and Wnt/b-catenin inhibitorSKLB-677, suppressed leukemia stem-like cells and had potentantileukemia activity in FLT3-mutated AML cells (43). Our studyfurther demonstrated that inhibition of b-catenin impaired theengraftment of FLT3-ITD cells derived from an AML patient inNSGS mice and that the combined inhibition of b-catenin andFLT3 signaling significantly prolonged survival compared withinhibiting each target alone in mice xenografted with either aFLT3-mutated cell line or PDX cells. Importantly, PRI-724 waswell tolerated, showing an acceptable toxicity profile in a phase I,dose-escalation study in patients with advanced AML (30). Thisstudywas recently completed suggesting that the combinationhasthe potential for clinical development.
Mechanistic studies showed that C-82 and TKIs effectivelyinhibited Wnt/b-catenin targets and FLT3 downstream signaling,respectively; while the combination more potently inhibitedboth. FLT3-ITD in AML was reported to induce c-Myc, which isone of Wnt/b-catenin targets and an essential regulator of cellcycle and apoptosis (10). Depletion of b-catenin and c-Myccontributed to the synergistic effect of combined inhibition ofb-catenin and histone deacetylase in FLT3-ITD mutations AML(1). We demonstrated that C-82 or TKI individually inhibited c-Myc expression in FLT3-mutated AML and more so by theircombination. Furthermore, we showed that, other than modu-lating b-catenin signaling, FLT3 inhibition directly suppressed c-Myc expression primarily through the FLT3-ITD/STAT5 signalingcascade.
Collectively, these findings provide a mechanistic basis forclinical development of this novel combinatorial strategy toovercome TKI resistance and improve outcomes in FLT3-mutatedAML patients. Importantly, constitutive activation of multiplesurvival signaling pathways that can further activate Wnt/b-cate-nin signaling is common in many types of malignant cells. Thecombination strategy that targets both Wnt/b-catenin and othersurvival signaling pathways likely also applies to the treatment ofother cancers.
Disclosure of Potential Conflicts of InterestB.Z. Carter reports receiving commercial research grants from Prism Pharma
and Eisai. No potential conflicts of interest were disclosed by the other authors.
Authors' ContributionsConception and design: M. Andreeff, B.Z. CarterDevelopment of methodology: X. Jiang, P.Y. Mak, H. Mu, W. Zhang,M. AndreeffAcquisition of data (provided animals, acquired and managed patients,provided facilities, etc.): X. Jiang, H. Mu, W. Tao, D.H. Mak, S. Kornblau,Q. Zhang, J.K. Burks, J. CortesAnalysis and interpretation of data (e.g., statistical analysis, biostatistics,computational analysis): X. Jiang, P.Y. Mak, H. Mu, S. Kornblau, P. Ruvolo,J.K. Burks, R. Pan, M. Konopleva, M. Andreeff, B.Z. Carter
www.aacrjournals.org Clin Cancer Res; 24(10) May 15, 2018 2427
Wnt/b-Catenin Signaling Inhibition in AML
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

Writing, review, and/or revision of the manuscript: X. Jiang, S. Kornblau,W. Zhang, R. Pan, H. Zhou, M. Konopleva, J. Cortes, Q. Liu, M. Andreeff,B.Z. CarterAdministrative, technical, or material support (i.e., reporting or organizingdata, constructing databases): X. Jiang, H. Mu, Q. Zhang, P. Ruvolo, W. Zhang,T. McQueen, Q. LiuStudy supervision: Q. Liu, B.Z. Carter
AcknowledgmentsThe authors thank Dr. Numsen Hail for assisting with the manuscript
preparation and PRISM Pharma for providing C-82 and PRI-724.This work was supported by the Ryan Gibson Foundation and PRISM
Pharma/Eisai research funding to B.Z. Carter, grants from theNIH (CA055164),
the MD Anderson Cancer Center Support Grant (CA016672), Cancer Preven-tion Research Institute of Texas (CPRIT, RP121010), and the Paul and MaryHaas Chair in Genetics to M. Andreeff.
The costs of publication of this article were defrayed in part by thepayment of page charges. This article must therefore be hereby markedadvertisement in accordance with 18 U.S.C. Section 1734 solely to indicatethis fact.
Received May 31, 2017; revised November 14, 2017; accepted February 14,2018; published first February 20, 2018.
