Cpr aed and first aid 2005 aha guidelines dec 2010
-
Upload
patty-melody -
Category
Education
-
view
3.594 -
download
1
Transcript of Cpr aed and first aid 2005 aha guidelines dec 2010
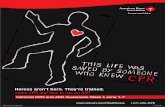
CPR/AED and First Aid Introduction: Recognizing and Dealing with Emergencies and Prevention Tips
Los Angeles Valley CollegePhysical Education DepartmentInstructor: Patty Melody, MAAmerican Red Cross guidelines based on the 2005 American Heart Association guidelines
What is CPR and the AED?
CPR stands for cardiopulmonary resuscitation and can be delivered to individuals who have had a heart attack or cardiac arrest and have stopped breathing and who have no heart rate. Beginning CPR is comprised of delivering 30 compressions followed by 2 rescue breaths continuously until paramedics arrive. The Automated External Defibrillator (AED) is a device we learn how to use in CPR classes as a means of analyzing the rhythm of the heart. Electrodes are placed on the chest to analyze the rhythm of the heart. If the AED detects either ventricular tachycardia or ventricular fibrillation (these are two possible shockable arrhythmias) the AED will deliver an electric shock to hopefully correct the arrhythmia and bring the heart back to normal sinus rhythm. This will enable the heart to correctly move blood thru the 4 chambers of the heart and then to the rest of the body delivering needed oxygen and nutrients to all cells to sustain life. With cardiovascular disease and strokes contributing to nearly half of all deaths each year in the United States the necessity for all of us to respond effectively to this major public health threat is critical.
Introduction to CPR/AED/First Aid
Good Samaritan Law / Negligence – your personal and legal safety first!
Top 10 killers in the U.S. – what to look for – awareness is key to responding effectively
Risk Factors for Cardiovascular Disease (CVD) and Prevention Efforts of CVD
Emergency Action Steps Primary versus Secondary Survey First Aid and Safety Tips
Good Samaritan Law and Guilty of Negligence: 3 conditions
It is important to protect yourself against legal liability when coming into contact with others whom you may be helping. The Good Samaritan Law should protect you from being sued for any damage or injury you may cause while giving care to the victim as long as you do what you were trained to do and are not negligent of any willful wrong doing.
Guilty of Negligence – 3 conditions1. Duty to Act (your job – nurse, paramedic, or parent)2. Not Acting or Acting Incorrectly3. Your Actions or Inactions caused Injury or Damages
U.S. Leading Causes of Death 2007
1. Heart Disease 616, 067 2. Cancer 562,876 3. Stroke 135,952 4. COPD 127,924 5. Unintentional injuries 123,706 6. Alzheimer’s Disease 74,632 7. Diabetes 71,382 8. Pneumonia/Influenza 52,717 9. Kidney Disease 46,448 10. Septicemia 34,828 11. Intentional self-harm (suicide) 34,598 12. Chronic Liver Disease and Cirrhosis 29,165 13. Essential Hypertension 23,965
and Hypertension Renal Disease (hypertension) 14. Parkinson’s Disease 19,544 15. Assault (homicide) 18,124
In 2007 there were 2,423,712 deaths in the U.S. Between 2006-7 there was a 2.1% decrease in deaths representing a record low historical figure. Life expectancy increased .2 years between 2006 (77.7 years) and 2007 (77.9 years). Deaths decreased for all age groups except 85+ age group remained unchanged.
Source: U.S Department of Health and Human Services. Centers for Disease Control and Prevention. National Center for Health Statistics. National Vital Statistics System, 2007.
48.6%
Top 10 Killers in U.S. 1997 – a look at the past
1. Heart Disease 31.4% 2. Cancer 23.2% 3. Stroke 6.9% 4. COPD 4.7% 5. Accidents 4.1% 6. Pneumonia/Influenza 3.7% 7. Diabetes 2.7% 8. Suicide 1.3% 9. Kidney Disease 1.1% 10. Chronic Liver Disease and Cirrhosis 1.1%
ACSM GUIDELINES 2005Coronary Artery Disease Risk Factors
Positive Risk Factors Family history Cigarette smoking Hypertension Dyslipidemia Impaired fasting glucose Obesity Sedentary lifestyleNegative Risk Factor High serum HDL cholesterol > 60mg/dL
(1.6mmol/L)
Benefits of Cardiorespiratory Endurance Exercise and Prevention of CVD
Improved cardiovascular functioning:
Reduces risk of CVD Glycogen-sparing effect Increases ventilatory capacity Increases cardiac output Reduces risk of dying prematurely Reduces risk of developing osteoporosis Maintenance of body weight Reduces risk of developing diabetes
CVD in Perspective
CVD – 953,110 deaths/year Cancer – 540,000 deaths/year Accidents – 96,000 deaths/year HIV/AIDS – 17,000 deaths/year
CVD cause of 41.2% of all deaths/year 1 out of every 2.4 deaths, 2,600 deaths/day,
1 death every 33 seconds CVD claims more lives each year than the
next seven leading causes of death combined
Types of CVD*
HypertensionCoronary heart diseaseStrokeRheumatic heart diseaseCongenital heart diseaseCongestive heart failure* CVD is the acronym for Cardiovascular Disease.
