CME MODERN MEDICINE · THE MULTIDISCIPLINARY PEER-REVIEWED CONTINUING MEDICAL EDUCATION JOURNAL ......
Transcript of CME MODERN MEDICINE · THE MULTIDISCIPLINARY PEER-REVIEWED CONTINUING MEDICAL EDUCATION JOURNAL ......

MIDDLE EAST
MODERNMEDICINE
Q2 | 2016THE MULTIDISCIPLINARY PEER-REVIEWED CONTINUING MEDICAL EDUCATION JOURNAL
VOLUME 33 | NUMBER 02 | 2016
CME
BEST OF CONTINUING MEDICAL EDUCATION 2016Acute Otitis Media in Young Children Diagnosis and ManagementAcute otitis media is one of the most common reasons children are
with certainty in infants and young children and management.
Investigation and Management of Recurrent Urinary Tract infectionRecurrent urinary tract infections are common in women; after investigations to exclude common predisposing causes and complications, the focus is on strategies to prevent recurrence.
Medical Management After Control of Myocardial IschaemiaAfter recovery from myocardial infarction, patients should receive aspirin and statin therapy and be evaluated regarding their need for coronary revascularisation, additional pharmacological treatment and possible device therapy.
MIDDLE EAST REVIEW Ludwig’s Angina A Life Threatening Emergency Ludwig’s angina is a potentially life threatening condition which is a known but rare condition.
CME Answers for the Quarter 1 - 2016


MIDDLE EAST BOARD OF CONSULTANTSin Alphabetical Order
PROF. ABDULRAHMAN S. AL-FRAYH, MD
• Prof. of Pediatrics• Chairman of the Saudi National
Asthma Committee• Vice President of the Saudi Pediatric
Association• Previous Dean of the Faculty of
Medicine, King Saud University
PROF. MANSOUR M. AL-NOZHA, MD, FRCP, FACC, FESC
• Professor of Medicine and consultant Cardiologist
• President, Taibah University, Madinah Munawwarah, Saudi Arabia
PROF. KHALED ALSAEID, MD, FAAP
• Dean of Students and Associate Professor and Consultant
• Pediatrics and Infectious Diseases & Rheumatology at Kuwait University.
• Practices Pediatrics at Mubarak Teaching Hospital.
DR. KHALID OBEAD BAWAKID, MBBS, DCH (Ireland), DAC (UK), ABFM, JBFM, AAFP
• Consultant Family Medicine • Medical Supervisor & Head of Training
and CME Program, Jeddah.• Member of the Saudi Society of Family
Medicine and of Pediatric.
PROF. GALAL LOTFI, MD, MRCOG
• Professor Ob. & Gynecology Canal Suez University
• Head department Obstetrics & Gynecology, Suez Canal University.
DR. ABDULWAHAB AHMED BAWAHAB, MBBS, FACHARZT (Internal Medicine & Endocrinology)
• Fellow Royal Society of Medicine (UK).• Member American Diabetes
Association & American Endocrine Association.
COMING NEXT MONTH
MODERN MEDICINE is marketed by HCP-MEPPO, Beirut, Lebanon, and printed in Lebanon and U.A.E. in order to service the respective surrounding countries. (ISSN: 0759-240X)
Copyright© 2016 by P&CC-Publishing and Communications Company, Ltd., Nicosia - Cyprus. All rights reserved. No part of this publication may be reproduced or trans-mitted in any form or by any means, electronic or mechanical, including, photocopy, recording, or any information or retrieval system, without permission in writing from the publisher. MODERN MEDICINE is a registered trademark owned by P&CC-Publishing and Communications Company, Ltd.
All the Modern Medicine editorial is selected from a pool of international editions. In order to determine the physician’s interest in reading any specific article, we pre-test all available editorial with a revolving ran-dom sample of doctors in the Middle East. Only articles rating more than 65% as interesting-to-read are cleared for publishing in Modern Medicine. Any article rating above 85% qualifies to become a CME article.
JEDDAH PRIMARY CARE CME UNIT
In collaboration with
P&CC PUBLISHING & COMMUNICATIONS CO. LTD.Registered office: 7, Stasandrou street | CY-1060 | Nicosia | CyprusOperations office: 11, Boumboulina street | Suite 22 | Nicosia | CyprusTel: +357.2 244-7727 | Email: [email protected]
Medical NewsThe latest medical news.
CME - Continuing Medical EducationThe Cardiac Complications of ObesityObesity is a powerful risk factor for cardiovascular events, but accumulating data suggest that patients can remodel their hearts and improve health outcomes by losing weight..
In the MedicineAAOS Guideline for the Treatment of Knee OsteoarthritisWhile this time of year usually brings cheerful weather and the growth of beautiful plants, millions of people will be gearing up once again to do battle with a problem that recurs every year. Itchy eyes, repetitive sneezing, a permanently runny nose - the symptoms of seasonal allergies.
Notes: The above articles are subject to change without prior notice.

