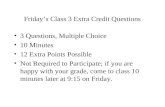
Cing$*- 16#-* · present Friday’s keynote address at the 2015 AMDA annual conference in March,...
Transcript of Cing$*- 16#-* · present Friday’s keynote address at the 2015 AMDA annual conference in March,...

January 2015 • vol. 16, no. 1 www.Caringfortheages.com
for the Agesfor the Ages A Monthly Newspaper for Long-Term Care Practitioners
™
In This Issue
Caring an offiCial PubliCation of aMDa – the SoCiety for PoSt-aCute anD long-terM Care MeDiCine
Give OR Get the Gift of Joy, Support and Recognition!
The 2015 Caring Canines Calendar is Here!
www.amdafoundation.org/canines
Three large international studies addressing sodium intake’s effect on blood
pressure and on cardiovascular and mortality outcomes are un-likely to quell the controversy surrounding sodium. Rather, since the findings of one study
directly oppose those of the other two, the results promise to fan the flames a bit higher.
All three studies were reported in the New England Journal of Medicine.
PURE SubstudyThe first report concerned a substudy of data from the
Prospective Urban Rural Epidemiology (PURE) study involving 102,216 adults aged 35-70 years residing in 667 com-munities in 18 low-, middle-, and high-income countries worldwide. Urinary sodium and potassium levels were used as surrogates for dietary intake of these elements, and these
excretion levels were correlated with the participants’ BP levels, said Andrew Mente, PhD, of the Population Health Research Institute, Hamilton (Ontario) Health Services, McMaster University, and his associates.
Current guidelines recom-mend a maximum sodium intake of 1.5-2.4 g per day, depending
on the country. Only 0.6% of the study population achieved the lowest level of 1.5 g per day, the level recommended in the United States, and only 10% achieved less than 3 g per day. The largest segment of the study population, 46%, had a
In a recent New York Times edito-rial (“Too Young to Die, Too Old to Worry,” Sept. 20, 2014), author, educa-
tor, and physician Jason Karlawish, MD, presented a thought-provoking question: “When should we set aside a life lived for the future, and instead embrace the plea-sures of the present?” He then offered an interesting idea: “A national invest-ment in communities and services that improve the quality of our aging lives might help us to achieve this. Instead of Death Panels, we can start talking about Pleasure Panels.” Dr. Karlawish, who will present Friday’s keynote address at the 2015 AMDA annual conference in March, told Caring for the Ages: “This issue is significant for long-term care practitio-ners, as they are on the front line with patients who face multiple risks while considering the lingering question of how much time they have left.”
The issue of prognosis – what is to be gained or lost depending on various inter-ventions and treatments – “looms large” for geriatrics practitioners, Dr. Karlawish observed. “How to talk about the many risks patients face is a necessary skill.” Practitioners, he suggested, need to be able to juggle truth, hope, and kindness at the same time.
There is no script for a successful con-versation. However, Dr. Karlawish starts with a simple question: What’s a typical day for you? “Much can be gained from the answer to this. You can use this infor-mation as concrete data to understand what works and what doesn’t work for
patients and what you can do to improve their qual-ity of life,” he said. For example, “If they tell you that their days are filled with doctors’ appoint-ments, this presents an opportunity to find a way to free more of their time for activities they enjoy.”
Dr. Karlawish asks fam-ily members this ques-tion even when a patient has advanced dementia. “This is a good way to focus on what is pleasant for the patient,” he said. For example, a family member may say, “Dad wouldn’t want to be in adult day care and listen to music or do arts and crafts all day.” However, as the practitioner talks with the family, he or she can help them realize that dad has changed as he’s become more ill, and he might enjoy those things now.
“We need to focus on what gives pleasure now in the present,” Dr. Karlawish said. This can be a challenge, but it’s an impor-tant one, he added. “When individuals have dementia, their lives – their very selves – are constructed by the people around them. We shape their person-hood, and that is a tremendous moral responsibility.”
