Differential Diagnosis of the Lumbar Spine and Lower Extremity Nerve · PDF file ·...
Transcript of Differential Diagnosis of the Lumbar Spine and Lower Extremity Nerve · PDF file ·...

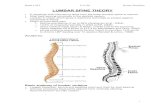
Differential Diagnosis of the Lumbar Spine and
Lower Extremity Nerve Entrapment
Cody J. Mansfield, PT, DPT, OCS, AT Paul Tadak, PT, DPT OCS, FAAOMPT Jake Bleacher, PT, OCS, FAAOMPT
Description of Presentation This presentation will benefit physical therapist in Ohio seeking board certification in orthopedics. To pass the orthopedic certified specialty (OCS) examination, physical therapist need to have an expert level knowledge of the lumbosacral plexus and lower extremity nerves. The presentation will help physical therapists differentiate between pathologies of the lumbar spine referring symptoms to the lower extremities and lower extremity neuropathies. Not only is this knowledge pertinent to pass the OCS exam, but also it is important to deliver exemplarily care to our patients. The presentation will focus on case based learning with audience interaction, review of anatomy, nerve distributions, and how to apply the information clinically. Agenda 9:00 AM- 10:15 AM
• Case # 1 o Presented by Cody Mansfield.
• Case # 2 o Presented by Cody Mansfield. o Brief demonstration by Paul Tadak of MDT directional preference lumbar
exam. 10:15 AM - 10:30 AM
• Intermission.
• Let us know how the presentation is going.
• Tweet at @MansfieldCody, @PaulTadak, @jbleacherpt
• #OPTAAC2017
10:30 AM - 11:45 AM
• Case # 3 o Presentation by Paul Tadak
• Case # 4 o Presentation by Jake Bleacher.
• Closing remarks

DISCLAIMER *** We are not sharing our slides, because we don’t want the audience to know ahead of time what the outcomes of the cases are. We think this will make for a better presentation.***
At the very end of the hand out you will find practice OCS-like questions.

References for presentation: Reiman MP, Hash TW 2nd, Mather RC 3rd. Acetabular Paralabral Cyst: An Unusual Cause of Lower Extremity Pain and Paresthesia. J Orthop Sports Phys Ther. 2016 Jan;46(1):35. doi: 10.2519/jospt.2016.0402. PubMed PMID: 26721454. Sizer PS Jr, Brismée JM, Cook C. Medical screening for red flags in the diagnosis and management of musculoskeletal spine pain. Pain Pract. 2007 Mar;7(1):53-71. Review. PubMed PMID: 17305681. Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin. 2007 May;25(2):387-405. Review. PubMed PMID: 17445735. Crowell MS, Gill NW. Medical screening and evacuation: cauda equina syndrome in a combat zone. J Orthop Sports Phys Ther. 2009 Jul;39(7):541-9. doi: 10.2519/jospt.2009.2999. PubMed PMID: 19574660. Reiman MP, Thorborg K. Clinical examination and physical assessment of hip joint-related pain in athletes. Int J Sports Phys Ther. 2014 Nov;9(6):737-55. PubMed PMID: 25383243; PubMed Central PMCID: PMC4223284. Fritz JM, Delitto A, Welch WC, Erhard RE. Lumbar spinal stenosis: a review of current concepts in evaluation, management, and outcome measurements. Arch Phys Med Rehabil. 1998 Jun;79(6):700-8. Review. PubMed PMID: 9630153. McCrory P, Bell S. Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med. 1999 Apr;27(4):261-74. Review. PubMed PMID: 10367335. Alrwaily M, Timko M, Schneider M, Stevans J, Bise C, Hariharan K, Delitto A. Treatment-Based Classification System for Low Back Pain: Revision and Update. Phys Ther. 2016 Jul;96(7):1057-66. doi: 10.2522/ptj.20150345. Epub 2015 Dec 4. PubMed PMID: 26637653. Delitto A, George SZ, Van Dillen LR, Whitman JM, Sowa G, Shekelle P, Denninger TR, Godges JJ; Orthopaedic Section of the American Physical Therapy Association. Low back pain. J Orthop Sports Phys Ther. 2012 Apr;42(4):A1-57. doi: 10.2519/jospt.2012.0301. Epub 2012 Mar 30. PubMed PMID: 22466247; PubMed Central PMCID: PMC4893951. Mansfield, CJ. Cervical Myelopathy Mimicking Lumbar Stenosis. Physiotherapy Theory and Practice. Under review. Mansfield CJ, Bleacher J, Tadak P, Briggs M. Differential Diagnosis for Tingling in Toes. JMMT. 2016. Logullo F, Ganino C, Lupidi F, Perozzi C, Di Bella P, Provinciali L. Anterior tarsal tunnel syndrome: a misunderstood and a misleading entrapment neuropathy. Neurol Sci. 2014 May;35(5):773-5. doi: 10.1007/s10072-013-1601-8. Epub 2013 Dec 12. PubMed PMID: 24337947. Craig A. Entrapment neuropathies of the lower extremity. PM R. 2013 May;5(5 Suppl):S31-40. doi: 10.1016/j.pmrj.2013.03.029. Epub 2013 Mar 28. Review. PubMed PMID: 23542774.