UAE.LEV.15.11.07
For f
urth
er m
edic
al in
form
atio
n, p
leas
e co
ntac
t : F
or U
AE: 8
00 M
edica
l Tol
l Fre
e N
umbe
r, F
or a
ll Gul
f Cou
ntrie
s: m
edica
l-info
rmat
ion.
gulf@
sano
fi.co
m Fu
ll pre
scrib
ing
info
rmat
ion
is a
vaila
ble
upon
requ
est a
t: Sa
nofi
Reg
iona
l Offi
ce, J
umei
rah
Lake
s To
wer
s, D
ubai
, UAE
To re
port
adve
rse
even
ts, p
leas
e ca
ll +9
7156
1747
001
or e
mai
l: gul
f.pha
rmac
ovig
ilanc
e@sa
nofi.
com
Abbr
evia
ted
Pres
crib
ing
Info
rmat
ion:
In
dica
tions
: Tav
anic
can
be u
sed
to tr
eat in
fect
ions
of th
e: si
nuse
s, b
ronc
hi/lu
ngs,
in p
eopl
e w
ith lo
ng-te
rm b
reat
hing
pro
blem
s or p
neum
onia
, urin
ary t
ract
, inclu
ding
the
kidne
ys a
nd b
ladd
er, p
rost
ate,
if yo
u ha
ve lo
ng-la
stin
g in
fect
ion,
skin
and
tissu
e un
der t
he sk
in, in
cludi
ng m
uscle
s (th
is is
som
etim
es c
alle
d “s
oft t
issue
”). C
ontra
indi
catio
ns: D
o no
t tak
e Ta
vani
c film
-coa
ted
tabl
ets
and
tell y
our d
octo
r: if y
ou a
re a
llerg
ic to
levo
floxa
cin, a
ny o
ther
qui
nolo
ne a
ntib
iotic
, if y
ou h
ave
or h
ave
ever
had
epi
leps
y, if
you
have
eve
r had
tend
on p
robl
ems,
suc
h as
tend
initis
, re
late
d to
trea
tmen
t with
a q
uino
lone
ant
ibio
tic. A
tend
on is
a co
rd th
at a
ttach
es, m
uscle
to b
one.
If yo
u ar
e a
child
or a
dole
scen
t in th
e gr
owth
pha
se, if
you
are
preg
nant
, may
bec
ome
preg
nant
, or t
hink
you
may
be
preg
nant
or b
reas
t-fee
ding
. Tal
k to
your
doc
tor o
r pha
rmac
ist b
efor
e ta
king
Tava
nic.
Dru
g in
tera
ctio
ns: T
akin
g th
is m
edica
tion
incr
ease
s the
risk o
f sid
e ef
fect
s of C
ortic
oste
roid
s, W
arfa
rin, T
heop
hyllin
e, N
on-s
tero
idal
ant
i-infla
mm
ator
y dru
gs (N
SAID
s), C
iclos
porin
, Med
icine
s kno
wn
to a
ffect
the
hear
t rat
e, d
rugs
for d
epre
ssio
n (tr
icycli
c ant
idep
ress
ants
), dr
ugs
for b
acte
rial in
fect
ions
(cer
tain
ant
ibio
tics
of th
e m
acro
lide
grou
p su
ch a
s er
ythr
omyc
in, a
zithr
omyc
in a
nd c
larit
hrom
ycin
), dr
ugs
for m
enta
l pro
blem
s (c
erta
in a
ntip
sych
otics
), Pr
oben
ecid
. If
you
have
redu
ced
kidne
y fu
nctio
n, y
ou d
octo
r may
redu
ce th
e do
se. S
ide
effe
cts:
Like
al
l med
icine
s, th
is m
edici
ne c
an c
ause
sid
e ef
fect
s, a
lthou
gh n
ot e
very
body
get
s th
em. T
hese
effe
cts
are
norm
ally
mild
or m
oder
ate
and
ofte
n di
sapp
ear a
fter a
sho
rt tim
e. C
omm
on S
ide
Effe
cts:
Tel
l you
r doc
tor i
f any
of t
he fo
llow
ing
side
effe
cts
get s
erio
us o
r las
t long
er th
an a
few
da
ys: S
leep
ing
prob
lem
s, H
eada
che,
dizz
ines
s, F
eelin
g sic
k (n
ause
a, v
omitin
g) a
nd d
iarrh
ea,
Incr
ease
in c
erta
in liv
er v
alue
s fo
und
thro
ugh
bloo
d te
sts.
Oth
er p
ossib
le s
ide
effe
cts
inclu
de: D
rop
in th
e nu
mbe
r of r
ed b
lood
cel
ls (a
nem
ia),
Feve
r, so
re th
roat
and
gen
eral
per
siste
nt
feel
ing
of b
eing
unw
ell,
Failu
re o
f circ
ulat
ion,
hyp
ergl
ycem
ia, d
yskin
esia
, ext
rapy
ram
idal
diso
rder
s, fa
intin
g, T
empo
rary
loss
of s
ight
, Dec
reas
e or
loss
of h
earin
g, A
bnor
mal
ly fa
st h
eartb
eat,
life-th
reat
enin
g irr
egul
ar h
eartb
eat i
nclu
ding
car
diac
arre
st, c
hang
es in
hea
rt ra
te,
bron
chos
pasm
, Alle
rgic
lung
reac
tions
, pan
crea
titis,
hep
atitis
, pho
tose
nsitiv
ity, v
ascu
litis,
sto
mat
itis, r
habd
omyo
lysis,
arth
ritis,
Pai
n, in
cludi
ng b
ack,
che
st a
nd lim
b pa
in, A
ttack
s of
por
phyr
ia in
peo
ple
who
alre
ady
have
por
phyr
ia (a
ver
y ra
re M
etab
olic
dise
ase)
, ben
ign
intra
cran
ial
hype
rtens
ion.
