Comparison of and - Heartventricular minoraxis dimensionat endsystole and end diastole (D. and Dd)....
Transcript of Comparison of and - Heartventricular minoraxis dimensionat endsystole and end diastole (D. and Dd)....

Br Heart J 1986; 55: 155-61
Comparison of electrocardiographic andechocardiographic measures of left ventricularhypertrophy in the assessment of aortic stenosisMARK DANCY
From the Department of Cardiology, St George's Hospital, London
SUMMARY One hundred and nineteen patients with a clinical diagnosis of important aorticstenosis were assessed clinically and by electrocardiography and M mode echocardiography todetermine the degree of left ventricular hypertrophy. Predicted left ventricular pressure wascalculated from two previously described formulas. Comparisons were made between the variousmethods for assessing left ventricular hypertrophy to see which method most reliably predictedthe severity of the stenosis as defined by invasive measurement of left ventricular pressure andpeak aortic valve gradient. Direct measurement of left ventricular wall thickness from theechocardiogram, expressed as the mean of septal and posterior wall thickness, was the mostaccurate predictor (r=0075 for 29 patients with high quality echocardiograms), and surpassedderived indices (left ventricular mass (r=0-68) and predicted left ventricular pressure derivedfrom the two formulas (r=0 39 and r=0 68)) in adults. Echocardiographic results weresignificantly better than electrocardiographic, but only when the recordings were of very highquality. Average quality echocardiograms were no better than precordial electrocardiographicvoltages for predicting the severity of aortic stenosis. The formulas for predicting left ventricularpressure were ofmore value in children than in adults, but they were still not sufficiently accurateto be predictive in individual cases. Electrocardiographic voltages were more accurate predictorsof the severity of aortic stenosis in children than in adults.
The detection of left ventricular hypertrophy hasbecome an important clinical goal, particularlyfor the diagnosis of aortic valve disease and theassessment of hypertension. There are severalmethods of evaluating left ventricular hyper-trophy-palpation of the apex beat, measurement ofnumerous electrocardiographic variables, and, morerecently, echocardiography-but there is littleinformation about the relative reliability of thesevarious techniques in predicting the severity ofaortic stenosis.This study compares the clinical, electro-
cardiographic, and echocardiographic assessmentsof left ventricular hypertrophy with the haemo-dynamic findings in patients suspected of havingimportant aortic stenosis.
Requests for reprints to Dr Mark Dancy, Department of Cardi-ology, St George's Hospital, London SW17 OQT.
Accepted for publication 6 August 1985
Patients and methods
One hundred and nineteen patients with a clinicaldiagnosis of important aortic stenosis were studiedat admission for cardiac catheterisation. There were71 males and 48 females (mean age of 51 years, range16-76). All patients had undergone clinicalassessment, 12 lead electrocardiogram, and M modeechocardiography in addition to cardiaccatheterisation. Mean peak systolic gradient acrossthe aortic valve was 68 (35) mm Hg, and mean leftventricular pressure was 197 (41) mm Hg. Patientswith bundle branch block, previous myocardialinfarction, established hypertension, or importantaortic valve regurgitation were excluded.The presence or absence of left ventricular
hypertrophy was assessed clinically by palpation ofthe cardiac apex with the patient turned on the leftside. Two measures of precordial electrocardio-graphic voltage were used: the Sokolow-Lyon
155
on July 21, 2021 by guest. Protected by copyright.
http://heart.bmj.com
/B
r Heart J: first published as 10.1136/hrt.55.2.155 on 1 F
ebruary 1986. Dow
nloaded from

156
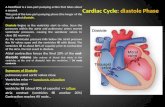
index' (S-Vi + R-V5 or V6> 35 mV) and theMcPhie index2 (max S+ max R 45 mV). Thepresence or absence of appreciable lateral STdepression (>1 mm) was noted. No patient wastaking digoxin. Standard M mode echocardiogramswere measured with a Numonics analyser (SmithKline instruments) that allows rapid repeatedmeasurements of the same variable in differentcardiac cycles and produces a mean value. At leastfive measurements were made for each variable. Thefollowing were measured by the method recom-mended by the American Society of Echocardio-graphy3: interventricular septal thickness at endsystole and end diastole (IVS, and IVSd); posteriorfree wall thickness of the left ventricle at end systoleand end diastole (LVW, and LVWd); and leftventricular minor axis dimension at end systole andend diastole (D. and Dd). From these data thefollowing were calculated:
(a) Mean left ventricular wall thickness at endsystole and end diastole (means and meand) bydividing the sum of septal and posterior wallthicknesses by two.