Often, families and other caregivers think they are doing the right thing for their loved ones by imposing bur-densome treatments or interventions, Dr. Karlawish said. He shared the story of a man with moderate dementia whose
Keynoter Puts Patient Pleasure FirstBy Joanne Kaldy
By MaRy ann Moon
Sodium Controversy: More Fuel for the Fire
Jason Karlawish will present the keynote address at the AMDA annual conference in March.
Dear Dr. JeffDoes legalized marijuana have a place in the nursing home? ... 3
Looking Forward to 2015Caring for the Ages editorial advisers predict the major issues they expect to arise this year in the field of post-acute/long-term care. ............................... 4
Legal IssuesA concise CPR policy can prevent serious state survey citations and helps honor residents’ end-of-life wishes. .... 8
Antipsychotic AlternativeRecent research shows a combination drug reduces aggression and agitation in patients with Alzheimer’s. ....... 9
See More Fuel • page 7
See Pleasure • page 6
Ph
ot
o c
ou
rt
es
y o
f J
as
on
Ka
rl
aw
ish

2 • CARIng FoR The AgeS JAnuARy 2015
Caring for the Ages ™
Editor in Chief Karl Steinberg, MD, CMD
Editorial advisory Board
Chair: Karl Steinberg, MD, CMD, California
Robin Arnicar, RN, West Virginia
Nicole Brandt, PharmD, CGP, BCPP, FASCP, Maryland
Ian L. Cordes, MBA, Florida
Jonathan Evans, MD, CMD, Virginia
Janet Feldkamp, RN, JD, BSN, Ohio
Robert M. Gibson, PhD, JD, California
Daniel Haimowitz, MD, FACP, CMD, Pennsylvania
Linda Handy, MS, RD, California
Jennifer Heffernan, MD, CMD, Texas
Bill Kubat, MS, LNHA, South Dakota
Jeffrey Nichols, MD, New York
Dan Osterweil, MD, CMD, California
Barbara Resnick, PhD, CRNP, FAAN, FAANP, Maryland
Dennis L. Stone, MD, CMD, Kentucky
AMDA headquarters is located at 11000 Broken Land Parkway, Suite 400, Columbia, MD 21044.
Caring for thE agEs is the official newspaper of AMDA – The Society for Post-Acute and Long-Term Care Medicine and provides long-term care professionals with timely and relevant news and commentary about clinical developments and about the impact of health care policy on long-term care. Content for Caring for thE agEs is provided by AMDA and by Elsevier Inc.
The ideas and opinions expressed in Caring for thE agEs do not necessarily reflect those of the Association or the Publisher. AMDA and Elsevier Inc., will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services mentioned herein.
©2015 AMDA – The Society for Post-Acute and Long-Term Care Medicine.
Caring for thE agEs (ISSN 1526-4114) is published monthly by Elsevier Inc., 360 Park Avenue South, New York, NY 10010. Business and Editorial Offices: Elsevier Inc., 360 Park Avenue South, New York, NY 10010. Accounting and Circulation Offices: Elsevier Health Sciences Division, 3251 Riverport Lane, Maryland Heights, MO 63043. Periodicals postage paid at New York, NY and additional mailing offices.
POSTMASTER: Send change of address to Caring for thE agEs, Elsevier, Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043. Subscription price is $219.00 a year (individual).
Editorial offiCEs 1600 JFK Blvd., Suite 1800, Philadelphia PA, 19103, 215-239-3900, fax 215-239-3990. Letters to the Editor: [email protected]
Editorial staff
Managing Editor Carey Cowles
Senior Contributing Writer Joanne Kaldy
Social Media Editor Lindsey Neal, MD
Display Sales Manager Carol Clark 212-633-3719, [email protected]
Classified Advertising Adam Moorad 212-633-3122, [email protected]
Customer Service Orders, claims, online, change of address: Elsevier Periodicals Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043; telephone (800) 654-2452 (United States and Canada), (314) 447-8871 (outside United States and Canada); fax: (800) 225-4030 (United States and Canada), (314) 447-8029 (outside United States and Canada); e-mail: [email protected] (for print support); [email protected] (for online support). Address changes must be submitted four weeks in advance.