Con
tent
: The
act
ive s
ubst
ance
is le
voflo
xacin
. One
500
mg
Tava
nic
film-c
oate
d ta
blet
con
tain
s 50
0 m
g of
levo
floxa
cin. T
avan
ic so
lutio
n fo
r inf
usio
n is
avai
labl
e in
500
mg
in a
100
ml g
lass
bot
tle. O
ne m
l of s
olut
ion
for i
nfus
ion
cont
ains
5 m
g of
levo
floxa
cin. D
osag
e:
Tava
nic
500
mg
tabl
et: A
dults
and
eld
erly
peop
le In
fect
ions
of t
he s
inus
es: 1
film
-coa
ted
tabl
et o
f Tav
anic
500
mg,
onc
e da
ily, I
nfec
tions
of t
he b
ronc
hi in
pat
ient
s w
ith lo
ng-te
rm b
reat
hing
pro
blem
s: 1
film
-coa
ted
tabl
et o
f Tav
anic
500
mg,
onc
e da
ily. P
neum
onia
: 1 fi
lm-c
oate
d ta
blet
of
Tav
anic
500
mg,
onc
e or
twice
dai
ly. In
fect
ions
of t
he u
rinar
y tra
ct in
cludi
ng th
e kid
neys
and
bla
dder
: ½ o
r 1 fi
lm-c
oate
d ta
blet
of T
avan
ic 50
0 m
g, o
nce
daily
. Inf
ectio
ns o
f the
pro
stat
e: 1
film
-coa
ted
tabl
et o
f Tav
anic
500
mg,
onc
e da
ily. I
nfec
tions
of t
he s
kin a
nd tis
sue
unde
r the
sk
in, in
cludi
ng m
uscle
: 1 fi
lm-c
oate
d ta
blet
of T
avan
ic 50
0 m
g, o
nce
or tw
ice d
aily.
Tav
anic
IV: A
dults
and
the
elde
rly: P
neum
onia
: 500
mg
once
or t
wice
dai
ly. In
fect
ion
of u
rinar
y tra
ct, in
cludi
ng y
our k
idne
ys o
r bla
dder
: 500
mg
once
dai
ly. P
rost
ate
glan
d in
fect
ion:
500
mg
once
dai
ly.
Infe
ctio
n of
skin
and
und
erne
ath
the
skin
inclu
ding
mus
cles:
500
mg
once
or t
wice
dai
ly. A
dults
and
the
elde
rly w
ith k
idne
y pr
oble
ms:
You
r doc
tor m
ay n
eed
to g
ive y
ou a
low
er d
ose.
Chi
ldre
n an
d Te
enag
ers.
Thi
s m
edici
ne m
ust n
ot b
e gi
ven
to c
hild
ren
or te
enag
ers.
Sto
rage
: Kee
p th
is m
edici
ne o
ut o
f the
sig
ht a
nd re
ach
of c
hild
ren.
Sto
re b
elow
30°
C.
This
leafl
et w
as la
st re
vised
in J
uly
2012
.

All Modern Medicine are submitted to a revolving random sample of doctors in the Middle East and are rated for their interest of reading. Only articles rating over 65% are published, highest rating articles are published as CME.
THE MULTIDISCIPLINARY PEER-REVIEWED CONTINUING MEDICAL EDUCATION JOURNAL
ARTICLESVOLUME 33 | NUMBER 02 | QUARTER 2 - 2016
Contents
31
In collaboration with
Jeddah Primary Care CME unit
04
13
22
MIDDLE EAST REVIEW
BEST OF CME 2015
Ludwig’s Angina A Life Threatening Emergency
Ludwig’s angina is a potentially life threatening condition which is a known but rare condition. It involves spreading infection of the floor of mouth – sublingual space to the submaxillary space and progressing into the deeper neck spaces
leading to trismus, dysphagia, airway compromise etc.
Acute Otitis Media in Young Children Diagnosis and Management
Acute otitis media is one of the most common reasons children are prescribed antibiotics. However, it is notoriously difficult to diagnose with certainty in infants and young children and management, especially when to use antibiotics, has
been controversial. Updated guidelines may help resolve these problems.
Investigation and Management of Recurrent Urinary Tract infection
Recurrent urinary tract infections are common in women; after investigations to exclude common predisposing causes and complications, the focus is on strategies to prevent recurrence. In children and men, there is a higher index of
suspicion for an underlying cause and further investigation is usually needed.
Medical Management After Control of Myocardial Ischaemia
After recovery from myocardial infarction, patients should receive aspirin and statin therapy and be evaluated regarding their need for coronary revascularisation,
additional pharmacological treatment and possible device therapy.

JEDDAH PRIMARY CARE CME UNIT
In collaboration with
CONTINUING MEDICAL EDUCATION
This is a CME (Continuing Medical Education) article. It is presented to you in collaboration with the Middle East CME organizations. Self-test answers will be published in two months.
1CREDIT HOUR
4 | Quarter 2 - 2016 | Volume 33 | MODERN MEDICINE
• Diagnosis of acute otitis media (AOM) can be challenging in infants and children because of factors such as poor compliance with examination and inconclusive signs.
• A reddened tympanic membrane alone is not sufficient for diagnosis; a cloudy, bulging membrane with reduced mobility on pneumatic otoscopy combined with a typical clinical history is pathognomonic of AOM.
• Antibiotic treatment is recommended for children with AOM aged 6 months or younger, those aged over 6 months with otorrhoea or severe symptoms, those aged between 6 and 24 months with bilateral AOM and those whose follow up is uncertain or difficult.
• Observation and follow up after 24 to 48 hours is an option for some children aged over 6 months who meet specific criteria.
• Specialist referral is warranted for persisting or recurrent disease, complications or concerns about speech and language.
IN SUMMARY
JOHN M. WOODMB BS, MSurg
Dr Wood is a Registrar in Otolaryngol-ogy in the Department of Otolaryngol-ogy, Head and Neck Surgery, Princess Margaret Hospital For Children, Univer-sity of Western Australia, Perth, WA.
SHYAN VIJAYASEKARANMB BS, FRACS
Professor Vijayasekaran is an Otolaryn-gologist and Clinical Associate Professor in the Department of Otolaryngology, Head and Neck Surgery, Princess Mar-garet Hospital For Children, University of Western Australia, Perth, WA.
