CPR in Infant
-
Upload
surya-luph -
Category
Documents
-
view
222 -
download
0
Transcript of CPR in Infant
-
8/3/2019 CPR in Infant
1/21
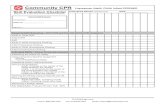
Definition
Cardiopulmonary resuscitation, commonly called CPR, combines rescue
breathing (one person breathing into another person) and chest compression in a
lifesaving procedure performed when a person has stopped breathing or a
person's heart has stopped beating.
Purpose
Ads by Google
When performed quickly enough, CPR can save lives in such emergencies as loss
of consciousness, heart attacks or heart "arrests," electric shock, drowning,
excessive bleeding, drug overdose, and other conditions in which there is no
breathing or no pulse. The purpose of CPR is to bring oxygen to the victim's lungs
and to keep blood circulating so oxygen gets to every part of the body. When a
person is deprived of oxygen, permanent brain damage can begin in as little as
four minutes and death can follow only minutes later.
Description
There are three physical symptoms that indicate a need for CPR to be performed
immediately and for emergency medical support to be called: unconsciousness,
not breathing, and no pulse detected.
1
http://www.google.com/url?ct=abg&q=https://www.google.com/adsense/support/bin/request.py%3Fcontact%3Dabg_afc%26url%3Dhttp://www.surgeryencyclopedia.com/A-Ce/Cardiopulmonary-Resuscitation.html%26hl%3Den%26client%3Dca-pub-5788426211617053%26adU%3Dmobil.tokobagus.com%26adT%3DCari%2BMobil%2BSecond%253F%26gl%3DID&usg=AFQjCNGaKrsO9mRIPFMpMB_GjhHedTcEaQhttp://www.google.com/url?ct=abg&q=https://www.google.com/adsense/support/bin/request.py%3Fcontact%3Dabg_afc%26url%3Dhttp://www.surgeryencyclopedia.com/A-Ce/Cardiopulmonary-Resuscitation.html%26hl%3Den%26client%3Dca-pub-5788426211617053%26adU%3Dmobil.tokobagus.com%26adT%3DCari%2BMobil%2BSecond%253F%26gl%3DID&usg=AFQjCNGaKrsO9mRIPFMpMB_GjhHedTcEaQ -
8/3/2019 CPR in Infant
2/21
CPR in basic life support. Figure A: The victim should be flat on his
back and his mouth should be checked for debris. Figure B: If the
victim is unconscious, open airway, lift neck, and tilt head back.
Figure C: If victim is not breathing, begin artificial breathing with
four quick full breaths. Figure D: Check for carotid pulse. Figure E: If
pulse is absent, begin artificial circulation by depressing sternum.
Figure F: Mouth-to-mouth resuscitation of an infant. (
Illustration by Electronic Illustrators Group.
)
Unconsciousness
Unconsciousness is when the victim seems to be asleep but has lost all awareness
and is not able to respond to questions or to touch or gentle shaking. A sleeping
person will usually respond to a loud noise, shouting, or gentle shaking. An
unconscious person will not respond to noise or shaking. When unconscious, a
2
-
8/3/2019 CPR in Infant
3/21
person can not cough or clear the throat, which can block the windpipe and cause
suffocation and death. People with a major illness or injury or who have had
recent surgery are at risk for losing consciousness. If the person has fainted,
which is brief unconsciousness, the cause may be dehydration (lack of body
fluids), low blood pressure, or low blood sugar. This is a temporary condition. If
the victim is known to have diabetes, a bit of fruit juice may revive the person
once they have regained consciousness.
Just before a person loses consciousness, symptoms may include:
lack of response to voice or touch
disorientation or stupor
light-headedness
headache
sleepiness
Not breathing
Not breathing, which is also called apnea, is the lack of spontaneous breathing. It
requires immediate medical attention. The victim may become limp and lifeless,
have a seizure, or turn blue. Prolonged apnea is called respiratory arrest. Inchildren, this can lead quickly to cardiac arrest in which the heart stops beating.