(b) Diastolic left ventricular mass by theTeichholz formula4 to derive left ventricular volume(taking the specific gravity of cardiac muscle to be1-05 g/cm3.5
Mass (g) = 105((LVWd + IVSd + Dd + 2.4)
(LVWd + IVSd + Dd)3 -(D 7 24) x Dd3)
(c) Predicted left ventricular pressure (LVPp) bytwo formulas:
LVPp = 225 x (LVWs/Ds)mm Hg6and
LVPp 6 + 298 x meand/rmmHg7where r = is the diastolic cavity radius.
(d) Mean rate of circumferential shortening (meanVcf) was calculated in circumferences per second asa measure of overall left ventricular function fromthe formula described by Fortuin et al.8
Patients with reduced left ventricular function(mean Vcf < 1 circ/s) were excluded from parts ofthe analysis as it had been stressed in a previousstudy that the assumptions necessary for applyingthe formulas for predicting left ventricular pressurewere invalid if left ventricular function wasabnormal.6 Mean Vcf was chosen as the measure ofleft ventricular function because it was the originalmeasure used by Bennett et al.6 Although there may,now be better methods of estimating left ventricularfunction, in the present study mean Vcf > 1 circlswas a valuable and fairly strict criterion for good left
Dancyventricular function, as was shown by subsequentcalculation of ejection fraction from thecineangiograms (by digitising end systolic and enddiastolic frames). Thus only one of 29 patients withmean Vcf > 1 circ/s had an ejection fraction of<50%, and the mean for the group was 67%. Allthe patients with a mean Vcf > 1 circ/s had a normalend systolic dimension on the echocardiogram.
All the echocardiograms were measuredregardless of their quality. The technical quality ofeach echocardiogram was assessed as either good(unquestionably high quality), fair (the sort ofquality which would normally be consideredacceptable for measurement but which was not quiteas clear as the good quality echocardiograms, forexample one endocardial boundary poorly defined),or poor. This classification meant that theimportance of technical quality in determining thepredictive value of echocardiographic measurementscould be assessed in the subsequent analysis.
All patients underwent cardiac catheterisationduring which peak left ventricular pressure and peaksystolic gradient across the aortic valve weremeasured. These two measurements were correlatedwith the estimates of left ventricular hypertrophyand predicted left ventricular pressure discussedabove. The advantage of using left ventricularpressure as an independent variable is that itcircumvents some of the problems associated withcoexisting hypertension. Cardiac output was notmeasured routinely, and although this could haveintroduced bias in the patients with low cardiacoutput, part of the subsequent analysis excludedpatients with poor left ventricular function (lowmean rate of circumferential shortening). None ofthe patients had important aortic regurgitation onclinical, echocardiographic, or aortographicgrounds.
ANALYSIS OF RESULTSThe ability of the different measures of leftventricular hypertrophy to predict the degree ofaortic stenosis (as measured by gradient across theaortic valve or left ventricular pressure) was assessedby calculating sensitivity and specificity, and, in thecase of continuous variables, by determining thecorrelation coefficient as well. To calculatesensitivity and specificity the dividing line betweenimportant and non-important aortic stenosis wastaken to be a gradient of 50 mm Hg or a leftventricular pressure of 180 mm Hg.Sensitivity.. (%) = (true positives correctlydiagnosed/total true positives) x 100Specificity. (%)= (true negatives correctlydiagnosed/total true negatives) x 100
on July 21, 2021 by guest. Protected by copyright.
