Construct validation and comparison of a novel postoperative quality-of-life metric and the Short...
Click here to load reader
Transcript of Construct validation and comparison of a novel postoperative quality-of-life metric and the Short...

Accepte
ReprintHospitaEuclid Auhhospi
0039-60
� 2013
http://d
690 S
Construct validation and comparisonof a novel postoperative quality-of-lifemetric and the Short Form-36 incolorectal surgery patientsDeborah S. Keller, MD,a Michael F. McGee, MD,b Subir Goyal, MBBS, MPH,c Tamar Nobel, BS,d
Bridget O’Brien Ermlich, MSN,a Vinay K. Cheruvu, PhD,d and Conor P. Delaney, MD, MCh, PhD,a
Cleveland, OH, and Chicago, IL
Purpose. Several methods have been used to measure quality of life (QOL) in colorectal patients, butexisting QOL assessment tools are often complex, require complicated analysis, lack specificity forcolorectal surgery, and are not focused on assessment of perioperative care. The postoperative QOL(PQL) assessment is designed to capture subtle yet important QOL factors in an easy tool validated forthe postoperative period. Although internally validated, PQL lacks external validation with auniversally accepted QOL metric, such as the Rand Short Form-36 (SF-36). The purpose of this studywas to externally validate the PQL metric to the SF-36 for colorectal surgery.Methods. The PQL was designed using 14 questions ranked on a Likert scale (1–10) with surgeon andpatient input. After obtaining institutional review board approval, 100 consecutive colorectal surgerypatients at University Hospitals, Case Medical Center were administered baseline and postoperative(2, 4, 8, 12, 30, 60, and 90 days) PQL and SF-36 questionnaires prospectively. Patients undergoingcolorectal surgery via an abdominal approach (laparoscopic or open) for benign or malignant diseasewere included. Factor analysis and Spearman’s rank test were performed between each of the 8 SF-36scales and the 14 PQL questions and summary score. Convergent validity was demonstrated usingSpearman’s correlation coefficient at the domain and scale levels. The degree of agreement between PQLand SF-36 was assessed through Bland-Altman plots. Pairwise comparisons were made to determine anysignificant differences between the 2 scales.Results. Eighty-eight patients met all inclusion criteria and had a complete dataset, and were includedin the analysis. SF-36 factor analysis confirmed comparability between the study group and the generalpopulation. All PQL items correlated with all 8 mental and physical health domains in the SF-36(P < .0001). Bland-Altman plots demonstrated consistently similar measure for level of agreementbetween PQL and SF-36 as indicated by the 95% limits of agreement.Conclusion. The PQL and SF-36 demonstrated a strong and consistent level of agreement across all 8domains for pre- and postoperative scores in colorectal surgery patients. PQL is constructually valid inthe perioperative period. Based on our analysis, the novel PQL metric represents a simple, point-of-carealternative to SF-36 for rapid QOL assessment, and validates use of the PQL metric in abdominalsurgery. (Surgery 2013;154:690-6.)
From the Department of Surgery,a Division of Colorectal Surgery, University Hospitals- Case Medical Center,Cleveland, OH; the Department of Surgery,b Division of Surgical Oncology, Northwestern University FeinbergSchool of Medicine, Chicago, IL; the Department of Epidemiology and Biostatistics,c Kent State University;and the Case Western Reserve University School of Medicine,d Cleveland, OH
d for publication June 25, 2013.
requests: Conor P. Delaney, MD, MCh, PhD, Universityls- Case Medical Center, Lakeside 7th Floor, 11100venue, Cleveland, OH 44106. E-mail: [email protected].
60/$ - see front matter
Mosby, Inc. All rights reserved.
x.doi.org/10.1016/j.surg.2013.06.037
URGERY
QUALITY OF LIFE (QOL) is a broad-ranging conceptaffected in a complex way by an individual’sphysical health, psychologic state, level of indepen-dence, social relationships, and their relationshipsto salient features of the environment.1 MeasuringQOL has become a focus in healthcare with recentpressures to prioritize spending on medical inter-ventions used.2-4 QOL tools assess both the clinicaloutcome and the patient’s perception of theclinical outcome.5-8 Measures of QOL are used

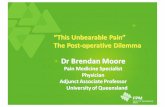
Name/Patient____________________________Date_________________
Quality of Life Questionnaire
The following questions are designed to gauge your current quality of life. Spot the answer that best indicates how you feel.
