DISORDERS OF THE ADRENAL GLANDS...DISORDERS OF THE ADRENAL GLANDS L. Michael Brunt, MD, FACS, and...
Transcript of DISORDERS OF THE ADRENAL GLANDS...DISORDERS OF THE ADRENAL GLANDS L. Michael Brunt, MD, FACS, and...

D I S O R D E R S O F T H E A D R E N A L G L A N D S
L. Michael Brunt, MD, FACS, and Linda P. Zhang, MD*
The adrenal glands may be affected by a variety of different pathologic conditions. Although not among the most common disorders encountered by surgeons, functioning adrenal tumors that produce excessive amounts of adrenal hormones are remarkable for the range of clinical syndromes they give rise to. In this chapter, the clinical presentation, diagnostic evaluation, and management of the various adre-nal tumors are reviewed, and the workup of incidentally discovered adrenal masses (adrenal incidentalomas) is outlined. The technical details of adrenalectomy (both open and laparoscopic) are discussed in detail, and factors that increase the diffi culty of adrenalectomy are also reviewed.
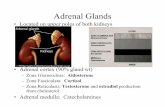
Anatomic Considerations
The adrenal glands are retroperitoneal organs that lie along the superomedial aspects of the two kidneys [see Figure 1]. Each gland comprises two discrete anatomic and functional units: the adrenal cortex, which is the site for synthesis and secretion of cortisol, aldosterone, and adrenal androgens, and the medulla, which is derived from the neu-ral crest and is the site for synthesis of the catecholamines epinephrine and norepinephrine. A normal adrenal gland typically weighs between 4 and 6 g and measures approxi-mately 4 to 5 cm × 2 to 3 cm × 0.5 to 1 cm. The right adrenal is relatively pyramidal in shape, whereas the left is some-what fl attened and is more closely applied to the kidney. Grossly, the adrenals may be distinguished from the sur-rounding retroperitoneal fat by their golden-orange color, which is a result of the high intracellular lipid content. The glands have a fi brous capsule but are relatively fragile and can be easily cracked or fragmented with surgical manipulation.
right adrenal
Anteriorly, the right adrenal is partially covered by the liver and the right triangular ligament. The gland abuts the inferior vena cava (IVC) medially and may, in part, lie posterior to the lateral aspect of the vena cava. Inferiorly, the adrenal sits just above the upper pole of the kidney. The diaphragm forms the posterior and lateral boundaries of the gland.
The blood supply of the right adrenal is derived from branches of the inferior phrenic artery, the right renal artery, and the aorta [see Figure 2]. Typically, multiple small branche s enter the gland along its superior, medial, and inferior aspects. Arterial branches from the aorta generally course posterior to the vena cava before entering the adrenal. Each adrenal is drained by a single central vein. On the right, this vein is short (1 to 1.5 cm long), runs transversely, and
Financial disclosure information is located at the end of this chapter before the references.
joins the lateral aspect of the IVC. In some cases, a more superiorly located accessory adrenal vein may enter either the IVC or one of the hepatic veins. Control of the adrenal vein is the most critical aspect of right adrenalectomy in that the short course of this vessel makes it susceptible to tearing or avulsion from the IVC.
left adrenal
The spleen and tail of the pancreas overlie the anterior and medial borders of the left adrenal. The inferolateral aspect of the gland lies over the superomedial aspect of the left kidney, to which it is more closely applied than the right adrenal is to the right kidney. The inferior aspect of the adrenal is in close proximity to the renal vessels, especially the renal vein. As on the right side, the posterior aspect of the adrenal rests on the diaphragm.
The arterial blood supply of the left adrenal is similar to that of the right adrenal [see Figure 2]. The left adrenal vein is longer than the right adrenal vein and runs somewhat obliquely from the inferomedial aspect of the gland to enter the left renal vein. The inferior phrenic vein courses in a superior-to-inferior direction just medial to the adrenal and usually joins the left adrenal vein cephalad to its junction with the renal vein.
Adrenal Physiology
The adrenal cortex is the site where cortisol, aldosterone, and androgens are synthesized. These steroid hormones are all derived from cholesterol, which is converted to pregnen-elone under the infl uence of adrenocorticotropic hormone (ACTH). There are three histologic zones within the adrenal cortex: the zona glomerulosa, the zona fasciculata, and the zona reticularis. The zona glomerulosa lacks the enzyme 17a-hydroxylase, which is necessary for synthesis of cortisol and androgens; consequently, it is the exclusive site for the synthesis of aldosterone. The principal action of aldosterone is regulation of extracellular fl uid volume and sodium and potassium balance. Aldosterone is secreted in response to increased renin production via the renin-angiotensin-aldosterone pathway. Decreased pressure in the renal afferent arterioles (as a consequence of hypotension or other conditions causing reduced intravascular volume) and decreased plasma sodium levels stimulate increased renin secretion from the juxtaglomerular cells. Renin then stimu-lates conversion of angiotensinogen into angiotensin I, which is in turn cleaved by angiotensin-converting enzyme (ACE) in the lung to form angiotensin II. Angiotensin II, in addition to its direct vasoconstrictive effects, acts on the zona glomerulosa to stimulate aldosterone secretion. Aldo-sterone then stimulates renal tubular retention of sodium, which is reabsorbed in exchange for potassium and hydro-gen ion. The ultimate effect of these actions is to expand intravascular volume. In pathologic states such as primary hyperaldosteronism, the cumulative effect is chronic volume expansion and sodium retention, leading to hypertension and hypokalemia.
Scientific American SurgeryDOI 10.2310/7800.2093
02/13
gastrointestinal tract and abdomen
* The authors and editors gratefully acknowledge the contribu-tion of the previous author, Steven Hodgett, MD, to the development and writing of this chapter.
Red text is tied to a SCORE learning objective.

02/13
gastro disorders of the adrenal glands — 2
Left SuperiorAdrenal Artery
Left InferiorPhrenic Artery
Left MiddleAdrenal Arte
Left InfeAdrenal
Right InferiorPhrenic Artery
Right MiddleAdrenal Artery
Right SuperiorAdrenal Artery
Right InferiorAdrenal Artery
Left AdVein
Right AdrenalVein
Liver
Liver
Duodenum LeftKidney
LeftAdrenal
Spleen
Stomach
Vena Cava
InferiorVena Cava
AdrenalTumor
Kidney
Pancreas
Colon
Right Left
Figure 1 The relation of the adrenal glands to adjacent structures.
Figure 2 The adrenal blood supply. Multiple adrenal arteries are present; a single central adre-nal vein drains into the inferior vena cava on the right side and the renal vein on the left side.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 3
Glucocorticoids are synthesized in the zona fasciculata. Cortisol secretion is regulated by the hypothalamus, which secretes corticotropin-releasing hormone (CRH), and the pituitary, which secretes ACTH. ACTH stimulates cortisol synthesis and secretion from the adrenal gland, and high circulating cortisol levels inhibit pituitary and hypothalamic secretion of ACTH and CRH. Cortisol exerts its effects on intermediary metabolism via a wide range of cells and tissues. These effects include stimulation of hepatic gluco-neogenesis and glycogen synthesis, inhibition of protein synthesis, increased protein catabolism, and lipolysis of fat. Cortisol also inhibits peripheral uptake of glucose in most tissues (except in the liver, the brain, and red blood cells), and this inhibitory effect may cause hyperglycemia and increased insulin secretion, especially in states of chronic cortisol excess. Other effects of glucocorticoids include pro-motion of collagen loss and impairment of wound healing by inhibition of fi broblast activity, inhibition of bone forma-tion and acceleration of the development of osteoporosis, and numerous antiinfl ammatory actions. Glucocorticoids are also critical for cardiovascular stability, which helps explain why some patients with acute adrenal insuffi ciency (AI) experience cardiovascular collapse.
Adrenal androgens are synthesized predominantly in the zona reticularis. The primary androgen produced by the adrenal is dehydroepiandrostenedione (DHEA), although DHEA sulfate and androstenedione also play important roles. Peripherally, the adrenal androgens undergo conver-sion to testosterone and dihydrotestosterone. A number of different conditions may result in increased adrenal androgen production, including Cushing syndrome, adrenal carcinoma, and congenital adrenal hyperplasia. In normal males, adrenal androgens account for less than 5% of total testosterone production, but in normal females, they are the major source of androgens.
The adrenal medulla is derived embryologically from the neural crest and is the principal site for synthesis of the catecholamines epinephrine and norepinephrine. Only the adrenal medulla has the enzyme phenylethanolamine-N-methyltransferase, which is necessary for conversion of norepinephrine to epinephrine; however, norepinephrine itself may be synthesized in other chromaffi n tissues. Cate-cholamines are secreted in response to a variety of stimuli, including bleeding, trauma, exercise, hypoglycemia, angina, myocardial infarction, hypoxia, and fright. The effects of increased catecholamine secretion include vasoconstriction (alpha receptor) and increased heart rate and myocardial contractility (beta1 receptor). The effects of epinephrine include vasodilatation and bronchial dilatation, which are mediated via beta2 receptors.
Disorders of the Adrenal Cortex
primary hyperaldosteronism
Clinical Evaluation
Primary hyperaldosteronism (Conn syndrome) is now known to be a much more common cause of hypertension than was previously thought, occurring in as many as 8 to 12% of hypertensive patients.1 The diagnosis of primary hyperaldosteronism should be considered in any patient who has hypertension of early onset, hypertension that is
diffi cult to control, or hypertension with hypokalemia [see Figure 3]. Although the classic presentation is that of hyper-tension with hypokalemia, many patients with primary hyperaldosteronism have a normal or low-normal serum potassium level; indeed, current data suggest that as many as 60% of patients diagnosed with this condition—and per-haps more—were normokalemic at the time of diagnosis.2 The hypertension that results from primary hyperaldoste-ronism is moderate to severe and may be refractory to standard antihypertensive medications. Symptoms are nonspecifi c and may include headache caused by the hyper-tension. Most of the other symptoms observed are attribut-able to hypokalemia; these include muscle weakness, cramps, fatigue, and, if the hypokalemia is severe, polydipsia, polyuria, nocturia, and even paralysis.
The pathophysiology of primary hyperaldosteronism primarily consists of increased aldosterone secretion by the adrenal gland, which leads to increased sodium retention, expansion of intravascular fl uid volume, and suppression of renin secretion by the kidney. Aldosterone also promotes the exchange of sodium for potassium and hydrogen ion in the distal tubule, which leads to potassium depletion and alkalosis. The alkalosis may be aggravated by the movement of hydrogen ions into the cells to replace intracellular potassium. Signifi cant potassium depletion may also be accompanied by mild glucose intolerance.
Figure 3 Algorithm illustrating diagnostic evaluation of the patient with suspected primary hyperaldosteronism. CT = computed tomo-graphy; PAC = plasma aldosterone concentration; PRA = plasma renin activity.
Measure plasma aldosterone concentrationand assess plasma renin activity. PAC:PRAratio > 25–30, with PAC > 15 ng/dL andPRA < 0.2–0.5 ng/mL/hr, is consistent withprimary hyperaldosteronism.
Confirm diagnosis by means of suppressiontesting with oral or IV salt loading.
Primary hyperaldosteronism is suspected
Patient does not have primary hyperaldosteronism.
Aldosterone is suppressible
Treat medically.
No lateralizationis apparent
Perform laparoscopic adrenalectomy.
Lateralization (aldosterone:cortisol > 4 times higher on one side than on the other) is apparent
Perform CT of adrenal with thin(3 mm) cuts.
Aldosterone is not suppressible(urinary aldosterone > 12 µg/24 hr;plasma aldosterone > 10 ng/dL )
Perform adrenal vein sampling.
Patient has microadenoma (< 1 cm),bilateral nodules, or normal adrenals or is older (> 40–50 yr)
Perform laparoscopicadrenalectomy.
Patient has unilateralmacroadenoma (> 1 cm)and is young (< 40–50 yr)
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 4
Investigative Studies
Endocrine practice guidelines are available for the diagno-sis and management of primary hyperaldosteronism.3 The initial biochemical evaluation for suspected primary hyperaldosteronism should consist of measurement of the plasma aldosterone concentration (PAC) and assessment of plasma renin activity (PRA). A PAC-to-PRA ratio greater than 25 to 30, in conjunction with suppressed PRA (< 0.2 to 0.5 ng/mL/hr) and a PAC higher than 15 ng/dL, is consis-tent with primary hyperaldosteronism. The patient should not be on spironolactone during testing. The diagnosis may be confi rmed by means of suppression testing with either oral salt loading or intravenous (IV) administration of saline. With oral salt loading, hypokalemia is corrected and the patient is placed on a high-salt diet for 3 days. On day 3, a 24-hour urine collection is obtained for measurement of sodium, potassium, creatinine, and aldosterone con-centrations. Patients with primary hyperaldosteronism should have a 24-hour urine aldosterone value higher than 12 µg/24 hr.1 Plasma aldosterone levels should be higher than 10 ng/dL after IV salt loading.
Once the diagnosis of primary hyperaldosteronism has been confi rmed biochemically, the next step is to identify the cause or determine the subtype [see Table 1]. Historically, aldosterone-secreting adenomas (aldosteronomas) have accounted for approximately 60% of cases, and idiopathic hyperaldosteronism from bilateral cortical hyperplasia has accounted for the bulk of the remaining cases. In the past few years, however, this picture has begun to change: several series in which hypertensive patients were screened on the basis of aldosterone-to-renin ratios found that only 30 to 50% of patients with primary hyperaldosteronism had aldosteronomas, whereas 50 to 70% had bilateral adrenal hyperplasia.2 It is important to distinguish between these two conditions because aldosteronomas are treated surgi-cally and idiopathic hyperaldosteronism is treated medical-ly. Aldosterone-producing carcinomas are rare and account for fewer than 1% of cases of primary hyperaldosteronism.
