Differential Limbic–Cortical Correlates of Sadness and ...directory.umm.ac.id/Data...
13
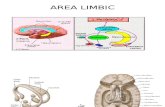
Differential Limbic–Cortical Correlates of Sadness and Anxiety in Healthy Subjects: Implications for Affective Disorders Mario Liotti, Helen S. Mayberg, Stephan K. Brannan, Scott McGinnis, Paul Jerabek, and Peter T. Fox Background: Affective disorders are associated with comorbidity of depression and anxiety symptoms. Positron emission tomography resting-state studies in affective disorders have generally failed to isolate specific symptom effects. Emotion provocation studies in healthy volunteers have produced variable results, due to differences in experimental paradigm and instructions. Methods: To better delineate the neural correlates of sad mood and anxiety, this study used autobiographical mem- ory scripts in eight healthy women to generate sadness, anxiety, or a neutral relaxed state in a within-subject design. Results: Sadness and anxiety, when contrasted to a neutral emotional state, engaged a set of distinct para- limbic– cortical regions, with a limited number of common effects. Sadness was accompanied by specific activations of the subgenual cingulate area (BA) 25 and dorsal insula, specific deactivation of the right prefrontal cortex BA 9, and more prominent deactivation of the posterior parietal cortex BAs 40/7. Anxiety was associated with specific activations of the ventral insula, the orbitofrontal and anterior temporal cortices, specific deactivation of para- hippocampal gyri, and more prominent deactivation of the inferior temporal cortex BAs 20/37. Conclusions: These findings are interpreted within a model in which sadness and anxiety are represented by segregated corticolimbic pathways, where a major role is played by selective dorsal cortical deactivations during sadness, and ventral cortical deactivations in anxiety. Biol Psychiatry 2000;48:30 – 42 © 2000 Society of Bio- logical Psychiatry Key Words: Sadness, anxiety, depression, positron emis- sion tomography, limbic system, dorsal/ventral pathways Introduction A ffective disorders as a group are commonly associ- ated with comorbidity of depression and anxiety symptoms. This comorbidity has implications for treat- ment as well as for strategies to understand underlying brain mechanisms (Mineka et al 1998). Although resting- state positron emission tomography (PET) studies of anxiety have been unrevealing, resting-state PET studies of depression, though generally dealing with syndromal markers, have suggested some symptom-specific changes. Using correlational analysis, some authors have identified associations with severity (e.g., Baxter et al 1989; Dolan et al 1992; Drevets et al 1997; Mayberg et al 1994), whereas studies focusing on other syndromal features, although provocative, have not identified reliable symptom pat- terns, including sad mood and anxiety (Bench et al 1993; Dolan et al 1992; Mayberg et al 1994). An alternative strategy commonly used to delineate brain regions mediating specific behaviors including sad mood and anxiety is the use of emotion provocation in healthy subjects (Gemar et al 1997; George et al 1995; Lane et al 1997b; Pardo et al 1993; Partiot et al 1995; Reiman et al 1997). Results have been highly variable, partially reflecting different induction paradigms, tasks, and instructions. Most importantly, it has been shown that picture-driven emotion (externally generated) and memo- ry-driven emotion (internally generated) involve by a large extent different regional changes (Lane et al 1997b; Reiman et al 1997). Given that these methodological confounds are con- trolled, a relative validation that a set of regions mediating a normal behavior is relevant to a disease state (such as in the cases of transient sadness vs. depression, and normal vs. pathological anxiety) is the demonstration that some or all brain regions mediating the normal emotional state colocalize with changes seen in patients with affective disorders. Additional corroboration is provided by changes in some or all of the identified regions with clinical remission. Using this approach, we recently demonstrated From the Research Imaging Center (ML, HSM, SKB, SM, PJ, PTF) and the Departments of Psychiatry (ML, HSM, SKB, PTF), Radiology (ML, HSM, PJ, PTF), and Medicine (ML, HSM, PTF), The University of Texas Health Science Center, San Antonio. HSM is currently affiliated with the Rotman Centre, Baycrest Centre for Geriatric Care, Toronto, Canada. Address reprint requests to Mario Liotti, M.D., Ph.D., University of Texas Health Science Center, Research Imaging Center, RIC, 7703 Floyd Curl Drive, San Antonio TX 78264. Received July 8, 1999; revised February 25, 2000; accepted March 2, 2000. © 2000 Society of Biological Psychiatry 0006-3223/00/$20.00 PII S0006-3223(00)00874-X














![RESEARCH ARTICLE Open Access Abnormalities of cortical ......campus [18], and basal ganglia [19]. These abnormal brain regions are predominantly located in the limbic-cortical-striatal-pallidal-thalamic](https://static.fdocuments.net/doc/165x107/60c2168295781709ed2436d2/research-article-open-access-abnormalities-of-cortical-campus-18-and.jpg)