Comorbidities in spondyloarthritis 23.01.2014
-
Upload
boris-garro -
Category
Health & Medicine
-
view
308 -
download
1
Transcript of Comorbidities in spondyloarthritis 23.01.2014

Comorbidities SpA specific SpA unspecific
• Inflammatory bowel disease
• Psoriasis
• Uveitis
• Aortitis / aortic insufficiency
• Conduction disturbances (AV block)
• Apical pulmonary fibrosis
• Renal involvement
• Common cardiovascular diseases: coronary heart disease, arterial hypertension, stroke…
• Osteoporosis
• Infections
• Malignancies
• …

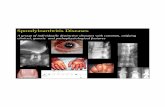
Extra-Articular Manifestations in Spondyloarthritis
Concept related
Eye-skin-gut-urogenital
• Frequent (20-60%) • Clinical inflammation - At any moment of the disease evolution
• Sometimes related to axial or joint inflammation • Effect of classical SpA drugs
=> Effect of TNF-blockers proven
Not concept related
Lung-kidney-heart-nerve
• Very rare (1%) • Mostly subclinical - Long standing disease
• Not related to locomotor disease
• No effect of classical SpA drugs
=> Effect of TNF-blockers unknown

Inflammatory Bowel Disease

Anterior UveitisPsoriasisIBDCombination
Ever present 42% Not Present
58% 51% 10%
20%
19%
n = 847
n = 355
Vander Cruyssen B et al. Ann Rheum Dis 2007;66:1072-7
Extra-Articular Manifestations in Ankylosing Spondylitis

Sensitivity Specificity LR+ LR- • inflammatory back pain 71-75 % 75-80 % 3.1 0.33 • enthesitis (heel pain) 16-37 % 89-94 % 3.4 0.71†
• peripheral arthritis 40-62 % 90-98 % 4.0 0.67† • dactylitis 12-24 % 96-98 % 4.5 0.85† • anterior uveitis 10-22 % 97-99 % 7.3 0.80† • psoriasis 10-20 % 95-97 % 2.5 0.94† • inflammatory bowel disease 5-8 % 97-99 % 4.0 0.97† • positive family history for SpA 7-36 % 93-99 % 6.4 0.72 • good response to NSAIDs 61-77 % 80-85 % 5.1 0.27 • elevated acute phase reactants 38-69 % 67-80 % 2.5 0.63 • HLA-B27 (axial involvement) 83-96 % 90-96 % 9.0 0.11 • Sacroiliitis on MRI 60-85 % 90-97 % 20.0* 0.41 • Sacroiliitis (≥ grade 3) on x-rays 40% 98 % 20.0* 0.61
Ankylosing Spondylitis / Axial Spondyloarthritis Typical Manifestations
Positive likelihood ratio (LR+) = sensitivity / (100 – specificity) Negative likelihood ratio (LR-) = (100 – sensitivity) / specificity
Modified from: Rudwaleit M et al. Ann Rheum Dis 2006;65:1251-2
* best estimate
† It is recommended to ignore a negative test result of these tests in an early state of possible axial SpA

Frequency of SpA manifestations in the GESPIC cohort
Rudwaleit M, et al. Arthritis Rheum 2009;60:717-27.
AS (n=236) non-radiographic axial SpA (n=226)
Inflammatory back pain, ever 98.7% 100%
Peripheral arthritis 37.4% 40.9% Enthesitis 39.4% 43.6%
Uveitis 20.9% 12.4%
Dactylitis 6.3% 4.0%
Psoriasis 10.2% 9.8% Inflammatory bowel disease 2.6% 1.8%

Typical Gut Lesions in Crohn‘s Disease
Crohn‘s disease lesions in the colon with deep ulcerations and islands of regenerative mucosa in between.