1. How would you rate your current, overall Quality of Life? Worst Best 0 1 2 3 4 5 6 7 8 9 10
2. How would you rate your current, overall Quality of Health? Worst Best 0 1 2 3 4 5 6 7 8 9 10
3. How would you rate your current, overall Level of Energy? Worst Best 0 1 2 3 4 5 6 7 8 9 10
4. What is your maximum level of pain while resting? No Pain Worst Pain 0 1 2 3 4 5 6 7 8 9 10
5. What is your maximum level of pain upon exertion? No Pain Worst Pain 0 1 2 3 4 5 6 7 8 9 10
6. Rate your severity of Nausea or Vomiting. No Nausea/Vomiting Severe Nausea/Vomiting 0 1 2 3 4 5 6 7 8 9 10
7. What is your current level of Fatigue? No Fatigue Extreme Fatigue 0 1 2 3 4 5 6 7 8 9 10
8. How would you rate your current bowel function? (0=abnormal; 10=100% normal)
Abnormal 100% Normal 0 1 2 3 4 5 6 7 8 9 10
9. Rate your ability to engage in your usual work activities. No Activity All Activity 0 1 2 3 4 5 6 7 8 9 10
10. Rate your ability to engage in your usual home activities, i.e.; cleaning, cooking, gardening, etc.
No Activity All Activity 0 1 2 3 4 5 6 7 8 9 10
11. Rate your ability to engage in your usual social activities, ie; sports, hobbies, going to dinner, etc.
No Activity All Activity 0 1 2 3 4 5 6 7 8 9 10
12. Rate your current level of sexual activity: (0=no sex; 10-100% normal)
No Sex 100% Normal 0 1 2 3 4 5 6 7 8 9 10
13. Rate your current level of happiness: (0=sad; 10=happy) Sad Happy 0 1 2 3 4 5 6 7 8 9 10
14. What is your satisfaction with your overall level of medical care? (0=dissatisfied; 10=100%satisfied) Dissatisfied 100% Satisfied 0 1 2 3 4 5 6 7 8 9 10
Fig 1. Postoperative quality of life questionnaire.
SurgeryVolume 154, Number 4
Keller et al 691
increasingly to evaluate outcomes of surgical care.As impairment in QOL is a main reason patientsseek surgical care, assessing the changes in QOLafter treatment is essential.9
Existing QOL assessment tools are often com-plex, require complicated analysis, lack specificityfor colorectal surgery, and are not focused onassessment of perioperative care. In addition,there exist no QOL questionnaires constructedand validated to measure postoperative QOL(PQL) in patients with colorectal disease in gen-eral (Fig 1).10 The PQL score was developed withsurgeon and patient input to meet this need.The PQL questionnaire uses 14 questions rankedon a Likert scale (1–10) assessing global QOL,nausea, pain (at rest and on maximal activity),bowel function, and return to normal health.PQL is specific to abdominal surgery patients andoffers improved sensitivity, enabling greater resolu-tion for comparisons between specific operativetechniques.11 Furthermore, the PQL tool was con-structed and tested on both open and laparoscopicpatients, and valid and reliable on both ap-proaches.11 We proved previously internal validityand internal consistency of PQL for a group of pa-tients undergoing abdominal surgery through a60-day postoperative period.11 Construct validationis a process used to show consistency of a new sur-vey instrument with a previously established ‘‘goldstandard’’ survey, thereby establishing the effective-ness of the new survey.12 The purpose of this studywas to externally validate the PQL metric to theShort Form-36 (SF-36) for colorectal surgery.
METHODS
After obtaining institutional review boardapproval and patient consent, 100 colorectal sur-gery patients were administered prospectively base-line and postoperative (2, 4, 8, 12, 30, 60, and 90days) PQL and SF-36 questionnaires. Patients wereincluded if between 18 and 85 years old, undergo-ing major colorectal surgery via an abdominalapproach (laparoscopic or open) for diagnoses ofinflammatory bowel disease, colorectal cancer,colorectal polyps, and diverticulitis, and completerecords of both PQL and SF-36 at baseline andeach postoperative time point were available.Patients requiring nonabdominal procedureswere excluded, as were patients undergoing mul-tiple (staged) procedures or status post recentabdominal surgery (<1 month postoperatively).
