CPR in Assisted Living: Not as Simple as it Seems
-
Upload
josh-allen -
Category
Documents
-
view
216 -
download
1
Transcript of CPR in Assisted Living: Not as Simple as it Seems

American Assisted Living Nurses AssociationOFFICIAL SECTION OF THE OFFICIAL SECTION OF THE
American Assisted Living Nurses Association
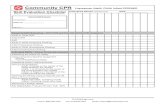
CPR in Assisted Living: Not asSimple as it Seems
Josh Allen, RNAmerican Assisted Living Nurses Association
Board Member
Nurses working in assisted living communitiesquickly learn that few things are as simpleas they seem in this surprisingly complex modelof care. Take cardiopulmonary resuscitation (CPR),for example; in acute care and skilled nursing fa-cilities, it is usually a simple matter of knowingthe “code” status of the resident. In assisted living,however, deciding whether to administer CPRcan require a nurse to wade through a quagmireof state regulations, staff competencies, policies,and conflicting wishes. Walking through thisdecision-making process reveals much aboutthe knowledge and skills needed for successfulassisted living nursing practice.
Resident Wishes
As in any setting, deciding whether to performCPR on a resident who is pulseless and is notbreathing starts with knowing the resident’swishes. A resident’s end-of-life care wishesshould be clearly communicated at the time ofmove in and updated whenever there are signifi-cant changes in condition. These wishes shouldbe documented using standardized, industry-recognized tools. In most cases, this will takethe form of an advance directive and/or do-not-resuscitate (DNR) order.
In far too many instances, a resident’s wishesare not clearly documented. This leads to confu-sion during an emergency when family membersor other responsible parties attempt to make dif-ficult decisions about life-sustaining treatmentthat they may not be legally authorized to make.
To combat the issues of miscommunication,several states now utilize the POLST (physicianorders for life-sustaining treatment) paradigmform to ensure clear and complete communica-tion of a resident’s wishes in the form of an ac-tionable medical order that is portable from onecare setting to another. More information about
470
the POLST and whether it is available in yourstate can be found at www.polst.org.
State Regulations and StaffCompetencies
Deciding if and when to administer CPR is ad-dressed to some extent in most state assisted liv-ing regulations, although the detail to which it isaddressed varies significantly from state to state.Some states, such as California, only require di-rect care staff to be trained in basic first aid, notrequiring CPR training at all. Other state assistedliving regulations, such as Arizona, require thatstaff be trained in administering CPR.
This can become even more challenging whenconsidering not only the act of administering CPRbut having the legal authority to “honor” a DNR.Some states may allow for assisted living directcare staff to administer CPR, but those same stateregulations may not allow them to honor a DNR,creating a question of whether it is advisable tohave unlicensed direct care staff administerCPR. In this situation, some assisted living pro-viders choose to simply train staff in first aid (as-suming state regulations allow them to limittraining to that level) and have a policy of calling911 for life-threatening emergencies, deferringthe issue of honoring the DNR to the respondingemergency medical services personnel. Fora nurse who has limited assisted living experi-ence, this practice can seem arcane, but a deeperunderstanding of the regulatory issues can revealthe necessity for the practice in some states.
Board of Nursing
Thefinal layer of complexitydthe state boardornursingdcan make things especially challenging,and even intimidating, for the nurse trying towork through these issues. The board of nursing,and, more specifically, the state nurse practiceact,may require a nurse to administer CPR to a res-ident who is a full code, is pulseless, and is notbreathing regardless of what the state assisted liv-ing regulations may require or allow. This leavesnurses feeling as though their licenses are in jeop-ardy by following the practices allowed in the state
Geriatric Nursing, Volume 31, Number 6

assisted living regulations. In somestates, the stateassisted living regulatory agency and the board ofnursing have worked together to rectify thesetypes of issues, but in far too many states, thistype of collaboration has not taken place.
Community Policies
Whatever the issues may be, every assisted liv-ing provider should have clear, written policiesand procedures addressing how CPR should behandled in the community. At a minimum, thesepolicies should address staff training, if andwhen to administer CPR, honoring DNRs andother end-of-life wishes, and nurses’ dutiesand responsibilities. Community policies mustbe in compliance with both the state assisted liv-ing regulations and the state board of nursing/nurse practice act requirements.
Lessons Learned
In analyzing the decision-making process re-lated to administering CPR, we have illustrated
Geriatric Nursing, Volume 31, Number 6
just one example of how complicated assisted liv-ing nursing practice can be. This same lesson canbe applied to many other clinical issues encoun-tered by nurses at the front line of assisted livingcare. By evaluating best practices, state assistedliving regulations, and board of nursing require-ments, the nurse and the assisted living providercan develop policies and procedures that ensurecompliance with regulatory requirements whilefocusing on meeting the residents needs andpreferences.
Resources
The National POLST Treatment Paradigm Initiative Task
Force. Frequently asked questions. Available at http://www.
ohsu.edu/polst/patients-families/faqs.htm. Cited September
23, 2010.
The National POLST Treatment Paradigm Initiative Task
Force. POLST State Programs. Available at http://www.ohsu.
edu/polst/programs/state+programs.htm. Cited September
23, 2010.
0197-4572/$ - see front matter
� 2010 Published by Mosby, Inc.
doi:10.1016/j.gerinurse.2010.10.008
471