Bakterium T- Zelle
IBD SpA
T-Cells
Bacteria
Identical (CD8+) T-cell expansions in the colon mucosa and the synovium of a patient with enterogenic spondyloarthropathy.
Hypothesized relationship between IBD and SpA
May E, et al. Gastroenterology 2000;119:1745-55.

inflammatory gut lesions in SpA without associated gastrointestinal symptoms
Inflammatory gut lesions:
• Macroscopic: ~30%
• Microscopic: ~60% (1/3 – acute und 2/3 – chronic, Crohn-like lesions)
Mielants H, et al. Br J Rheumatol 1988;27 Suppl 2:95-105. De Vos M, et al. Gastroenterology 1989;96:339-44. Mielants H, et al. J Rheumatol 1995;22:2273-8.

normal acute chronic
reactive arthritis undifferentiated SpA
Ankylosing spondylitis
Inflammatory gut lesions in various forms of SpA without associated gastrointestinal symptoms
Mielants H, et al. J Rheumatol 1995;22:2273-8.

Van Praet L, et al. Ann Rheum Dis 2013;72:414-7.
Inflammatory gut lesions in SpA

Active SpA
3
13
4 1
11
16 patients
6
9
1
14
SpA in remission
15 patients
Acute Chronic Normal
Evolution of SpA and inflammatory gut lesions over time
Mielants H, et al. J Rheumatol 1995;22:2273-8.
Follow-up: 2 bis 9 years
Remission of joint inflammation in SpA was always associated with disappearance of gut inflammation, whereas persistence of locomotor (joint) inflammation was mostly associated with persistence of gut inflammation.

Colombel JF, et al. N Engl J Med 2010;362:1383-95.
SONIC-Studie: Infliximab, Azathioprine, or Combination Therapy for Crohn’s Disease

Efficacy of Anti-TNFα-Therapy in Crohn’s Disease
Response (CDAI score <150 points)
Hanauer SB et al. Lancet 2002;359:1541-9
Colombel JF et al. Gastroenterology 2007;132:52-65
Week 26
Week 30
§
# #
# p<0.01 vs Placebo
§
§p<0.001 vs Placebo
Infliximab 5 mg/kg at week 0 for all patients, then infusions of placebo or infliximab at weeks 2, 6 and every 8 weeks thereafter.
Adalimumab 80 mg at week 0 and 40 mg at week 2 for all patients. At week 4 patients were randomized to 1 of 3 groups .

A : before anti-TNF therapy: colitis and ulcers B : after treatment with infliximab: normal findings
A B
Efficacy of Anti-TNF-α-Therapy in Chronic Inflammatory Bowel Disease
Ileocolonoscopy in a patient with Crohn’s disease

Weeks
Swol
len
Join
t Cou
nt (S
JC)
0
1
2
3
4
5
6
SJC
1 5 9 13 17 21 25 29 33
Effect of Anti-TNFα-Therapy on Articular Symptoms in Crohn’s Disease
van den Bosch F et al. Lancet 2000;356:1821-2 (with permission)
CR
P (m
g/dl
)
0
5
10
15
20
25
CRP
30 Infliximab (i.v. infusion of 5 mg/kg body weight)

0%10%20%30%40%50%60%70%80%90%
100%
Week 0 Week 12
severemoderatemildno symptoms
Herfarth H, et al. Am J Gastroenterol 2002;97:2688-90.
Improvement of arthritis/arthralgia (n=59) during therapy of Crohn’s disease with Infliximab

Cox II-inhibitors in IBD?
• RCT with Etoricoxib 60-120 mg/day over 3 months in patients with IBD
– Etoricoxib group (n=76): 10.53% flare – Control group (n=70): 11.43% flare
• All adverse events, which resulted in study discontinuation, occurred during the first month.
El Miedany Y, et al. Am J Gastroenterol 2006;311-317.

• Placebo-controlled trial with Celecoxib 200 mg/day over 14 days in patients with IBD in remission
– Celecoxib group (n=110): 3% flare – Control group (n=112): 4% flare
• Definition of remission und flare: combination of clinical and endoscopic parameters
Sandborn WJ, et al. Clin Gastroenterol Hepatol 2006;4:157-9.
Cox II-inhibitors in IBD?

