De Biologie van de Mannelijke Fertiliteit infertility • Impaired semen quality –Below WHO...
Transcript of De Biologie van de Mannelijke Fertiliteit infertility • Impaired semen quality –Below WHO...
De Biologie van de
Mannelijke Fertiliteit
Sjoerd Repping, PhD
Professor of Human Reproductive Biology
Academic Medical Center, University of Amsterdam,
Amsterdam, the Netherlands ([email protected])
Apale Adark
B
Pre-Leptotene
Leptotene
Zygotene
Pachytene
Diplotene
50%50%
1st meiotic division
Spermatogenesis
spermatogonia
Male infertility
• Impaired semen quality
– Below WHO guidelines
– Correlation between semen quality and chance of pregnancy
WHO guidelines, (1999, 2010), Van der Steeg, et al., F&S (2010)
Causes of male infertility
• Causative factors
– Hyperprolactinemia
– Hypogonadotrophic hypogonadism
– Bilateral cryptorchidism
– Orchitis
– Previous chemo- or radiotherapy
– Genetic causes
• Numerical and structural chromosome abnormalities
• Y-chromosome deletions
• More than 80% of unknown cause
Silber & Repping, HRU (2002), Visser & Repping, Reproduction (2010)
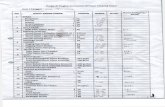
Variability in sperm count
WHO Laboratory Manual for the Examination of Human Semen
and Sperm-Cervical Mucus Interaction (1999)
Patients and controls
• Patients– Men with reduced semen quality according to WHO criteria
– Known causes of spermatogenic failure excluded
• Controls– Proven fertile fathers
• Non-paternity excluded?
• (severely) oligozoospermic men can father children
– Vasectomy reversals
• Pre-operative sperm count unknown
– Population controls
• Sperm count unknown
– Men with proven normal spermatogenesis
• Cohort based approach– Methodologically more powerful
• No a priori distinction between healthy and ill
• Comparison of genetically affected vs unaffected
Sperm production variation
Consecutively included cohort male partners of subfertile couples
(n=1,041)
Median concentration: 52 x106/ml
Median total count: 149 x106
Our view on spermatogenesis
Spermatogenesis is a quantitative trait
Obstructive azoospermiaNon-obstructive azoospermia
(sperm with TESE)
Non-obstructive azoospermia
(no sperm with TESE)
Many (genetic) factors control
the rate of sperm production
Testis Epididymis / Vas / Duct Ejaculate
Established genetic causes
• Karyotype abnormalities
– Klinefelter syndrome (47, XXY)
– Translocations
• Y-chromosome aberrations
– Deletions
– Isodicentric Y-chromosomes
• Monogenic disorders
– Kallmann syndrome
– Cystic Fibrosis mutations (CBAVD)
sperm count (x106 / ml)
n
“normal”
population
gr/grAZFc
5x106 / ml
Y-chromosome deletions
AZFa
P5/P1
Treatment of male infertility
• General treatment
– Intra cytoplasmic Sperm Injection
• Treatment of the non-affected female partner
• Invasive / burdensome
• Rare cases
– Dopamine-agonist (hyperprolactinemia)
– Gonadotropins (hypogonadotropic hypogonadism)
• Future treatment
– Spermatogonial stem cell autotransplantation
• Especially in childhood cancer survivors
Nude mouse
40 mg/kg Busulphan treatment
4-6 weeks before transplantation
Xenotransplantation
Colonization?