Practice OCS-like questions are shared with the permission of www.FastTwitchPress.com Questions #1-3 are based on the following vignette.
Question #1
A. Sciatic nerve B. Femoral nerve C. Saphenous nerve D. Tibial nerve Question #2
A. Passive hip flexion, knee extension, dorsiflexion B. Passive hip extension, knee flexion, plantar flexion C. Passive hip flexion, knee extension, dorsiflexion, eversion D. Passive hip flexion, knee extension, dorsiflexion, inversion
A 30-year-old female accountant is referred to physical therapy with complaints of sharp pain originating in the left groin and radiating to the medial aspect of upper thigh, lower leg and foot.
What nerve is most likely affected?
How would you assess the neurodynamics of the nerve affected in this case?

Question #3
A. Acetabular labral cyst B. L3-L4 disc herniation C. Adhesion of the gracilis D. Hip osteoarthritis
You are able to reproduce the patient’s symptoms with your neurodynamics testing. Further questioning reveals that she only experiences the sharp pain and radicular symptoms with sitting. Your repeated motions testing of the lumbar spine has no effect on the patient’s symptoms. Examination of the hip reveals a positive FADIR
test, passive range of motion of the left hip to 105° of flexion, 5° of
extension and 12° of internal rotation. The right hip was within normal
limits for all testing. What is the most likely diagnosis?

Question #1
A. Sciatic nerve B. Femoral nerve C. Saphenous nerve The paresthesias experienced by this patient are in a saphenous nerve sensory distribution. D. Tibial nerve PubMed Citation: Reiman MP, Hash TW 2nd, Mather RC 3rd. Acetabular
Paralabral Cyst: An Unusual Cause of Lower Extremity Pain and Paresthesia. J Orthop Sports Phys Ther. 2016 Jan;46(1):35. doi: 10.2519/jospt.2016.0402. PubMed PMID: 26721454.
Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/26721454 Question #2
A. Passive hip flexion, knee extension, dorsiflexion Neurodynamic testing with sciatic nerve bias. B. Passive hip extension, knee flexion, plantar flexion Neurodynamic testing with femoral nerve bias. C. Passive hip flexion, knee extension, dorsiflexion, eversion The combination of these movements will put increased tension on the saphenous nerve and likely reproduce the patient’s concordant symptoms. D. Passive hip flexion, knee extension, dorsiflexion, inversion Neurodynamic testing with tibial nerve bias. PubMed Citation: Reiman MP, Hash TW 2nd, Mather RC 3rd. Acetabular
Paralabral Cyst: An Unusual Cause of Lower Extremity Pain and Paresthesia. J Orthop Sports Phys Ther. 2016 Jan;46(1):35. doi: 10.2519/jospt.2016.0402. PubMed PMID: 26721454. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/26721454
What nerve is most likely affected?
How would you assess the neurodynamics of the nerve affected in this
case?