Low but Different Incidence of Acute Inflammatory Bowel Disease (IBD) in AS Patients on Anti-TNFα-Therapy
Braun J et al. Arthritis Rheum 2007;57:639-47
*OR = odds ratio in comparison with Infliximab
0
1
2
3
Infliximab Etanercept Adalimumab Placebo
Incidence of IBD (9 trials, pooled data, n = 1130)
1.3/ 100 patient years
0.2/ 100 patient years
2.3/ 100 patient years
Even
ts/1
00 p
atie
nt y
ears
Infliximab: 618.0
exposure years
Etanercept: 625.4
exposure years
Adalimumab: 132.3
exposure years
Placebo: 150.4
exposure years
2.2/ 100 patient years
*OR = odds ratio in comparison with Infliximab
OR: 4.2*
OR: 18.0*

Psoriasis

Sensitivity Specificity LR+ LR- • inflammatory back pain 71-75 % 75-80 % 3.1 0.33 • enthesitis (heel pain) 16-37 % 89-94 % 3.4 0.71†
• peripheral arthritis 40-62 % 90-98 % 4.0 0.67† • dactylitis 12-24 % 96-98 % 4.5 0.85† • anterior uveitis 10-22 % 97-99 % 7.3 0.80† • psoriasis 10-20 % 95-97 % 2.5 0.94† • inflammatory bowel disease 5-8 % 97-99 % 4.0 0.97† • positive family history for SpA 7-36 % 93-99 % 6.4 0.72 • good response to NSAIDs 61-77 % 80-85 % 5.1 0.27 • elevated acute phase reactants 38-69 % 67-80 % 2.5 0.63 • HLA-B27 (axial involvement) 83-96 % 90-96 % 9.0 0.11 • Sacroiliitis on MRI 60-85 % 90-97 % 20.0* 0.41 • Sacroiliitis (≥ grade 3) on x-rays 40% 98 % 20.0* 0.61
Ankylosing Spondylitis / Axial Spondyloarthritis Typical Manifestations
Positive likelihood ratio (LR+) = sensitivity / (100 – specificity) Negative likelihood ratio (LR-) = (100 – sensitivity) / specificity
Modified from: Rudwaleit M et al. Ann Rheum Dis 2006;65:1251-2
* best estimate
† It is recommended to ignore a negative test result of these tests in an early state of possible axial SpA

Frequency of SpA manifestations in the GESPIC cohort
Rudwaleit M, et al. Arthritis Rheum 2009;60:717-27.
AS (n=236) non-radiographic axial SpA (n=226)
Inflammatory back pain, ever 98.7% 100%
Peripheral arthritis 37.4% 40.9% Enthesitis 39.4% 43.6%
Uveitis 20.9% 12.4%
Dactylitis 6.3% 4.0%
Psoriasis 10.2% 9.8% Inflammatory bowel disease 2.6% 1.8%

CASPAR, ClASsification criteria for Psoriatic ARthritis Taylor W et al. Arthritis Rheum 2006;54:2665-2673
Classification of Psoriatic-Arthritis: CASPAR Criteria
To meet the CASPAR criteria for PsA, a patient must have inflammatory articular disease (joint, spine, or entheseal) and score ≥3 points based on these categories.
POINTS
1. Evidence of psoriasis Current psoriasis Personal history of psoriasis Family history of psoriasis
2 or 1 or
1
2. Psoriatic nail dystrophy Pitting, onycholysis, hyperkeratosis 1
3. Negative test result for rheumatoid factor 1
4. Dactylitis Current swelling of an entire digit History of dactylitis
1 or
1
5. Radiologic evidence of juxta-articular new bone formation Ill-defined ossification near joint margins on plain x-rays of hand/foot 1

ASAS Classification Criteria for Peripheral Spondyloarthritis (SpA)
≥ 1 SpA feature • uveitis • psoriasis • Crohn‘s/colitis • preceding infection • HLA-B27 • sacroiliitis on imaging
Arthritis or enthesitis or dactylitis
plus
≥ 2 other SpA features • arthritis • enthesitis • dactylitis • IBP (ever) • family history for SpA
OR
Sensitivity: 77.8%, Specificity: 82.2%; n=266 Peripheral arthritis: usually predominantly lower limbs and/or asymmetric arthritis Enthesitis: clinically assessed Dactylitis: clinically assessed IBP: Inflammatory back pain
Rudwaleit M et al. Ann Rheum Dis 2011;70:25-31 (with permission)

Psoriasis management (in close collaboration with a dermatologist)
Nast A, et al. Arch Dermatol Res 2012;304:87-113.