http://heart.bmj.com
/B
r Heart J: first published as 10.1136/hrt.55.2.155 on 1 F
ebruary 1986. Dow
nloaded from

Assessment of left ventricular hypertrophy in aortic stenosis
Table 1 Sensitivity and specificity ofvarious measures of left ventricular hypertrophy as predictors either of the gradientacross the aortic valve or of left ventricular pressure in patients with aortic stenosis
Predictor Criterion Predicted Sensitivity (%) Specificity (%) Accuracy (%) Group
Clinical LVH Present or absent AVG 81 54 68 1LVP 73 44 58 1
ST depression ST depression >1 mm AVG 78 73 76 1LVP 83 61 75 1
Sokolow-Lyon' S-VI +R-V5/6 >35 mV AVG 85 31 69 1LVP 83 24 64 1
McPhie2 MaxS+MaxR 45mV AVG 74 57 69 1LVP 77 47 68 1
Med Weand, 1 15cm AVG 89 73 83 4LVP 77 81 79 4
Bennett6 LVPP A 180 mm Hg AVG 34 83 60 4LVP 38 75 59 4
Aziz7 LVPP >180mmHg AVG 33 100 56 4LVP 38 93 69 4
Meand, mean diastolic left ventricular wall thickness; LVH, left ventricular hypertrophy; AVG, aortic valve gradient; LVP, leftventricular pressure; LVPP, predicted left ventricular pressure. Bennett and Aziz are the two formulas for calculating LVP .
Accuracy (%)= ((positives + negatives correctlydiagnosed)/total tested) x 100
(reference9)Correlations between the gradient or left ventricularpressure and the various measures of left ventricularhypertrophy were made initially with all the patientsincluded (group 1), and then with subgroupsselected from group 1: group 2, all patients withhigh quality echocardiograms; group 3, thosepatients with a mean rate of circumferentialshortening > 1 circ/s (a prerequisite for theapplication of Bennett's formula)6; group 4, thosepatients with high quality echocardiograms andmean rate of circumferential shortening > 1 circ/s;group 5, those patients with fair qualityechocardiograms and mean rate of circumferentialshortening > 1 circ/s.Although these groupings could only be expected
to affect the correlations of the echo-derived
variables, identical groups were used to determinethe correlation of electrocardiographic variableswith the pressure gradient across the aortic valveand left ventricular pressure to avoid the possibilitythat selection of patients from the total studypopulation might have created unrepresentativegroups. A group of 13 children aged less than 16years was also analysed separately (group 6).
Results
CLINICAL ASSESSMENTLeft ventricular hypertrophy detected clinicallyhad a reasonable sensitivity but poor specificity(Table 1).
PREDICTION OF SEVERITY OF AORTIC STENOSIS
BY ELECTROCARDIOGRAMTable 1 gives the sensitivity and specificity for the
Table 2 Correlation coefficients for relations between measures of left ventricular hypertrophy and the pressure gradientacross the aortic valve or left ventricular pressure
Group
Measure ofLVH AVGorLVP 1 2 3 4 5 6(n=119) (n=SO) (n=62) (n=29) (n=25) (n= 13)
S-Vi + R-V5/6 AVG 0 27 0-42 0-12 0*34 0-34 0-32LVP 0-08 0-14 -0-10 0-05 0 05 0-42
Max R + Max S AVG 0-23 0-23 0-22 0-12 0 40 0-41LVP 0-12 0-24 0 07 0-01 0-22 0 58
Meand AVG 0-45 0-63 0 43 0-59 0-23 0 37LVP 0-52 0-66 0-63 0-75 0-44 0-19
Mass AVG 0-36 0 50 0-41 0-51 0-29 -
LVP 0 40 0 54 0-58 0-68 0 40 -Bennett6 AVG 0-18 0 05 0-31 0 39 0 35 0-72
LVP 0-16 0 005 0 34 0-39 0-35 0-68Aziz7 AVG 0 35 0-58 0 33 0-60 0-12 0-48
LVP 0-39 0-58 0-46 0-68 0-13 0 30
Meand, mean diastolic left ventricular wall thickness; AVG, aortic valve gradient; LVH, left ventricular hypertrophy; LVP, leftventricular pressure.
157
on July 21, 2021 by guest. Protected by copyright.
http://heart.bmj.com
/B
r Heart J: first published as 10.1136/hrt.55.2.155 on 1 F
ebruary 1986. Dow
nloaded from

95'1. CI
SE 300 -
250 -
200.
150.
100.