The internal consistency and reliability amongthe components of the PQL questionnaire wasdetermined at each time point using Cronbach’salpha. Factor analysis----a data-reduction technique
used to group items into factors using key under-lying attributes---was used to map the PQL ques-tions to cover all 8 SF-36 domains. The factoranalysis confirmed the validity of the study groupwith all SF-36 scales and confirmed comparabilitybetween the study group and the general popula-tion. Spearman’s rank and correlation coefficients(determined via the CORR algorithm) determinedthe strength of the relationship between each ofthe principle SF-36 scales (Physical Function, Role

Table I. Patient demographics and operative data
Data n (%)
SurgeryOpen 29 (33)Laparoscopic 59 (67)
IndicationInflammatory (diverticulitis/IBD) 32 (36)Cancer 24 (27)Polyp 21 (24)Other 11 (13)
ProcedureSegmental colectomy 53 (60)Low anterior/APR 15 (17)Total/proctocolectomy 11 (13)Small bowel resection/fistula repair 1 (1)Other 6 (7)Ostomy 2 (2)
APR, Abdominoperineal resection; IBD, inflammatory bowel disease.
SurgeryOctober 2013
692 Keller et al
Physical, Body Pain, General Health, Vitality, SocialFunctioning, Role Emotional, Mental Health) andeach PQL question item at baseline. Convergentvalidity was demonstrated with Spearman’s corre-lation coefficient at the domain and scale levels.Spearman’s rank test determined correlations be-tween each of the 8 SF-36 scales and the 14 PQLquestions and summary score. In addition, severalPQL questions relevant---on fatigue, nausea/vom-iting, and satisfaction with medical care---are notcovered by any SF-36 domain, showing the addedspecificity for this tool over the SF-36 in thepostoperative period.
The degree of agreement between PQL and SF-36 was assessed through Bland-Altman plot usingstandardized scores. Pairwise comparisons weremade to determine any significant differencesbetween the 2 scales. All statistical analyses wereperformed with SAS (The SAS Institute, Cary, NC).
RESULTS
One hundred patients were administered thePQL tool during the study period; 88 patients metinclusion criteria and were included in the anal-ysis. The procedures were 67% laparoscopic (n =59) and 33% open (n = 29). The majority of casesperformed were segmental colectomies (60%).The main indications for operation were inflam-matory bowel disease (36%), cancer (27% ), andpolyps (24%; Table I).
The Cronberg alpha test showed strong internalconsistency and reliability among the componentsof the PQL questionnaire at baseline and eachpostoperative time point (Fig 2). Most expertsrequire a reliability of $0.70 before they will usean instrument; all of our reliability measures werein the good to excellent range.
Factor analysis demonstrated SF-36 scores acrossall 8 mental and physical health domains corre-lated significantly with all PQL questions, confirm-ing the validity of the study group with the generalpopulation and study group with all SF-36 scales.On Spearman’s rank correlation test, each of the 8SF-36 core scales measured favorably with $1 PQLquestion item, demonstrating the strong positivecorrelation for all comparisons. The correlationcoefficients ranged from 0.53 to 0.78 for allassessments, and all measures of the correlationwere significant (P < .0001). Spearman’s correla-tion matrix mapped the 14 PQL question itemswith each SF-36 core domain, finding all SF-36 do-mains were covered by the PQL tool (Table II). Inaddition, several PQL questions items relevant toabdominal surgery on fatigue, nausea/vomiting,and satisfaction with medical care are not covered
by any SF-36 domain, showing the added specificityfor this tool over the SF-36 in the postoperativeperiod.
Bland-Altman analysis proved a strong degree ofagreement between the PQL and the SF-36 instru-ment. Our results demonstrated consistent, strongagreement between the PQL questions and each ofthe 8 principle SF-36 domains (Fig 3).
DISCUSSION
Assessing QOL is challenging endeavor, espe-cially in colorectal surgery patients. Several ques-tionnaires have been used to measure QOL incolorectal patients. The most commonly usedQOL questionnaire is the SF-36, a 36-item instru-ment that encompasses 8 dimensions of mentaland physical well-being.13 Unfortunately, the SF-36lacks specificity to surgery; common postoperativecomplaints such as pain, energy level, bowel anddietary habits, sexual function, and fatigue are un-derrepresented. The tool is also time consuming toadminister and can be difficult to interpret,because it requires advanced, nonparametric statis-tical analysis.14 Surgical-specific QOL scores havebeen developed as an attempt to address theseshortcomings. The Gastrointestinal Quality ofLife Index assesses bowel-related QOL. This toolalso contains 36 items and covers symptoms, aswell as physical, emotional, and social functioning,over a 2-week observation period.15 Other QOLtools have been designed to be more disease-spe-cific.16 The European Organization for Researchand Treatment of Cancer Quality of Life Question-naire (EORTC-QLQ-C30) is a self-reported patienttool that covers 5 functional scales (physical, role,

Fig 2. The Cronberg alpha test for PQL internal validity.