References1. Fiskus W, Sharma S, Saha S, Shah B, Devaraj SG, Sun B, et al. Pre-clinical
efficacy of combined therapy with novel b-catenin antagonist BC2059and histone deacetylase inhibitor against AML cells. Leukemia 2015;29:1267–78.
2. Lane SW, Wang YJ, Lo Celso C, Ragu C, Bullinger L, Sykes SM, et al.Differential niche and Wnt requirements during acute myeloid leukemiaprogression. Blood 2011;118:2849–56.
3. Dietrich PA, Yang C, Leung HH, Lynch JR, Gonzales E, Liu B, et al. GPR84sustains aberrant b-catenin signaling in leukemic stem cells for mainte-nance of MLL leukemogenesis. Blood 2014;124:3284–94.
4. Ysebaert L, Chicanne G, Demur C, De Toni F, Prade-Houdellier N, Rui-davets JB, et al. Expression of b-catenin by acute myeloid leukemia cellspredicts enhanced clonogenic capacities and poor prognosis. Leukemia2006;20:1211–6.
5. Gandillet A, Park S, Lassailly F, Griessinger E, Vargaftig J, Filby A, et al.Heterogeneous sensitivity of human acute myeloid leukemia to b-catenindown-modulation. Leukemia 2011;25:770–80.
6. Kim Y, Thanendrarajan S, Schmidt-Wolf IG. Wnt/b-catenin: a new thera-peutic approach to acute myeloid leukemia. Leuk Res Treatment 2011;2011:428960.
7. Eaves CJ, Humphries RK. Acutemyeloid leukemia and theWnt pathway. NEngl J Med 2010;362:2326–7.
8. Schnittger S, Schoch C,DugasM, KernW, Staib P,Wuchter C, et al. Analysisof FLT3 length mutations in 1003 patients with acute myeloid leukemia:correlation to cytogenetics, FAB subtype, and prognosis in the AMLCGstudy and usefulness as a marker for the detection of minimal residualdisease. Blood 2002;100:59–66.
9. Kajiguchi T, Chung EJ, Lee S, Stine A, Kiyoi H, Naoe T, et al. FLT3regulates b-catenin tyrosine phosphorylation, nuclear localization, andtranscriptional activity in acute myeloid leukemia cells. Leukemia 2007;21:2476–84.
10. Tickenbrock L, Schw€able J,WiedehageM, Steffen B, Sargin B, ChoudharyC,et al. Flt3 tandem duplication mutations cooperate with Wnt signaling inleukemic signal transduction. Blood 2005;105:3699–706.
11. Kiyoi H, Ohno R, Ueda R, Saito H, Naoe T. Mechanism of constitutiveactivation of FLT3with internal tandemduplication in the juxtamembranedomain. Oncogene 2002;21:2555–63.
12. Al-Mawali A, Gillis D, Lewis I. Characteristics and prognosis of adult acutemyeloid leukemia with internal tandem duplication in the FLT3 gene.Oman Med J 2013;28:432–40.
13. Daver N, Cortes J, Ravandi F, Patel KP, Burger JA, Konopleva M, et al.Secondary mutations as mediators of resistance to targeted therapy inleukemia. Blood 2015;125:3236–45.
14. Li L, Osdal T, Ho Y, Chun S, McDonald T, Agarwal P, et al. SIRT1 activationby a c-MYC oncogenic network promotes the maintenance and drugresistance of human FLT3-ITD acute myeloid leukemia stem cells. CellStem Cell 2014;15:431–46.
15. Kida A, Kahn M. Hypoxia selects for a quiescent, CML stem/leukemiainitiating-like population dependent on CBP/catenin transcription. CurrMol Pharmacol 2013;6:204–10.
16. Gang EJ, Hsieh YT, Pham J, Zhao Y, Nguyen C, Huantes S, et al. Small-molecule inhibition of CBP/catenin interactions eliminates drug-resis-tant clones in acute lymphoblastic leukemia. Oncogene 2014;33:2169–78.
17. Zhou H, Mak PY, Mu H, Mak DH, Zeng H, Cortes J, et al.Combined inhibition of b-catenin and Bcr-Abl synergistically targetstyrosine kinase inhibitor-resistant blast crisis chronic myeloid leu-kemia blasts and progenitors in vitro and in vivo. Leukemia 2017;31:2065–74.