BERLIN – Chronic use of benzodiaz-epines by elderly patients is associated with a 43%-51% increased risk of being diagnosed with Alzheimer’s disease 5-10 years later, according to a large case-control study. “Considering the extent to which benzodiazepines are prescribed in the elderly population and the growing incidence of demen-tia, unwarranted chronic use of ben-zodiazepines in the elderly should be viewed as a public health issue,” Sophie Billioti de Gage said at the annual congress of the European College of Neuropsychopharmacology.
Her case-control study used the Quebec health insurance database. The subjects were 1,796 elderly individuals
diagnosed with Alzheimer’s disease, each matched with four controls based upon age, gender, and duration of follow-up. The Quebec database permitted identi-fication of all subjects with prescriptions for benzodiazepines during 2000-2009, a period 5-10 years prior to diagnosis of Alzheimer’s disease. This substantial time lag was chosen because previous studies reporting a link between ben-zodiazepines and dementia have often been criticized for possible confounding due to reverse causality. That is, because many earlier studies featured a shorter interval between medication use and dementia diagnosis, skeptics argued that benzodiazepines might not have caused the dementia, but rather were prescribed to treat early manifestations of the disease, such as anxiety, depressive
symptoms, and insomnia, explained Ms. Billioti de Gage, a PhD student at the University of Bordeaux, France.
The database enabled her to deter-mine how many cumulative days worth of benzodiazepine prescriptions partici-pants filled during the study years, as well as whether the medications had a short or long half-life.
In a multivariate analysis adjusted for stroke, myocardial infarction, hyperten-sion, diabetes, and use of antiplatelet agents or anticoagulants during the period 5-10 years prior to diagnosis of Alzheimer’s disease, the use of benzo-diazepines was independently associated with a 51% increased risk of subsequent Alzheimer’s, compared with nonusers.
A dose-response relationship was apparent. Individuals with prescriptions for up to 90 days worth of benzodiaz-epines were not at significantly greater risk for future Alzheimer’s disease than nonusers. Those with a cumulative 91- to 180-day exposure had a 32% increased risk compared with nonusers, however, and patients with more than 180 days of benzodiazepine use had an 84% increased risk.
The association with later Alzheimer’s disease was stronger in patients who used benzodiazepines with a half-life of 20 hours or longer. In a multivariate analysis they had a 70% greater risk of Alzheimer’s, compared with nonusers. Patients who used a benzodiazepine hav-ing a half-life of less than 20 hours had a 43% increase in risk.
When the multivariate analyses were further adjusted for anxiety, depressive symptoms, and insomnia – all of which can be prodromes of dementia – the results were not meaningfully altered, she added.
This case-control study confirms the results of an earlier prospective popula-tion-based study by Ms. Billioti de Gage and colleagues. That French study also found a roughly 50% increased risk of
dementia in elderly patients who initi-ated chronic benzodiazepine therapy (BMJ 2012;345:e6231). However, with only 1,063 participants, 253 of whom were diagnosed with dementia during 15 years of follow-up, the sample size was too small to draw firm conclusions. The current case-control study, with 8,980 subjects representative of the Quebec community-dwelling elderly population, is more persuasive, the investigator said.
Guidelines recommend preferential use of short half-life benzodiazepines and short durations of use in the elderly; however, in clinical practice the medica-tions are often used long-term.
The biologic mechanism by which chronic use of benzodiazepines by elderly individuals might predispose to Alzheimer’s disease hasn’t been worked out, but the medications’ short-term adverse effects on memory and cogni-tion are well recognized.