Glucocorticoid-remediable hyperaldosteronism (also known as familial hyperaldosteronism type 1) is a rare type of hyperaldosteronism that is inherited in an autosomal dominant pattern. This condition is due to a chimeric gene that results from fusion of two components: (1) the promote r region for the enzyme 11a-hydroxylase (CYP11B1), which catalyzes the conversion of deoxycortisol to cortisol, and (2) the gene that codes for aldosterone synthesis (CYP11B2). As a result, aldosterone synthesis is primarily dependent on activation by ACTH and is suppressed by exogenous glucocorticoid administration. Familial hyperaldosteronism type 1 has been associated with a signifi cant increased risk of hemorrhagic stroke. Familial hyperaldosteronism type 2
is associated with the development of both aldosteronomas and idiopathic hyperaldosteronism.
The initial step in subtype determination should be to perform cross-sectional imaging to look for an adrenal adenoma. Aldosteronomas are generally small, typically measuring no more than 1 to 2 cm in diameter. Thin-section imaging with computed tomography (CT) possesses excel-lent spatial resolution for small adrenal nodules and is therefore the preferred imaging modality for this purpose [see Figure 4]. Magnetic resonance imaging (MRI) may also be used but is more costly, and the images can be harder for clinicians to interpret. Findings on CT or MRI may include a unilateral macroadenoma (> 1 cm) or a microadenoma (< 1 cm) with a normal contralateral adrenal gland, bilateral adrenal nodules or bilateral adrenal thickening, and bilateral normal glands.
Patients who are young (age < 40 to 50 years) with a uni-lateral macroadenoma and a normal contralateral adrenal gland may be considered for adrenalectomy, without any need for further testing. For all other patients, adrenal vein sampling is recommended to differentiate aldosteronoma from idiopathic hyperaldosteronism. Some authors use adrenal vein sampling in all patients regardless of cross-sectional imaging fi ndings and age. In this procedure, aldo-sterone and cortisol levels are measured from both adrenal veins and from the IVC. ACTH is usually infused during the procedure to minimize stress-related fl uctuations in cortisol and aldosterone levels. An aldosterone-to-cortisol ratio that is at least four times greater on one side than on the other is considered diagnostic of a unilateral source of increased aldosterone production (i.e., an aldosteronoma) and constitutes an indication for adrenalectomy [see Table 2].
Adrenal vein sampling is a technically demanding procedure that should be carried out only by radiologists who have considerable experience with it. The value of this procedure was demonstrated in a 2004 study of 194 patients with hyperaldosteronism at the Mayo Clinic.4 In this study,
Table 1 Subtypes of Primary Hyperaldosteronism
Aldosterone-producing adenomaIdiopathic hyperaldosteronismAldosterone-producing adrenal carcinomaFamilial hyperaldosteronism Type I (glucocorticoid remediable) Type II (aldosteronoma or carcinoma idiopathic)
Figure 4 Computed tomographic scan showing a right adrenal aldosteronoma (arrow).
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 5
adrenal vein sampling identifi ed a unilateral source of increased aldosterone production in 87 of 176 patients with the following CT fi ndings: a normal CT scan (24 of 58), a unilateral micronodule (24 of 47), a unilateral macronodule (21 of 32), bilateral micronodules (16 of 33), and bilateral macronodules (2 of 6). If the treating physicians had relied on CT scan fi ndings alone, 42 patients (21.7%) would have been inappropriately excluded from consideration for adrenalectomy, and an additional 48 patients (24.7%) who showed no lateralization on adrenal vein sampling might have been subjected to an unnecessary operation. In a more recent study, a lateralizing source of increased aldosterone production was found in only 1 of 22 patients (5%) with bilaterally normal adrenals on CT, 3 of 9 (33%) with bilateral nodules or thickening, and 27 of 39 (69%) with a unilateral nodule. However, all fi ve patients under age 40 who had a solitary unilateral nodule greater than 1 cm and normal contralateral adrenal had aldosteronomas proven on vein sampling.5 These results argue for liberal use of adrenal vein sampling in middle-aged and older patients with primary hyperaldosteronism.
Management
For patients with an aldosteronoma, the treatment of choice is laparoscopic adrenalectomy. Before the operation, hypertension should be controlled and hypokalemia cor-rected. The aldosterone antagonist spironolactone may be useful for preoperative control of blood pressure. Adrenal-ectomy cures hypertension in as many as 30 to 80% of patients and improves blood pressure control in the remain-der.6–8 The reasons for failure to cure hypertension in some patients may be related to the effects of long-standing hypertension from the hyperaldosteronism, more advanced age, or coexisting essential hypertension. In two follow-up studies, the best predictors of resolution of hypertension after adrenalectomy were the use of less than two antihyper-tensive medications preoperatively, a body mass index of 25 kg/m2, duration of hypertension of 6 years or less, and female sex.6,9 Hypokalemia should be corrected in virtually 100% of patients.
For patients with idiopathic hyperaldosteronism, treat-ment is medical, consisting of dietary sodium restriction and potassium supplementation. As in patients with aldoster-onomas, spironolactone is effective in controlling hyperten-sion and hypokalemia. However, it also blocks testosterone synthesis and peripheral androgen action and thus may
have undesirable side effects—namely, impotence, decreased libido, and gynecomastia. Eplerenone is a newer aldosterone receptor antagonist that exhibits little binding to androgen receptors and therefore may not have the same side effects as spironolactone.
secondary hyperaldosteronism
In secondary hyperaldosteronism, an elevation of plasma aldosterone occurs in response to increased renin produc-tion by the kidney. It may be caused by a variety of conditions, including renovascular hypertension [search the
], reduced intravascular volume (from congestive heart failure, nephro-sis, or cirrhosis), Bartter syndrome, and normal pregnancy. Adrenal function is normal in such cases, and treatment should be directed at the underlying disorder.
cushing syndrome
Cushing syndrome is an uncommon condition, with an annual incidence of one to 10 cases per million. It may be caused by ACTH-secreting pituitary tumors, by ectopic ACTH-secreting tumors, or by cortisol-producing adrenal tumors. Of these conditions, ACTH-secreting tumors of the pituitary are the most common cause of Cushing syndrome, accounting for approximately 65 to 70% of cases. Ectopic production of ACTH accounts for between 10 and 15% of cases; small cell lung carcinomas are the most common ectopic ACTH-secreting tumors (50% of ectopic cases), but thymic tumors, carcinoid tumors, and medullary thyroid carcinomas may also give rise to this syndrome. Adrenal tumors account for about 20% of cases of Cushing syndrome. Cortisol-producing adenomas are the most common cause of adrenal Cushing syndrome, followed by adrenocortical carcinomas (ACCAs). Primary nodular adrenal hyperplasia is a rare cause of adrenal Cushing syndrome.
Clinical Evaluation
A number of characteristic clinical symptoms and signs are associated with Cushing syndrome [see Table 3]. Obesity is the most consistent feature and is typically distributed
Table 2 Adrenal Vein Sampling Results in a Patient with Primary Hyperaldosteronism
Sampling Site
Aldosterone Level
(ng/dL)
Cortisol Level
(µg/dL)
Aldosterone-to-Cortisol
Ratio
Aldoste-rone
Ratio*
Right adrenal vein 480 346.7 1.38 16.9
Left adrenal vein 33,765 1,448 23.3
Inferior vena cava 67.0 24.1 2.78
*Defi ned as the aldosterone-to-cortisol ratio in the left adrenal vein divided by the aldosterone-to-cortisol ratio in the right adrenal vein. The results show a lateraliz-ing source of increased aldosterone production from the left adrenal gland.
Table 3 Symptoms and Signs of Cushing Syndrome
Symptoms Weight gain Florid complexion Oligomenorrhea or amenorrhea Decreased libido Spontaneous bruising Muscle weakness and fatigue Mood swings, depression Insomnia Signs Obesity (central distribution) Facial fullness (moon facies) Buffalo hump Prominent supraclavicular fat pads Telangiectasias Skin striae (violaceous) Osteopenia and osteoporosis Hirsutism*
*May be associated with adrenocortical carcinoma.
Scientific American Surgery
publication for renovascular hypertension and stenosis

02/13
gastro disorders of the adrenal glands — 6
in a central pattern around the face, the trunk, the neck, and the abdomen. Patients may have especially prominent supraclavicular fat pads and fat over the upper back (so-called buffalo hump). Skin changes are common and include easy bruising, increased fragility, and skin striae (often pigmented). Facial plethora is also frequently present. Generalized skin hyperpigmentation is seen more often in patients with ectopic ACTH production. Hirsutism from increased secretion of adrenal androgens may be present in women, but virilizing features are more often associated with ACCA. Increased production of adrenal androgens also causes gonadal dysfunction, manifested by amenorrhea and infertility. In men, increased cortisol secretion may result in reduced libido, decreased body hair, and testicular atrophy.
The initial goal in the evaluation of a person who may have Cushing syndrome is to determine whether a state of increased cortisol production exists. If it does, subsequent testing should be undertaken (1) to determine whether the cause is ACTH dependent (a pituitary or ectopic ACTH-producing tumor) or ACTH independent (a primary adrenal lesion) and (2) to locate the source [see Figure 5].
Investigative Studies
Detection of Cushing syndrome When Cushing syn-drome is suspected on clinical grounds, the initial diagnostic tests should be measurement of 24-hour urinary free cortisol and an overnight dexamethasone suppression test [see Figure 5]. Urinary free cortisol levels are elevated in more than 90% of patients with Cushing syndrome.10 False positive elevations can, however, occur as a result of the use of medications (e.g., barbiturates or phenytoin), obesity, serious illnesses, or depression. Furthermore, mild degrees of hypercortisolism may be missed in a single 24-hour collection because of variation in cortisol secretion rates.
Dexamethasone is a potent glucocorticoid that suppresses adrenal production of corticosteroids in normal persons but not in persons with Cushing syndrome. To screen for this
syndrome, the low-dose dexamethasone suppression test is usually employed. A single 1 to 3 mg dose of dexametha-sone is administered orally at 11:00 pm, and the plasma cortisol level is measured at 8:00 am. In normal persons, the 8:00 am plasma cortisol levels are typically lower than 1.8 µg/dL, whereas in patients with Cushing syndrome, the cortisol levels are usually higher than 10 µg/dL. If both the dexamethasone test and the urinary free cortisol measure-ment yield normal results, the patient does not have Cush-ing syndrome. A notable feature of Cushing syndrome is the loss of the normal diurnal variation in cortisol; however, because of variation in levels, random cortisol determina-tions cannot be relied on in making the diagnosis. Late-night (11:00 pm) salivary cortisol levels have now been found to be highly sensitive and specifi c in screening for Cushing syndrome and, as a result, may see increasing use in the future.11,12
Levels of 17-hydroxycorticosteroid and 17-ketosteroid (urinary metabolites of cortisol) may be measured, but these levels are less useful in the diagnosis of Cushing syndrome than urinary free cortisol levels are. If the patient exhibits virilizing features, a plasma testosterone level should be obtained.
Differentiation of ACTH-dependent causes from inde-pendent causes Once the diagnosis of Cushing syndrome is established, a plasma ACTH level should be obtained to differentiate ACTH-dependent causes of the syndrome (i.e., pituitary and ectopic ACTH-secreting tumors) from ACTH-independent causes (i.e., adrenal lesions). In patients with pituitary Cushing syndrome, ACTH levels are typically nor-mal or only moderately elevated (> 20 pg/mL). In patients with ectopic ACTH-secreting tumors, ACTH levels are usu-ally higher, although there is some overlap with the levels measured in patients with Cushing disease. In patients with Cushing syndrome caused by an adrenocortical tumor, plasma ACTH levels are suppressed (< 5 pg/mL).
If it appears that the syndrome has an ACTH-dependent cause, the next step is to determine whether the cause is of pituitary or ectopic origin. Historically, the high-dose dexa-methasone suppression test has generally been employed for this purpose. The rationale for this test is that high doses of glucocorticoids will suppress ACTH secretion from most ACTH-secreting pituitary adenomas but not from ectopic ACTH-secreting tumors. Dexamethasone is administered either in eight doses over 2 days (2 mg every 6 hours) or in a single oral 8 mg dose. Cortisol levels (in plasma for the single-dose version, in urine for the 2-day version) are measured before, during, and after administration of dexa-methasone. With either version of the test, if the patient has pituitary Cushing syndrome, the plasma or urinary cortisol levels should be markedly suppressed (< 50% of the basal level), whereas if the patient has an ectopic ACTH-producing tumor, the cortisol levels should generally be unchanged. However, between 20 and 30% of patients with mildly increased ACTH secretion and pituitary Cushing syndrome do not show suppression of steroid production to a level below 50% of baseline, and some patients with ACTH-secreting tumors do show this degree of suppression of plasma or urinary steroids. Therefore, the overall diag-nostic accuracy of high-dose dexamethasone suppression
Figure 5 Algorithm illustrating diagnostic evaluation of the patient with suspected Cushing syndrome. ACTH = adrenocorticotropic hormone; CT = computed tomographic; MRI = magnetic resonance imaging.
