Development of a real-world evidence platform for MPS Type ...
Transcript of Development of a real-world evidence platform for MPS Type ...

Development of a real-world evidence platformfor MPS Type III (Sanfilippo Syndrome) Kristina Cotter, MS, PhD, CGC; Charlene Fernandez, BS; Brenda Simpson, BS; Nancy Yu, BA, BS AllStripes Research, San Francisco, CA (formerly RDMD); [email protected]
Introduction
Objectives
Methods
ResultsMPS III is a rare, autosomal recessive lysosomal storage condition characterized by progressive neurocognitive decline, behavioral issues, and systemic complications starting in early childhood. There are four subtypes (A, B, C, and D); Types A and B are more common than C and D. Significant phenotypic heterogeneity exists within and between the subtypes. There are no approved disease-modifying therapies available for MPS III. Robust natural history (NH) data is needed, particularly in Types C and D, to facilitate clinical trial design, decrease time to diagnosis, and guide future management.
Traditional NH studies are site-based and require significant resources to capture longitudinal data. This is challenging in rare diseases, wherein small patient populations are spread across wide geographic areas. Additionally, the clinical complexity of MPS III often requires patients to receive care from multiple institutions, complicating retrospective chart reviews. Real-world data (RWD), or data collected outside of clinical trials, can be used to generate real-world evidence (RWE) that describes the pre- and post-diagnostic journeys of patients with rare diseases. Here, we demonstrate that a RWD platform can be utilized to collect comprehensive, longitudinal clinical data for a cohort of MPS III patients.
1. Utilize a RWD platform to collect clinical data from the medical records of MPS III patients
2. Assess the feasibility of utilizing a RWD platform to abstract longitudinal clinical data for a larger NH study
This work was performed in compliance with Western IRB. A broad, umbrella consent was developed to allow for de-identified data from medical records to be used in minimal risk research.
Cohort: Recruitment occurred via digital marketing and collaboration with the Cure Sanfilippo Foundation. Parents / guardians were asked to sign a HIPAA release, provide a list of hospitals and clinics where the patient receives care, and to sign a consent form approved under a central IRB. Complete medical records were requested and digitized; re-requests were made every 6-12 months. Individuals were included in the study if clinical notes confirmed a genetic diagnosis of MPS III.
Clinical Data Abstraction: In order to structure patient journeys, an iterative protocol consisting of clinical modules that define data to abstract from medical records was developed. When possible, modules were designed according to CDASH standards. Modules included: demographics, diagnosis, medical history, procedures, and genetic testing. During abstraction into the AllStripes database, an electronic audit trail to the source documents was maintained for quality assurance.
Data Analysis: Structured, de-identified data was exported, and analysis was performed using descriptive statistics. Analysis was only performed on data abstracted from patients whose guardians consented to research.
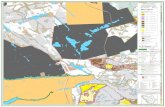
Figure 1: AllStripes RWD Platform Workflow
Figure 2: MPS III Cohort Demographics
Total N (%) Male (%) Female (%)AllStripes MPS III Cohort 32 - -Consented with Records 21 (65.6%) 8 (38.1%) 13 (61.9%)
Twenty-one guardians consented to research and had patient medical records for review. The mean patient age was 9.6 years (SD±5.4); a majority of the cohort was female and from the South or Northeastern regions of the United States.
Figure 3: MPS III Medical Record Assessment
19%
29%33%
19%
Age Distribution
1-4 years
5-9 years
10-14 years
15+ years
Geographic Distribution (N)
Figure 4: Diagnosis of MPS III
Figure 5: MPS III Genetic Testing
Figure 6: Top Signs & Symptoms of MPS III
Discussion
Median Min MaxHospitals Listed by Guardian 4 1 20Clinical Documents Available 172 24 2,805Years of Data 5 1 16
90.5%
Patients with Pre-Diagnostic Data Available
Category % Patients
Genetics 90.5%
Radiology & Imaging 85.7%
General Practitioner 85.7%
Psych & Development 76.2%
Audiology 71.4%
Common Document Types
N %Genetic Testing 15 71.4%Enzymatic Testing Only (genetic report unavailable) 2 9.5%
Clinician Confirmation Only 4 19.1%
Confirmation of Diagnosis
*Represents confirmation by the AllStripes research team upon review of records.
0 50 100 150 200 250 300
Max: 257 mo (21.4 yrs)
Min: 3 mo
Median: 50.5 mo (4.2 yrs)
Age of Diagnosis
N=20; one patient did not have date of diagnosis recorded In medical records.