18. Kornblau SM, Tibes R, Qiu YH, Chen W, Kantarjian HM, Andreeff M, et al.Functional proteomic profiling of AML predicts response and survival.Blood 2009;113:154–64.
19. Carter BZ, Qiu YH, Zhang N, Coombes KR, Mak DH, Thomas DA, et al.Expression of ARC (apoptosis repressor with caspase recruitment domain),an antiapoptotic protein, is strongly prognostic in AML. Blood 2011;117:780–7.
20. Tse KF, Allebach J, Levis M, Smith BD, Bohmer F, Small D. Inhibition ofthe transforming activity of FLT3 internal tandem duplication mutantsfrom AML patients by a tyrosine kinase inhibitor. Leukemia 2002;6:2027–36.
21. Zhang W, Gao C, Konopleva M, Chen Y, Jacamo RO, Borthakur G, et al.Reversal of acquired drug resistance in FLT3-mutated acute myeloidleukemia cells via distinct drug combination strategies. Clin Cancer Res2014;20:2363–74.
22. Romano P, Manniello A, Aresu O, Armento M, Cesaro M, Parodi B.Cell Line Data Base: structure and recent improvements towardsmolecular authentication of human cell lines. Nucleic Acids Res2009;37:D925–32.
23. Carter BZ, Mak DH, Wang Z, Ma W, Mak PY, Andreeff M, et al. XIAPdownregulation promotes caspase-dependent inhibition of proteasomeactivity in AML cells. Leuk Res 2013;37:974–9.
24. Jacamo R, Chen Y, Wang Z, Ma W, Zhang M, Spaeth EL, et al. Reciprocalleukemia-stroma VCAM-1/VLA-4-dependent activation of NF-kBmediateschemoresistance. Blood 2014;123:2691–702.
25. Carter BZ, Mak PY, Chen Y,MakDH,MuH, Jacamo R, et al. Anti-apoptoticARC protein confers chemoresistance by controlling leukemia-microenvi-ronment interactions through a NFkB/IL1b signaling network. Oncotarget2016;7:20054–67.
26. Bendall SC, Simonds EF, Qiu P, el-AD Amir, Krutzik PO, Finck R,et al. Single-cell mass cytometry of differential immune and drugresponses across a human hematopoietic continuum. Science 2011;332:687–96.
27. Han L,Qiu P, Zeng Z, Jorgensen JL,MakDH, Burks JK, et al. Single-cellmasscytometry reveals intracellular survival/proliferative signaling in FLT3-ITD-mutated AML stem/progenitor cells. Cytometry A 2015;87:346–56.
28. Carter BZ, Mak PY, Mu H, Zhou HS, Mak DH, Schober W, et al. CombinedTargeting of BCL-2 and BCR-ABL Tyrosine Kinase Eradicates ChronicMyeloid Leukemia Stem Cells. Sci Transl Med 2016;8:355ra117.
29. Chou TC, Talalay P. Quantitative analysis of dose-effect relationships: thecombined effects of multiple drugs or enzyme inhibitors. Adv EnzymeRegul 1984;22:27–55.
30. Cortes JE, Carter BZ, Quintas-Cardama A, Inada T, Morita K, Fujimori M,et al. A phase I dose-escalation study of PRI-724, a CBP/b-catenin mod-ulator in patients with advanced acute myeloid leukemia (AML). Haema-tologica 2014;99(s1):222–3. abstract n. s648.
31. Hu K, Gu Y, Lou L, Liu L, Hu Y, Wang B, et al. Galectin-3 mediates bonemarrowmicroenvironment-induced drug resistance in acute leukemia cellsvia Wnt/b-catenin signaling pathway. J Hematol Oncol 2015;8:1.
Clin Cancer Res; 24(10) May 15, 2018 Clinical Cancer Research2428
Jiang et al.
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

32. Konopleva M, Tabe Y, Zeng Z, Andreeff M. Therapeutic targeting ofmicroenvironmental interactions in leukemia: mechanisms andapproaches. Drug Resist Updat 2009;12:103–13.
33. Wang NS, Wei M, Ma WL, Meng W, Zheng WL. Knockdown of CD44enhances chemosensitivity of acute myeloid leukemia cells to ADM andAra-C. Tumour Biol 2014;35:3933–40.