There is little doubt that acute otitis media (AOM) is one of the most common inflammatory diseases in childhood. It is a major cause of morbidity in children and one of the most common reasons children are prescribed antibiotics.
However, diagnosis of AOM can be difficult as symptoms and signs are not necessarily definitive and physical examination can be challenging in this age group. In addition, management of AOM has been widely debated, with
Acute Otitis Media in Young ChildrenDiagnosis and ManagementAcute otitis media is one of the most common reasons children are prescribed antibiotics. However, it is notoriously difficult to diagnose with certainty in infants and young children and management, especially when to use antibiotics, has been controversial. Updated guidelines may help resolve these problems.

CONTINUING MEDICAL EDUCATION
MODERN MEDICINE | Volume 33 | Quarter 2 - 2016 | 5
most commonly implicated in upper respiratory tract infections and most frequently isolated from middle ear effusions in AOM (Table 1).12,13
Viruses also appear to have a role. AOM is typically preceded by a viral infection of the upper respi-ratory tract, most commonly due to respiratory syncytial virus; other common causes include influenza viruses, parainfluenza viruses, rhi-noviruses and adenoviruses. A role for viruses in the pathogenesis of AOM is further supported by the results of a randomised controlled trial of the early use of oseltamivir in influenza. The incidence of AOM development during the influenza illness was decreased by 85% in children who commenced oselta-mivir within 12 hours of the onset of influenza symptoms.14
There is further evidence of a virus–bacterial interaction in AOM. The presence of the respiratory viruses rhinovirus and adenovirus in the
numerous different treatment guidelines in the published litera-ture.1-4 The use of these guidelines is further complicated by confu-sion between the categories of otitis media. Overdiagnosis of AOM is believed to be common, leading to the inappropriate use of antibiotics, which promotes anti-biotic resistance and unnecessarily increases the risk of side effects.
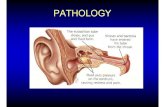
DEFINITIONS OF OTITIS MEDIAOtitis media is a collective of infec-tive or inflammatory disorders of the middle ear. It has been described as a continuum, ranging from AOM and recurrent AOM through to otitis media with effusion and chronic suppurative otitis media, and can have a significant impact on hearing.5,6 The categories of otitis media are defined in the box.6
EPIDEMIOLOGYTwo-thirds of children will have an episode of AOM by their third birth-day, and around half will have three or more episodes. The incidence of AOM is highest in the first two years of life.7 There is a peak in incidence in babies aged under 1 year, with a further peak around age 5 years.6 In the community, AOM is one of the most common reasons for children under 5 years of age both to present to a doctor and to be prescribed antibiotics.8 The burden to the com-munity is significant, with a recent survey showing that more than 50% of parents with children diagnosed with AOM have to take time off work.8
It has been well documented that certain populations have a much higher incidence of AOM and otitis media with effusion. Aboriginal children have the highest published
prevalence of AOM in the world, with a study of around 700 children showing that nearly 91% had some form of otitis media. Of these, nearly a third were classified as having AOM.9 This study was conducted in 29 remote communities before the introduction of the seven-valent pneumococcal conjugate vaccine, which has reduced the incidence of AOM.10 Nevertheless, the incidence of ear disease in the Aboriginal popula-tion, and in indigenous communities worldwide, remains much higher than in the general population.
AETIOLOGYThe pathogenesis of AOM is mul-tifactorial, involving a complex interaction between microbial agents, host immune response, cell biology of the middle ear and nasopharynx and environmental factors.11 The bacteria Haemophilus influenzae, Streptococcus pneumoniae and Moraxella catarrhalis are those
CATEGORIES OF OTITIS MEDIA*
Acute otitis media (AOM): Infection of the middle ear with acute onset, middle ear effusion and signs of inflammation
Recurrent AOM: At least three episodes of AOM in six months, or four episodes in 12 months
Otitis media with effusion: A middle ear effusion without signs of acute infection or inflammation (‘glue ear’)
Chronic suppurative otitis media:Continuing inflammation in the middle ear leading to otorrhoea and perforation of the tympanic membrane
* Adapted from Birman C. Med Today 2005; 6(8):14-22.6
TABLE 1. BACTERIA ISOLATED FROM CHILDREN WITH ACUTE OTITIS MEDIA*
Bacterium % of cases
Haemophilus influenzae 57%
Streptococcus pneumoniae 31%
Moraxella catarrhalis 5–10%
Group A streptococci 2%
Staphylococcus aureus 1%
Pseudomonas aeruginosa 1%
* Modified from Qureishi A, et al. Infect Drug Resist 2014; 7: 15-2412 and Coker TR, et al. JAMA 2010; 304: 2161-2169.13

CONTINUING MEDICAL EDUCATION
6 | Quarter 2 - 2016 | Volume 33 | MODERN MEDICINE
nasopharynx in asymptomatic children has been associated with the detection of M. catarrhalis.15
Further studies in an Indigenous population suggested that a virus–bacterial interaction led to more severe symptoms.16 In addition, studies in animal models found an increased load of H. influenzae in the nasopharynx after nasopharyngeal inoculation with respiratory syncytial virus. Infection of the airway has been proposed to downregulate expression of β-defensin, an anti-microbial peptide implicated in the resistance of epithelial surfaces to microbial colonisation.17 In addition, Sendai virus co-infection with S. pneumoniae and M. catarrhalis was noted to increase the incidence and duration of AOM and bacterial load.18
FACTORS INFLUENCING AOM INCIDENCEAge and other biological factorsThe most important risk factor for AOM is young age, with the high-est incidence of the condition in the first two years of life.7 This may be partly explained by the anatomy of the Eustachian tube, which is shorter, more horizontal and more compliant at this age than in older children and adults. Other factors that may play a role include the limited immunologi-cal response to antigens in this age group, cessation of breastfeeding and increased exposure to environmental pathogens.19 The role of the latter is supported by the second peak of incidence, which occurs at around 4 to 5 years of age, when children typically begin to attend preschool.5