Measure 24 hr urinary free cortisol leveland perform overnight dexamethasonesuppression test.
Cushing syndrome is suspected
Evaluate patient for pituitaryCushing syndrome (pituitary MRI) or ectopic ACTH-secreting tumor (chest/abdomen CT, octreotide scanning).
Plasma ACTH level is elevatedor in upper normal range
Obtain abdominal CT scanto localize adrenal lesion.
Plasma ACTH level is esuppressed (< 5 pg/mL)
Patient does not haveCushing syndrome.
Initial test results are normal
Measure plasma ACTH level.
Initial test results are abnormal
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 7
Most patients with SCS are detected during workup of an adrenal incidentaloma, usually by screening with an over-night dexamethasone test. Failure to suppress with dexa-methasone should be evaluated further as outlined above for Cushing syndrome. Patients with SCS are at increased risk for AI after adrenalectomy; therefore, they should be given perioperative glucocorticoids intravenously until they can take oral replacement. Replacement therapy may be necessary for up to 6 to 12 months until the pituitary-adrenal axis recovers.
disorders of excess adrenal androgen production
Excess androgen production may be either acquired (as in Cushing syndrome or ACCA) or congenital (as in congenital adrenal hyperplasia). Congenital adrenal hyperplasia com-prises a group of autosomal recessive disorders character-ized by defective synthesis of cortisol. This defect in cortisol synthesis results in increased ACTH production, which, in turn, leads to adrenal hyperplasia and increased production of adrenal androgens and androgen precursors. The most common variant of congenital adrenal hyperplasia is 21a-hydroxylase defi ciency, which accounts for about 95% of cases. 21a-Hydroxylase defi ciency may be divided into three main subtypes: classic salt wasting, classic non–salt wasting, and nonclassic. The two classic subtypes generally are more severe and typically present early in life (i.e., in infancy or early childhood) with virilizing features and AI. The nonclassic subtype tends to be milder: the androgen excess is less pronounced, and there is no cortisol defi ciency. As many as 80% of patients with the classic salt-wasting subtype experience severe electrolyte and fl uid losses as a result of an associated defect in aldosterone production.
Excess adrenal androgen production from an androgen-secreting tumor can lead to testicular atrophy (in men) or to hirsutism, acne, and irregular or absent menses (in women). Women may also experience other virilizing features, such as male pattern baldness, clitoral enlargement, increased facial hair, and deepening of the voice. Biochemically, the diagnosis is established by measuring plasma levels of androgens, including DHEA, DHEA sulfate, testosterone, and dihydrotestosterone. Other causes of hirsutism and virilism that must be considered in women include the polycystic ovary syndrome and androgen-secreting ovarian tumors.
adrenocortical carcinoma
ACCA is a rare tumor: the estimated annual incidence ranges from 0.5 to 2 per 1 million adults. The age distribu-tion is bimodal, with peak occurrences noted in childhood and in the fourth and fi fth decades of life.18
Clinical Evaluation and Investigative Studies
ACCAs are typically large (> 6 to 8 cm) at presentation, and most patients present with advanced (i.e., stage III or IV) disease [see Table 4]. In two large series, the mean tumor size at diagnosis was 12 cm and 15 cm.19,20 The increased use of imaging in clinical practice in recent years has not led to detection of ACCA at an earlier stage or impacted patient survival.21,22 The clinical presentation may be related to the large size of the tumor (e.g., abdominal or back pain or other mass effects) or to increased secretion of one or more
testing is only 70 to 80%. Other tests, such as the CRH stim-ulation test, are available for differentiating among the possible causes of ACTH-dependent Cushing syndrome, but at present, they are less commonly employed.
Localization Once biochemical evaluation is complete, the next step is radiographic localization of the source of the Cushing syndrome. If adrenal Cushing syndrome is suspected, abdominal cross-sectional imaging with CT is recommended. If a pituitary source is suspected, MRI of the pituitary should be the initial imaging test. Pituitary MRI with gadolinium enhancement will identify an adenoma in more than 60% of patients with pituitary Cushing syndrome. However, as much as 10% of the general population may have an incidental pituitary mass that is not functional, although these lesions are typically small (< 5 mm in dia-meter). If MRI is not conclusive, measurement of inferior petrosal sinus ACTH levels is recommended as the most direct method of differentiating pituitary from nonpituitary causes of ACTH-dependent Cushing syndrome. In this test, ACTH levels are simultaneously measured peripherally and in the two inferior petrosal sinuses both before and after IV administration of CRH (100 µg). An inferior petrosal sinus–to–periphery ACTH ratio that is higher than 3.0 is diagnostic of pituitary Cushing syndrome; a ratio that is lower than 1.8 is indicative of an ectopic ACTH-secreting tumor.13 In experienced hands, this procedure has a sensitivity and specifi city of 80 to 90%.10,13 Ectopic ACTH-producing tumors are most often detected by means of CT scanning or radionuclide imaging with indium-111–labeled octreotide analogues, which detect tumors that express somatostatin receptors.
Subclinical Cushing Syndrome
Subclinical Cushing syndrome (SCS) is characterized by abnormalities in cortisol secretion in the absence of overt signs of classic Cushing syndrome. Such fi ndings have been observed in up to 20% of adrenal incidentalomas.14,15 The array of biochemical abnormalities that defi ne subclinical hypercortisolism include nonsuppressibility of cortisol secretion with dexamethasone, loss of the diurnal variation in cortisol secretion, low or suppressed plasma ACTH levels, and blunted response of ACTH to CRH. Twenty-four-hour urine free cortisol levels are elevated in only about 50% of patients with SCS, and the degree of elevation is usually mild.
The natural history of SCS has not been carefully studied, but these patients do have a higher incidence of hyperten-sion, obesity, and diabetes than controls. In one series, the progression to overt Cushing syndrome at 1 year was 12.5%.16 Recently, outcomes were compared in 45 patients with SCS randomized to undergo adrenalectomy or conser-vative management.17 Assessment was carried out yearly with a mean follow-up of 7.7 years. In the adrenalectomy group, diabetes normalized or improved in 62.5% of patients, hypertension in 67%, hyperlipidemia in 37.5%, and obesity in 50%. In contrast, some worsening of diabetes, hypertension, and hyperlipidemia was observed in the conservatively managed group. No changes in osteoporosis parameters were seen in either group. These results suggest that adrenalectomy results in improved outcomes over conservative management in patients with SCS.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 8
steroid hormones. Approximately 60% of ACCAs are hyper-functioning,23 about 30% secrete cortisol and give rise to Cushing syndrome, and 20% secrete androgen and have virilizing effects. A mixed hormone secretion pattern is frequently present. Adrenal cancers that secrete estrogen or aldosterone exist but are much less common.
Biochemical evaluation of ACCA patients should consist of testing for hypercortisolism [see Cushing Syndrome, above] and measurement of adrenal androgens (i.e., DHEA sulfate and testosterone).
Management
ACCA is an aggressive tumor that may spread locally to regional lymph nodes, adjacent organs, and distant sites (including the liver, the lungs, and bones). Complete surgi-cal resection offers the only chance for a cure and is the best predictor of clinical outcome.18,24 Standardization of surgical resection to include fi rst-order lymph nodes (ipsilateral renal hilar, celiac, and para-aortic and/or paracaval) has been recommended, but nephrectomy is not indicated unless the kidney is directly involved.25 Overall 5-year actu-arial survival rates after complete resection range from 32 to 48%.18 Patients whose tumors are incompletely resected (i.e., who have residual local or distant gross disease) have a median survival of less than 1 year. The presence of tumor thrombus in the renal vein or IVC is not a contraindication for surgical resection provided that the tumor can be completely excised.18,23
Treatment options for patients with unresectable or recur-rent ACCA are limited. Locally recurrent tumors may be resected surgically. Radiation therapy is generally ineffec-tive, although a few investigators have reported tumor response rates as high as 42%.25 Mitotane is toxic for adreno-cortical cells and is the most specifi c chemotherapeutic agent available for the treatment of ACCA. Objective tumor response rates as high as 25% have been reported, but com-plete responses to mitotane are rare,23 and treatment is often limited by gastrointestinal and central nervous system side effects. In addition, because of mitotane’s toxic effects on normal adrenal cortical function, patients being treated for ACCA with this agent require glucocorticoid replacement. Mitotane has occasionally been used as adjuvant therapy after resection of ACCA, but the data are inconclusive. The results of conventional cytotoxic chemotherapy in ACCA patients have been disappointing. The poor response rates to chemotherapy may be related to high expression of the multiple drug resistance gene MDR1; this results in high lev-els of P-glycoprotein, which acts as a drug effl ux pump.23,26
adrenal insufficiency
AI may be either primary or secondary. In industrialized countries, the primary cause of spontaneous AI is auto-immune adrenal disease; in the developing world, it is tuberculosis.27 Other causes of primary AI include bilateral adrenal hemorrhage, adrenal metastases, adrenal leukodys-trophy, and certain viral or fungal infections. The primary cause of secondary AI is suppression of ACTH secretion and normal adrenal cortical function as a result of long-term steroid administration. Several weeks of exogenous admin-istration of glucocorticoids are required before AI develops upon steroid withdrawal.27
Clinical Evaluation
Chronic AI (Addison disease) is characterized by weak-ness, chronic fatigue, anorexia, loss of appetite, abdominal pain, nausea, and diarrhea. Hyperpigmentation of the skin from chronic hypersecretion of melatonin (a product of the ACTH precursor pro-opiomelanocortin) may be apparent as well. Many patients with primary AI also have an associated mineralocorticoid defi ciency, the symptoms and signs of which include salt craving, postural hypotension, and elec-trolyte abnormalities. Because many of the symptoms of AI are nonspecifi c, patients may go undiagnosed for a long time. The symptoms of primary AI are usually more severe than those of secondary AI.
In patients with inadequate adrenal reserve, an acute adrenal crisis may be precipitated by the stress imposed by surgery, trauma, infection, or dehydration and may result in vascular collapse with hypotension, shock, and, if untreated, death. Consequently, patients with unexplained cardiovas-cular collapse in whom this diagnosis is suspected should be treated empirically with replacement corticosteroids.
Investigative Studies
Laboratory abnormalities associated with AI include hyponatremia, hyperkalemia (in primary AI), hypoglyce-mia, and azotemia, with increased blood urea nitrogen and creatinine concentrations. The diagnosis is confi rmed by measurement of plasma cortisol and ACTH levels. In primary adrenal insuffi ciency, 8 am plasma cortisol levels are typically low (< 3 µg/dL)28 and plasma ACTH levels are high (> 100 pg/mL). Plasma ACTH levels are usually low or inappropriately normal if pituitary failure or hypothalamus pathology is the cause.27 The ACTH stimulation test may be necessary to establish the diagnosis in patients with partial AI or to assess recovery of the pituitary-adrenal function after treatment of Cushing syndrome. For this test, 250 µg of synthetic ACTH is administered intravenously, and plasma cortisol levels are measured at 0, 30, and 60 minutes. A serum cortisol level higher than 18 µg/dL at either 30 or 60 minutes is considered a normal response.
Management
AI is treated with exogenously administered glucocorti-coids [see Table 5]. If the patient is in an acute adrenal crisis, hydrocortisone should be given in a dosage of 100 mg IV every 8 hours. If the patient requires oral replacement therapy for chronic AI, hydrocortisone should be given in a dosage of 10 to 12.5 mg/m2/day.27 Hydrocortisone (20 to 30 mg/day) is often preferred to other steroids because its
Table 4 Staging of Adrenocortical Carcinoma23
Stage Description
I T1 (< 5 cm) N0 M0
II T2 (> 5 cm) N0 M0
III T3 (locally invasive) or T1–2 N1 M0
IV T4 (invasion of adjacent organs) or any T with distant metastases (M1)
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 9
short half-life (8 to 12 hours) more closely mimics the nor-mal circadian rhythm of cortisol secretion; however, it must be administered twice or three times daily, whereas predni-sone (equivalent dose, 5 mg/day) may be administered once or twice daily. For patients who are on long-term steroid therapy, outcomes after surgery appear to be essentially the same whether they received their normal replacement doses orally or whether they received stress doses intravenously.29 Patients who have primary AI or have undergone bilateral adrenalectomy should also receive mineralocorticoid therap y (fl udrocortisone 0.05 to 0.2 mg/day).
Disorders of the Adrenal Medulla
pheochromocytoma
Pheochromocytomas (often referred to as pheos) are catecholamine-producing tumors that arise from chromaffi n tissue.30 The majority (85 to 90%) develop in the adrenal gland, but some occur at extra-adrenal sites. These tumors have their peak incidence during the fourth and fi fth decades of life, and they affect males and females with equal frequency. The prevalence of pheochromocytoma in hyper-tensive patients is approximately 0.1 to 0.5%. Clinically silent pheochromocytomas may be present in as many as 10% of patients who present with an adrenal incidentaloma, and in some series, 30 to 40% of all pheochromocytomas present as incidentalomas.31,32 Several features of pheochro-mocytomas have been characterized by a 10% frequency of distribution: 10% are extra-adrenal, 10% are bilateral, 10% occur in children, 10% are familial, and 10% are malignant. Some more recent series, however, have reported lower percentages of malignant pheochromocytomas.33,34 Because extra-adrenal pheochromocytomas (also referred to as paragangliomas) lack the enzyme phenylethanolamine-N-methyltransferase (PNMT), they can secrete norepinephrine but not epinephrine.