Table II. Spearman’s correlation coefficient matrix: PQL question item v SF-36 Core Scale
PQL
SF-36 scale
Physical Function Role Physical Body Pain General Health Vitality Social Functioning Role Emotional Mental Health
PQL#1 0.369 0.567 0.59 0.494 0.614 0.495 0.486 0.398PQL#2 0.357 0.592 0.573 0.559 0.63 0.464 0.419 0.35PQL#3 0.345 0.59 0.625 0.471 0.783 0.535 0.387 0.47PQL#4 0.312 0.357 0.579 0.305 0.432 0.502 0.207 0.356PQL#5 0.425 0.399 0.577 0.356 0.376 0.433 0.213 0.364PQL#6 0.338 0.309 0.42 0.252 0.275 0.467 0.208 0.216PQL#7 0.219 0.273 0.4 0.285 0.412 0.304 0.196 0.296PQL#8 0.314 0.497 0.498 0.269 0.544 0.511 0.393 0.369PQL#9 0.531 0.56 0.609 0.32 0.564 0.608 0.518 0.352PQL#10 0.662 0.659 0.667 0.401 0.579 0.663 0.534 0.416PQL#11 0.665 0.715 0.691 0.345 0.666 0.69 0.534 0.404PQL#12 0.629 0.51 0.418 0.103 0.383 0.473 0.368 0.18PQL#13 0.367 0.54 0.538 0.287 0.675 0.554 0.483 0.531PQL#14 0.336 0.406 0.301 0.275 0.246 0.303 0.297 0.327
SurgeryVolume 154, Number 4
Keller et al 693
emotional, social, and cognitive), 3 symptom scales(fatigue, nausea and vomiting, and pain), a globalhealth status/QOL scale, and 6 independent items(dyspnea, insomnia, appetite loss, constipation,diarrhea, and financial difficulties).17 TheEORTC-QLQ-C38 has an additional module specif-ically for colorectal cancer; this module was de-signed to cover symptoms and side effects relatedto different treatment modalities, body image,sexuality, and future perspective.18 These instru-ments are time consuming to administer andscore. Further, these metrics may be too general-ized and lack the ability to discriminate QOL dif-ferences between operative techniques andprocedures. A prime example of this risk is theQOL component of the Clinical Outcomes of Sur-gical Therapy study,19 where QOL was measured
with tools unspecific to surgery or colorectal sur-gery---the Symptoms Distress Scale20 and theQOL Index. With these tools, differences betweenlaparoscopic and open colectomy did not translateinto significant improvements in symptoms orQOL.19 If less general QOL instruments wereused, differences may have been detected earlier.
The 3-question Cleveland Global Quality of Lifehas been validated in patients with inflammatorybowel disease,21,22 but in not a wider range of colo-rectal diseases. Although this tool is not timeconsuming to administer, it is limited by its generalnature. The tool may also lack the ability to discernsubtle, but clinically important, effects of mini-mally invasive procedures from traditional openoperative techniques in a wide variety of colorectaldiseases. With these limitations, there was a

Fig 3. Bland-Altman plots: Degree of agreement between the Short Form-36 and the Postoperative quality of lifequestionnaire domains.
SurgeryOctober 2013
694 Keller et al
continued need for a simple, patient-centric QOLtool specific to colorectal disease.