TNF α blockers in psoriasis
Reich K, et al. Lancet 2005; 366: 1367-1374.
Baseline PASI = 21.3
Week 24 PASI = 0.9
PASI: Psoriasis Area Severity Index
Treatment with infliximab

60
1
0
20
40
60
80
100
2338
3020406080100
1
56
1
0
20
40
60
80
100
59
1
0
20
40
60
80
100
Improvement of the skin: PASI 75-response rates at week 24 in PsA in Biologicals trials
1 Mease P. et al. Arthritis Rheum 2005; 52: 3279–3289 2 Mease P. et al. Arthritis Rheum 2004; 50: 2264–2272 3 Kavanaugh A. et al. Ann Rheum Dis 2007; 66: 498–505 4 Kavanaugh A. et al. EULAR 2008 OP-0161; Arthritis Rheum 2009; 60: 976–986
Patie
nten
(%)
Placebo n = 69
Adalimumab 40 mg alle 2 Wo.
n = 69
Adalimumab1 *
Patie
nten
(%)
Placebo n = 62
Etanercept Wo 24
25 mg 2 x/Wo. n = 66
Etanercept2
*
Patie
nten
(%)
Placebo n = 87
Infliximab 5 mg/kg n = 83
Infliximab3 *
Patie
nten
(%)
Placebo n = 73
Golimumab 50 mg alle 4 Wo.
n = 102
Golimumab4 *
* p < 0,001 vs. Placebo
Etanercept Wo 52
25 mg 2 x/Wo.

Biologics other than TNF α Inhibitors and Small Molecules Target Targeting substance
Interleukin-12/23 Ustekinumab (monoclonal antibody to p-40-chain IL-12/23)
Briakinumab (monoclonal antibody to p-40-chain IL-12/23)
Phosphodiesterase 4 Apremilast (PDE4 inhibitor, small molecule)
Interleukin-17
Secukinumab (monoclonal antibody to IL-17)
Ixekizumab (monoclonal antibody to IL-17)
Brodalumab (monoclonal antibody to IL-17-receptor)

Efficacy of ustekinumab at week 12 in two clinical trials for moderate-to-severe psoriasis
Leonardi CL, et al. Lancet 2008;371:1665-74. Papp KA, et al. Lancet 2008;371:1675-84.
p < 0.001 ustekinumab vs. placebo

Week 12 data of a head-to-head comparison of etanercept and ustekinumab in patients with psoriasis
*p = 0.012 superiority versus etanercept; **p < 0.001 superiority versus etanercept
ACCEPT trial
Griffiths CE, et al. N Engl J Med 2010;362:118-28.

Ustekinumab efficacy (ACR 20) in a phase III trial in PsA PSUMMIT 1 study
McInnes IB, et al. Lancet 2013;382:780-9.


Efficacy of IL-17 Inhibitors (PASI 75) in Plaque Psoriasis
1Leonardi et al. N Engl J Med 2012;366:1190-9 2Papp et al. Br J Dermatol. 2013;168:412-21. 3Papp et al. N Engl J Med 2012;366:1181-9
Ixekizumab (LY2439821)1
n=141
Secukinumab (AIN457)2
n=125
Brodalumab (AMG827)3
n=198

Apremilast, an oral Phosphodiesterase-4 Inhibitor Apremilast specifically inhibits Phosphodiesterase-4 which leads to an increase of intra-cellular cAMP and modulation of different mediators of inflammation.
Schafer P. Biochem Pharmacol 2012;83:1583-90.

Efficacy of apremilast in psoriasis (change in PASI scores)
Papp K, et al. Lancet 2012;380:738-46.

Achievement of PASI 100 in a patient treated with apremilast 30 mg twice daily
Papp K, et al. Lancet 2012;380:738-46.