Clinical Evaluation
The clinical features of pheochromocytoma are related to the effects of increased secretion of norepinephrine and epi-nephrine.30 Hypertension is the most consistent feature and may be either paroxysmal or sustained. Paroxysmal hyper-tension can be severe and may be associated with “spells” consisting of pounding in the chest, tachycardia, headache, anxiety, and pallor; these spells are related to catecholamine surges. Other symptoms that may be noted include temper-ature elevation, fl ushing, and sweating, and some patients experience a feeling of marked anxiety and an impending
sense of doom. Most attacks are short and last less than 15 minutes. The paroxysms may occur spontaneously, or they may be precipitated by postural changes, vigorous exercise, sexual intercourse, alcohol, and the use of certain drugs (e.g., histamine, tricyclic antidepressants, and meto-clopramide) or anesthetic agents.
Some patients with pheochromocytoma present with an extreme hypertensive crisis that may result in severe headaches, diaphoresis, visual changes, acute myocardial infarction, cardiac dysrhythmias, congestive heart failure, pulmonary edema, or even stroke. Sudden death has been reported in patients with unsuspected pheochromocytomas who have undergone percutaneous biopsy of the tumor35,36 or surgical procedures for other indications. Hypertensive emergencies are treated with IV esmolol, phentolamine (or sodium nitroprusside), or both.
Pheochromocytoma should be suspected in any patient with severe hypertension, any patient with hypertension that is episodic or associated with spells, any hypertensive pediatric patient, any patient with a family history of pheo-chromocytoma or multiple endocrine neoplasia type 2A (MEN 2A) or 2B (MEN 2B), and any hypertensive patient with medullary thyroid carcinoma.
Investigative Studies
Laboratory tests The diagnosis of pheochromocytoma is established by demonstrating elevated levels either of catecholamines and metabolites (metanephrines) in urine or of fractionated metanephrines in plasma.37,38 The urinary vanillylmandelic acid (VMA) concentration is the least specifi c test because of the frequency of false positive results caused by ingestion of related foods (e.g., coffee, tea, and raw fruits) or drugs (e.g., alpha-methyldopa) and is no longer routinely used. Because the plasma fractionated metanephrine concentration is both sensitive for pheochro-mocytoma and considerably simpler than a 24-hour urine collection, it is the preferred initial screening test in many institutions; however, some investigators have found that measurement of 24-hour urinary catecholamine and meta-nephrine levels yields fewer false positive results.37 In most cases, abnormal plasma metanephrine and norepinephrine levels should be confi rmed by measurement of urinary catecholamine and metanephrine concentrations. In the rare case where the biochemical diagnosis is diffi cult, direct measurement of plasma catecholamine levels during a hypertensive episode may be useful.
Certain agents may interfere with biochemical testing for pheochromocytoma, including iodine-containing contrast media, labetalol, tricyclic antidepressants, and levodopa.39 Major stress (e.g., from a recent stroke, a major operation, obstructive sleep apnea, or renal failure) may also affect cat-echolamine and metabolite levels. Because of the sensitivity of current tests and the risk of blood pressure alterations, provocative testing with agents such as glucagon or hista-mine and suppression testing with clonidine are no longer commonly used for diagnosis of pheochromocytoma.
Imaging Given that only 2 to 3% of pheochromocyto-mas are found outside the abdomen, localization of suspecte d tumors should begin with abdominal CT or MRI.38 The uniquely bright appearance pheochromocytomas typically
Table 5 Equivalent Dosages for Commonly Used Glucocorticoids21,22
GlucocorticoidRelative Potency
Dose Equivalent (mg/day)
t½ (hr)
Hydrocortisone 1 20 8–12
Prednisone 4 5 18–36
Methylprednisolone 5 4 18–36
Dexamethasone 25–50 0.5 36–54
t½ = half-life.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 10
exhibit on T2-weighted MRI sequences [see Figure 6] makes MRI the preferred imaging modality in many institutions. Another option is scintigraphy with iodine-labeled metaiodobenzylguanidine (I-MIBG). MIBG labeled with iodine-131 or 123I selectively accumulates in chromaffi n tissues but does so more rapidly in pheochromocytomas than in normal adrenal medullary tissue. Multi-institutional experience with 131I-MIBG imaging for pheochromocytomas has found this modality to have an overall sensitivity of 77 to 90% and a specifi city of 96 to 100%.40 123I-MIBG is now available for use and appears to have greater sensitivity than does 131I-MIBG scintigraphy. Indium-labeled octreotide scin-tigraphy has also been used to localize pheochromocytomas but has much less sensitivity for benign pheochromocyto-mas than does MIBG and should be reserved for cases in which all other imaging studies are inconclusive.41 I-MIBG scintigraphy is most useful for localizing extra-adrenal tumors that are not visualized by conventional imaging modalities and for following patients with malignant pheochromocytomas. Its main disadvantages are its greater complexity and cost (in comparison with other imaging techniques), the need to block thyroid uptake with oral iodine, and the fact that some medications interfere with pharmacologic uptake of the tracer. I-MIBG is not warranted in patients with uncomplicated pheochromocytomas that are localized on CT or MRI as it is expensive and rarely alters treatment in this setting.42,43
Pharmacologic Preparation for Operation
Once the diagnosis of pheochromocytoma has been estab-lished biochemically and radiographically, the next step is to prepare the patient for adrenalectomy pharmacologically so as to prevent an intraoperative hypertensive crisis. Preop-erative alpha blockade with phenoxybenzamine is initiated, usually starting at a dosage of 10 mg twice daily, which is then gradually increased to a total of 60 to 90 mg/day in divided doses until hypertension is controlled and the patient is mildly orthostatic. As alpha blockade progresses,
fl uids should be administered liberally to fi ll the expanded intravascular space. If the patient has marked tachycardia or dysrhythmia, beta blockade with atenolol or metoprolol may also be required. Beta blockade should never be initiated until alpha blockade has fi rst been achieved because unopposed alpha-receptor stimulation can induce a hypertensive crisis and acute cardiac failure.
Associated Inherited Syndromes
Pheochromocytomas may occur in the setting of a number of different inherited endocrine tumor syndromes [see Table 6]. Of these, the ones most commonly associated with pheochromocytoma are von Hippel-Lindau (VHL) syndrome and the MEN type 2 syndromes.44 In addition to pheochromocytoma, VHL syndrome is characterized by bilateral renal tumors and cysts, cerebellar and spinal hemangioblastomas, retinal angiomas, pancreatic cysts and tumors, epididymal cystadenomas, and inner ear canal tumors. MEN 2A and 2B are associated with medullary thyroid carcinoma in 100% of cases. The incidence of pheo-chromocytomas in MEN 2A and 2B patients ranges from 30 to 50%. MEN type 2 arises from mutations in the ret proto-oncogene on chromosome 10. Specifi c ret mutations associated with pheochromocytoma occur predominantly on codons 618 and 634.44 In addition, familial paraganglio-mas of the neck are now known to be associated with muta-tions in the succinate dehydrogenase subunit B (SDHB) and succinate dehydrogenase subunit D (SDHD) genes,45,46 which encode mitochondrial enzymes involved in oxidative phosphorylation.47
Familial pheochromocytoma may be more common than was previously thought. A 2002 study found mutations in 24% of patients who presented without a known familial pheochromocytoma association: 30 had mutations of the VHL gene, 13 of ret, 11 of the SDHD gene, and 12 of the SDHB gene.48 These fi ndings suggest the need for careful screening for a familial disorder in this setting.
Figure 6 Magnetic resonance image showing a left adrenal pheo-chromocytoma (arrows). Pheochromocytomas typically appear bright on T2-weighted images.
Table 6 Inherited Pheochromocytoma Syndromes
Syndrome Mutation ChromosomeFrequency
(%)*
MEN 2A and 2B ret (proto-oncogene)
10q11 30–50
von Hippel-Lindau syndrome
VHL (tumor suppressor gene)
3p25 15–20
Neurofibromatosis NF1 17q11 1–5
Familial paraganglioma and extra-adrenal pheochromocytoma
SDHD† 11q23 —
SDHB† 1p35-36 —
SDHC† 1q21 —
MEN = multiple endocrine neoplasia.*Clinical incidence of tumors within persons affected by the mutation.†SDHD, SDHB, and SDHC designate specifi c mutations within the succinate dehy-drogenase gene (SDH). Patients with SDHD mutations are more likely to have head and neck paragangliomas, whereas SDHB mutations are more likely to be associ-ated with extra-adrenal pheochromocytomas and malignant tumors.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 11
Management
Patients undergoing adrenalectomy for pheochromocytom a should be monitored intraoperatively via an arterial line. Although pheochromocytomas are highly vascular, and the larger ones can be quite challenging to remove, a laparo-scopic approach is feasible in most cases. Intraoperative exacerbations of hypertension may be managed with esmolol or nitroprusside.
After resection, patients who have signifi cant cardiac dis-ease or who exhibited signifi cant hemodynamic changes during the operation should be observed in the intensive care unit overnight. Glucose levels should be monitored because catecholamine-induced suppression of insulin secretion may lead to rebound hyperinsulinemia and then to hypoglycemia. Most patients can be discharged within 24 to 48 hours after adrenalectomy. Periodic follow-up biochemica l testing is indicated because of the potential for recurrence after resection of even benign-appearing tumors.
Adrenal Incidentaloma
Today, the incidentally discovered adrenal mass is by far the most commonly encountered adrenal lesion, primarily because of the frequency with which patients currently undergo cross-sectional imaging.49 Various series have reported fi nding adrenal incidentalomas in 1 to 5% of patients who undergo CT scanning for other reasons.50,51
clinical evaluation
Most adrenal incidentalomas are clinically silent, do not secrete excess adrenal hormones, and do not cause pain. The differential diagnosis of an adrenal incidentaloma includes all of the functioning adrenal tumors, primary or metastatic adrenal malignancy, and various nonfunctioning lesions.52 Nonfunctioning cortical adenoma is the most common adrenal incidentaloma, accounting for approximately 60% of cases.52 Other miscellaneous adrenal lesions that are some-times seen in this setting are myelolipomas and cysts. Of the hyperfunctioning tumors, cortisol-producing adenomas (most of which are subclinical in behavior) and pheochro-mocytomas are the most frequently identifi ed. Some adrenal incidentalomas are bilateral; in such cases, the differential diagnosis includes adrenocortical hyperplasia, bilateral pheochromocytomas, metastases, lymphoma, myelolipoma s, and infection (tuberculosis).
investigative studies
Evaluation of the patient with an adrenal incidentaloma should be directed toward determining whether the lesion is hypersecretory and assessing the likelihood of malignancy [see Figure 7].
Laboratory Tests
For all patients with adrenal incidentalomas, biochemical screening should include, at a minimum, an overnight dexa-methasone test to exclude hypercortisolism and measure-ment of the concentrations of either plasma metanephrines or urinary catecholamines and metabolites to test for pheo-chromocytoma. Although aldosteronomas, being relatively small, do not often present as incidentalomas, measurement
of plasma aldosterone and renin levels is nonetheless indi-cated for hypertensive or hypokalemic patients with an incidentally discovered adrenal mass. Approximately 8% of patients with adrenal incidentalomas have subclinical Cushing syndrome [see Cushing Syndrome, above].14 Adre-nalectomy is appropriate in these patients if the operative risk is acceptable.
Imaging
The second component of the evaluation of an adrenal incidentaloma is assessment of the imaging features. Size is the variable that should be addressed fi rst; a lesion smaller than 4 cm in a patient without a known malignancy is very unlikely to be malignant. The shape and visual texture of the lesion should then be considered. Benign lesions tend to be smooth and homogeneous, whereas malignant lesions often have irregular contours and areas of inhomogeneity. Corti-cal adenomas are further characterized by the presence of intracellular lipid, which on noncontrast CT scanning gives the mass an appearance that is homogeneous and low in attenuation (< 10 Hounsfi eld units, which is less than the liver or the kidney but higher than retroperitoneal fat) [see Figure 8]. ACCAs and metastases are higher in water content, as are pheochromocytomas, and therefore have higher attenuation values (usually > 18 Hounsfi eld units). There may, however, be some overlap in attenuation values between adenomas and malignancies, and in any case, many patients with incidentalomas initially underwent CT scan-ning with IV contrast, which makes subsequent assessment of attenuation values problematic. Pheochromocytomas, because of their vascularity, show prominent enhancement
Perform adrenalectomy.
Observe patient.Repeat imaging at 4 and12 mo. Repeat biochemicalevaluation at 12 mo.
Leslon is nonfunctioning,< 4 cm, and benignappearing
Lesion is functioning
Lesion is > 4–5 cmor has atypicalappearance
Carry out radiographic assessment, reviewingimages for lesion size, attenuation, and homogeneity.If CT cannot determine the nature and characteristicsof the lesion, perform MRI.
Carry out biochemical evaluation:· Measure plasma concentrations of fractionated metanephrines or urinary levels of catecholamines and metanephrines.· Perform dexamethasone suppression test.· If the patient is hypertensive or hypokalemic, measure plasma concentrations of aldosterone and renin.
