Cysts of jaws1
-
Upload
fiza0727 -
Category
Health & Medicine
-
view
521 -
download
0
Transcript of Cysts of jaws1
Cyst
“Pathologic cavity having fluid , semi fluid, or gaseous content but not always lined by an epithelium.”
-KRAMER IN 1974
GENERAL DIAGNOSTIC FEATURES OF CYSTS
SIGNS SYMPTOMS
Factors affecting diagnosis Pain and swelling
Expansion Anesthesia or paresthesia
Enlargement Salty taste
Consistency Displacement of denture
Window formation Tooth discoloration
Fluid discharge
Effect on teeth
Topics of today’s discussionOdontogenic cysts
Gingival cyst Lateral periodontal cyst Calcifying odontogenic cyst Radicular cyst
Gingival cyst• Uncommon cyst of gingival soft tissue,
occuring either in the free or attached gingiva.
• Regarded as soft tissue counterpart of lateral periodontal cyst.
ETIOLOGY AND PATHOGENESIS :
• It may arise from odontogenic epithelial cell rests;
• by traumatic implantation of surface epithelium;
• or by cystic degeneration of deep projections of surface epithelium
CLINICAL FEATURES
Clinical photograph of a gingival cyst of an adult
AGE :5th – 6th decade of life
SITE : mandibular canine and Pre Molar area; attached gingiva or I/D papillaGENDER: male predominance
Signs and symptoms:• Slowly enlarging, well circumscribed painless
swelling.• Invariably occurs on facial aspect of free / attached
gingiva.• Dome shaped soft, fluctuant swelling which is
<1cm in diameter• Surface of lesion is smooth and of normal color of
gingiva or bluish.• Fluctuant lesion, adjacent teeth are vital.
LATERAL PERIODONTAL CYST
• Uncommon, but well recognized type of odontogenic cyst.
• The designation ‘lateral periodontal cyst’ is confined to those cysts that occur in the lateral periodontal position and in which an inflammatory etiology and a diagnosis of collateral OKC have been excluded on clinical and histological grounds
(Shear and Pindborg, 1975).
Etiology :Results from an early dentigerous cyst left in place after
tooth eruption Okc Rests of malassez Remanents of dental lamina
CLINICAL FEATURES
• Age : 20 – 60 years, peak in 6th decade.
• Sex : Male predilection.
• Site : Lateral PDL regions of mandibular canines and premolars, followed by anterior maxilla
Signs & symptoms
• Usually asymptomatic as it occurs on the lateral aspect of root of tooth.
• Occasionally pain and swelling may occur.
• Overlying mucosa appears normal in color.
• Associated teeth are vital, unless otherwise affected.
• Cysts rarely < 1cm in size. Except for the BOTRYOID VARIETY.
Radiological features
• Round to ovoid ‘lucency with sclerotic margins.
• Cyst can be present anywhere between cervical margin to root apex.
Radiograph of a lateral periodontal cyst lying between the mandibular premolar teeth. The margins are well corticated, indicative of slow enlargement.
Radiological features
Lateral periodontal cyst. Radiolucent lesionbetween the roots of a vital mandibular canine and first premolar.
Lateral periodontal cyst. A larger lesion causingroot divergence.
CALCIFYING ODONTOGENIC CYST
• Also called as Odontogenic ghost cell cyst or Gorlin cyst.
• It Has many features of odontogenic tumor, therefore it is placed in the category of tumors in the latest WHO classification of odontogenic cysts and tumors.
• In the latest WHO publication on odontogenic tumours (Prætorius and Ledesma-Montes, 2005) it was classified as a benign odontogenic tumour and was renamed calcifying cystic odontogenic tumour (CCOT).
Pathogenesis
• COC is a unicystic process and develops from the reduced dental epithelium or remnants of dental lamina.
• The cyst lining has the potential to induce formation of odontoma in adjacent CT wall.