In adults, cardiac arrest usually happens first and then respiratory arrest. The
common causes of apnea in adults are obstructive sleep apnea (something blocks
the airway during sleep), choking, drug overdose, near-drowning, head injury,
heart irregularities (arrhythmia, fibrillation) or cardiac arrest, nervous system
disorders, or metabolic disorders. In children the causes may be different, such as
prematurity, bronchial disturbances or pneumonia, airway blockage or choking
on a foreign object, holding the breath, seizures, meningitis, regurgitating food,or asthma attacks.
No pulse detected
3
-
8/3/2019 CPR in Infant
4/21
If the rescuer is unable to detect a pulse or has difficulty in feeling a pulse it can
be an indication of the use of improper technique by the rescuer, or shock or
cardiac arrest in the victim. If a sudden, severe decrease occurs in pulse quality
(such as pulse weakness) or pulse rate (how many beats in a minute) when other
symptoms are also present, life-threatening shock is suspected. The rescuer may
need to explain to a doctor or medical professional where on the victim's body the
pulse was measured, if the pulse is weak or absent altogether, and what other
symptoms are present.
Medical help and CPR are needed immediately if any of these symptoms is found.
Time is critical. A local emergency number should be called immediately. If more
than one person is available to help, one can call 911 or a local emergency medical
service, while the other person begins CPR. Ideally, someone CPR certified
performs the procedure. Local medical personnel, a hospital, or the American
Heart Association teaches special accredited CPR courses. If a critically ill patient
or post-operative patient is being cared for at home, it is a good idea for a family
member to take a CPR course to be better prepared to help in case of an
emergency.
The steps usually followed in CPR are as follows:
If the victim appears to be unconscious with either no breathing or no
pulse, the person should be shaken or tapped gently to check for any
movement. The victim is spoken to loudly, asking if he or she is OK. If
there is no response, emergency help must be called and CPR begun
immediately.
The victim is placed on his or her back on a level surface such as the
ground or the floor. The victim's back should be in a straight line with the
head and neck supported slightly by a rolled up cloth, small towel, or piece
of clothing under the neck. A pillow should not be used to support the
head. The victim's clothing should be loosened to expose the chest.
The rescuer kneels next to the victim, tilts the victim's head back, lifts the
jaw forward, and moves the tongue forward or to the side, making sure it
4
-
8/3/2019 CPR in Infant
5/21
does not block the opening to the windpipe. The victim's mouth must be
kept open at all times, reopening as necessary.
The rescuer listens close to the victim's mouth for any sign of breathing,
and watches the chest for movement. If the victim is found to be breathing,
and has perhaps fainted, he or she can be placed in the recovery position
until medical assistance arrives. This is done by straightening the victim's
legs and pulling the closest arm out away from the body with the elbow at
a right angle or 3 o'clock position, and the other arm across the chest. The
far leg should be pulled up over the victim's body with the hip and knee
bent. This allows the victim's body to be rolled onto its side. The head
should be tilted back slightly to keep the windpipe open. The head should
not be propped up. If the victim is not breathing, rescue breathing begins, closing the victim's
nostrils between a thumb and index finger, and covering the victim's
mouth with the rescuer's mouth. Two slow breaths, about two seconds
each, are breathed into the victim's mouth with a pause in between. This is
repeated until the chest begins to rise. The victim's head should be
repositioned as often as necessary during the procedure. The mouth must
remain open and the tongue kept away from the windpipe.
When the chest begins to rise, or the victim begins to breathe on his or herown, the rescuer looks for signs of circulation, such as coughing or
movement. If a healthcare professional has arrived by this time, the pulse
will be checked before resuming resuscitation.
If chest compressions are needed to restart breathing, the rescuer will
place the heel of a hand above the lowest part of the victim's ribcage where
it meets the middle-abdomen. The other hand will be placed over the heel
of the first hand, with fingers interlocked. Keeping the elbows straight, the
rescuer will lean his or her shoulders over the hands and press downfirmly about 15 times. It is best to develop an up-and-down rhythm,
keeping the hands firmly on the victim's chest.
After the compressions, the rescuer will give the victim two long breaths.
The sequence of 15 compressions and two breaths will be repeated until
5
-
8/3/2019 CPR in Infant
6/21
there are signs of spontaneous breathing and circulation or until
professional medical help arrives.
Precautions
There are certain important precautions for rescuers to remember in order to
protect the victim and get the best result from CPR. These include:
Do not leave the victim alone.