Study ID Gene Allele 1 / Allele 2 Study ID Gene Allele 1 / Allele 21 HGSNAT SP / MS 13 SGSH MS / MS2 NAGLU TR / FS 14 SGSH MS / MS3 HGSNAT MS / MS 15 NAGLU MS / MS (1 VUS)
4 NAGLU TR / MS 16 SGSH TR / MS5 NAGLU TR / MS 19 SGSH MS / MS6 SGSH MS / MS 20 SGSH MS / MS7 SGSH FS / MS 21 SGSH MS / MS11 SGSH MS / MS
SP = Splice site; MS = Missense; TR = Truncating; FS = Frameshift; VUS = Lab report classified variant as a variant of uncertain significance
Age (months)
Figure 7: Surgical & Procedure History
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Chronic Otiti
s Media
Speech
& Langu
age Delay
Behavioral
Issues
Developmental D
elay or ID
GI Issu
es
Gross or F
ine Motor D
elay
Hearing Lo
ss
Coarse Fa
cial F
eatures
Autism
Seizu
res
Vision Iss
ues
Hepatomegaly
Macroce
phaly
Umbilical o
r Inguinal H
ernia
Hypotonia
Scolio
sis
Perc
enta
ge o
f MPS
III C
ohor
t
53%26%
21%
MPS III Subtype
A
B
C
D
Conclusions This study was a pilot study to assess the feasibility of using a RWD platform to structure clinical insights from the medical records of MPS III patients. We demonstrated that our site-less model allows for patient recruitment without the geographic restrictions present in traditional observational studies. We were also able to collect and review records from multiple hospitals per patient, allowing for structuring of complete patient journeys from pre-diagnosis through management. Given that our research consent allows for patient recontact, we can re-engage patients and families over time to ensure that the database is kept up to date.
Using five clinical modules, we were able to confirm patient diagnosis, glean insights regarding healthcare utilization, and characterize the cohort by frequent MPS III-related signs and symptoms. Future work will focus on expanding the MPS III protocol to allow for structuring of longitudinal MPS III patient journeys in a larger cohort. This data can be used as a part of natural history studies, to assist in clinical trial design, and to understand healthcare patterns and utilization in rare diseases such as MPS III.
Acknowledgements AllStripes would like to thank the Cure Sanfilippo Foundation for assisting in recruitment, providing research advice, and for their partnership. AllStripes would also like to thank the patients and families who have generously contributed their data to help make this study possible.
References 1. Whitley et al (2018). The Journal of Pediatrics 197:198 2. Delgadillo et al (2013). Orphanet Journal of Rare Diseases 8:1893. Wagner and Northrup (2019). GeneReviews: Mucopolysaccharidosis Type III
The majority of guardians listed > 1 hospital or clinic. Medical records were requested from birth to date of sign-up, allowing for pre-diagnostic data to be captured for the majority of patients. All clinical documents were classified by specialty and note type; the most common document types available for review were clinical genetic notes and genetic testing.
The majority of patients in the cohort have MPS III Type A. While genetic or enzymatic testing was available for most patients, 19% did not have confirmatory testing available in the medical records for review. Future assessment of genetic testing reports for all patients may require guardian recontact for additional information. All guardians consented to recontact.
Genetic test results were available for 15 patients. Variants were classified by variant type; missense variants were most common across all represented subtypes.
Most Common MPS III-Related Signs and Symptoms
MPS III-related signs and symptoms were abstracted from the medical records and the frequency of each was assessed across the cohort. Signs and symptoms identified pre- and post-diagnosis were included in analysis.
Patients with Surgeries / Procedures in Records: 19 (90.5%)
Procedure % of Total Procedures
PE Tube Placement 20.7%
Myringotomy 18.6%
Adenoidectomy 12.1%
ABR Testing 10.0%
Tonsillectomy 5.0%
Most Common Surgeries / Procedures
*Of the n=140 procedures identified in the MPS III cohort medical records
*Of patients with surgeries / procedures in medical record (n=19)
0 5 10 15 20Number of Procedures / Surgeries
Min: 1 Max: 19
Median: 6
Number of Surgeries / Procedures in Records
Total Surgeries / Procedures Identified in MPS III Cohort Records: 140
All surgeries & procedures were abstracted from the medical records and the frequency of each procedure type was assessed across the cohort.
Limitations This was a small feasibility study and should not be considered a representative sample of all MPS III patients. Hospital lists are also provided by guardians and there may be unidentified gaps in care. Additionally, the results must be interpreted within the context of the limitations of RWD.
Data from Participants Unstructured medical records
Physician notes
Genetic reports Surgeries & Procedures
Labs & Imaging
Rxhistory
Participant-Facing Portal AllStripes Clinical Portal
RWD Abstraction Platform
ü21 CFR 11
üRobust audit trail üFlexible protocol
üCentral IRB & Consent üDe-identification
Research PortalStructured data Research & insights
Demographics Doctors & facilities
Consent & recontact Survey Questions
N=1 in Canada
34
8
5