Adrenal mass is incidentally discovered ondiagnostic imaging
Figure 7 Algorithm illustrating diagnostic evaluation of the patient with an incidentally discovered adrenal mass. CT = computed tomo-graphy; MRI = magnetic resonance imaging.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 12
Moreover, if the lesion is an undiagnosed pheochromocy-toma, needle biopsy may lead to hypertensive crisis and sudden death. Despite these known drawbacks, in three series from the past few years, a number of patients with undiagnosed pheochromocytomas presenting as inciden-talomas underwent adrenal biopsy before any biochemical testing.33,34,55,56
management
Most adrenal surgeons recommend removing nonfunc-tioning adrenal masses larger than 5 cm and observing masses smaller than 3 cm unless they are obvious myeloli-pomas or cysts [see Miscellaneous Adrenal Lesions, below]. Management of masses 4 to 5 cm in size should be individu-alized, with adrenalectomy favored if the patient is young or if the imaging features are at all atypical for an adenoma. Patients for whom resection is not appropriate should be followed with repeat imaging at 4 to 6 months and with both repeat imaging and biochemical testing at 1 year. If the lesion is nonfunctioning and stable in size throughout the follow-up period, no further monitoring is required.
on IV contrast studies and may have areas of cystic degen-eration. On unenhanced scans, their density is similar to that of the liver.
In cases where the nature of the lesion cannot be deter-mined on the basis of CT scanning, MRI can provide addi-tional characterization of the lesion that may help direct management. For example, on T2-weighted sequences, adenomas typically exhibit low signal activity, whereas pheochromocytomas and metastases appear bright. Mag-netic resonance (MR) chemical shift imaging may also have signifi cant diagnostic value. This modality is based on the different resonance frequencies of the protons in water and those in fat. Depending on the imaging parameters, the water and lipid magnetic dipoles will be either in phase or out of phase. If an adrenal lesion with a high lipid content (e.g., an adrenal adenoma) is imaged with MR chemical shift imaging, the mass will lose signal intensity on opposed-phase images (because the water signal and the fat signal will tend to cancel each other out) [see Figure 9]. In contrast, if an adrenal lesion with a low lipid content (e.g., an adrenal malignancy or a pheochromocytoma) is imaged with this technique, the mass will not show a signifi cant loss of signal intensity on opposed-phase images (because there will not be suffi cient fat protons to cancel out the water signal). The presence of low attenuation (< 10 Hounsfi eld units) on CT scanning and the loss of signal on MR chemical shift imag-ing are highly predictive of a benign lesion.53,54 Although positron emission tomography (PET) is increasingly employed for evaluation of adrenal incidentalomas, its role in this setting remains to be determined. The main value of PET with respect to adrenal disease is to identify extra-adrenal tumor sites in patients with a known cancer.
Biopsy
Needle biopsy of adrenal masses is rarely indicated. It does not often yield diagnostic information, it cannot differentiate benign from malignant adrenal cortical tumors, and it is associated with a signifi cant risk of complications.55
Figure 8 Computed tomographic scan showing a nonfunctioning cortical adenoma (arrow).
Figure 9 Chemical shift magnetic resonance imaging of a 3 cm left adrenal adenoma (arrows). (a) In-phase sequences and (b) opposed-phase sequences. Note the loss of signal intensity on opposed-phase imaging.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 13
Adrenal metastases occur most commonly in the setting of more widespread metastatic disease. Renal cell cancer, lung cancer, and melanoma are the malignancies that most frequently metastasize to the adrenal gland, but various other tumors (e.g., breast cancers, colon and other gastroin-testinal cancers, and lymphomas) may also involve the adrenal. Occasionally, the adrenal gland is the site of an apparent solitary metastasis for which resection is indicated. Imaging characteristics associated with adrenal metastases include larger size (> 3 cm), higher attenuation on CT, and no signal loss on MR chemical shift imaging. PET is often indicated to exclude extra-adrenal metastatic disease that would preclude resection [see Figure 10]. Biopsy of a sus-pected adrenal metastasis should be carried out only if a tissue diagnosis is needed to direct therapy—that is, if the patient is not a surgical candidate either for medical reasons or because of metastases at other sites. Biopsy is not indi-cated before resection of a solitary resectable lesion, because it could lead to tumor seeding or other complications. Reported 5-year actuarial survival rates after resection of an isolated adrenal metastasis range from 24 to 29%.57
Miscellaneous Adrenal Lesions
The adrenal disorders previously described (see above) are the ones most frequently seen and managed by surgeons; however, surgeons may also encounter a number of other adrenal lesions, such as myelolipomas, ganglioneuromas, cysts, and hemorrhage.
Myelolipomas are benign lesions that are composed of fat and bone marrow elements and are usually identifi ed as incidentalomas. In most instances, they can be diagnosed radiographically on the basis of macroscopic fat that is present within the mass [see Figure 11]. Myelolipomas may become quite large (> 6 cm), but regardless of their size, they should not be removed unless they are causing symptoms.
Ganglioneuromas are benign tumors that may arise either within the adrenal medulla or at an extra-adrenal site. Most adrenal cysts are lymphangiomatous cysts, but pseudocysts from previous hemorrhage may also develop.
Hemorrhage in the adrenal gland is most often the conse-quence either of trauma or of an underlying adrenal tumor. Accordingly, follow-up imaging should be performed to search for an adrenal mass that may be obscured by the bleeding.
A summary of the above tumors regarding clinical presentation and diagnostic features is given in Table 7.
Indications for Adrenalectomy
Any adrenal lesion that is hyperfunctioning or that is sus-pected of being malignant or possibly malignant on the basis of imaging criteria discussed above should be removed. Size alone, however, should not be used as the basis for selection for operation because some adrenal lesions (e.g., cortical adenomas, myelolipomas, cysts) may be greater than 4 cm but otherwise have completely benign imaging characteris-tics and therefore should not be removed.54 Adrenal metas-tases should be resected only if they are solitary and appear in the absence of extra-adrenal metastatic disease. Adrenal myelolipomas and cysts should not be removed unless they cause symptoms or if there is uncertainty in the diagnosis.
Most of the adrenal disorders discussed in this chapter are amenable to laparoscopic resection. At present, the only absolute contraindication to laparoscopic adrenalectomy is a tumor with local or regional extension because of the need to perform en bloc resection of the tumor and any adjacent involved structures.
Laparoscopic removal of large (> 6 to 8 cm) or potentially malignant primary adrenal lesions is controversial, as dis-cussed below.58 Surgeons who attempt laparoscopic adrenal-ectomy in this setting should be highly experienced with the procedure.
Figure 10 (a) Computed tomographic and (b) positron emission tomographic images of a metastasis to the left adrenal gland (arrows).
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 14
Table 7 Clinical and Diagnostic Features of Common Adrenal TumorsAdrenal Tumor Clinical Presentation Biochemical Testing Preferred Method of Imaging/Localization
Aldosteronoma Hypertension ± hypokalemia Elevated PAC with suppressed PRA (PAC:PRA > 20–30)
Thin-section (3 mm) adrenal CT
Urine aldosterone > 12 µg/24 hr Adrenal vein sampling
Urine potassium > 30 mEq/24 hr
Cortisol-producing adenoma (Cushing syndrome)
Centripetal obesity, moon facies, hypertension, purple skin striae, osteopenia, plethora, amenorrhea
Elevated 24 hr urinary free cortisol Abdominal CT
Nonsuppressed low-dose dexamethasone test
Decreased plasma ACTH
Pheochromocytoma Severe episodic hypertension or hypertension with spells of tachycardia, headache, anxiety, and diaphoresis
Elevated plasma fractionated meta-nephrines or urinary catechol-amines and metabolites
MRI (T2-weighted sequences showing bright-appearing adrenal lesion)
123I-MIBG scan or Octreoscan reserved for malignant or extra-adrenal tumors not seen on conventional imaging
Adrenal cortical carcinoma
Cushing syndrome, virilizing features, local pain or mass
24 hr urinary free cortisol and metabolites
CT of chest/abdomen/pelvis
Plasma DHEA sulfate
Adrenal metastasis None (often seen on follow-up imaging) or local pain
Plasma fractionated metanephrines and low-dose DM test to exclude functioning lesion
Abdominal CT, PET imaging to evaluate for extra-adrenal metastatic disease as appropriate for the type of tumor
FNA biopsy only if unresectable
Myelolipoma None; occasionally local pain None if radiographic appearance is unequivocal for myelolipoma
Presence of macroscopic fat on CT or MRI
ACTH = adrenocorticotropic hormone; CT = computed tomography; DHEA = dehydroepiandrosterone; DM = dexamethasone; FNA = fi ne-needle aspiration; MIBG = metaiodolbenzylguanidine; MRI = magnetic resonance imaging; PAC = plasma aldosterone concentration; PET = positron emission tomography; PRA = plasma renin activity.
Figure 11 A myelolipoma of the right adrenal gland. The areas of macroscopic fat (arrows) are typical for this lesion.
Operative Planning
preparation for operation
Preoperative preparation of the patient for adrenalectomy entails control of hypertension and correction of any electro-lyte imbalances. Patients with a pheochromocytoma should
receive 7 to 10 days of alpha-adrenergic blockade with phenoxybenzamine to minimize any exacerbation of hyper-tension during the operation [see Pheochromocytoma, above]. Patients with Cushing syndrome or SCS should receive perioperative dosages of stress steroids. Mechanical bowel preparation is not necessary.
choice of procedure
The retroperitoneal location of the adrenals renders them accessible via either transabdominal or retroperitoneal approaches.59,60 The choice of surgical approach in any given patient depends on a number of factors, including the nature of the underlying adrenal pathology, the size of the tumor, the patient’s body habitus, and the experience of the operat-ing surgeon. For the vast majority of adrenal lesions, laparo-scopic adrenalectomy is preferred. Most centers favor the transabdominal lateral approach to laparoscopic adrenalec-tomy, which has the advantages of a large working space, familiar anatomic landmarks, and widespread success. Increasingly, however, a number of centers prefer a retro-peritoneal endoscopic approach.61,62 The advantages of this technique are that the peritoneal cavity is not entered, there is no need to retract overlying organs, and the incidence of postoperative ileus may be lower. It may also simplify access in patients who have previously undergone extensive upper abdominal procedures. The disadvantages are that the retroperitoneal approach employs a smaller working space, is more diffi cult to learn with fewer anatomic land-marks for orientation, and is more diffi cult in obese patients and those with larger tumors.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 15
The only absolute contraindications to laparoscopic adre-nalectomy are local tumor invasion and the presence of regional lymphadenopathy. Cases in which the adrenal tumor is large (> 8 to 10 cm) or is suspected to be a primary adrenal malignancy or in which there is a history of previ-ous nephrectomy, splenectomy, or liver resection on the side of the lesion to be removed should be considered relative contraindications to a laparoscopic approach in all but the most experienced hands. Portal hypertension may also be a contraindication to a laparoscopic approach because of the dilated collateral vessels in the retroperitoneum.
Options for open adrenalectomy include transabdominal, fl ank, posterior retroperitoneal, and thoracoabdominal approaches. The lateral fl ank approach and the posterior retroperitoneal approach have been replaced by laparoscopi c approaches and are now rarely used. Most large or malig-nant adrenal tumors that necessitate an open approach can be removed via an anterior abdominal incision, usually a unilateral or bilateral subcostal incision (with subxiphoid extension if necessary); a thoracoabdominal incision is rarely needed.
Operative Technique
laparoscopic adrenalectomy
Transabdominal Approach
Patient positioning A gel-padded bean-bag mattress is placed on the operating table before the patient enters the room. The patient is placed in the supine position, general anesthesia is induced, and sequential compression stockings are placed. A urinary catheter may be optional for uncom-plicated cases but should be used for all pheochromocyto-mas and larger tumors. Invasive monitoring is not usually necessary unless the patient has a vasoactive pheochromo-cytoma, in which case, an arterial line is routinely placed.
Next, the patient is moved into a lateral decubitus posi-tion with the affected side up [see Figure 12]. A roll is placed
underneath the chest wall to protect the axilla. The bean-bag mattress is molded around the patient, and the legs are wrapped in a foam pad to protect all pressure points. The patient is secured to the operating table with tape placed across the padded lower extremities and a safety strap across the pelvis. The operating table is then fl exed at the waist. The combination of the lateral position, the fl exed operating table, and the reverse Trendelenburg position facilitates placement of the laparoscopic ports and provides optimal access to the superior retroperitoneum.
Initial access and placement of trocars Because of the lateral position, initial access to the peritoneal cavity is usually achieved in a closed fashion with a Veress needle. After insuffl ation to a pressure of 15 mm Hg, a 5 mm optical view trocar is placed. An open insertion technique may be used instead but requires a larger incision and is hindered somewhat by the bulky overlapping muscle layers in the subcostal region. Open insertion at the umbilicus is an option in nonobese patients.
The initial access site is generally at or somewhat medial to the anterior axillary line about two fi ngerbreadths below the costal margin [see Figure 13]. Subsequent ports should be placed at least 5 cm apart to allow freedom of movement externally. The most dorsal port should be approximately at the posterior axillary line. It is helpful to outline the anterior and posterior axillary lines with a marker before the patient is prepared to ensure that the ports are positioned properly. Whereas four ports are required for a right adre-nalectomy, a left adrenalectomy can be done with either three or four ports depending on the surgeon’s preference and experience.
Right adrenalectomy Step 1: exposure of right adrenal gland and vein The key to exposure of the right adrenal gland is extensive division of the right triangular ligament of the liver. This maneuver should be continued until the liver can be easily elevated and retracted medially and both
Figure 12 Laparoscopic adrenalectomy: transabdominal approach. The patient is placed in a lateral decubitus position with the affected side up (here, right lateral decubitus for left adrenalectomy).