Do not give chest compressions if the victim has a pulse. Chest
compression when there is normal circulation could cause the heart to
stop beating.
Do not give the victim anything to eat or drink. Avoid moving the victim's head or neck if spinal injury is a possibility. The
person should be left as found if breathing freely. To check for breathing
when spinal injury is suspected, the rescuer should only listen for breath
by the victim's mouth and watch the chest for movement.
Do not slap the victim's face, or throw water on the face, to try and revive
the person.
Do not place a pillow under the victim's head.
The description above is not a substitute for CPR training and is not intended to
be followed as a procedure.
Normal results
Successful CPR will restore breathing and circulation in the victim. Medical
attention is required immediately even if successful CPR has been performed and
the victim is breathing freely.
Prevention
6
-
8/3/2019 CPR in Infant
7/21
Loss of consciousness is an emergency that is potentially life threatening. To
avoid loss of consciousness and protect themselves from emergency situations,
people at risk can follow these general guidelines:
People with known conditions or diseases, such as diabetes or epilepsy,
should wear a medical alert tag or bracelet.
People with diabetes should avoid situations that will lower their blood
sugar level.
People who feel weak, become dizzy or light-headed, or have ever fainted,
should avoid standing in one place too long without moving.
People who feel faint, can lie down or sit with their head lowered between
their knees.
Risk factors that contribute to heart disease should be reduced or
eliminated. People can reduce risks if they stop smoking, lower blood
pressure and cholesterol, lose weight, and reduce stress.
Illegal recreational drugs should be avoided.
Seeing a doctor regularly and being aware of any disease conditions or risk
factors can help prevent or complicate illness, as can seeking and following
the doctor's advice about diet and exercise.
Using seat belts and driving carefully can help avoid accidental injury.
People with poor eyesight or those who have difficulty walking because of
disability, injury, or recovery from illness, can use a cane or other
assistance device to help them avoid falls and injury.
Resources
ORGANIZATIONS
American CPR Training.http://www.cpr-training-classes.com .
American Heart Association, National Center. 7272 Greenville Avenue, Dallas,
TX 75231. http://www.americanheart.org .
OTHER
7
http://www.cpr-training-classes.com/http://www.cpr-training-classes.com/http://www.americanheart.org/http://www.cpr-training-classes.com/http://www.americanheart.org/ -
8/3/2019 CPR in Infant
8/21
Emergency Cardiovascular Care. [cited April 2003]. http://www.cpr-ecc.org .
Check the Scene
- make sure it is safe for you to help.Don't become another victim.
Check the Victim
- tap and shout to get response.
Call for Help
- If no response, tell someone to call 9-1-1.If you are alone, perform 5 cycles of CPR First, then call 9-1-1.Call 9-1-1 for any unconscious victim, including an infant that isbreathing.
Circulation
- pump the chest 30 times.
Place two fingertips of one hand in the center of the chest.Press chest down about 1 1/2 inches at a rate of 100 per minute (16in 10 seconds).
Airway
- tilt head back, lift chin up to open airway.
Breathing
- Take a normal breath, cover victim's mouth and nose with yourmouth, and give a breath until the chest rises.
Give a second breath. Take about 1 second per breath.If chest doesn't rise, open airway again.
Repeat C - A - B
until help arrives or the victim begins breathing.If there are two rescuers, one does the breathing and one does the
8
http://www.cpr-ecc.org/http://www.cpr-ecc.org/ -
8/3/2019 CPR in Infant
9/21
compressions - CPR steps and ratios remain the same.
Remember to save an infant's life at any time!
CPR - infant
CPR is a lifesaving procedure that is performed when an infant's breathing or heartbeat hasstopped, as in cases of drowning, suffocation, choking, or injuries. CPR is a combination of:
Rescue breathing, which provides oxygen to the infant's lungs.
Chest compressions, which keep the infant's blood circulating.
Permanent brain damage or death can occur within minutes if an infant's blood flow stops.
Therefore, you must continue these procedures until the infant's heartbeat and breathing return,
or trained medical help arrives.
Considerations
CPR can be lifesaving, but it is best performed by those who have been trained in an accredited
CPR course. The procedures described here are not a substitute for CPR training.
All parents and those who take care of children should learn infant and childCPR if they haven't
already. This jewel of knowledge is something no parent should be without.