Atherosclerosis
Principle cause of coronary artery disease. Defined as the thickening, narrowing and hardening of the blood vessels in the body. The etiology of this chronic disease stems from long-term injury and plaque build-up within the inner lining (endothelial lining) of the arteries. This narrowing of the diameter of the vessels (lumen) leads to various forms of occlusion which can result in an MI (myocardial infarction). Coronary arteries are only as wide as a pencil lead.
Myocardial Infarction
Necrosis of a part of cardiac muscle caused by obstruction in a coronary artery through either atherosclerosis or a thrombus or a spasm. The onset of an MI is characterized by a crushing, viselike chest pain that may radiate to the left arm, neck, or epigastrium and sometimes stimulates the sensation of acute indigestion or a gallbladder attack.
The Cardiorespiratory System
Cardio: heart and blood vesselstransports oxygen, nutrients,
and wastes among vital organs and tissues
Respiratory: lungs, air passages, and
breathing musclessupplies oxygen and removes
carbon dioxide
Heart Attack Signals
Pale, clammy, SOB Faint, anxious, feeling
that death is imminent Tachycardia, thready
pulse, low BP Chest pain > 2 min. Radiating pain,
pressure, discomfort in arm, jaw and back
EKG might detect elevation of ST segment and Q wave
ALOC – altered level of consciousness measured using Glasgow Coma Scale
Nausea/Vomiting Gastrointestinal Distress Activate E.M.S. as soon as
possible. Forty percent of people die within the first hour of a heart attack.
Common Blood Vessel Disorders
Thrombus – clotEmbolus – moving clotHemorrhage – sudden burst of blood
vesselAneurysm – blood vessel balloons,
weakens and can rupture
Heart Attack Trivia
70% of heart attacks take place at home 30% of heart attacks outside of home Most heart attacks occur Monday mornings Men and post-menopausal women are at
highest risk Men deny they are having a heart attack Women are treated for gastric or gynecology
problems – treatment delayed because women present different s/s for heart attacks – Women’s Health Initiative 1991
The Cardiac Chain of Survival
The United States Chain of Survival has 4 links:
1. Early Recognition and access 911
2. Early CPR3. Early Defibrillation4. Early ACLS
The Canadian Chain of Survival has 7 links:
1. Healthy Habits – prevention of risk factors
2. Recognition of problem3. Early 9114. Early CPR5. Early Defibrillation6. Early ACLS7. Early Rehabilitation
Life-threatening Conditions
Unconsciousness Breathing problems or not breathing Heart problems/Heart attack/Sudden Cardiac
Arrest/No pulse Choking Severe bleeding These conditions can cause death within
minutes and brain death within 3-6 minutes if there is no oxygen delivered to the brain.
Why check the scene during an emergency?
For your safety. You do not want to become a possible victim also. If there is a fire, or you smell fumes, or electrical wires are down you may need to call 911 and stay clear for your safety.
Emergency Action Steps
Checkcheck the scene, then check victimCallhave someone call 911 and have them get
back to you – make eye contactCareABC’s – A=airway, B=breathing,
C=circulation
Primary / Secondary Survey
Primary Survey – ABC’s –
This is YOUR job when you are CPR certified
Secondary Survey – Head to Toe check
This is your job if you are First Aid certified or an EMT or paramedic or advanced medical personnel
How do you check if someone is unconscious?
Tap and shout “are you okay?”.Before calling 911 you want to establish
that the victim is not just someone laying on the floor taking a nap. If they do not respond to your touch or voice then assume they are unconscious and CALL 911.
After you check the scene and victim and call 911 then…Care (ABC’s)
During an emergency when you activate the Emergency Action Steps (check, call, care) to help the victim after you check the scene, then check the victim, then call 911 if you assess that this is an emergency then…
You begin your Primary Survey or your Care – your ABC’s of the airway (A=open airway – head tilt, chin lift, B=breathing – look, listen, feel for breathing for 5-10 seconds, deliver 2 breaths if the victim is not breathing, THEN IF THE CHEST RISES check circulation or pulse of the child or infant to decide which lifesaving protocol you will use (either Rescue Breathing, CPR, Conscious Choking, Unconscious Choking).