Figure 13 Laparoscopic adrenalectomy: transabdominal approach. Shown is the recommended port site placement for laparoscopic adre-nalectomy (here, left adrenalectomy). Dashed lines indicate the costal margin and the anterior and posterior axillary lines. IPS = initial port site.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 16
the right adrenal and the IVC are visible. A retractor is then inserted through the most medial port to hold the right lobe of the liver up and away from the operative site.
Next, the plane between the medial border of the adrenal and the lateral aspect of the IVC is developed. An L-hook monopolar instrument is used for gentle elevation and division of the peritoneum and the small arterial branches here [see Figure 14]. The adrenal is pushed laterally with an atraumatic grasper to apply traction to the dissection site; however, the gland itself should not be grasped, because it is fragile and the capsule and adrenal parenchyma are easily fractured. At all times, it is imperative to know where the lateral border of the vena cava is, both to ensure that the dissection is extra-adrenal and to avoid injuring it. The right adrenal vein should come into view as the medial border is dissected.
Step 2: isolation, clipping, and division of right adrenal vein The right adrenal vein is fi rst exposed by gentle blunt spreading, and a right-angled dissector is then used to isolate enough of the vein to permit clip placement [see Figure 15]. A medium-large clip is usually suffi cient for securing the vein, although sometimes it is necessary to use larger clips or even an endovascular stapler. (We use an endovascular stapler primarily in cases in which the tumor is located in the medial area of the adrenal and the vein must be taken along with a portion of the IVC junction.) Usually, two clips are placed on the IVC side and one or two on the adrenal side, depending on the length of vein available.
Liver
AdrenalTumor
Kidney
Figure 14 Laparoscopic right adrenalectomy: transabdominal ap-proach. Depicted is the anatomic exposure for right adrenalectomy. The liver is retracted medially, and the right triangular ligament of the liver is divided with an L-hook electrocautery.
Figure 15 Laparoscopic right adrenalectomy: transabdominal approach. Once the right adrenal and adrenal vein are exposed, the vein is isolated and clipped. Shown are (a) a schematic representation and (b) an intraoperative view showing the right adrenal gland/tumor (A), the right adrenal vein (AV), and the inferior vena cava (IVC).
Meticulous hemostasis throughout the dissection is impor-tant: even minimal bleeding will stain the tissue planes and make the dissection more diffi cult and potentially treacherous.
Step 3: mobilization and detachment of specimen Once the adrenal vein is divided, dissection is continued superiorly and inferiorly with the L-hook. The numerous small arteries that enter the gland at its superior, medial, and inferior margins can be safely bovied, but larger branches should be
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 17
clipped or taken with an advanced energy device. Superi-orly, as the adrenal is mobilized, the musculature of the posterior diaphragm is exposed and serves as a marker of the proper plane for the posterior dissection. Inferiorly, the dissection should stay close to the margin of the adrenal so as not to injure vessels to the superior pole of the kidney. The inferior dissection then proceeds in a medial-to-lateral direction as the gland is elevated off the superior pole of the right kidney. The remaining attachments and retroperito-neal fat are relatively avascular and can be divided as above.
Once the specimen has been detached, it is placed in an impermeable bag. The retroperitoneum is then irrigated and inspected for hemostasis and for secure placement of the clips on the IVC.
Step 4: extraction of specimen The fascial opening at the 10/12 mm port site is enlarged somewhat, and the specimen bag is removed through this site. Large pheochromocytomas may be morcellated within the entrapment bag and removed piecemeal, but, ideally, cortical and other tumors should be extracted intact to permit full pathologic examination.
Left adrenalectomy Step 1: exposure of left adrenal gland and vein The splenic fl exure of the colon is mobilized, and the colon is then released from the inferior pole of the spleen and away from the left kidney. Next, the splenorenal ligament is incised from the inferior pole of the spleen to the diaphragm to allow full medial rotation of the spleen and provide access to the left retroperitoneum [see Figure 16]. It is important not to dissect lateral to the kidney; doing so will cause the kidney to tilt forward and will interfere with exposure. Once the spleen is completely mobilized, it should fall medially, with minimal or no retraction needed to keep it out of the operative fi eld. Division of the ligaments can be accomplished more quickly and with less bleeding if an ultrasonic or advanced bipolar coagulator is used.
At this point in the dissection, the tail of the pancreas should be visible, along with the splenic artery and vein. The plane between the pancreas and the left kidney is then developed, and this key maneuver allows the tail of the pancreas along with the spleen to be retracted medially. The adrenal is located on the superomedial aspect of the kidney just cephalad to the tail of the pancreas and is usually closely applied to the kidney, more so than on the right side. If the adrenal gland is not readily visible (more often a prob-lem in obese patients) laparoscopic ultrasonography should be employed to help locate it and to delineate the surround-ing anatomy, upper kidney, and renal hilar vessels. If the dissection starts too low, the renal hilar vessels or the ureter could be injured.
Once the adrenal is visualized, the medial and lateral bor-ders are defi ned and the dissection is continued inferiorly to locate the adrenal vein as it obliquely exits the inferomedial border of the gland [see Figure 17]. The inferior border of the adrenal often sits adjacent to the left renal vein, from which it can be separated by means of gentle blunt dissection.
Step 2: isolation, clipping, and division of left adrenal vein The adrenal vein is isolated, doubly clipped, and divided. Because the adrenal vein is usually joined by the inferior
Liver
Spleen
Pancreas
LeftKidney
a
S
A
K
b
Figure 16 Laparoscopic left adrenalectomy: transabdominal ap-proach. Depicted is the anatomic exposure for left adrenalectomy. (a) The splenic fl exure of the colon is divided fi rst (dotted line), and the splenorenal ligament is then divided (dashed line). (b) An intraoperative view. A = adrenal; K = kidney; S = spleen.
phrenic vein cephalad to its junction with the renal vein, it is often necessary to take the inferior phrenic vein again as the dissection proceeds more proximally.
Step 3: mobilization and detachment of specimen The dissec-tion is continued cephalad along both the lateral and the medial borders of the gland. Because of the surrounding ret-roperitoneal fat, it is advisable to use an advanced energy device for this part of the left-side dissection. One must be
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 18
careful to stay close to the adrenal until the gland is off the upper kidney to avoid injuring a superior pole renal artery. Finally, the posterior and superior attachments to the diaphragm and the retroperitoneal fat are divided.
Step 4: extraction of specimen The retroperitoneum is inspected and the specimen extracted as in a right adrenal-ectomy. If there is any possibility that the pancreatic paren-chyma may have been violated, a closed-suction drain is left in place.
Retroperitoneal Approach
The technique for performing retroperitoneoscopic adre-nalectomy has been well described by Walz and colleagues in over 500 cases.61 The patient is in a prone position and is lying on a rectangular support that allows the abdominal wall to hang freely so that the retroperitoneum may be more easily expanded by the CO2 gas [see Figure 18a]. The lateral aspect of the working side of the body is at the lateral aspect of the operating table. The 12 mm initial 1.5 to 2 cm access incision is placed just below the tip of the 12th rib and the retroperitoneum is entered under direct visualization. The cavity is developed digitally, and the fi nger in the retroperi-toneal space allows for direct palpation and guidance of the second and third trocars. Both the second and third ports can be 5 mm [see Figure 18b]. It is helpful to use an adjustable blunt trocar with an infl atable balloon for the initial access site to maintain a good seal. The retroperitoneal space should be infl ated at 20 to 25 mm Hg pressure to aid in both increas-ing the size of the working space and decreasing the amount of bleeding.
The retroperitoneal approach can be disorienting as most surgeons are not familiar with this viewpoint. When per-forming a right adrenalectomy, the right lobe of the liver is seen at the right side of the video monitor, with the lateral diaphragm seen at the top side of the screen. The kidney is seen at the bottom of the screen, and the spine is seen on the left side. The upper pole of the kidney should be dissected fi rst, which allows for better visualization of the adrenal gland. The lower pole of the adrenal gland should then be dissected medially to laterally. On the right, the IVC then comes into view medially and deep to the adrenal after the lower pole of the adrenal is dissected. With upward traction of the adrenal, the adrenal vein can be found on the medial-posterior aspect of the gland. With the retroperitoneal approach, the adrenal vein can be secured with an advanced bipolar energy device, and the remaining posterior and lateral attachments can then be divided. As with the trans-abdominal approach, if the adrenal is diffi cult to locate, laparoscopic ultrasonography should be used.
During left adrenalectomy, the tail of the pancreas and spleen are deep to the adrenal above the kidney. The steps in exposure of the left adrenal are similar to the right approach, but the adrenal vein is located at the medial/infe-rior (i.e., right lower) aspect of the gland. The specimen is extracted similar to the transabdominal approach.
Robotic-Assisted Laparoscopic Adrenalectomy
Certain centers have incorporated robotic-assisted laparo-scopic adrenalectomies into their practice. The pros and cons of this approach compared with conventional laparoscopy are under investigation.63 Although the robotic approach has not demonstrated any advantages in operative time, safety, cost, hospital stay, or postoperative complications than laparoscopic surgery, it may provide surgeons with better ergonomics. In experienced hands, the conversion rate from robotics to laparoscopy is about 5 to 7% and to laparotomy is about 1%.62 Overall, the robotic approach could offer comparable outcomes and feasibility for patients in high-volume centers.
a
PV
AV
A
b
Figure 17 Laparoscopic left adrenalectomy: transabdominal ap-proach. Once the left adrenal and adrenal vein are exposed, the vein is isolated and clipped. Shown are (a) a schematic representation and (b) an intraoperative view showing the left adrenal gland/tumor (A), the left adrenal vein (AV), and the phrenic vein (PV). The phrenic vein joins the left adrenal vein above its junction with the renal vein.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 19
Figure 18 Laparoscopic left adrenalectomy: retroperitoneal endo-scopic approach. Shown are (a) patient positioning and (b) port site placement.
open adrenalectomy
Of the four approaches to open adrenalectomy [see Opera-tive Planning, Choice of Procedure, above], the anterior transabdominal approach is the preferred method for tumors that are too large to be removed laparoscopically and for all invasive adrenal malignancies. The incision most commonly used is an extended unilateral or bilateral sub-costal incision, although a midline incision is also an option
[see Figure 19]. The extended subcostal incision yields exposure of both adrenal glands, as well as the rest of the peritoneal cavity. If necessary, it may be extended superi-orly in the midline to the xiphoid to provide better upper abdominal exposure for full mobilization of the liver and access to the hepatic veins and the vena cava. The exposure obtained with this incision is suffi cient for all but the most extensive adrenal malignancies. If the tumor involves the vena cava, the incision may be extended into a median sternotomy to provide access to the superior vena cava and the heart. The classic thoracoabdominal incision, which extends from the abdomen up through the seventh or eighth intercostal space and through the diaphragm, provides excellent exposure but is associated with increased incision-related morbidity and is rarely used today.
Much of the exposure and dissection is the same as in a laparoscopic adrenalectomy; however, because open adre-nalectomy is often employed for removal of particularly large tumors, some additional maneuvers may be necessary to achieve adequate exposure and vascular control. For example, it may be helpful to elevate the fl ank with a roll or a bean-bag mattress and then fl ex the operating table to open up the space between the costal margin and the iliac crest. Once the abdomen is entered, exploration is carried out for the presence of metastatic disease.
Exposure of the adrenal on the right side is similar to the laparoscopic approach. With large tumors, a Kocher maneuver should be performed to afford better exposure
Figure 19 Open adrenalectomy. The procedure is generally done through a unilateral or bilateral subcostal incision. For better exposure for large adrenal malignancies, the incision may be extended cephalad in the midline.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 20
of the vena cava and the renal vessels. The remainder of the dissection proceeds in much the same manner as in a laparoscopic right adrenalectomy. For suspected adrenal malignancies, a wide resection should be carried out, with removal of periadrenal fat and lymphatic tissue and any suspicious lymph nodes. For tumors that appear to involve the vena cava, vascular control of both the IVC proximal and distal to the tumor and the renal veins should be achieved before the lesion is removed.
Open left adrenalectomy entails refl ection of the spleen, the tail of pancreas, and the stomach medially en bloc to expose the left kidney and the left adrenal. The remainder of the dissection proceeds as in a laparoscopic left adrenalec-tomy. For left-side primary adrenal malignancies, periaortic lymphatic vessels and lymph nodes should be removed along with the specimen. If a large left-side tumor is invading adjacent structures, removal may require en bloc resection of the spleen, the distal pancreas, and the kidney.