(See www.americanheart.org for classes near you.)
Time is very important when dealing with an unconscious infant who is not breathing. Permanent
brain damage begins after only 4 minutes without oxygen, and death can occur as soon as 4 - 6
minutes later.
Causes
In infants, major reasons that heartbeat and breathing stop include:
Choking
Drowning
9
http://www.americanheart.org/http://www.nlm.nih.gov/medlineplus/ency/article/000022.htmhttp://www.addthis.com/bookmark.php?v=250&username=medlineplus&ui_508_compliant=true&ui_language=enhttp://www.nlm.nih.gov/cgi/medlineplus/email_request.pl?refPage=http://www.nlm.nih.gov/medlineplus/ency/article/000011.htm&emailTitle=CPR+-+infanthttp://www.americanheart.org/http://www.nlm.nih.gov/medlineplus/ency/article/000022.htm -
8/3/2019 CPR in Infant
10/21
Electrical shock
Excessive bleeding
Head trauma or serious injury
Lung disease
Poisoning
Suffocation
Symptoms
No breathing
No pulse
Unconsciousness
First Aid
The following steps are based on instructions from the American Heart Association.
1. Check for responsiveness. Shake or tap the infant gently. See if the infant moves or
makes a noise. Shout, "Are you OK?"
2. If there is no response, shout for help. Send someone to call 911. Do not leave the
infant yourself to call 911 until you have performed CPR for about 2 minutes.
3. Carefully place the infant on their back. If there is a chance the infant has a spinal
injury, two people should move the infant to prevent the head and neck from twisting.
4. Open the airway. Lift up the chin with one hand. At the same time, tilt the head by
pushing down on the forehead with the other hand.
5. Look, listen, and feel for breathing. Place your ear close to the infant's mouth and
nose. Watch for chest movement. Feel for breath on your cheek.
6. If the infant is not breathing:
o Cover the infant's mouth and nose tightly with your mouth.
o Alternatively, cover just the nose. Hold the mouth shut.
o Keep the chin lifted and head tilted.
o Give 2 rescue breaths. Each breath should take about a second and make the
chest rise.
7. Perform chest compressions:
o Place 2 fingers on the breastbone -- just below the nipples. Make sure not to
press at the very end of the breastbone.
o Keep your other hand on the infant's forehead, keeping the head tilted back.
o Press down on the infant's chest so that it compresses about 1/3 to 1/2 the depth
of the chest.
o Give 30 chest compressions. Each time, let the chest rise completely. These
compressions should be FAST and hard with no pausing. Count the 30
compressions quickly:
"1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,
30, off."
10
http://www.nlm.nih.gov/medlineplus/ency/article/003069.htmhttp://www.nlm.nih.gov/medlineplus/ency/article/000022.htmhttp://www.nlm.nih.gov/medlineplus/ency/article/003069.htmhttp://www.nlm.nih.gov/medlineplus/ency/article/000022.htm -
8/3/2019 CPR in Infant
11/21
8. Give the infant 2 more breaths. The chest should rise.
9. Continue CPR (30 chest compressions followed by 2 breaths, then repeat) for about 2
minutes.
10. After about 2 minutes of CPR, if the infant still does not have normal breathing, coughing,
or any movement, leave the infant if you are alone and call 911.
11. Repeat rescue breathing and chest compressions until the infant recovers or help arrives.
If the infant starts breathing again, place him or her in the recovery position. Periodically re-check
for breathing until help arrives.
DO NOT
Lift the infant's chin while tilting the head back to move the tongue away from the
windpipe. If a spinal injury is suspected, pull the jaw forward without moving the head or
neck. Don't let the mouth close.
If the infant has signs of normal breathing, coughing, or movement, DO NOT begin chestcompressions. Doing so may cause the heart to stop beating.
Unless you are a health professional, DO NOT check for a pulse. Only a health care
professional is properly trained to check for a pulse.
When to Contact a Medical Professional
If you have help, tell one person to call 911 while another person begins CPR.
If you are alone, shout loudly for help and begin CPR. After doing CPR for about 2
minutes, if no help has arrived, call 911. You may carry the infant with you to the nearest
phone (unless you suspect spinal injury).
Prevention
Unlike adults, who often require CPR because of a heart attack, most children need CPR
because of a preventable accident.