95,1.CI
0 50 100 150 200 250 300Predicted left ventricular pressure (mmHg)
i) 95/0. Cl
r_0-39n= 29 /, SE
0 0 [email protected] -.1
- _.SO4- 0
*~~~0 m~~
,--
S
0 50 100 150 200 250 300Predicted left ventricular pressure (mmHg)
Correlation of measured left ventricular pressure with three variables in 29 patients with high qualityechocardiograms andgood left ventricularfunction: (a) mean end diastolic left ventricular wall thickness (meand);(b) predicted left ventricular pressure as calculatedfrom theformula of Bennett et alP; and (c) predicted leftventricular pressure as calculatedfrom theformula of Aziz et al.7 95% confidence intervals (95% CI) forstandard error (SE) for the prediction of left ventricular pressures measured at catheterisation are shown.
voltage criteria and ST depression. Sensitivity was
fair but specificity poor for the voltage criteria.Sensitivity was similar and specificity greater withST depressions, giving an overall accuracy that was5-8% more than by voltage criteria. Correlationcoefficients relating precordial voltages to pressure
gradient across the aortic valve and left ventricularpressure were low (Table 2).
PREDICTION OF SEVERITY OF AORTIC STENOSIS BYECHOCARDIOGRAPHYLeft ventricular wall thicknessCorrelations were determined between leftventricular pressure or pressure gradient across theaortic valve and septal thickness, left ventricularposterior wall thickness, and mean left ventricularwall thickness at end systole and end diastole. Ingeneral end diastolic measurements correlated betterwith the haemodynamic variables than end systolicmeasurements, and mean wall thickness correlated
better than either septal or posterior wall thicknessalone. In the group as a whole (group 1) leftventricular wall thickness predicted the severity ofstenosis better than precordial electrocardiographicvoltages. The highest correlation coefficient was
found when 29 patients with good qualityechocardiograms and mean Vcf >1 circ/s were
selected (group 4) and the relation between mean
diastolic wall thickness and left ventricular pressurewas examined (r=0 75) (Table 2, Fig. a).
Sensitivity and specificity were calculated basedon the premise that a mean left ventricular wallthickness > 1-15 cm at end diastole indicatedimportant ventricular hypertrophy (all echocardio-graphic measurements were made to the nearest 0-1cm, but the process of calculating means producedfigures with two places of decimals). For group 4this gave a sensitivity of 89%, specificity of 73%,and accuracy of 83% for the prediction of pressuregradient across the aortic valve, the highest values
158 Dancy
300-
250-
200-:c
E 150-E4,
100-4,
:3
.C4, 300-
.-1
- 250-* la
:3M' 200-
150 -
100 I
on July 21, 2021 by guest. Protected by copyright.
http://heart.bmj.com
/B
r Heart J: first published as 10.1136/hrt.55.2.155 on 1 F
ebruary 1986. Dow
nloaded from

Assessment of left ventricular hypertrophy in aortic stenosis
for any of the methods used in this study. When thefair quality echocardiograms of patients with a meanrate of circumferential shortening > 1 circ/s wereanalysed separately (group 5) correlations with leftventricular pressure and pressure gradient acrossthe aortic valve were poor and resembledcorrelations with precordial electrocardiographicvoltage. Even with the high qualityechocardiograms, 95% confidence intervals forpredicing left ventricular pressure from meandiastolic wall thickness were wide (Fig. a)-with amean wall thickness of 1-15 cm predicting a leftventricular pressure of between 130 and 230 mmHg. A mean wall thickness of 1-75 cm or greater washighly likely to be associated with a left ventricularpressure of greater than 180 mm Hg.
Left ventricular massThe pattem of correlation coefficients for leftventricular mass was qualitatively similar to thatwith wall thickness, but less close (Table 2).
Predicted left ventricular pressureNeither of the two formulas for predicting leftventricular pressure was as closely correlated withmeasured left ventricular pressure as was meandiastolic wall thickness, and 95% confidenceintervals were wider (Table 2, Fig. b). Again, enddiastolic measurements (as used in the formula ofAziz) were better predictors than end systolicmeasurements (as used in the formula of Bennett).When a group (group 6) of children (< 16 years)
was analysed, the results were completely different(Table 2). The correlation of pressure gradientacross the aortic valve or left ventricular pressurewith mean diastolic wall thickness was poor,presumably because of the wide range of ages andtherefore heart sizes in the group. The formulas forpredicting left ventricular pressure, particularly theBennett formula, were considerably more accurate.