Clinical features
• Age : Wide range, peak in 2nd – 3rd decade.
• Sex : slight female predilection
• Site : Anterior segment of both jaws
Signs & symptoms
• Swelling is the commonest complaint, seldom associated with pain.
• Intraosseous lesions can cause hard bony expansion and resulting in facial asymmetry.
• Displacement of teeth can also occur.
RADIOLOGICAL FEATURES
• Intraosseous lesions produce well defined lucency which is usually unilocular.
• Irregular calcified masses of varying sizes may be seen within the lucency.
• Displacement of root/roots with or without root resorption and expansion of cortical plates also seen
Radiograph of a calcifying odontogenic cyst of the maxilla. There is a well-demarcated margin and calcifications suggestive of tooth material.
DIFFERENTIAL DIAGNOSIS
Based on radiographic appearance, following lesions must be included in the provisional diagnosis –
• Ameloblastic fibro odontoma • Fibrous dysplasia• Ossifying fibroma
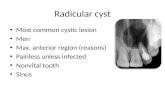
RADICULAR CYST
• Also called APICAL PERIODONTAL CYST
• Radicular cysts are the most common inflammatory cysts and arise from the epithelial residues in the periodontal ligament as a result of periapical periodontitis following death and necrosis of the pulp.
• Quite often a radicular cyst remains behind in the jaws after removal of the offending tooth and this is referred to as a residual cyst.
CLINICAL FEATURES
• Age : peak in 3rd, 4th and 5th decades.
• Sex : Slightly more in males.
• Site : Maxillary anterior region.
• Frequency: Commonest cystic lesion of jaws.
Signs & symptoms
• Primarily symptom less.
• Discovered accidentally during routine dental X ray exam.
• Slowly enlarging hard bony swelling initially. Later, if cysts breaks through cortical plates, lesion becomes fluctuant.
• Diagnostic criteria – associated teeth are non vital
• Rare in deciduous teeth.
RADIOLOGICAL FEATURES
• Classically presents as round / ovoid lucency with sclerotic borders and associated with pulpally affected tooth / teeth.
• If infection supervenes, the margins become indistinct, making it impossible to distinguish it from a peripaical granuloma.
Radiograph of a radicular cyst. The lesion is a well defined radiolucency associated with the apex of a non-vital root filled tooth.
DIFFERENTIAL DIAGNOSIS:
Following lesions must be distinguished from other periapical radiolucencies–
1. Periapical granuloma2. Peripaical cemento – osseous dysplasia (early lesions)
Nasopalatine Duct (Incisive Canal) Cyst
• Also classified as “FISSURAL CYSTS”.
• Believed to be derived from epithelial remnants included during closure of embryonic facial processes.
• Controversy – actual “closure” of embryonic processes does not occur. Grooves between processes is smoothed by proliferation of underlying mesenchyme.
• Usually occurs within the nasopalatine canal or in soft tissue of palate at the opening of canal.
PATHOGENESIS
• In lower animals, the NP duct concerned with olfactory sensation – in humans only vestigial remnants persist in incisive canal in form of epithelial islands, ducts, cords etc.
• These nests can show central degenration to form cysts. Etiology for cyst transformation is yet unclear.
• Some believe, it may arise spontaneously like an OKC.
CLINICAL FEATURES
• Age : 4th, 5th & 6th decades.
• Sex : More in females
• Frequency: Commonest non odontogenic developmental cyst
Signs & symptoms
• Commonest symptom is swelling, usually in anterior region of mid palate.
• Swelling can also occur in midline on labial aspect of alveolar ridge.
• If pressure on NP nerves – pain
• Exclude possibility of periapical cyst by testing vitality of incisors.
Nasopalatine Duct (Incisive Canal) Cyst
Small nasopalatine cyst presenting as a soft ovoidswelling in the midline of the maxilla, posterior to the central incisor teeth.
Large nasopalatine duct cyst extending laterally andposteriorly to involve much of the hard palate.