Children with recurrent AOM are slightly more likely to be male and to have ceased breastfeeding before
the age of six months.20 Recurrent AOM is also increased in patients with immune deficiencies and in those with craniofacial disorders (including cleft palate) and Down syndrome, possibly because of Eustachian tube dysfunction.21
Genetic factors may also have a role in susceptibility to otitis media.21,22 Twin and triplet studies have shown a substantial heritable component to the clinical spectrum of otitis media.23
Pneumococcal immunisationThe use of the seven-valent pneu-mococcal vaccine has reportedly reduced the risk of AOM by up to 34%, but little information has been published as yet on the further impact of the 13-valent vac-cine.10 There is, however, evidence that pneumococcal vaccination may allow nonvaccine serotypes of S. pneumoniae to increase in prevalence, as they did in the USA.24 Nevertheless, there has been a reduction in the incidence of
pneumococcal diseases overall and otitis media has become a milder condition since the introduction of the pneumococcal vaccine together with the H. influenzae vaccine.25,26 Furthermore, studies show that H. influenzae is now the most common-ly isolated organism in the middle ear of children with recurrent AOM.27
Environmental factorsIt is well documented that children attending daycare are significantly more likely to develop AOM. A study of more than 600 children found that those who attended daycare had more than twice the odds of having an ear infection in the preceding week.20 Interestingly, the same study failed to demon-strate an increased incidence of AOM in children with increased m e a s u re s o f o v e rc ro w d i n g . Nevertheless, low socioeconomic status and overcrowding are often documented as risk factors for AOM.5 Overcrowding facilitates the transmission of upper respiratory
TABLE 2. SYMPTOMS OF ACUTE OTITIS MEDIA AND SENSITIVITY AND SPECIFICITY FOR DIAGNOSIS*
Symptoms Sensitivity (%) Specificity (%)
Common symptoms
Otalgia 54 82
Pulling/tugging of ear 42 87
Fever 40 48
Irritability 55 69
Other symptoms
Otorrhoea – –
Vomiting 11 89
Anorexia 36 66
Diarrhoea – –
Lethargy – –* Adapted from Coates HL. Med Today 2001; 2(11): 42-525 and Pichichero ME. Pediatr Clin N Am 2013; 60: 391-407.30

CONTINUING MEDICAL EDUCATION
MODERN MEDICINE | Volume 33 | Quarter 2 - 2016 | 7
tract infections, the most frequent risk factor for AOM.5
In addition, a multivariate analysis of factors related to otitis media showed that maternal smoking increases the infant ’s r isk of otitis media more than ninefold, and paternal smoking more than sixfold.20
Seasonal variationThere is some evidence that the incidence of AOM may be highest in autumn and winter, and lowest in summer.28 It is also suggested that children born in autumn may be more susceptible to recurrent AOM as they are exposed to winter pathogens during their most vul-nerable months.
Indigenous statusAs discussed above, the rate of AOM and chronic suppurative otitis media is significantly higher in the Aboriginal population than in the general population.
DIAGNOSISRecent guidelines from the American Academy of Pediatrics emphasise the importance of accurate diagnosis of AOM for clinical decision-making and also for providing the framework for high quality research.2 Overdiagnosis leads to overtreatment, with the risks of antibacterial resistance and medication side effects such as skin rash and diarrhoea. Underdiagnosis may delay adequate treatment and potentially increase the risk of complications.However, diagnosis of AOM may be difficult as there are no definitive symptoms and no ‘gold standard’ for diagnosis. Signs can cover a spectrum as the disease progresses.
An erythematous tympanic mem-brane together with otalgia have been regarded as indicating AOM, but only 40% of children with these features actually have AOM.5 In addition, otoscopy is recognised as one of the most technically difficult tasks to perform in young children.A recent systematic review recom-mended three main criteria that need to be met for a diagnosis of AOM:• acute symptoms of infection• evidence of middle ear inflamma-
tion, such as tympanic membrane erythema
• presence of middle ear effusion.13
Requirements of Australian guide- lines are similar.29 This approach provides a simple framework for diagnosis, but clinical practice can be more complicated.
Symptoms of AOMTypical symptoms associated with AOM and their sensitivity and specificity for diagnosis are shown in Table 2.5,30 A systematic review found that otalgia had the high-est predictive value for diagnosis of AOM but was present in only 50 to 60% of cases.31 Not only may specific ear symptoms be absent but they may also fail to be recog-nised by parents, particularly in very young children.32
Evidence suggests that symptoms such as restless sleep, ear rubbing, fever, and nonspecific respiratory or gastrointestinal tract symptoms are not able to differentiate children with and without AOM. For example, a questionnaire survey of 469 par-ents who suspected their child had AOM based on symptoms found that fewer than half actually had AOM, based on strict otoscopic cri-teria.33 The time course of symptoms
is important, with AOM typically hav-ing a short history.
OtoscopySimilarly, diagnosing AOM based on otoscopic signs can be difficult in children. Otoscopy requires patience, a compliant child and a parent con-fident enough to adequately restrain their child if required.34 Furthermore, in nearly 80% of children under the age of 12 months, the tympanic membranes are either partially or totally obscured by wax, hindering accurate diagnosis.35
Otoscopy can be more fruitful if the child is positioned on the parent’s lap, with one of the parent’s arms restraining the child’s shoulder and the other arm holding the child’s head against the parent’s chest.If wax is present, it can be removed in a compliant child with a wax curette or with the help of topical preparations.