Discussion
The electrocardiographic9 l and echocardio-graphic12 methods of demonstrating left ventricularhypertrophy have been separately evaluated inseveral studies, but the strengths and weaknesses ofthe methods cannot be demonstrated except bycomparing them within the same group of patients.In one study in which this has been done it wasconcluded that precordial voltages were moreaccurate in predicting the severity of aortic stenosisthan was echocardiographic measurement of leftventricular hyertrophy. 3 The criteria fordiagnosing left ventricular hypertrophy byechocardiogram were not stated, however, and the
quality of the echocardiograms was not assessed.One of the strengths of electrocardiography is that
it can be performed on all patients and there are noimportant technical constraints in making arecording. With echocardiography the technicalquality of the recording is of great importance,particularly when thicknesses are measured, sinceeven small errors are a considerable proportion ofthe total measurement.'4 In this study highstandards were achieved in 42% of patients. Whenpoorer quality echocardiograms were analysed, thecorrelations with pressure gradient across the aorticvalve and left ventricular pressure were reduced tothose achieved by electrocardiogram. When highquality echocardiograms were available, meandiastolic left ventricular wall thickness was the bestpredictor of the severity of aortic stenosis. Inchildren wall thickness was a poor predictor of aorticstenosis because the range of heart sizes was muchgreater than that in adults. Precordial voltage,however, was if anything more accurate whenapplied to children than when applied to adults.
HYPERTENSIONHypertension is a potentially confounding variablein the relation between left ventricular wallthickness and pressure gradient across the aorticvalve. Patients with established hypertension wereexcluded from the study, and no patients were onhypotensive treatment (even for angina). Onadmission to hospital five patients had a diastolicblood pressure of > 100mm Hg, but none was > 110mm Hg. Their mean (SD) systolic blood pressurewas 158 (13) mm Hg. Because hypertension had notpreviously been recognised in these patients theywere included in the study. Only two satisfied thecriteria for group 4 (mean rate of circumferentialshortening > 1 circ/s and high qualityechocardiograms).
FORMULAS FOR PREDICTING LEFTVENTRICULAR PRESSUREThe theoretical basis for predicting left ventricularpressure is a highly simplified form of the law ofLaplace, which states that circumferential stress in athin-walled sphere is proportional to internalpressure and cavity diameter and inverselyproportional to wall thickness. With several majorassumptions this may be applied to the leftventricle.'5 On the basis that the hypertrophicresponse acts to keep peak circumferential wallstress constant in pressure overload (at least until theleft ventricle fails'6), left ventricular pressure isproportional to the ratio of left ventricular wallthickness to cavity dimension. Bennett et al were thefirst to realise the potential of this relation to predict
159
on July 21, 2021 by guest. Protected by copyright.
http://heart.bmj.com
/B
r Heart J: first published as 10.1136/hrt.55.2.155 on 1 F
ebruary 1986. Dow
nloaded from

160 Dancy
left ventricular pressure by non-invasive means.6 Anumber of similar formulas have since beendevised7 2'and have been shown to predict leftventricular pressure with some accuracy, althoughthere have been reservations.2223 The formula ofAziz et a17 was claimed to be superior because it usedend diastolic measurements (rather than the endsystolic measurements of Bennett's formula), sincepeak systolic wall stress occurs at the onset of systolebefore there has been appreciable fibre shortening.