Never underestimate what an infant can do. Play it safe and assume the child is more mobile and
more dexterous than you thought possible. Never leave an infant unattended on a bed, table, or
other surface from which the infant could roll. Always use safety straps on high chairs and
strollers. Never leave an infant in a mesh playpen with one side down. Follow the guidelines for
using infant car seats.
Start teaching your infant the meaning of "Don't touch." The earliest safety lesson is "No!"
Choose age-appropriate toys. Do not give infants toys that are heavy or fragile. Inspect toys for
small or loose parts, sharp edges, points, loose batteries, and other hazards.
11
http://www.nlm.nih.gov/medlineplus/ency/article/000029.htmhttp://www.nlm.nih.gov/medlineplus/ency/article/000029.htm -
8/3/2019 CPR in Infant
12/21
Create a safe environment and supervise children carefully, particularly around water and near
furniture. Keep toxic chemicals and cleaning solutions safely stored in childproof cabinets.
Dangers such as electrical outlets, stove tops, and medicine cabinets are attractive to infants and
small children.
To reduce the risk ofchoking accidents, make sure infants and small children cannot reachbuttons, watch batteries, popcorn, coins, grapes, or nuts. It is also important to sit with an infant
while he or she eats. Do not allow an infant to crawl around while eating or drinking from a bottle.
Never tie pacifiers, jewelry, chains, bracelets, or anything else around an infant's neck or wrists.
Alternative Names
Rescue breathing and chest compressions - infant; Resuscitation - cardiopulmonary - infant;
Cardiopulmonary resuscitation - infant
References
Emergency Cardiovascular Care Committee, Subcommittees, and Task Forces of the American
Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary
Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 Suppl):IV1-203.
Hauda WE II. Pediatric cardiopulmonary resuscitation. In: Tintinalli JE, Kelen GD, Stapczynski
JS, Ma OJ, Cline DM, eds. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New
York, NY: McGraw-Hill; 2004:chap 14.
12
http://www.nlm.nih.gov/medlineplus/ency/article/000047.htmhttp://www.nlm.nih.gov/medlineplus/ency/article/000047.htm -
8/3/2019 CPR in Infant
13/21
1. Shout and Tap
Shout and gently tap the child on the shoulder. Ifthere is no response and not breathing or notbreathing normally, position the infant on his or herback and begin CPR.
2. Give 30 Compressions
Give 30 gentle chest compressions at the rate of atleast 100 per minute. Use two or three fingers in thecenter of the chest just below the nipples. Pressdown approximately one-third the depth of thechest (about 1 and a half inches).
3. Open The Airway
Open the airway using a head tilt lifting of chin. Donot tilt the head too far back
4. Give 2 Gentle Breaths
If the baby is not breathing or not breathingnormally, cover the baby's mouth and nose withyour mouth and give 2 gentle breaths. Each breath
should be 1 second long. You should see the baby'schest rise with each breath.
CONTINUE WITH 30 PUMPS AND 2 BREATHS UNTIL HELPARRIVES
13
-
8/3/2019 CPR in Infant
14/21
CPR - infant - series
Check for breathing
1. Check for responsiveness. Shake or tap the infant gently. See if the infant moves or makes a
noise. Shout, Are you OK?
2. If there is no response, shout for help. Send someone to call 911. Do not leave the infant
yourself to call 911 until you have performed CPR for about 2 minutes.
3. Carefully place the infant on their back. If there is a chance the infant has a spinal injury,
two people should move the infant to prevent the head and neck from twisting.
4. Open the airway. Lift up the chin with one hand. At the same time, push down on the forehead
with the other hand.
5. Look, listen, and feel for breathing. Place your ear close to the infants mouth and nose.
Watch for chest movement. Feel for breath on your cheek.
Infant not breathing
14
-
8/3/2019 CPR in Infant
15/21
6. If the infant is not breathing:
Cover the infants mouth and nose tightly with your mouth.
Alternatively, cover just the nose. Hold the mouth shut.
Keep the chin lifted and head tilted.
Give 2 breaths. Each breath should take about a second and make the chest
rise.
Chest compressions
7. Perform chest compressions:
15
-
8/3/2019 CPR in Infant
16/21
Place 2 fingers on the breastbone -- just below the nipples. Make sure not to
press at the very end of the breastbone.