Efficacy of Apremilast in PsA
Schett G, et al Arthritis Rheum 2012;64:3156-67.
PALACE 1 Study, response at week 12
n = 67
n = 69
n = 68

4. Extra-articular manifestations and comorbidities
• The frequently observed extra-articular manifestations, for example, psoriasis, uveitis and IBD, should be managed in collaboration with the respective specialists.
• Rheumatologists should be aware of the increased risk of cardiovascular disease and osteoporosis.
ASAS/EULAR Recommendations for the Management of Ankylosing Spondylitis (4/11)
Braun J et al. Ann Rheum Dis 2011;70:896-904

Cardiovascular comorbidities

Risk of myocardial infarction and stroke in AS • A systematic literature review with 8 longitudinal studies.
• AS (n=3,279): 224 MI cases (incidence 7.4%; 95%CI 5.2%, 10.0%).
• Controls (n=82,745): 1318 MI cases (incidence 4.6%; 95%CI 1.2%, 10.0%).
• Risk ratio for MI 1.88 (95% CI 0.83, 4.28).
• No risk increase for stroke, but higher weighted mean intima-media thickness and higher risk of metabolic syndrome.
• Lipid profile in AS: a significant decrease in triglycerides, total cholesterol, and high-density lipoprotein (HDL).
Mathieu S, et al. Arthritis Care Res (Hoboken) 2011;63:557-63.

Standardized morbidity-rate ratios in AS patients as compared to general population in Sweden
Bremander A, et al. Arthritis Care Res (Hoboken) 2011;63:550-6.
Males
Females

Increased risk of cardiovascular and cerebrovascular diseases in individuals with ankylosing spondylitis
Szabo SM, et al. Arthritis Rheum 2011;63:3294-304.
A population-based study in Quebec, n = 8 616 individuals with AS diagnosed over the period 1996-2006.
Aortic valvular heart disease
Nonaortic valvular heart disease
Any cardiovascular hospitalization
Ischemic heart disease
Congestive heart failure
Cerebrovascular disease
Other cardiovascular disease
Standardized Prevalence Ratio (95% CI)

Increased mortality in AS Population based estimation of the standardized mortality ratios (SMRs) in Hong-Kong, China N = 5243 SLE, 8367 RA, 2154 AS, and 778 PsA patients
Mok CC, et al. Arthritis Rheum 2011;63:1182-9.

Hospital-based study in Norway, n = 677 patients, follow-up period: 1977-2009



Osteoporosis

Prevalence of low bone mineral density of lumbar spine and femoral neck in AS
van der Weijden MA, et al. Clin Rheumatol 2011;30:497-503.
Overall prevalence of • decreased BMD (T-score <−1.0): 51-54%, • osteopenia: 38-39%, • osteoporosis: 13-16%.

Osteoporosis and osteopenia in long-standing AS
Grazio S, et al. Rheumatol Int 2012;32:2801-8.
N = 80, mean disease duration: 21.8 ± 10.3 years
BMD correlated negatively with inflammatory activity (CRP, ESR)

Risk of fractures in AS
Vosse D, et al. Ann Rheum Dis 2009;68:1839-42.
Risk of fractures is increased: • in the presence of IBD. Risk of fractures is decreased: • with NSAIDs intake.
A primary care-based nested case-control study

High frequency of vertebral fractures in early spondyloarthritis
van der Weijden MA, et al. Osteoporos Int 2012;23:1683-90.
Fracture = reduction of ≥20% of the vertebral height (Genant score grade 1)
Factors significantly associated with fractures: • lower BMD in the lumbar spine, • psoriasis.

Genant vertebral fracture score
Genant HK, et al. J Bone Miner Res 1993;8:1137-48.

Prevalence of vertebral fractures in AS
Klingberg E, et al. J Rheumatol 2012;39:1987-95.
The majority of fractures were subclinical. Factors significantly associated with fractures: • lower BMD, • higher age and longer disease duration, • impaired mobility, • syndesmophyte formation, • smoking.

Osteoporosis: summary • Patients with ankylosing spondylitis are at risk for osteoporosis and
osteoporotic vertebral fractures.
• Significant bone loss might occur even early in the course of the disease.
• In patients with long-standing AS, a BMD measurement in the hip neck might provide more reliable results in comparison to lumbar spine.
• Risk of osteoporosis and fractures is increased in patients with high inflammatory activity, long-standing disease, presence of syndesmophytes and limited spinal mobility and in smokers. Psoriasis and IBD are also associated with higher risk for osteoporosis.
• Whether antiosteoporotic treatment initiated early might improve the long-term outcome is unclear.