Distinguishing AOM from other forms of otitis mediaAOM is differentiated from otitis media with effusion and chronic suppurative otitis media based on history and examination find-ings.12 Differentiating AOM from otitis media with effusion enables unnecessary antibiotic treatment to be avoided. Typically, as AOM is a purulent middle ear process, signs and symptoms consistent with acute inflammation should be present.The American Academy of Pediatrics guidelines state that AOM should be diagnosed in:• children with moderate to severe
bulging of the tympanic mem-brane and new-onset otorrhoea in the absence of otitis externa
• children with mild bulging of the tympanic membrane and

CONTINUING MEDICAL EDUCATION
8 | Quarter 2 - 2016 | Volume 33 | MODERN MEDICINE
clear ear canal. The best predictor of AOM is a cloudy, bulging tym-panic membrane. Although there is evidence that a distinctly red, haemorrhagic tympanic membrane may indicate AOM, only 40% of children with this sign have AOM.32 The addition of pneumatic otos-copy increases the accuracy of AOM diagnosis, but lack of access to adequate equipment and lack of education and skills may hinder the use of this technique.
MANAGEMENTControversy about managementThe rapid increase in antibiotic resistance and major contribution of AOM to antibiotic prescription in children has prompted concern about the accuracy of AOM diag-nosis and inappropriate prescribing of antibiotics. Treatment of AOM also remains controversial, with dif-ferent national guidelines around the world.1-4 Typically, AOM follows a relatively benign course in the absence of antibiotic treatment, with symptomatic rel ief with analgesia and antipyretics alone. A recent meta-analysis showed that nearly 80% of children had sponta-neous relief within two to 14 days.12 However, in children younger than 2 years the corresponding percentage is estimated at around 30%.Because of the high rates of sponta-neous resolution of AOM, the use of antimicrobials has been questioned, with a recent Cochrane review finding only a modest reduction in symptoms with use of antimicrobi-als.38 However, closer analysis of the studies included in this review identi-fied issues with both the populations and diagnosis of AOM. Children with severe symptoms were specifically
recent-onset otalgia or intense erythema of the tympanic mem-brane (Figure 1a).2
A recent systematic review con-firmed that otoscopic findings of middle ear inflammation, effusion and a bulging tympanic membrane are positive predictors of AOM.13
The presence of a ‘cloudy’ bulging tympanic membrane with impaired mobility on pneumatic otoscopy (discussed below) is considered the best predictor of AOM.2 A bulg-ing tympanic membrane is also highly correlated with the finding of a bacterial pathogen on tympa-nocentesis: middle ear fluid from children with a bulging tympanic membrane alone yielded a positive bacterial culture in 75% of cases, increasing to 80% if the tympanic membrane was discoloured to yel-low.36 The absence of middle ear fluid excludes AOM.In the presence of the above symp-toms and signs, the diagnosis of AOM is almost unequivocal, but in their absence, the diagnosis can be difficult to make with any certainty. The addition of pneumatic otoscopy to assess the mobility of the tym-panic membrane increases the
accuracy of AOM diagnosis, with a sensitivity of over 90% and specificity of nearly 80%.32 In this technique, positive and negative pressure is applied to the tympanic membrane in the presence of a well-formed seal between the speculum and the external auditory meatus. Mobility of the tympanic membrane is typically decreased or absent in the presence of a middle ear effusion. This test cannot differentiate AOM from otitis media with effusion (Figure 1b), but its use together with clinical history and other examination results can help diagnosis.Nevertheless, a study using video otoendoscopic images found that the ability of different doctor groups to differentiate AOM from otitis media with effusion varied. A correct diagnosis was made by otolaryngologists 70% of the time, by paediatricians 50%, and by GPs 45%.37 In addition, there is evidence AOM may be overdiagnosed clini-cally in more than 30% of children.32
In summary, diagnosis of AOM should be based on clinical history and careful evaluation of the tym-panic membrane, using adequate illumination in the presence of a
FIGURE 1A AND B. OTOSCOPIC VIEW IN PATIENTS WITH (A, LEFT) ACUTE OTITIS MEDIA, SHOWING A REDDENED BULGING TYMPANIC MEMBRANE, AND (B, RIGHT) OTITIS MEDIA WITH EFFUSION, SHOWING A FLUID LEVEL.

CONTINUING MEDICAL EDUCATION
MODERN MEDICINE | Volume 33 | Quarter 2 - 2016 | 9
It is important to note that these guidelines are not appropriate for Aboriginal and Torres Strait Islander people, who should commence antibiotic treatment in all cases.40
What antibiotics should be used?Bacterial resistance is a significant concern and an increasing clinical problem in AOM. Although some strains of H. influenzae and M. catarrhalis are resistant to amoxy-cillin through their production of beta-lactamase, this can typically be overcome by including a beta-lac-tamase inhibitor such as clavulanic acid in the treatment regimen. The prevalence of antibiotic-resistant S. pneumoniae and beta-lactamase producing H. influenzae is influenced by patient age, recent exposure to antibiotics, attendance at daycare and pneumococcal immunisation. A study reported penicillin resistance in nearly half of all nasopharyngeal isolates of these two bacteria.12
First-line antibiotics for AOM include:• amoxycillin (50 to 60 mg/kg per
day in two or three doses), unless the child has received this antibio-tic in the previous month
• cefuroxime (30 mg/kg per day in two divided doses) as an alternative
• in the case of penicillin allergy, erythromycin (30 to 50 mg/kg
excluded but are the group most likely to require antibiotics. Secondly, in a number of the studies only a minority of children had a bulging tympanic membrane, a clinical sign previously discussed as being impor-tant in the diagnosis of AOM.