Question #3
A. Acetabular labral cyst Give then patient’s positive hip findings, limited hip range of motion, and inconclusive lumbar spine examination, you should suspect answer choice A as the primary pathology. Refer the reference below for a short case describing an acetabular paralabral cyst compressing the medial femoral neurovascular bundle. B. L3-L4 disc herniation Lumbar evaluation was inconclusive. Groin pain is a common pain referral pattern for acetabular labral pathology. Also, the majority of lumbar disc herniations occur at the L4-L5 and L5-S1 levels. C. Adhesion of the gracilis Gracilis follows the path of the saphenous nerve, however this is not the best answer given the positive findings at the hip. D. Hip osteoarthritis Hip osteoarthritis could be a factor, however she is under 50-years-old and less likely to have significant arthritis. PubMed Citation: Reiman MP, Hash TW 2nd, Mather RC 3rd. Acetabular
Paralabral Cyst: An Unusual Cause of Lower Extremity Pain and Paresthesia. J Orthop Sports Phys Ther. 2016 Jan;46(1):35. doi: 10.2519/jospt.2016.0402. PubMed PMID: 26721454. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/26721454
You are able to reproduce the patient’s symptoms with your neurodynamics testing. Further questioning reveals that she only experiences the sharp pain and radicular symptoms with sitting. Your repeated motions testing of the lumbar spine has no effect on the patient’s symptoms. Examination of the hip reveals a positive FADIR
test, passive range of motion of the left hip to 105° of flexion, 5° of
extension and 12° of internal rotation. The right hip was within normal
limits for all testing. What is the most likely diagnosis?

Question #4
A. Rheumatoid arthritis B. Central sensitization C. Whiplash associated disorder D. Back pain with Lhermittes sign
A patient presents to you with a 10 year history of back pain. She reports having global pain along her entire upper and lower back. She states that any quick movements increase her pain to a 10/10. She said that all of her pain stems from a car accident that occurred 10 years ago at a traffic stop light. What condition does the patient most
likely present with?

Question #4
A. Rheumatoid arthritis Autoimmune disorder that commonly affects wrist and hands. B. Central sensitization The patient in this case demonstrates classic signs of central sensitization and will benefit from a multidisciplinary approach of specific rehabilitation, psychotherapy, and pharmacological management. The patient may have initially had symptoms of whiplash associated disorder, but the severity of pain has lasted well beyond the regular time frame for healing and may not follow an anatomical pattern. C. Whiplash associated disorder Symptoms can last as long as two years after a motor vehicle accident. Symptoms would be unlikely to last 10 years. D. Back pain with Lhermittes sign Electrical sensation radiates into back and extremities that is reproducible with cervical flexion. Suggestive of spinal cord pathology. PubMed Citation: Alrwaily M, Timko M, Schneider M, Stevans J, Bise C, Hariharan
K, Delitto A. Treatment-Based Classification System for Low Back Pain: Revision and Update. Phys Ther. 2015 Dec 4. [Epub ahead of print] PubMed PMID: 26637653. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/26637653
A patient presents to you with a 10 year history of back pain. She reports having global pain along her entire upper and lower back. She states that any quick movements increase her pain to a 10/10. She said that all of her pain stems from a car accident that occurred 10 years ago at a traffic stop light. What condition does the patient most
likely present with?

Question #5
A. Magnetic Resonance Imaging B. Radiograph C. Diagnostic ultrasound D. Myelography and CT scan
A 25-year-old female presents to you in a direct access setting with intermittent low back pain that started four weeks ago. You go to the waiting room and see that she is in a wheel chair due to lower extremity weakness. She reports that her symptoms have worsened within the last few days. She complains of incontinence and decreases sensation
in the perianal region. What imaging modality is most recommended?

Question #5
A. Magnetic Resonance Imaging According to the American College of Radiology Appropriateness Guidelines, MRI is the imaging modality of choice when cauda equina syndrome is suspected. B. Radiograph C. Diagnostic ultrasound D. Myelography and CT scan PubMed Citation: O'Laughlin SJ, Kokosinski E. Cauda equina syndrome in a
pregnant woman referred to physical therapy for low back pain. J Orthop Sports Phys Ther. 2008 Nov;38(11):721. doi: 10.2519/jospt.2008.0411. PubMed PMID: 18978454. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/18978454
A 25-year-old female presents to you in a direct access setting with intermittent low back pain that started four weeks ago. You go to the waiting room and see that she is in a wheel chair due to lower extremity weakness. She reports that her symptoms have worsened within the last few days. She complains of incontinence and decreases sensation
in the perianal region. What imaging modality is most recommended?

Question #6
A. L3 B. L4 C. L5 D. S1
If a patient experiences a L3-L4 disc herniation, which nerve root is most likely to be affected based on the anatomical orientation of the nerves?

Question #6
A. L3 B. L4 Although the L3 nerve root goes beneath the L3 vertebrae, based on the orientation of the nerves, it is most likely to affect the L4 nerve root. C. L5 D. S1 PubMed Citation: Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin.
2007 May;25(2):387-405. Review. PubMed PMID: 17445735. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/17445735
If a patient experiences a L3-L4 disc herniation, which nerve root is most likely to be affected based on the anatomical orientation of the nerves?