Keep your other hand on the infants forehead, keeping the head tilted back.
Press down on the infants chest so that it compresses about 1/3 to 1/2 the depth
of the chest.
Give 30 chest compressions. Each time, let the chest rise completely. Thesecompressions should be FAST and hard with no pausing. Count the 30 compressions
quickly:
1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30, off.
8. Give the infant 2 more breaths. The chest should rise.
9. Continue CPR (30 chest compressions followed by 2 breaths, then repeat) for about 2 minutes.
10. After about 2 minutes of CPR, if the infant still does not have normal breathing, coughing, or
any movement, leave the infant to call 911.
11. Repeat step 9 until the infant recovers or help arrives.
If the infant starts breathing again, place them in the recovery position. Periodically re-check for
breathing until help arrives.
16
-
8/3/2019 CPR in Infant
17/21
Can you save a life? In an emergency, when every second is criticial, would you kno
what to do?
According to recent statistics sudden cardiac arrest is rapidly becoming the leading cause of death
in America. Once the heart ceases to function, a healthy human brain may survive without oxygen
for up to 4 minutes without suffering any permanent damage. Unfortunately, a typical EMS
response may take 6, 8 or even 10 minutes.
CPR TIME LINE
0-4 mins. brain damage unlikely
4-6 mins. brain damage possible
6-10 mins. brain damage probable
over 10 mins. probable brain death
It is during those critical minutes that CPR (Cardio Pulmonary Resuscitation) can prov
oxygenated blood to the victim's brain and the heart, dramatically increasing his chance of survivAnd if properly instructed, almost anyone can learn and perform CPR.
Let's begin with CPR Basics
HOW CPR WORKS
The air we breathe in travels to our lungs where oxygen is picked
up by our blood and then pumped by the heart to our tissue andorgans. When a person experiences cardiac arrest - whether due to
heart failure in adults and the elderly or an injury such as neardrowning, electrocution or severe trauma in a child - the heart goes
from a normal beat to an arrhythmic pattern called ventricularfibrillation, and eventually ceases to beat altogether.
This prevents oxygen from circulating throughout the body, rapidlykilling cells and tissue. In
essence, Cardio (heart) Pulmonary (lung)Resuscitation (revive,revitalize) serves as an artificial heartbeat and an artificial
respirator.
CPR may not save the victim even when performed properly, but if
started within 4 minutes of cardiac arrest and defibrillation is
provided within 10 minutes, a person has a 40% chance of survival. The circulatory system
Invented in 1960, CPR is a simple but effective procedure that allows almost anyone to suminutes of cardiac arrest. CPR provides oxygenated blood to the brain and the heart long enou
until emergency equipment arrives.
To make learning CPR easier, a system was devised that makes remembering it as simple as A-
17
http://www.firstaidweb.com/how_cpr_works.htmlhttp://www.firstaidweb.com/how_cpr_works.html -
8/3/2019 CPR in Infant
18/21
A irway
B reathing
C irculation
Let's begin by emphasizing the very first step ofBasic Life Support
WHEN TO DIAL 9-1-1
It is critical to remember that dialing 9-1-1 may be the mostimportant step you can take to save a life.
If someone besides you is present, they should dial 9-1-1immediately. If youre alone with the victim, try to call for
help prior to starting CPR on an adult and after a minute ona child. Before we learn what to do in an emergency, we must
first emphasize what NOT to do:
DO NOT leave the victim alone.
DO NOT try make the victim drink water.
DO NOT throw water on the victim's face.
DO NOT prompt the victim into a sitting position.
DO NOT try to revive the victim by slapping his face.
Provide 9-1-1 operator with:Location & phone numberType of emergencyVictim's condition and age
Always remember to exercise solid common sense. When faced with an emergencysituation we may act impulsively and place ourselves in harm's way. Although time should not
be wasted, only approach the victim after determining that the scene is safe: always check for
cars, fire, gas, downed electrical lines, and any other potential hazards before attempting toperform CPR
CPR FOR INFANTS
According to generally accepted guidelines, Infant CPR is administered to any victim under the
age of 12 months.
Infants, just as children, have a much better chance of survival if CPR is performed
immediately. If you are alone with the infant, do not dial 9-1-1 until after you have made an
attempt to resuscitate the victim.