Antibiotic treatmentWho should be treated with antibiotics?Currently, guidelines appear to be unanimous in recommending antibiotic treatment for children aged 6 months or younger with AOM.2,29
The American Academy of Pediatrics updated their guidelines in 2013, rec-ommending that antibiotics should also be given to children older than 6 months with evidence of AOM if:2,10
• they have otorrhoea or• they have severe symptoms or• they are aged between 6 months
and 2 years and have bilateral AOM or
• follow up is uncertain or difficult.The role of observation, with fol-low up after 24 to 48 hours, for the management of AOM is limited to:2,10
• children older than 2 years who do not have otorrhoea or severe symptoms
• children aged between 6 months and 2 years who do not have
otorrhoea or severe symptoms and have only unilateral AOM.
Australian guidelines recommend that in the absence of systemic features such as fever, antibiotic therapy be delayed in children over the age of 6 months.29 Review is recommended after 24 hours in children aged between 6 months and 2 years and after 48 hours in childen older than 2 years, with antibiotics typically prescribed if there has been no improvement.Reportedly, for every 100 healthy children with AOM, 80 will improve within three days without antibiotic therapy, compared with 92 if treat-ed with amoxycillin.38 Of those 100 children treated with the antibiotic, reportedly 10 would develop a rash and 10 would develop diarrhoea.39
Consequently, the prescription of antibiotics is not without risk.The fear of developing a complica-tion of AOM, such as mastoiditis, is thought to prompt the prescrip-tion of antibiotics; however, 4800 children must be treated to prevent one case of mastoiditis. Additionally, the recommended follow up after 24 to 48 hours would identify patients who are not improving. Therefore, with adequate assessment and fol-low up such cases should be rarer.
TABLE 3. AMERICAN ACADEMY OF PEDIATRICS TREATMENT RECOMMENDATIONS FOR ACUTE OTITIS MEDIA (2013)*
Age of child AOM with otorrhoea AOM without otorrhoea AOM with severe symptoms
Unilateral Bilateral Unilateral Bilateral Unilateral Bilateral
0 to 6 months Antibiotics Antibiotics Antibiotics Antibiotics Antibiotics Antibiotics
6 months to 2 years Antibiotics Antibiotics Antibiotics or observation
Antibiotics Antibiotics Antibiotics
Over 2 years Antibiotics Antibiotics Antibiotics or observation
Antibiotics or observation
Antibiotics Antibiotics
ABBREVIATION: AOM = acute otitis media. * Adapted from Lieberthal AS, et al. Pediatrics 2013; 131: e964-e9992 and Dickson G. Prim Care 2014; 41: 11-18.10

CONTINUING MEDICAL EDUCATION
10 | Quarter 2 - 2016 | Volume 33 | MODERN MEDICINE
than 4 years of age with otitis media with effusion.43 The role of adenoid-ectomy together with the insertion of ventilation tubes has been con-troversial, with some studies noting benefits in only some subgroups.28 A 2014 meta-analysis suggested that children with otitis media with effusion who also underwent ade-noidectomy had a greater chance of clinical improvement.43
CONCLUSIONAlthough AOM typically presents with a set of distinct diagnostic features, diagnosis can be challen-ging in infants and young children because of poor compliance with examination, anatomical features and inconclusive signs. A reddened tympanic membrane alone is not sufficient for a diagnosis of AOM, but a cloudy, bulging membrane with pneumatic otoscopic features consistent with effusion on the back-ground of a typical clinical history is pathognomonic of the disease.Nevertheless, overdiagnosis is com-mon, with evidence that nearly a third of all AOM diagnoses are in fact otitis media with effusion.30
This leads to the inappropriate use of antibiotics, with the accompany-ing problem of increased bacterial resistance. The rate of spontaneous resolution in AOM is high, but a careful examination is required for diagnosis, along with adequate symptomatic support. Further management should be decided in conjunction with the parent, par-ticularly if observation is chosen as initial management.
ReferencesA list of references is available on request to the editorial office.
Consequently, referral to an otolaryn-gologist is recommended for children who have recurrent episodes of AOM or persisting effusion.10 Earlier referral is recommended for children with speech and language delay, cognitive delay or craniofacial abnormalities affecting middle ear and Eustachian tube function. Emergent referral is recommended in patients who have suspected complications such as mastoiditis, facial paralysis, labyrin-thitis, meningitis or brain abcess.5 In addition, children with a chronically discharging ear should be referred for further management and examina-tion for suspected cholesteatoma.6
Further management optionsOptions for further management by an otolaryngologist include a formal assessment of hearing and insertion of ventilation (tympa-nostomy) tubes, either alone or in conjunction with adenoidectomy. A Cochrane review noted that the number of patients free from acute otitis media in the included studies was higher in those with ventila-tion tubes.41 There is also significant evidence of short-term improve-ment in quality of life with the insertion of ventilation tubes. Their role in preventing recurrent AOM is still debated, particularly given the difficulty surrounding inclusion criteria for randomised controlled trials.42 Consequently, the American Academy of Otolaryngology Head and Neck Surgery clinical practice guidelines currently recommend ventilation tubes in children who have recurrent AOM and an effu-sion at the time of assessment.42
A recent meta-analysis found a benefit for adenoidectomy in children under 2 years of age with recurrent AOM and in those older
per day in three divided doses) or clarithromycin (15 mg/kg per day in two divided doses).