Troubleshooting
inability to locate adrenal
The adrenal is usually not diffi cult to fi nd on the right side, where it should be visible once the right lobe of the liver has been mobilized. Important landmarks on that side are the IVC, which is medial to the adrenal, and the kidney, which is inferior to the adrenal. Once these structures have been identifi ed, the location of the adrenal should be appar-ent. In contrast, the adrenal can be diffi cult to fi nd on the left side, especially if the tumor is small or the patient is obese. To locate the left adrenal, the splenorenal ligament should be fully divided, and then the plane between the kidney and the tail of the pancreas should be developed, with the tail of the pancreas rotated medially. As dissection proceeds superiorly, the adrenal can be visually distinguished from the retroperitoneal fat by its golden-orange appearance. If the adrenal is not yet visualized at this point, laparoscopic ultrasonography should be used to verify the locations of the superior pole of the left kidney and the renal vessels. Ultrasonography should also be able to image the adrenal gland and tumor within the retroperitoneal fat [see Figure 20].
conversion to open adrenalectomy
Conversion to open adrenalectomy may sometimes be necessary because of bleeding, failure to progress with the dissection, or a locally invasive tumor. If the patient is in the lateral decubitus position, conversion may be accomplished by means of a subcostal incision extended into the fl ank. With the patient on a bean-bag mattress, the operating table can be rotated out of the straight lateral plane so that the patient comes to occupy more of a hemilateral position. If the procedure is a bilateral adrenalectomy, then either a bilateral subcostal incision or a midline incision may be employed after the patient has fi rst been returned to more of a supine position. For this reason, it is important to extend the initial preparation and draping past the midline of the abdomen. Alternatively, if the conversion is not being done on an urgent basis because of bleeding, the port sites may be closed, and the patient may then be moved into the supine position, reprepared, and redraped.
An option that may be considered before conversion to an open procedure is the use of a hand access port. A hand-assisted technique may be particularly useful for larger, noninvasive tumors that are harder to manipulate with laparoscopic instruments. The location of the incision for the hand port may vary according to the patient’s body habitus; generally, however, an ipsilateral subcostal or midline location medial to the working ports allows adequate hand access while preserving visualization through the more lateral ports.
large tumors
As surgeons become more familiar and profi cient with laparoscopic adrenalectomy, the indications for removing large tumors laparoscopically have expanded. Large adrenal tumors (> 6 to 8 cm) are more diffi cult to remove than smaller ones because they are bulkier and more vascular and because they are harder to manipulate and retract. Accordingly, the dissection should stay extra-adrenal, and care must be exercised during manipulation to avoid enter-ing the tumor. Surgeons should keep in mind that the larger an adrenal tumor is, the more likely it may be malignant. Laparoscopic ultrasonography should also be employed to verify that the tumor is well circumscribed and noninvasive. Surgeons who attempt to remove large adrenal tumors lapa-roscopically should be highly experienced in laparoscopic adrenalectomy techniques.
For large invasive adrenal malignancies, an open approach, involving a generous bilateral subcostal incision, is indicated, and the chest should be prepared in case a thoracoabdominal or median sternotomy extension proves necessary. The important principles are to obtain wide expo-sure of the operative fi eld and to control all major vessels that may be involved before removing the tumor.
Figure 20 If the left adrenal proves diffi cult to fi nd, laparoscopic ultrasonography may be employed to locate the gland and the lesion within the retroperitoneal fat. This laparoscopic ultrasonogram shows an enlarged left adrenal gland secondary to metastatic squamous cell carcinoma of the lung.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 21
obese patients
Obese patients present a particular challenge during adre-nalectomy, for several reasons: initial access is more diffi -cult; retraction and exposure are more challenging; and the copious amount of retroperitoneal fat makes it diffi cult to identify the adrenal and to clearly defi ne the margins of the gland within the retroperitoneum. Our practice is to attempt to gain initial access to the peritoneal cavity by using a closed Veress needle technique. Because resting intra-abdominal pressure may be higher in obese patients, espe-cially if they are in the lateral position, it may be necessary to increase the CO2 pressure to 20 mm Hg temporarily until the fi rst trocar is inserted. If it proves diffi cult to establish pneumoperitoneum with the Veress needle technique, the initial trocar should be placed at the umbilicus by means of an open insertion technique. On the right side, the presence of a bulky, fatty liver should be anticipated, and the loca-tions of the port sites should be adjusted accordingly by placing them somewhat more caudad. It may be benefi cial to place obese patients on a restricted-calorie diet (< 1,400 calories/day) for 2 to 3 weeks before surgery to decrease the extent of fat and thereby overall bulk of the liver. Ample time should be taken to mobilize the liver fully so that the adrenal and the IVC can be safely accessed. On the left, the ports may be placed in the standard locations. Laparoscopic ultrasonography is often needed to locate the gland in the retroperitoneal fat.
Postoperative Care
After laparoscopic adrenalectomy, most patients are admitted to a regular nursing unit, although some patients with pheochromocytomas will need to undergo a short stay in the intensive care unit for invasive monitoring. Patients are started on clear liquids once they are awake and alert, and the diet is advanced as tolerated. A complete blood count is obtained on postoperative day 1 in all patients, and electrolyte levels are monitored in patients with aldoste-ronomas and hypercortisolism. Patients with Cushing syndrome should be given stress doses of steroids periop-eratively and should be discharged on a maintenance pred-nisone dosage of 10 to 15 mg/day in divided doses. These patients should be advised that it may take 6 to 12 months or longer for the contralateral adrenal to recover to the point where prednisone can be discontinued. Patients undergoing bilateral adrenalectomy will need lifelong replacement ther-apy with a glucocorticoid (e.g., prednisone) and a mineralo-corticoid (e.g., fl udrocortisone acetate 0.1 mg/day).
Postoperative management of hypertensive medications depends on the pathology of the underlying adrenal lesion. In patients with aldosteronomas, spironolactone is stopped immediately after adrenalectomy, and the other antihyper-tensive agents are usually continued while blood pressure is monitored closely on an outpatient basis; further medica-tion reductions are made as clinically warranted. In most patients with Cushing syndrome, antihypertensive medica-tions are continued, whereas in most patients with pheochromocytomas, they are not. In both sets of patients, however, close outpatient monitoring of blood pressure should be carried out in the early postoperative period.
Adrenalectomy can have a dramatic impact on hypertensive control and can lead to hypotension if medications are not appropriately adjusted.
In most routine cases, patients can be discharged within 24 hours after laparoscopic adrenalectomy, although some patients require longer in-hospital observation for blood pressure monitoring, for adjustment of steroid replacement therapy, or for resumption of a regular diet. After open adrenalectomy, resumption of an oral diet occurs later, and postoperative hospital stays of 4 to 5 days are more typical.
After discharge, patients are seen in the clinic within 2 to 3 weeks for a wound check, blood pressure evaluation, and a review of antihypertensive medications. In patients who underwent adrenalectomy for an aldosteronoma, electrolyte levels and the creatinine concentration and plasma aldoste-rone and renin levels should be checked. In patients who underwent adrenalectomy for pheochromocytoma, yearly clinical and biochemical follow-up is indicated, with mea-surement of plasma fractionated metanephrines (or urine levels of catecholamines and metanephrines). Likewise, patients with ACCA should be followed at regular intervals with periodic cross-sectional imaging and, where appropri-ate, biochemical testing because of the high recurrence rates. In selected patients on steroid replacement therapy who are proving diffi cult to wean from prednisone, an ACTH stimu-lation test may be necessary to assess the responsiveness of the pituitary-adrenal axis.
Complications
It appears that laparoscopic adrenalectomy has a major advantage over open adrenalectomy in terms of the inci-dence of postoperative complications. In a meta-analysis of 98 adrenalectomy series reported between 1980 and 2000, the overall complication rate was 10.9% with laparoscopic procedures and 25.2% with open procedures.64 This difference between the complication rates was primarily attributable to the occurrence of fewer wound, pulmonary, and infectious complications in the laparoscopic series. The operative mortality associated with laparoscopic adrenalectomy is about 0.3%.
bleeding
The most common complication of laparoscopic adrenal-ectomy is bleeding, which was reported in 4.7% of patients from the series reviewed in the meta-analysis. Bleeding is also the most common reason for conversion to open adre-nalectomy; however, major bleeding that leads to transfu-sion is relatively uncommon. The most effective strategy for managing bleeding during adrenalectomy is prevention. Important measures for minimizing bleeding risk include obtaining good exposure of the operative fi eld and employ-ing meticulous dissection and gentle handling of the adrenal and surrounding structures. When bleeding does occur, it may be from the adrenal veins, the adrenal gland itself, the IVC, the renal veins, the liver, the pancreas, the spleen, or the kidney. For bleeding during laparoscopic adrenalec-tomy, the fi rst maneuver should be to tamponade the bleed-ing site with an atraumatic instrument as the bleeding will often stop with pressure. If this maneuver is successful,
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 22
dissection should be directed away from the bleeding site for a while, until better exposure of the area can be obtained. Major hemorrhage from the IVC, renal veins, or arterial ves-sels that is not immediately controlled should be managed by prompt conversion to open adrenalectomy. Lesser bleeding may also be an indication for conversion to open adrenalectomy if it obscures the tissue planes and thereby increases the risk of inadvertent entry into the adrenal gland or tumor.
injury to adjacent organs
Other potential complications of adrenalectomy (either laparoscopic or open) include injury to the tail of the pan-creas, injury to the diaphragm, and pneumothorax. When performing a left transabdominal adrenalectomy, the tail of the pancreas can be mistaken for the left adrenal, resulting in inadvertent pancreatic resection with pancreatic leak or pancreatitis. This risk may be greater in obese patients due to the abundance of retroperitoneal fat. To avoid this com-plication, one must be aware of the appearance and texture of the adrenal gland and its anatomic location immediately superior and adherent to the left kidney. It is important to defi ne the plane between the pancreas and left kidney and then to rotate the tail of the pancreas and spleen medially during dissection. One should also see the splenic vein and artery as the pancreas is mobilized to the left. Unusual or large vessels encountered during the dissection should alert the surgeon to the possibility that the dissection plane may not be appropriate. Recently, severe high-grade complica-tions after adrenalectomy have been described, including porta hepatis and hepatic artery injuries that resulted in liver transplantation and injuries to the renal vessels and to the ureter that resulted in a loss of renal function.65
recurrence
Several cases of local or regional tumor recurrence have been reported after laparoscopic adrenalectomy. In most of these cases, the tumors removed were either suspected or unsuspected adrenal malignancies, and the extensive nature of the recurrences was probably related to aggressive tumor biology rather than to the minimally invasive surgical technique. In some of these cases, however, the pattern of recurrence, characterized by the development of multiple intraperitoneal or port-site metastases, suggested that lapa-roscopic dissection and pneumoperitoneum might have contributed to tumor spread.66–69 One group treated three patients for recurrent pheochromocytomatosis that devel-oped after laparoscopic adrenalectomy.70 These patients were found to have multiple small tumor nodules in the adrenalectomy bed during open reoperation after removal of apparently benign pheochromocytomas. Fragmentation of the tumor and excessive tumor manipulation during the laparoscopic dissection were considered the probable mechanisms of tumor recurrence.
These reports highlight the need for caution in approach-ing large, malignant, or potentially malignant adrenal tumors. Surgeons who attempt a laparoscopic approach in this setting should be highly experienced in laparoscopic adrenalectomy techniques, and the tumor should be well circumscribed and not locally invasive. The use of a hand port may be a valuable adjunct to resection in these cases.
Regardless of the specifi c surgical approach followed, wide excision of the lesion along with the surrounding periadre-nal fat is crucial for minimizing recurrence rates in this population.
Outcome Evaluation
The safety and effi cacy of laparoscopic adrenalectomy for the removal of small, benign adrenal tumors have been clearly established. Rates of conversion to open adrenalec-tomy in high-volume centers have ranged from 3 to 13%, and operating times have averaged 2 to 3 hours. Most patients are now discharged from the hospital within 24 to 48 hours after operation. Although no prospective, random-ized trial comparing laparoscopic with open adrenalectomy has been carried out, several retrospective studies have con-sistently shown that the laparoscopic approach is associated with decreased pain, a shorter hospital stay, and a faster recovery.71–74
The results of a laparoscopic approach in patients with large (> 6 cm) adrenal tumors or malignant primary or metastatic adrenal lesions have been reviewed58; generally, the conversion rates for large or malignant tumors have been higher than those reported in other laparoscopic adrenalectomy series. Overall, tumor recurrence rates after laparoscopic adrenalectomy have been low.75–79 In one series, however, local or regional tumor recurrence developed in three of fi ve patients with adrenocortical carcinomas that were treated laparoscopically.80 In another series from MD Anderson Cancer Center of patients with local recurrence after adrenalectomy, peritoneal carcinomatosis developed in fi ve of six patients (83%) after laparoscopic resection compared with only 8% of patients with local recurrences after open adrenalectomy.81 Whether the recurrences in these reported cases were related primarily to the surgical technique employed or to the underlying tumor biology is unclear. It would appear, therefore, that in most cases, primary adrenal malignancies are best approached in an open fashion unless the tumor is small and well circum-scribed and the surgeon is highly experienced.
Financial Disclosures: None Reported
References
1. Young WF Jr. Primary aldosteronism: a common and curable form of hypertension. Cardiol Rev 1999;7:207.
2. Mulatero P, Stowasser M, Loh K-C, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from fi ve continents. J Clin Endocrinol Metab 200;89:1045.
3. Funder JW, Carey RM, Fardella C, et al. Case detection, diagnosis, and treatment of patients with primary aldoste-ronism: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2008;93:3266–81.
4. Young WF, Stanson AW, Thompson GB, et al. Role for adre-nal venous sampling in primary aldosteronism. Surgery 2004;136:1227.
5. Mulatero O, Bertello C, Rossato D, et al. Roles of clinical criteria, computed tomography scan, and adrenal vein
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 23
sampling in differential diagnosis of primary aldosteronism subtypes. J Clin Endocrinol Metab 2008;93:1366–71.
6. Sawka AM, Young WF, Thompson GB, et al. Primary aldo-steronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med 2001;135:258.