Whatever the theoretical basis for the formulas,they all contain the well documented relationbetween left ventricular pressure and wall thickness,and for practical purposes it is important to knowhow much the formulas depends on this relation fortheir correlation, and how much the inclusion of thesecond variable, cavity dimension, alters the cor-relation. In the present study it was quite clear thatexcept in children the correlation between left ven-tricular pressure and ventricular wall thickness wascloser than the correlation between measured andpredicted left ventricular pressures from the twoformulas whatever group of adult patients was cho-sen. Left ventricular wall thickness was a poor pre-dictor of left ventricular pressure in children, how-ever, presumably because of the large range of heartsizes, and in children the Bennett formula per-formed reasonably well (r=0 68). There is a closerelation between cavity dimension and body surfacearea in children, even in those with aortic stenosis,7and the most likely explanation of these findings isthat cavity dimension functions as a normalisingvariable and therefore is of most value in childrenwhere the range of cavity dimensions is largest.Although sensitivity was very low for the Aziz for-mula, specificity was high (93%). This was largelydue to the fact that the formula tended to under-estimate left ventricular pressure, particularly at thelower end of the pressure range as is shown by theregression line (Fig. c).There are several other possible reasons why the
formulas for predicting left ventricular pressurefrom echocardiographic recordings are inaccurate.
Poor quality of echocardiographic recordingsPoor images cannot provide accurate measurements,and it is clear that the quality of echocardiographicrecording is highly important. Poor image qualitydoes not, however, explain why in the present studyleft ventricular wall thickness was a better predictorof left ventricular pressure than the two formulassince the same echocardiograms were used for deter-mining both sets of correlations.
Inaccuracies of measurementSmall inaccuracies of measurement are inevitable
even in good quality echocardiograms,24 althoughmaking repeated measurements minimises theerrors.'4 In the calculation of a ratio such asLVWd/Dd, however, inaccuracies tend to be ampli-fied because an error in locating either endocardialboundary will increase one measurement anddecrease the other. An error of as little as 1 mm ineither endocardial boundary may change the pre-dicted left ventricular pressure by as much as20mmHg.
Assumptions in the derivation of peak circumferentialwall stressThe estimation of peak circumferential wall stressby M mode echocardiography requires the assump-tion that the left ventricle behaves as a thin walledsphere. If this assumption is only partly correct thenthe accuracy with which left ventricular pressure canbe predicted by M mode echocardiography will belimited, even with a technically perfect recording.
Constancy of wall stress in aortic stenosisThere is now a considerable body of experience sug-gesting that the process of adaptation to increaseafterload is stimulated by abnormal wall stress andcompleted only when wall stress is returned to nor-mal.'6 2S There have, however, been two reports ofabnormal wall stress in patients with compensatedaortic stenosis.262The results of this study allow a clearer under-
standing of the place of these various methods ofassessing left ventricular hypertrophy in theinvestigation of patients suspected of havingimportant aortic stenosis. Of course in the clinicalsetting none of these variables would be used alonefor the assessment of an individual patient, but aknowledge of the sensitivity, specificity, andconfidence intervals indicates how much weight toplace on a particular result. In adults, who ate goodechocardiographic subjects, mean diastolic wallthickness provides more reliable information thaneither the electrocardiogram or left ventricular pres-sure predicted from formulas. If the echo-cardiograms are anything less than high quality theirreliability resembles that of the electrocardiogram.In children left ventricular pressure predicted fromthe echocardiogram is the most accurate method,but the correlations are not sufficiently strong for aninvestigator to be confident in borderline cases.
I am grateful to Graham Leech for his criticism ofthis paper.
References
1 Sokolow M, Lyon TP. The ventricular complex in left
on July 21, 2021 by guest. Protected by copyright.
http://heart.bmj.com
/B
r Heart J: first published as 10.1136/hrt.55.2.155 on 1 F
ebruary 1986. Dow
nloaded from

Assessment of left ventricular hypertrophy in aortic stenosis 161
ventricular hypertrophy as obtained by unipolar pre-cordial and limb leads. Am Heart J 1948; 37: 161-86.
2 McPhie J. Left ventricular hypertrophy: electro-cardiographic diagnosis. Australasian Annals of Medi-cine 1958; 7: 317-27.
3 Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recom-mendations regarding quantitation in M-mode echo-cardiography: results of a survey of echocardiographicmeasurements. Circulation 1978; 58: 1072-83.
4 Teichholz LE, Kreulen TH, Herman MV, Gorlin R.Problems in echocardiographic volume determinationsechoangiographic correlations in the presence orabsence of asynergy. Am J Cardiol 1976; 37: 7-11.
5 Bardeen CR. Determination of the size of the heart bymeans of X-rays. Am J Anat 1918; 23: 423-87.
6 Bennett DW, Evans DW, Raj MVJ. Echocardiographicleft ventricular dimensions in pressure and volumeoverload. Their use in assessing aortic stenosis. BrHeartJ 1975; 37: 971-7.