For treatment failure, second-line antibiotics include:• amoxycillin plus clavulanic acid (22.5 + 3.2 mg/kg three times per day)
• clindamycin (30 to 40 mg/kg per day in three doses)
• a third-generation cephalosporin, such as ceftriaxone 50 mg/kg per day intramuscularly or intravenous-ly, particularly if amoxycillin has been used in the previous 30 days.2
Adults are nearly 20 times less likely to develop AOM than children; their management should follow similar principles to those used in children.
AnalgesiaAnalgesia is an important part o f AO M m a n a g e m e n t , a n d under-reported in the literature. Paracetamol or NSAIDs can be used for pain relief. This may be required for up to seven days despite antibiotic treatment. Other oral medications (such as antihistamines) and decongestants have little evi-dence to support their use but a five to eight times increase in the risk of side effects.10
SPECIALIST REFERRALWhen to referAlthough most episodes of AOM resolve, it is important to recog-nise when to refer children to an otolaryngologist. Even after an uncomplicated episode of AOM, there is a possibility of developing recurrent AOM or a persisting mid-dle ear effusion. Such an effusion is recognised in 63% of children after AOM at two weeks, 40% at one month, and 26% at three months.6 After three months, the likelihood of this effusion resolving is reduced.

CME QUESTIONS
JEDDAH PRIMARY CARE CME UNIT
In collaboration with
MODERN MEDICINE | Volume 33 | Quarter 2 - 2016 | 11
This is a CME (Continuing Medical Education) article. It is presented to you in collaboration with the Middle East CME organizations. Self-test answers will be published in two months.
Case study 1. Bella’s mother has brought her to see you because Bella ‘has another ear infection’. Bella is 3 years old.
QUESTION 1. Which two of the following statements about the epidemiology of acute otitis media are correct?
A. The incidence is the highest in the first seven years of life
B. Aboriginal children have an increased prevalenceC. Parental smoking increases the riskD. It is far more common in girls than boys
Case study 1 (continued). Last night Bella started crying and tugging at her right ear. She and her older sister have both recently had runny noses. You wish to check for possible acute otitis media and try to examine Bella’s tympanic membrane.
QUESTION 2. List at least three factors that can affect your ability to diagnose acute otitis media in young children.
QUESTION 3. Middle ear effusion is one of three recommended criteria that need to be met for a diagnosis of acute otitis media. Which two of the following are the other criteria?
A. Acute symptoms of infectionB. FeverC. Evidence of middle ear inflammationD. Otalgia
Case study 1 (continued). Otoscopy shows that Bella’s tympanic membrane is reddened but you are unable to visualise it well enough to determine whether it is bulging, indicating a middle ear effusion.
QUESTION 4. Which one of the following techniques is recommended in addition to otoscopy to help detect a middle ear effusion in a patient such as Bella?
A. AudiologyB. TympanostomyC. TympanocentesisD. Pneumatic otoscopy
Case study 1 (continued). On further examination you detect signs of a middle ear effusion and diagnose acute otitis media. You consider how to treat Bella. Her family are not Indigenous.
QUESTION 5. Which three of the following patient groups with acute otitis media should be treated with antibiotics according to the current guidelines of the American Academy of Pediatrics?
A. All children under 12 months of ageB. All children with severe symptomsC. All children who may be lost to follow upD. Children aged between 6 months and 2 years
with bilateral infection
ACUTE OTITIS MEDIA IN YOUNG CHILDRENDIAGNOSIS AND MANAGEMENTSECTION A.

CME QUESTIONS
12 | Quarter 2 - 2016 | Volume 33 | MODERN MEDICINE
Case study 1 (continued). You explain the likely course of acute otitis media and the pros and cons of antibiotic treatment to Bella’s mother.
QUESTION 6. What should you tell Bella’s mother about the likely course of acute otitis media?
Case study 1 (continued). You recommend that Bella’s mother treat her with paracetamol and then bring her back for review.
QUESTION 7. What is the recommended interval before review in a child with acute otitis media such as Bella who is not treated initially with antibiotics? Select one of the following.
A. 24 hoursB. 48 hoursC. One weekD. Two weeks
Case study 2. Joshua, aged 5 months, has been crying all night and refusing to feed. He is still inconsolable and has a low-grade fever when his mother brings him to see you today. After examining him, you make a diagnosis of acute otitis media. Given his age, you prescribe an antibiotic.
QUESTION 8. List at least two antibiotics used for the first-line treatment of patients with acute otitis media.
Case study 2 (continued). Joshua does not respond to the initial antibiotic you prescribed. You consider his further treatment.
QUESTION 9. Which three of the following are recommended second-line antibiotics to treat acute otitis media in the case of treatment failure?
A. Amoxycillin plus clavulanic acidB. Doxycycline C. Ceftriaxone D. Clindamycin
Question 10. Before prescribing an antibiotic, how do you ascertain whether a patient has any drug allergies? Select as many answers as you think appropriate.
A. Reading the patient recordB. Asking the patient C. Asking the patient’s carerD. Other – please write the strategies you use
SECTION B.
MM
ME
ad u
pdat
ed-0
8/20
14
MIDDLE EAST
MODERNMEDICINE
THE MULTIDISCIPLINARY PEER-REVIEWED CONTINUING MEDICAL EDUCATION JOURNAL
15,100 Doctors as a BOOK26,300 Doctors by EMAIL
MAGAZINE&
Stay updated with Modern Medicine
in the Middle East
SEEN BY
ELECTRONIC












![Acute and Chronic Otitis Media[1]](https://static.fdocuments.net/doc/165x107/577d2ca91a28ab4e1eac8be8/acute-and-chronic-otitis-media1.jpg)