A QOL score is necessary, because traditionalsurgical outcome measures, such as postoperativemorbidity, mortality, and long-term disease recur-rence, have centered on patient-specific experien-tial variables, such as convalescence, pain, andquality of gastrointestinal function. The PQLquestionnaire was intended to be a simple, point-of-care instrument applicable widely to a range ofabdominal operations allowing clinicians todiscriminate subtle, but important, QOL changesattributed to different operative approaches andtechniques. Criteria such as reproducibility, reli-ability, validity, ease of use, responsiveness, mean-ingfulness of results, and sampling of patient’s
perspective have been defined as important foroptimal measurement of health-related QOL.23
Before introducing the PQL survey as a newQOL instrument, validation was sought in a multi-step process. Previously, internal consistency wasshown over a large and broad patient popula-tion.11 Most experts require a reliability of $0.70before they will use an instrument; all of our reli-ability measures were in the good (0.80) to excel-lent (0.90) range. We concentrated on externalconstruct validation in the current study. ThePQL and SF-36 demonstrated a strong and consis-tent level of agreement across all 8 domains forpre- and postoperative scores in colorectal surgerypatients. On all question items, the PQL surveycorrelated favorably with each of the SF-36 core

SurgeryVolume 154, Number 4
Keller et al 695
scales, indicating adequate construct (external)validity. Furthermore, the PQL showed advantagesover the SF-36 for abdominal surgery patients. Inthe Spearman correlation coefficient matrix,several PQL questions items relevant to abdominalsurgery---questions on fatigue, nausea/vomiting,and satisfaction with medical care---were notcovered by any SF-36 domain. Thus, the additionalspecificity of the PQL has benefits over the existinggold standard for QOL in postoperative abdominalsurgery patients.
The reliability and validity of the PQL question-naire were highly consistent with the SF-36. ThePQL tool was constructed and tested on both openand laparoscopic patients, and has therefore beenproven valid and reliable on both approaches.With internal and external validity now demon-strated, the PQL can be used as QOL instrumentin postoperative abdominal surgical patients. Thissimple tool can be used as a measure of QOL andas a measure to assess return to normal functionafter abdominal surgery. Future studies will applythe validated PQL tool to compare differences inQOL across different patient populations, opera-tive procedures, and operative approaches.
REFERENCES
1. The World Health Organization Quality of Life Assessment(WHOQOL): development and general psychometric prop-erties. Soc Sci Med 1998;46:1569-85.
2. Hadorn DC, Brook RH. The health care resource allocationdebate. Defining our terms. JAMA 1991;266:3328-31.
3. Klevit HD, Bates AC, Castanares T, Kirk EP, Sipes-MetzlerPR, Wopat R. Prioritization of health care services. A prog-ress report by the Oregon Health Services Commission.Arch Intern Med 1991;151:912-6.
4. Mangione CM, Goldman L, Orav EJ, Marcantonio ER,Pedan A, Ludwig LE, et al. Health-related quality of life af-ter elective surgery: measurement of longitudinal changes.J Gen Intern Med 1997;12:686-97.
5. Bergner M, Bobbitt RA, Carter WB, Gilson BS. The SicknessImpact Profile: development and final revision of a healthstatus measure. Med Care 1981;19:787-805.
6. Hunt SM, McEwen J, McKenna SP. Measuring health status:a new tool for clinicians and epidemiologists. J R Coll GenPract 1985;35:185-8.
7. Stewart AL, Hays RD, Ware JEJ. The MOS short-form gen-eral health survey. Reliability and validity in a patient popu-lation. Med Care 1988;26:724-35.
8. Ware JEJ, Sherbourne CD. The MOS 36-item short-formhealth survey (SF-36). I. Conceptual framework and itemselection. Med Care 1992;30:473-83.
9. Urbach DR. Measuring quality of life after surgery. SurgInnov 2005;12:161-5.
10. Delaney CP, Kiran RP, Senagore AJ, O’Brien-Ermlich B,Church J, Hull TL, et al. Quality of life improves within30 days of surgery for Crohn’s disease. J Am Coll Surg2003;196:714-21.
11. Delaney CP, Lindsetmo RO, O’Brien-Ermlich B, CheruvuVK, Laughinghouse M, Champagne B, et al. Validation of
a novel postoperative quality-of-life scoring system. Am JSurg 2009;197:382-5.
12. Panacek EA. Survey-based research: general principles. AirMed J 2008;27:14-6.
13. Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ,Usherwood T, et al. Validating the SF-36 health survey ques-tionnaire: new outcome measure for primary care. BMJ1992;305:160-4.
14. Velanovich V. Behavior and analysis of 36-item Short-FormHealth Survey data for surgical quality-of-life research.Arch Surg 2007;142:473-7.
15. Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM,Schmulling C, Neugebauer E, et al. Gastrointestinal Qualityof Life Index: development, validation and application of anew instrument. Br J Surg 1995;82:216-22.
16. Guyatt GH, Bombardier C, Tugwell PX. Measuringdisease-specific quality of life in clinical trials. CMAJ1986;134:889-95.
17. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, CullA, Duez NJ, et al. The European Organization for Researchand Treatment of Cancer QLQ-C30: a quality-of-life instru-ment for use in international clinical trials in oncology.J Natl Cancer Inst 1993;85:365-76.
18. Sprangers MA, te Velde A, Aaronson NK. The constructionand testing of the EORTC colorectal cancer-specific qualityof life questionnaire module (QLQ-CR38). European Orga-nization for Research and Treatment of Cancer StudyGroup on Quality of Life. Eur J Cancer 1999;35:238-47.
19. Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G.Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: arandomized trial. JAMA 2002;287:321-8.
20. McCorkle R, Quint-Benoliel J. Symptom distress, currentconcerns and mood disturbance after diagnosis of life-threatening disease. Soc Sci Med 1983;17:431-8.
21. Fazio VW, O’Riordain MG, Lavery IC, Church JM, Lau P,Strong SA, et al. Long-term functional outcome and qualityof life after stapled restorative proctocolectomy. Ann Surg1999;230:575-84.
22. Kiran RP, Delaney CP, Senagore AJ, O’Brien-Ermlich B, Ma-scha E, Thornton J, et al. Prospective assessment of Cleve-land Global Quality of Life (CGQL) as a novel marker ofquality of life and disease activity in Crohn’s disease. Am JGastroenterol 2003;98:1783-9.
23. Maunder RG, Cohen Z, McLeod RS, Greenberg GR. Effectof intervention in inflammatory bowel disease on health-related quality of life: a critical review. Dis Colon Rectum1995;38:1147-61.
DISCUSSION
Dr Janice Rafferty (Cincinnati, OH): So essentiallythe authors have devised an instrument called thePQL to assess the quality of life for patients undergoingan abdominal operation because no specific scoring sys-tem is currently used for the assessment of postopera-tive quality of life after abdominal surgery. Dr Delaneyand others were previously able to demonstrate excel-lent internal consistency of their instrument, publish-ing their results in 2009. But the purpose of thisstudy, as I understand it, was to assess external consis-tency of the scoring system in patients undergoingmajor open or laparoscopic abdominal operations,comparing it with the more commonly known andfrequently used SF-36.

SurgeryOctober 2013
696 Keller et al
So although it’s more known and commonly used,the SF-36 does not assess quality-of-life issues specific topostoperative patients, as you said, specifically, pain,fatigue, nausea, and satisfaction with their outcome. Andit’s cumbersome.
Dr Keller, could you tell us a little more aboutexternal and internal validation? It’s not somethingthat’s commonly discussed in my surgeons’ lounge.
Second, as clinical surgeons, we don’t usually admin-ister our own SF-36. Do you envision this as somethingmore user friendly, that a surgeon such as myself inpractice could use to measure my own outcomes?
And finally, I’m also interested in your vision for howto use this. I’m specifically interested in knowing if youthink it will be useful to distinguish the differences inpatient satisfaction with perhaps a different approach tothe same operation as well as long-term outcomes,particularly looking at, say, a low anterior section doneopen versus laparoscopic, single-site, or some othertechnique that might be on our horizon.
Again, I would like to compliment you for tacklingthis topic and look forward to seeing this instrumentused in practice.
Dr Deborah Keller (Cleveland, OH): First, as far asvalidity and internal and external distinctions, I thinkthe easiest way to look at it is that internal is a test of
the test. Are the conclusions that we are making off ofthis test valid? Is this test useful?
And external is a test of the test versus the goldstandard. Is it comparable? Are our results validcompared with the gold standard?
As far as, is it user friendly? Yes, it’s extremely userfriendly. We do use it ourselves. Every patient who comesin for surgery, it’s part of the history and physical we dofor the patients. We take that 3 minutes in the clinic andprospectively administer the PQL, and then, in thehospital and at each follow-up survey. So it’s just secondnature at this point. You don’t even realize that the3 minutes are gone.
And because it is so easy to roll that into the thirdquestion, we have recently applied it to rectal cancersurgery patients. Looking at the quality-of-life differ-ences by procedure, Abdominoperineal Resection andLow Anterior Resection, and by approach, laparoscopicand open.
And looking at this abstract tool in a meaningful wayhas been really interesting, because we found that, byprocedure, at 60 days, there is no difference in quality oflife between an Abdominoperineal Resection and a LowAnterior Resection. And by approach, by 30 days, there’sno difference between open and laparoscopic. We’ll bepresenting those results at ASCRS this year.