If the chest DOES NOT RISE – this is a possible unconscious choking victim – re-tilt the head – try again two more breaths – if the chest STILL DOES NOT RISE – this is an unconscious choking victim – DO NOT CHECK CIRCULATION (PULSE) – go directly to 30 compressions: look in month for obstruction: then give two breaths. Circulation is omitted with the unconscious choking (obstructed) victim. Also circulation is no longer taken on the adult. If the adult is not breathing, and the chest rises with your two breaths, go directly to CPR (30 compressions: 2 breaths).
What is the most important thing you can do in an emergency?
CALL 911 and local emergency. At LAVC our 24-hour sheriff’s phone number is 818-947-2911. After you have checked the scene for safety, and then checked
the victim, if you assess this situation is an emergency, call 911 right away or have someone else call 911 while you begin your Primary Survey or your ABC’s.
Delivering any needed breaths or compressions or direct pressure for severe bleeding or resolving an obstruction can save the life of the victim. Immediate action is needed during life-threatening emergencies. Average response time in L.A. County can be as high as 33 minutes. If the victim is not breathing or has no pulse this victim’s chance of survival is very low unless you intervene to “buy them time” until advanced personnel arrives and takes over.
Life-Saving Protocols We Learn in a CPR/AED Class
Rescue Breathing (victim is not breathing but they have a pulse – no longer performed on adult by the basic/lay rescuer – if the adult is not breathing we assume they do not have a pulse).
CPR/AED – victim is not breathing and does not have a pulse – breaths and compressions are given for the adult, child, infant at a 30:2 ratio of 30 compressions followed by 2 breaths – the American Heart Association in 2008 stated that Compression-Only-CPR is acceptable – particularly for rescuers who feel uncomfortable with giving mouth-to-mouth. If an AED (automated external defibrillator) is available – this can be used on the adult and child (not infants or children under 55 pounds – check with current guidelines as they change periodically – training available by your local American Heart Association or American Red Cross – training and certification is highly recommended to ensure better survival and care for the victim – certify the whole family!).
Conscious Obstruction (choking) – 5 back blows between shoulder blades followed by 5 abdominal thrusts (or chest thrusts if the victim is pregnant or too large for you to put your arms around). ASK FOR PERMISSION FIRST before giving care to a conscious victim or you may be sued for battery. If victim is unconscious consent is implied.
Unconscious Obstruction (choking) – Establish unconscious choking victim during Primary Survey (ABC’s) when initial 2 breaths and the second attempt of 2 breaths do not make the victim’s chest rise – then go right to 30 compressions, then look in the mouth for any food or object, do a finger sweep in a hook-like fashion IF you see something (blind sweep no longer given), then follow this with 2 breaths. Continue until object comes out or you see the victim’s chest rise – then re-assess victim with the ABC’s (Airway, Breathing, Circulation).
When giving breaths into the victim…
You are looking at filling the victim’s chest (not the abdomen – which may cause the victim to vomit). So, use your peripheral vision while you deliver breaths into the victim. Breath-in just enough to allow the victim’s chest to rise and then allow the chest to recoil before delivering the second breath.
Positioning Your Hands for Chest Compressions
Adult/Child – position one hand or two hands on the sternum (midline of the chest) on the nipple line. Lock your elbows with your shoulders directly over your elbows and hands as you compress the victim’s chest 1/3 to ½ the width towards the floor. Use your body weight to prevent excess fatigue. You may perform chest compressions for 5 to 10 minutes or longer depending on when the paramedics or another trained rescuer arrive and take over.
Infant – use 2 to 3 fingers on the sternum one finger-width below the nipple line – also compress 1/3 to ½ the width of the chest to ensure compression of the heart and sufficient blood circulation to allow circulation of oxygen and nutrients to the brain and heart and cells of the body.
Sufficient chest compressions and breaths are usually where critical care is not done appropriately. The survival of the victim necessitates that chest compressions are done DEEP ENOUGH and that the breaths ALLOW THE VICTIM’S CHEST TO RISE.
Rescue Breathing Ratios
Again, Rescue Breathing is a life-saving protocol performed on an individual who is not breathing BUT they have a pulse – so we are only breathing for the victim not performing chest compressions.
Adult – Rescue Breathing not performed as of the AHA 2005 Guideline changes – if the adult is not breathing and the chest rises with the 2 initial rescue breaths go directly to CPR/AED
Child/Infant – 1:3 (one breath every 3 seconds – breath, one-one-thousand, two-one-thousand, BREATH). Do not count to 3 – you need to breath on 3 – if you count to 3 then breath you are actually breathing every 4 seconds instead of every 3.
Practice, practice, practice! Be ready to save a life. When an emergency occurs that is probably not the best time to practice right?!