Check the infant for responsiveness by patting his feet and gently tapping his chest orshoulders. If he does not react (stirring, crying, etc.), immediately check his airway
AIRWAY
18
http://www.firstaidweb.com/dial911.htmlhttp://www.firstaidweb.com/adult.htmlhttp://www.firstaidweb.com/infant1.htmlhttp://www.firstaidweb.com/dial911.htmlhttp://www.firstaidweb.com/adult.htmlhttp://www.firstaidweb.com/infant1.html -
8/3/2019 CPR in Infant
19/21
"A" is for AIRWAY. It is normal for an infant to take shallow
and rapid breaths, so carefully look, listen and feel forbreathing. If you cannot detect any signs of breathing, the
tongue may be obstructing the infant's airway.
Although the head tilt/chin lift technique is similar to adults
and children, when clearing an infant's airway it's important
not to tilt the head too far back. An infant's airway isextremely narrow and overextending the neck may actually
close off the air passage.1. "Sniffer's position"
Tilt the head back into what is called the "sniffer's position" - far enough to make the infantlook as if he is sniffing (Figure 1).
If the victim is still not breathing on his own, you will have to assist him breathing
BREATHING
"B" is for BREATHING. Cover the infant's mouth and nose with your mouth creating a seal,and give a quick, gentle puff from your cheeks.
Let the victim exhale on his own - watch his chest and listen and feel for breathing. If he doesnot breathe on his own, again place your mouth over his mouth and nose and give another
small puff (Figure 1).
If the infant remains unresponsive (no crying or moving), immediately check his circulation
1. Puff from the cheeks
CIRCULATION
"C" is for CIRCULATION. An infant's pulse is checked at thebrachial artery, which is located inside of the upper arm,
19
http://www.firstaidweb.com/infant2.htmlhttp://www.firstaidweb.com/infant3.htmlhttp://www.firstaidweb.com/infant2.htmlhttp://www.firstaidweb.com/infant3.html -
8/3/2019 CPR in Infant
20/21
between the elbow and the shoulder (Figure 1).
Place two fingers on the brachial artery applying slightpressure for 3 to 5 seconds. If you do not feel a pulse withinthat time, then the infant's heart is not beating, and you will
need to perform chest compressions
1. Brachial ar
INFANT CPR REVIEW
What to remember when giving an infant CPR:
1. Check for responsiveness by patting the infant's
shoulders or chest.
2. Remember your A-B-C:
A irway: an infant's head should be tilted intothe "sniffer position". Do not overextend an
infants neck as this may close off the airway.
B reathing: cover the infant's nose and mouthwith your mouth and use gentle puffs,
breathing from your cheeks, not your lungs.
C irculation: check for pulse at the brachialartery, in the infant's inside upper arm. If
there is none, perform five compressions - 2fingers (approximately the size of a hand),
inch.
3. Perform rescue efforts for 1 to 2 minutes beforedialing 9-1-1.
4. Continue performing rescue efforts, checking for
pulse every minute until help arrives.
Congratulations! You've completed Pediatric Basic Life Support and should now take the
following quiz to reinforce what you've learned about Infant CPR before proceeding to the
final review/test.
Recovery position
20
http://www.firstaidweb.com/infant4.htmlhttp://www.firstaidweb.com/infant4.html -
8/3/2019 CPR in Infant
21/21
1. Position the infant face-down along your forearm.
2. Support the head and neck with your other hand while keeping the mouth andnose clear.
3. Keep the head and neck slightly lower than the chest.
Baby
A baby is considered to be less than 1 year old for the purposes of these instructions. For a baby less than a
year old, a modified recovery position must be adopted. Cradle the infant in your arms, with his head tilted
downwards to prevent him from choking on his tongue or inhaling vomit. Monitor and record vital signs -
level of response, pulse and breathing until medical help arrives.








![Effectiveness of self-directed cardiopulmonary ... · attempting CPR[2-5]. It was only for adult CPR previously, however, SDL kit for infant BLS was developed and translated into](https://static.fdocuments.net/doc/165x107/6006ad8dded6e13a35212bcd/effectiveness-of-self-directed-cardiopulmonary-attempting-cpr2-5-it-was-only.jpg)