7. Lo CY, Tam PC, Kung AW, et al. Primary aldosteronism: results of surgical treatment. Ann Surg 1996;224:125.
8. Proye CAG, Mulliez, EA, Carnaille, BM, et al. Essential hypertension: fi rst reason for persistent hypertension after unilateral adrenalectomy for primary aldosteronism? Surgery 1998;124:1128.
9. Zarnegar R, Young WF, Lee J, et al. The aldosteronoma resolution score: predicting complete resolution of hyper-tension after adrenalectomy for aldosteronoma. Ann Surg 2008;247:511–8.
10. Findling JW, Raff H. Diagnosis and differential diagnosis of Cushing’s syndrome. Endocrinol Metab Clin North Am 2001;30:729.
11. Arnaldi G, Angeli A, Atkinson AB, et al. Diagnosis and complications of Cushing’s syndrome: a consensus state-ment. J Clin Endocrinol Metab 2003;88:5593.
12. Papanicolaou DA, Mullen N, Kyrou I, et al. Nightime sali-vary cortisol: a useful test for the diagnosis of Cushing’s syndrome. J Clin Endocrinol Metab 2002;87:4515.
13. Invitti C, Giraldi FP, Cavagnini F. Inferior petrosal sinus sampling in patients with Cushing’s syndrome and contra-dicting response to dynamic testing. Clin Endocrinol 1999;51:255.
14. Reincke M. Subclinical Cushing’s syndrome. Endocrinol Metab Clin North Am 2000;29:43.
15. Sippel RS, Chen H. Sublinical Cushing’s syndrome in adre-nal incidentaloma. Surg Clin North Am 2004;84:875–85.
16. Barzon L, Fallo F, Sonimo N, Boscaro M. Development of overt Cushing’s syndrome in patients with adrenal inciden-taloma. Eur Endocrinol 2002;146:61–6.
17. Tomiato A, Merante-Boschin I, Opocher G, et al. Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized trial. Ann Surg 2009;249:388–91.
18. Dackiw AP, Lee JE, Gagel RF, et al. Adrenal cortical carci-noma. World J Surg 2001;25:914.
19. Harrison LE, Gaudin PB, Brennan MF. Pathologic features of prognostic signifi cance for adrenocortical carcinoma after curative resection. Arch Surg 1999;134:181.
20. Icard P, Goudet P, Charpenay C, et al. Adrenocortical car-cinomas: surgical trends and results of a 253-patient series from the French Association of Endocrine Surgeons Study Group. World J Surg 2001;25:891.
21. Paton BL, Novitsky YW, Zerey M, et al. Outcomes of adrenal cortical carcinoma in the United States. Surgery 2006;140:914–20.
22. Kebebew E, Reiff E, Duh Q-Y, et al. Extent of disease at presentation and outcome for adrenocortical carcinoma: have we made progress? World J Surg 2006;30:872–8.
23. Allolio B, Fassnacht M. Adrenocortical carcinoma: clinical update. J Clin Endocrinol Metab 2006;91:2027.
24. Hermeson IGC, Kerkhos TMS, den Butter G, et al. Surgery in adrenocortical carcinoma: importance of national coop-eration and centralized surgery. Surgery 2012;152:50–6.
25. Gaujoux S, Brennan MF. Recommendation for standardized surgical management of primary adrenocortical carcinoma. Surgery 2012;152:123–32.
26. Abraham J, Bakke S, Rutt A, et al. A phase II trial of combi-nation chemotherapy and surgical resection for the treat-ment of metastatic adrenocortical carcinoma: continuous infusion doxorubicin, vincristine, and etoposide with daily mitotane as a P-glycoprotein antagonist. Cancer 2002;94:2333.
27. Salvatori R. Adrenal insuffi ciency. JAMA 2005;294:2481.28. Krasner AS. Glucocorticoid-induced adrenal insuffi ciency.
JAMA 1999;282:671.29. Glowniak JV, Loriaux DL. A double-blind study of
perioperative steroid requirements in secondary adrenal insuffi ciency. Surgery 1997;121:123.
30. Bravo EL, Tagle R. Pheochromocytoma: state-of-the-art and future prospects. Endocr Rev 2003;24:539.
31. Kudva YC, Young WF Jr, Thompson GB, et al. Adrenal incidentaloma: an important component of the clinical presentation spectrum of benign sporadic adrenal pheo-chromocytoma. Endocrinologist 1999;9:77.
32. Lee JA, Zarnegar R, Shen WT, et al. Adrenal incidentaloma, borderline elevations of urine or plasma metanephrine levels, and the “subclinical” pheochromocytoma. Arch Surg 2007;142:870–3.
33. Cheah WK, Clark OH, Horn JK, et al. Laparoscopic adrenal-ectomy for pheochromocytoma. World J Surg 2002;26:1048.
34. Kercher KW, Novitsky YW, Park A, et al. Laparoscopic curative resection of pheochromocytomas. Ann Surg 2005;241:919.
35. McCorkell SJ, Niles NL. Fine-needle aspiration of catechol-amine-producing adrenal masses: a possibly fatal mistake. AJR Am J Roentgenol 1985;145:113.
36. Casola G, Nicolet V, van Sonnenberg E, et al. Unsuspected pheochromocytoma: risk of blood-pressure alterations during percutaneous adrenal biopsy. Radiology 1986;159:733.
37. Sawka AM, Jaeschke R, Singh RJ, et al. A comparison of biochemical tests for pheochromocytoma: measurement of fractionated plasma metanephrines compared with the combination of 24-hour urinary metanephrines and cate-cholamines. J Clin Endocrinol Metab 2003;88:553.
38. Ilias I, Pacak K. Current approaches and recommended algorithm for the diagnostic localization of pheochromocy-toma. J Clin Endocrinol Metab 2004;89:479.
39. Grant CS. Pheochromocytoma. In: Clark OH, Duh Q-Y, Kebebew E, editors. Textbook of endocrine surgery. Philadelphia: Elsevier Saunders; 2005. p. 621.
40. Reisch N, Peczkowska M, Januszewicz A, Neumann HP. Pheochromocytoma: presentation, diagnosis and treatment. J Hypertens 2006;24:2331–9.
41. Rufi ni V, Calcagni ML, Baum RP. Imaging of neuroendo-crine tumors. Semin Nucl Med 2006;36:228–47.
42. Miskulin J, Shulkin BL, Doherty GM, et al. Is preoperative iodine 123 meta-iodobenzylguanidine scintigraphy routinely necessary before initial adrenalectomy for pheochromocy-toma? Surgery 2003;134:918–23.
43. Greenblatt DY, Shenker Y, Chen H. The utility of metaiodo-benzylguanidine (MIBG) scintigraphy in patients with pheochromocytoma. Ann Surg Oncol 2008;15:900–5.
44. Quayle FJ, Fialkowski EA, Benveniste R, Moley JF. Pheo-chromocytoma penetrance varies by RET mutation in MEN 2A. Surgery 2007;142:800–5.
Scientific American Surgery

02/13
gastro disorders of the adrenal glands — 24
45. Neumann HP, Pawlu C, Peczowska M, et al. Distinct clini-cal features of paraganglioma syndromes associated with SDHB and SDHD gene mutations. JAMA 2004;292:943.
46. Benn DE, Gimenez-Roqueplo A-P, Reilly JR, et al. Clincial presentation and penetrance of pheochromocytoma/paraganglioma syndromes. J Clin Endocrinol Metab 2006;91:827.
47. Baysal BE, Ferrell RE, Willett-Brozick JE, et al. Mutations in SDHD, a mitochondrial complex II gene, in hereditary paraganglioma. Science 2000;287:848.
48. Neumann HP, Bausch B, McWhinney SR, et al. Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med 2002;346:1459.
49. Young WF Jr. The incidentally discovered adrenal mass. N Engl J Med 2007;356:601.
50. Bittner JB, Brunt LM. Evaluation and management of adrenal incidentaloma. J Surg Oncol 2012;106:557–64.
51. Davenport C, Liew A, Doherty B, et al. The prevalence of adrenal incidentaloma in routine clinical practice. Endocrine 2011;40:80–3.
52. Brunt LM, Moley JF. Adrenal incidentaloma. In: Cameron JL, editor. Cameron’s current surgical therapy. 9th ed. Philadelphia: Mosby Elsevier; 2008. p. 597–602.
53. Mitchell DG, Crovello M, Matteuci T, et al. Benign adreno-cortical masses: diagnosis with chemical shift MR imaging. Radiology 1992;185:345.
54. Yip L, Tublin ME, Falcone JA, et al. The adrenal mass: cor-relation of histopathology with imaging. Ann Surg Oncol 2010;17:846–52.
55. Quayle FJ, Spitler JA, Pierce RA, et al. Needle biopsy of incidentally discovered adrenal masses is rarely informa-tive and potentially hazardous. Surgery 2007;142:497–504.
56. Vanderveen KA, Thompson SM, Callstrom MR, et al. Biopsy of pheochromocytomas and paragangliomas: potential for disaster. Surgery 2009;146:1158–66.
57. Sarela A, Murphy I, Coit DG, et al. Metastasis to the adrenal gland: the emerging role of laparoscopic surgery. Ann Surg Oncol 2003;10:1191.
58. Brunt LM. Minimal access adrenal surgery. Surg Endosc 2006;20:351–61.
59. Gagner M, Lacroix A, Bolte E, et al. Laparoscopic adrenal-ectomy: the importance of a fl ank approach in the lateral decubitus position. Surg Endosc 1994;8:135.
60. Mercan S, Seven R, Ozarmagan S, et al. Endoscopic retroperitoneal adrenalectomy. Surgery 1995;118:1071.
61. Walz M, Alesina Piero, Wenger F, et al. Posterior retroperi-toneoscopic adrenalectomy—results of 560 procedures in 520 patients. Surgery 2006;140:943.
62. Brunaud L, Ayav A, Zarnegar R, et al. Prospective evalua-tion of 100 robotic-assisted unilateral adrenalectomies. Surgery 2008;144:995–1001.
63. Karabulut K, Agcaoglu O, Aluyev S, et al. Comparison of intraoperative time use and perioperative outcomes for laparoscopic vs robotic adrenalectomy. Surgery 2012;151:537–42.
64. Brunt LM. The positive impact of laparoscopic adrenalec-tomy on complications of adrenal surgery. Surg Endosc 2001;16:252.
65. Tessier DJ, Iglesias R, Chapman WC, et al. Previously unre-ported high grade complications of adrenalectomy. Surg Endosc 2009;23:97–102.
66. Foxius A, Ramboux A, Lefebvre Y, et al. Hazards of laparo-scopic adrenalectomy for Conn’s adenoma. Surg Endosc 1999;13:715.
67. Deckers S, Derdelinckx L, Col V, et al. Peritoneal carcino-matosis following laparoscopic resection of an adrenocorti-cal tumor causing primary hyperaldosteronism. Horm Res 1999;52:97.
68. Iino K, Oki Y, Sasano H. A case of adrenocortical carcinoma associated with recurrence after laparoscopic adrenalec-tomy. Clin Endocrinol 2000;53:243.
69. Iacconi P, Bendinelli C, Miccoli P, et al. Re: A case of Cush-ing’s syndrome due to adrenocortical carcinoma 19 months after laparoscopic adrenalectomy [letter]. J Urol 1999;161:1580.
70. Li ML, Fitzgerald PA, Price DC, et al. Iatrogenic pheochro-mocytomatosis: a previously unreported result of laparo-scopic adrenalectomy. Surgery 2001;130:1072.
71. Brunt LM, Doherty GM, Norton JA, et al. Laparoscopic compared to open adrenalectomy for benign adrenal neoplasms. J Am Coll Surg 1996;183:1.
72. Imai T, Kikumori T, Phiwa M, et al. A case-controlled study of laparoscopic compared with open lateral adrenalectomy. Am J Surg 1999;178:50.
73. Prinz RA. A comparison of laparoscopic and open adrenal-ectomies. Arch Surg 1995;130:489.
74. Thompson GB, Grant CS, van Heerden JA, et al. Laparo-scopic versus open posterior adrenalectomy: a case-control study. Surgery 1997;122:1132.
75. Heniford BT, Arca MJ, Walsh RM, et al. Laparoscopic adrenalectomy for cancer. Semin Surg Oncol 1999;16:293.
76. Henry J-F, Defechereux T, Gramatica L, et al. Should lapa-roscopic approach be proposed for large and/or potentially malignant adrenal tumors? Langenbecks Arch Surg 1999;384:366.
77. Hobart MG, Gill IS, Schweizer D, et al. Laparoscopic adrenalectomy for large-volume (> 5 cm) adrenal masses. J Endourol 2000;14:149.
78. Sarela A, Murphy I, Coit DG, et al. Metastasis to the adrenal gland: the emerging role of laparoscopic surgery. Ann Surg Oncol 2003;10:1191.
79. Miccoli P, Materazzi G, Mussi A, et al. A reappraisal of the indications for laparoscopic treatment of adrenal metasta-ses. J Laparoendosc Adv Surg Tech 2004;14:139.
80. Kebebew E, Siperstein AE, Clark OH, et al. Results of lapa-roscopic adrenalectomy for suspected and unsuspected malignant adrenal neoplasms. Arch Surg 2002;137:948.
81. Gonzalez RJ, Shapiro S, Sarlis N, et al. Laparoscopic resec-tion of adrenal cortical cancer: a cautionary note. Surgery 2005;138:1078–86.
Acknowledgment
Figures 1, 2, 14, 15a, 16a, 17a, 19 Tom Moore
Scientific American Surgery