34. Siapati EK, Papadaki M, Kozaou Z, Rouka E, Michali E, SavvidouI, et al. Proliferation and bone marrow engraftment of AML blastsis dependent on b-catenin signaling. Br J Haematol 2011;152:164–74.
35. Jin L, Hope KJ, Zhai Q, Smadja-Joffe F, Dick JE. Targeting of CD44eradicates human acute myeloid leukemic stem cells. Nat Med 2006;12:1167–74.
36. Gilliland DG. Molecular genetics of human leukemias: new insights intotherapy. Semin Hematol 2002;39:6–11.
37. Fr€ohling S, Schlenk RF, Breitruck J, Benner A, Kreitmeier S, Tobis K,et al. Prognostic significance of activating FLT3 mutations in youngeradults (16 to 60 years) with acute myeloid leukemia and normalcytogenetics: a study of the AML Study Group Ulm. Blood 2002;100:4372–80.
38. Kindler T, Lipka DB, Fischer T. FLT3 as a therapeutic target in AML: stillchallenging after all these years. Blood 2010;116:5089–102.
39. Chang E, Ganguly S, Rajkhowa T, Gocke CD, Levis M, Konig H. Thecombination of FLT3 and DNA methyltransferase inhibition is synergis-tically cytotoxic to FLT3/ITD acute myeloid leukemia cells. Leukemia2016;30:1025–32.
40. Kajiguchi T, Katsumi A, Tanizaki R, Kiyoi H, Naoe T. Y654 of b-catenin isessential for FLT3/ITD-related tyrosine phosphorylation and nuclear local-ization of b-catenin. Eur J Haematol 2012;88:314–20.
41. Jiang J, Griffin JD. Wnt/b-catenin pathway modulates the sensitivity of themutant FLT3 receptor kinase inhibitors in a GSK-3b dependent manner.Genes Cancer 2010;1:164–76.
42. Yi H, Zeng D, Shen Z, Liao J, Wang X, Liu Y, et al. Integrin alphavbeta3enhances b-catenin signaling in acute myeloid leukemia harboring Fms-like tyrosine kinase-3 internal tandemduplicationmutations: implicationsfor microenvironment influence on sorafenib sensitivity. Oncotarget2016;7:40387–97.
43. Ma S, Yang LL, Niu T, Cheng C, Zhong L, Zheng MW, et al. SKLB-677, anFLT3 and Wnt/b-catenin signaling inhibitor, displays potent activity inmodels of FLT3-driven AML. Sci Rep 2015;5:15646.
www.aacrjournals.org Clin Cancer Res; 24(10) May 15, 2018 2429
Wnt/b-Catenin Signaling Inhibition in AML
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556

2018;24:2417-2429. Published OnlineFirst February 20, 2018.Clin Cancer Res Xuejie Jiang, Po Yee Mak, Hong Mu, et al. Leukemia
-Mutant Acute MyeloidFLT3Synergizes with FLT3 Inhibition in -Catenin Exerts Antileukemia Activity andβDisruption of Wnt/
Updated version
10.1158/1078-0432.CCR-17-1556doi:
Access the most recent version of this article at:
Material
Supplementary
http://clincancerres.aacrjournals.org/content/suppl/2018/02/20/1078-0432.CCR-17-1556.DC1
Access the most recent supplemental material at:
Cited articles
http://clincancerres.aacrjournals.org/content/24/10/2417.full#ref-list-1
This article cites 43 articles, 14 of which you can access for free at:
Citing articles
http://clincancerres.aacrjournals.org/content/24/10/2417.full#related-urls
This article has been cited by 3 HighWire-hosted articles. Access the articles at:
E-mail alerts related to this article or journal.Sign up to receive free email-alerts
Subscriptions
Reprints and
To order reprints of this article or to subscribe to the journal, contact the AACR Publications Department at
Permissions
Rightslink site. Click on "Request Permissions" which will take you to the Copyright Clearance Center's (CCC)
.http://clincancerres.aacrjournals.org/content/24/10/2417To request permission to re-use all or part of this article, use this link
on November 12, 2020. © 2018 American Association for Cancer Research.clincancerres.aacrjournals.org Downloaded from
Published OnlineFirst February 20, 2018; DOI: 10.1158/1078-0432.CCR-17-1556