7 Aziz KU, van Grondelle A, Paul MH, Muster AJ.Echocardiographic assessment of the relation betweenleft ventricular wall and cavity dimensions and peaksystolic pressure in children with aortic stenosis. Am JCardiol 1977; 40: 775-80.
8 Fortuin NJ, Hood WP Jr, Craige E. Evaluation of leftventricular function by echocardiography. Circulation1972; 46: 26-35.
9 Reichek N, Devereux RB. Left ventricular hyper-trophy: relationship of anatomic, echocardiographicand electrocardiographic findings. Circulation 1981; 63:1391-8.
10 Romhilt DW, Bove KE, Norris RJ, et al. A criticalappraisal of the electrocardiographic criteria for thediagnosis of left ventricular hypertrophy. Circulation1969; 40: 185-95.
11 Clementy J, Bergere P, Bricaud H. Electro-cardiography and vectocardiography in the evaluationof left ventricular hypertrophy due to pressure over-load. Eur Heart J 1982; 3 (suppl A): 37-47.
12 Voeklel AG, Kendrick M, Pietro DA, et al. Non-invasive tests to evaluate the severity of aortic stenosis.Chest 1980; 77: 15540.
13 Nakamura V, Hultgren HN, Shettigar UR, Fowles RE.
Non-invasive evaluation of the severity of aortic steno-sis in adult patients. Am Heart J 1984; 107: 959-67.
14 Bullock RE, Amer H, Albers C, et al. Digitisation ofM-mode echocardiography. Its reproducibility andsources of imprecision. In: Hunter S, Hall R, eds. Echo-cardiography 2. Edinburgh and London: Churchill Liv-ingstone, 1984: 15-32.
15 Ford LE. Heart size. Circ Res 1976; 39: 297-303.16 Grossman W, Jones D, McLaurin LP. Wall stress and
patterns of hypertrophy in the human left ventricle. JClin Invest 1975; 56: 56-64.
17 Glanz S, Hellenbrand WE, Berman MA, Talner NS.Echocardiographic assessment of the severity of aorticstenosis in children and adolescents. Am J Cardiol1976; 38: 620-5.
18 Schwartz A, Vignola PA, Walker HJ, King ME, Gold-blatt A. Echocardiographic estimation of aortic valvegradient in aortic stenosis. Ann Intern Med 1978; 89:329-35.
19 Blackwood RA, Bloom KR, Williams CM. Aorticstenosis in children. Circulation 1978; 57: 263-8.
20 Gaasch WH. Left ventricular radius to wall thicknessratio. Am J Cardiol 1979; 43: 1189-94.
21 Quinones MA, Mokotoff DM, Nouri S, Winters WLJr, Miller RR. Non-invasive quantification of left ven-tricular wall stress. Am J Cardiol 1980; 45: 782-90.
22 Bass JL, Einzig S, Hong CY, Moller JH. Echo-cardiographic screening to assess the severity of con-genital aortic stenosis in children. Am J Cardiol 1979;44: 82-7.
23 Riggs T, Hirschfeld S. Left ventricular pressure in aor-tic stenosis [Letter]. Am J Cardiol 1978; 42: 690.
24 Felner JM, Blumenstein BA, Schlant RC, et al.Sources of variability in echocardiographic mea-surements. Am J Cardiol 1980; 45: 995-1004.
25 Linzbach AJ. Heart failure from the point of view ofquantitative anatomy. Am J Cardiol 1960; 5: 370-82.
26 Hood WP. Dynamics of hypertrophy in the left ven-tricular wall ofman. In: Alpert NR, eds. Cardiac hyper-trophy. New York: Academic Press, 1971: 445-52.
27 Donner R, Carabello BA, Black I, Spann JF. Left ven-tricular wall stress in compensated aortic stenosis inchildren. Am J Cardiol 1983; 51: 946-51.
on July 21, 2021 by guest. Protected by copyright.
http://heart.bmj.com
/B
r Heart J: first published as 10.1136/hrt.55.2.155 on 1 F
ebruary 1986. Dow
nloaded from