Question #7
A. Symptoms decrease with sitting B. Symptoms are abolished with sitting C. Symptoms improved walking with shopping cart D. Pain below buttocks
Which of the following has the best utility to diagnose lumbar spinal
stenosis?

Question #7
A. Symptoms decrease with sitting B. Symptoms are abolished with sitting All of the answer choices are suggestive have lumbar spinal stenosis, however, only answer choice B has the highest specificity. C. Symptoms improved walking with shopping cart D. Pain below buttocks PubMed Citation: Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH,
Chang LC, Lipson SJ. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995 Sep;38(9):1236-41. PubMed PMID: 7575718. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/7575718
Which of the following has the best utility to diagnose lumbar spinal stenosis?

Question #8
A. Vascular claudication B. Chronic exertional compartment syndrome C. Lumbar stenosis D. Neurogenic claudication
A 70-year-old female patient referred to physical therapy for low back pain reports that her primary complaint is bilateral cramping sensation after walking 200 feet and when riding a bike for 15 minutes. What is causing her cramping?

Question #8
A. Vascular claudication Answer choices C and D are similar and therefore can be eliminated, since lumbar stenosis commonly causes neurogenic claudicaiton. Lumbar stenosis causes neurogenic claudication. Patient’s symptoms are not suggestive of chronic exertional compartment syndrome. The patient has symptoms with both walking and riding a bike, which would indicate vascular claudication. A patient with symptoms of neurogenic claudication due to lumbar stenosis would likely have symptoms with walking but not with riding the bike. B. Chronic exertional compartment syndrome C. Lumbar stenosis D. Neurogenic claudication PubMed Citation: Fritz JM, Delitto A, Welch WC, Erhard RE. Lumbar spinal
stenosis: a review of current concepts in evaluation, management, and outcome measurements. Arch Phys Med Rehabil. 1998 Jun;79(6):700-8. Review. PubMed PMID: 9630153. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/9630153
A 70-year-old female patient referred to physical therapy for low back pain reports that her primary complaint is bilateral cramping sensation after walking 200 feet and when riding a bike for 15 minutes. What is causing her cramping?

Question Type #9-15 are based on the following vignette.
Question #9
A. Disc herniation producing radiculopathy B. Spinal stenosis C. Cauda equina syndrome D. Myasthenia gravis Question #10
A. < 12 hours B. < 48 hours C. < 72 hours D. < 96 hours
A 45-year-old male patient presents to a physical therapist in a direct access outpatient orthopedic clinic. He complains of intermittent low back pain that worsened recently after picking up a box from the ground. He reported radicular symptoms into his right thigh to above his knee. No red flags are present and his symptoms improve with repeated active lumbar extension. Symptoms worsen with repeated active lumbar flexion. Symptoms appear to be due to disc pathology. A week later he reports to the physical therapist with worsening constant low back pain and complaints of symptoms suggestive of urinary retention. He has bilateral radiculopathy along posterior aspect of his thighs. Your examination reveals hyporeflexive plantar flexor deep tendon reflexes and decreased sphincter tone.
The patient’s symptoms a week after the first visit are suggestive of
what pathology?
What is the maximum time the patient can wait before undergoing surgery for this pathology?

Question #11
A. Increase in anal sphincter tone B. Perianal sensation deficit C. No anal wink or cremasteric reflex D. Urinary retention Question #12
A. Diagnostic ultrasound B. Radiographs C. CT scan D. MRI Question #13
A. Primary care physician B. Urgent Care C. Emergency Department D. Neurosurgeon
All of the following items are suggestive of the pathology in this vignette except for what?
Once the pathology from this vignette is identified, which imaging modality is most recommended?
What would be the most appropriate referral for the patient in this vignette?

Question #14
A. Ablation of sacral nerves B. Laminectomy and discectomy C. L4-L5 fusion D. L5-S1 fusion Question #15
A. L1-L2 and L3-L4 B. L2-L3 and L4-L5 C. L4-L5 and L5-S1 D. L2-L3 and L5-S1
Which surgical procedure is most indicated for the pathology in this
vignette?
Which are the most common levels for a disc herniation to occur?