CPR Skills
Key point: supply what is missing
A – airway (head tilt, chin lift)
B – breathing (10cc/kg/min) 2 breaths
C – circulation – we no longer check pulse for the adult – if victim is not breathing start CPR unless AED is immediately available (30 compressions: 2 breaths) – for child check carotid pulse, infant check brachial pulse – either rescue breathing (1:5) or CPR (30:2)
D – defibrillation (“I’m clear, your clear, we’re all clear”) AED will shock for 2 rhythms 1. ven. Fib 2. pulseless ven. Tach.
Reasons to STOP CPR
When the scene becomes unsafeYou detect signs of circulationAn AED becomes availableYou are too exhausted to continueAnother trained person takes over CPREMS personnel arrive and take over
Conscious Obstruction (choking)
Try to encourage victim with a calm voice to cough object out themselves
If they are not effective and obviously need your help – ask permission first
Then stand in a lunge position behind victim and deliver 5 back blows between the victim’s shoulder blades while you hold the victim with your other hand
Then give 5 abdominal thrusts (Heimlich maneuver) or chest thrusts if the victim is pregnant.
How do you deal with severe bleeding?
Direct pressure on wound with a sterile gauze or towel (preferably). Do not remove saturated gauze or towel. Apply more gauze or towels.
Indirect pressure no longer taught with basic rescuers however if you have training and knowledge of local blood vessels near the wound site – adding pressure to these blood vessels can help stop bleeding excessively.
Tourniquets are also not taught in basic rescuer classes any longer. You would learn this technique as a paramedic or in a wilderness survival class perhaps.
Leading Cause of Death
Adults – heart disease/heart attackChildren – accidents – motor vehicle
accidents, drowning, suffocation, poisoning, falls
First Aid Outline1. Injury prevention and recognition (acute vs. chronic)
2. Statistics: Morbidity/Mortality
3. Primary prevention: CPR skills
4. Secondary prevention: Head to Toe survey
5. Work-related Injuries: Ergonomics
6. Soft tissue injuries: cuts, scrapes and bruises / Injuries to muscles, bones, and joints
7. Sudden illness / Poisoning
8. Heat or Cold Related Emergencies
9. Special Situations and Circumstances
10. Asthma / Anaphylaxis and Epinephrine Auto-Injectors
Injury Prevention: Acute
Intentional versus Unintentional InjuriesMajor Public Health Problem in U.S.Unintentional Injuries are the leading
cause of death for the population under 44 years old
Accidents are the 5th leading cause of death in this country
Vehicle Safety
16-24 years old highest death rate Inexperience and Immaturity In 2002, 38,309 died in auto crashes Each year 1.9 million are disabled (140,000
permanently) Prevention: Risk Management 1 car length for every 10mph, constantly scan around
you for new variables (drivers, road conditions, weather, signs), drive w/low beams, drive refreshed/sober, obey traffic laws, use seat belts, AAA accident-avoidance techniques, when buying a car look for safety technology, stay in car when in breaks down
Pedestrian Safety
13% of all motor vehicle deaths involve pedestrians 82,000 pedestrians injured each year Very young & elderly have the highest death rates High risk situations – after dark, urban setting,
intersections w/blind corners Alcohol not a variable Prevention – wear reflective material/clothing, cross
only at crosswalks, look both ways, watch for turning cars, walk facing traffic, don’t wear headphones
Cyclist safety
63 million Americans ride bikes 800 cyclists die each year Biggest risk factors – not wearing a helmet (ANSI approved),
riding after dark, children 10-14 years highest risk for injury, 87% of fatal collisions are due to cyclist error – failure to yield, alcohol plays a significant role in cyclists death/injuries
Prevention – wear a helmet (ANSI approved), 85% of head trauma due to not wearing a helmet, don’t drink & ride, respect traffic, don’t assume right of way, know and use proper hand signals, keep bicycle in proper working condition, ride w/the flow of traffic, use bike paths when you can, same laws apply to drivers and cyclist so share the road, stop at stop signs and red lights
Water safety
3rd most common cause of accidental death 85% of victims are teenage males Usually strong swimmers but they choose bad situations Risk factors – alcohol consumption, unorganized, unsupervised
conditions, swimming alone, diving into shallow, murky water Prevention – don’t drink alcohol and swim, you should be able to
swim at least 50 feet unassisted, know your limitations, never swim alone, don’t leave children/infants unattended in water (pools or bath tubs) even if it is shallow you can drown in 1” of water, most neck and back injuries result from diving into shallow water, careful when getting into a pool or other water source if it is raining so hard you can’t see the bottom of the pool, river currents. If you have a pool party hire a lifeguard.
Awareness of people who have conditions where they might lose consciousness (epileptics, diabetics, drug use)