RADIOLOGICAL FEATURES
Radiograph of a nasopalatine duct cyst showing a pear-shaped radiolucency in the anterior maxilla. The lamina dura on the left is intact although the apex appears to be in the cyst.
RADIOLOGICAL FEATURES
Shows a large round radiolucency. The roots of the maxillary incisor teeth are displaced laterally.
RADIOLOGICAL FEATURES
• Seen as lucency usually in incisive canal – DIFFICULT TO DISTINGUISH FROM A NATURALLY LARGE INCISIVE CANAL.
• Lucency with AP dimension upto 10 mm considered as enlarged incisive canal, but if lucency < 14 mm, then NP duct cyst.
• The lucency appears well defined with sclerotic borders, in midline of palate between roots of incisors.
DIFFERENTIAL DIAGNOSIS
• Radicular cyst, if it is associated with a pulpally involved tooth.
• Large incisive canal.
NASOLABIAL CYST
• The nasolabial cyst occurs outside the bone in the nasolabial folds below the alae nasi.
• It is traditionally regarded as a jaw cyst although strictly speaking it should be classified as a soft tissue cyst.
Clinical features
• Age : Peak incidence in 4th & 5th decades.
• Sex : More in females.
• Frequency: Rare in occurrence.
Signs & symptoms
• Commonest complaint – slowly growing swelling and occasionally, pain and difficulty in nasal breathing.
• Extra orally – filling out of nasolabial fold and may lift ala of nose.
• Intra orally – bulge in labial sulcus.
• Fluctuant lesion.
Nasolabial cyst producing a swelling of the right upper lip, forming a bulge in the labial sulcus.
RADIOLOGICAL FEATURES
• Difficult to interpret on radiograph.
• May be seen as localized increased lucency of alveolar process above apices of incisors.
• Lucency results from pressure resorption on labial surface of maxilla. Standard occlusal radiograph of a patient with a nasolabial
cyst. There is a posterior convexity of the left half of the radiopaque line that forms the bony border of the nasal aperture.
Paradental Cysts
• A cyst of inflammatory origin- occurring on lateral aspect of root of partially erupted mandibular 3rd molar with an associated history of pericoronitis
• Age : 20-40 years
• Tooth is vital
• Facial swelling
• Facial sinus in some cases
Radiographic features
• Affected tooth is tilted Well demarcated Radiolucency Distal to partially erupted tooth
• Lamina Dura is intact
• New bone may be laid down
a
b
(a,b) Two cases of bilateral paradental cysts associated with erupting mandibular third molar teeth. The cysts are distal and buccal to the involved teeth. Note that the periodontal ligament space is not widened and that the distal part of the cyst is separate from the distinct distal follicular space.
Aneurysmal Bone Cyst
• Uncommon cyst, found mostly in long bones and spine.
• CLINICAL FEATURES: -
1. Age : First 3 decades.2. Sex : Mainly females.3. Site : molar regions of mandible & maxilla.
• Signs & symptoms: Hard, rapidly growing swelling which can cause
malocclusion. If lesion perforates cortical plates, can cause “egg
shell crackling”.
PATHOGENESIS
• Controversy whether lesion arises de novo or from a vascular disturbance in the form of sudden venous occlusion or development of an AV shunt occurring secondarily in a pre existing lesion like central giant cell granuloma, Osteosarcoma etc.
• Due to the malformation, change in hemodynamic forces occurs which can lead to ABC.
RADIOLOGICAL FEATURES
• Classically seen as a unilocular, ovoid / fusiform lucency which balloons the cortical plates.
• Teeth displacement and root resorption also observed.
• Lesions are usually unilocular but longer-standing lesions may show a ‘soap-bubble’ appearance and may become progressively calcified
Radiograph of an aneurysmal bone cyst involving the angle and ascending ramus of the mandible. There is a ballooning expansion of the cortex.