Question #9
A. Disc herniation producing radiculopathy B. Spinal stenosis C. Cauda equina syndrome Progressive neurological deficits, bilateral lower extremity radiculopathy, urinary retention, hyporeflexive deep tendon reflexes, and decreased sphincter tone are all suggestive of cauda equina syndrome. D. Myasthenia gravis PubMed Citation: Crowell MS, Gill NW. Medical screening and evacuation: cauda
equina syndrome in a combat zone. J Orthop Sports Phys Ther. 2009 Jul;39(7):541-9. doi: 10.2519/jospt.2009.2999. PubMed PMID: 19574660. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/19574660 Question #10
A. < 12 hours B. < 48 hours C. < 72 hours Surgical intervention for cauda equina syndrome needs to be performed within 72 hours to decrease risk of permanent neurological compromise. Surgical intervention less than 48 hours from onset of symptoms has been associated with better outcomes. D. < 96 hours PubMed Citation: Crowell MS, Gill NW. Medical screening and evacuation: cauda
equina syndrome in a combat zone. J Orthop Sports Phys Ther. 2009 Jul;39(7):541-9. doi: 10.2519/jospt.2009.2999. PubMed PMID: 19574660. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/19574660
The patient’s symptoms a week after the first visit are suggestive of
what pathology?
What is the maximum time the patient can wait before undergoing surgery for this pathology?

Question #11
A. Increase in anal sphincter tone Since cauda equina syndrome is a lower motor neuron injury, you would expect a decrease in in anal sphincter tone, not an increase. B. Perianal sensation deficit C. No anal wink or cremasteric reflex D. Urinary retention PubMed Citation: Crowell MS, Gill NW. Medical screening and evacuation: cauda
equina syndrome in a combat zone. J Orthop Sports Phys Ther. 2009 Jul;39(7):541-9. doi: 10.2519/jospt.2009.2999. PubMed PMID: 19574660. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/19574660 Question #12
A. Diagnostic ultrasound B. Radiographs C. CT scan D. MRI For signs and symptoms suggestive of cauda equina syndrome, MRI is the preferred first line imaging modality. PubMed Citation: Crowell MS, Gill NW. Medical screening and evacuation: cauda
equina syndrome in a combat zone. J Orthop Sports Phys Ther. 2009 Jul;39(7):541-9. doi: 10.2519/jospt.2009.2999. PubMed PMID: 19574660. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/19574660
All of the following items are suggestive of the pathology in this vignette except for what?
Once the pathology from this vignette is identified, which imaging
modality is most recommended?

Question #13
A. Primary care physician B. Urgent Care C. Emergency Department D. Neurosurgeon All answer choices are appropriate, however, the most preferred immediate referral option, is to a neurosurgeon or an orthopedic spine surgeon. PubMed Citation: Crowell MS, Gill NW. Medical screening and evacuation: cauda
equina syndrome in a combat zone. J Orthop Sports Phys Ther. 2009 Jul;39(7):541-9. doi: 10.2519/jospt.2009.2999. PubMed PMID: 19574660. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/19574660 Question #14
A. Ablation of sacral nerves B. Laminectomy and discectomy The preferred surgical intervention is a laminectomy followed by discectomy in order to decompress the nerves. C. L4-L5 fusion D. L5-S1 fusion PubMed Citation: Crowell MS, Gill NW. Medical screening and evacuation: cauda
equina syndrome in a combat zone. J Orthop Sports Phys Ther. 2009 Jul;39(7):541-9. doi: 10.2519/jospt.2009.2999. PubMed PMID: 19574660. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/19574660
What would be the most appropriate referral for the patient in this vignette?
Which surgical procedure is most indicated for the pathology in this vignette?

Question #15
A. L1-L2 and L3-L4 B. L2-L3 and L4-L5 C. L4-L5 and L5-S1 Lumbar radiculopathy most commonly affects the L4-L5 and L5-S1 disc space. Of 40,000 operations, 95% of disc herniations were at these two levels. D. L2-L3 and L5-S1 PubMed Citation: Dohrmann GJ, Mansour N. Long-Term Results of Various
Operations for Lumbar Disc Herniation: Analysis of over 39,000 Patients. Med Princ Pract. 2015;24(3):285-90. doi: 10.1159/000375499. Epub 2015 Mar 27. PubMed PMID: 25832729. Link to Article: http://www.ncbi.nlm.nih.gov/pubmed/25832729
Which are the most common levels for a disc herniation to occur?