Solitary Bone Cyst
• Also called as Hemorrhagic bone cyst, or Traumatic bone cyst.
• Commonly seen in mandible, rare in maxilla.
• Identical to solitary bone cyst of humerus in children and adolescents.
CLINICAL FEATURES
• Age : Young individuals
• Sex : Equal
• Site : Body and symphysismenti of mandible.
PATHOGENESIS
• None of the theories are certain about exact cause.
• First theory – cyst may follow trauma to bone which causes intra medullary hemorrhage which fails to organize. This clot subsequently liquefies - CYST.
• Recent theory osteogenic cells fail to differentiate locally and thus instead of bone, the undifferentiated cells form synovial tissue.
Signs & symptoms
• Asymptomatic.
• Rarely, swelling and pain may be seen.
• Half of all patients give a history of trauma to the area.
RADIOLOGICAL FEATURES
• Appears as a lucency with irregular but well defined edges and slight cortication.
• On occlusal view the ‘lucency is seen to extend along cancellous bone.
Radiograph of a solitary bone cyst involving anextensive area in the right body of the mandible. Thisexample has a well-defined margin with cortication.Interradicular scalloping is a prominent feature.
Principles of Treatment
REASONS
• Cysts tend to increase in size.• Cysts tend to get infected.• Cysts weaken the jaw. ( pathological fracture)• Some cysts undergo changes. Eg: Ameloblastoma, Mucoepidermoid
carcinoma ( histological study to be done) • Cysts prevent eruption of teeth. (dentigerous cyst)• Involvement of neighboring structures.( maxillary sinus, nose,
adjacent tooth)
Various Aspirates
PATHOLOGY ASPIRATE Other Findings of Aspirates
Dentigerous Cyst Clear, pale straw colour fluid
Cholesterol crystals. Total protein in excess 4 g / 100ml. Resembles serum
Odontogenic Keratocyst Dirty, creamy white viscoid suspension
Para keratinized squames. Total protein less than 4 g /100ml. Mostly albumin
Periodontal Cyst Clear, pale yellow straw colour fluid
Cholesterol crystals. Total protein 5 — 11g / 100ml
Infected Cyst Pus, brownish fluid Polymorphonuclear leukocytes, ,Cholesterol clefts
Mucocele, Ranula Mucus -----
Gingival Cysts Clear fluid -----
Various Aspirates
PATHOLOGY ASPIRATE Other Findings of Aspirates
Solitary Bone Cyst Serous fluid, blood or empty cavity
Necrotic blood clot
Stafne’s Bone Cyst Empty cavity – yield air ---
Dermoid Cyst Thick sebaceous material ---
Fissural Cyst Mucoid fluid ----
treatment
Cysts of the jaws are treated in one of the following four basic methods:
(1) Enucleation, (2) Marsupialization, (3) A staged combination of the two procedures, and (4) Enucleation with curettage.
1. Enucleation
• Enucleation is the process by which the total removal of a cystic lesion is achieved.
• By definition, it means a shelling- out of the entire cystic lesion without rupture.
2. Marsupialization
• Marsupialization, decompression, and the Partsch operation all refer to creating a surgical window in the wall of the cyst, evacuating the contents of the cyst, and maintaining continuity between the cyst and the oral cavity, maxillary sinus, or nasal cavity.
• The only portion of the cyst that is removed is the piece removed to produce the window. The remaining cystic lining is left in situ.
• This process decreases intracystic pressure and promotes shrinkage of the cyst and bone fill. Marsupialization can be used as the sole therapy for a cyst or as a preliminary step in management, with enucleation deferred until later.
4. Enucleation with Curettage
• Enucleation with curettage means that after enucleation a curette or bur is used to remove 1 to 2 mm of bone around the entire periphery of the cystic cavity
• Any remaining epithelial cells that may be present in the periphery of the cystic wall or bony cavity must be removed.
• These cells could proliferate into a recurrence of the cyst.