The case-control study was funded by the French Ministry of Health and the Funding Agency for Health Research of Quebec as well as by university grants. CfA
Bruce Jancin is with the Denver bureau of Frontline Medical News.
Alzheimer’s Risk Rises With Chronic Benzodiazepine useBy BRUCe JanCIn
Editor’s NoteOne more good reason not to use benzos indiscriminately. Although I am not sure this observed increase in dementia is cause and effect, we already have plenty of evidence that these drugs can be harmful, increasing falls and causing more disinhibition of behavior. And we have better drugs for anxiety (e.g., SSRIs) and insomnia anyway. Think twice before prescribing a benzo in this population, especially a long-acting one.
—Karl Steinberg, MD, CMD Editor in Chief
Atrial fibrillation was associated with a more than twofold increase in the risk of silent cerebral infarc-
tions, even in patients with no history of symptomatic stroke, a systematic review and meta-analysis has found.
The analysis of 11 studies involving 5,317 adults with atrial fibrillation but no history of stroke or prosthetic valves showed a significant increase in the risk of silent cerebral infarctions (OR, 2.62), independent of whether their AF was paroxysmal or persistent, according to meta-analysis published in the Annals of Internal Medicine (Ann Intern Med 2014;161:650-58).
“Although SCIs [silent cerebral infarc-tions] do not present with acute stroke symptoms, they have been reported to be associated with more than three- and
twofold increases in the risk for symp-tomatic stroke and dementia, respec-tively,” wrote Shadi Kalantarian, MD, MPH, and colleagues from the Institute for Heart Vascular and Stroke Care and Massachusetts General Hospital. “Consequently, the higher prevalence of SCI in patients with AF may put this population at a greater risk for cognitive impairment, future stroke, and disability.”
The study was funded by the Deane Institute for Integrative Research in Atrial Fibrillation and Stroke, Massachusetts General Hospital, and the Harvard Catalyst and the Harvard Clinical and Translational Science Center. Two authors declared grants and personal fees from private industry. CfA
Bianca Nogrady is a Frontline Medical News freelance writer based in New South Wales, Australia.
Atrial Fibrillation Doubles Silent Cerebral Infarct Risk
By BIanCa noGRady

CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 3
Dear Dr. Jeff:Our state is considering legalizing marijuana. Clearly, we will be admitting residents who are already using marijuana and some others for whom it might be recommended. I know that the details vary from state to state, but do you have any general or specific recommenda-tions for our nursing home?
Dr. Jeff responds: As of this writing, 23 states have legalized marijuana for medical use under various circum-stances and with various limitations and regulations. Several others are con-sidering legislation or ballot proposi-tions. Additionally, many localities have decriminalized possession of small quan-tities for personal use while retaining laws against sales. Legislation dates back to Alaska and Oregon in the late 1990s and includes states that have legalized marijuana but failed to create the regu-lations needed to make the laws effec-tive and clear. Colorado, Washington, Oregon, and Alaska also have legalized recreational use, production, and distri-bution. From the viewpoint of a skilled nursing facility, these represent two quite different situations.
Despite these legislative activities, the Drug Enforcement Administration still classifies marijuana (or rather, tetra-hydrocannibinols, which are believed to be the major psychoactive components in marijuana) as a Schedule I controlled substance, meaning only available for research purposes but without approved medical uses. Two cannabinoid prepa-rations, dronabinol and nabilone, have been approved by the Food and Drug Administration for the treatment of nausea and vomiting in cancer patients receiving chemotherapy and for anorexia in AIDS patients. These are synthetic oral preparations, not marijuana extracts, and were placed on DEA Schedule II.
Dronabinol, sold in the United States as Marinol, was moved from DEA Schedule II to Schedule III, allowing pre-scribers to authorize up to five refills, due to observational studies of its low potential for abuse or addiction. Thus, cannabinoid preparations are already available and used, albeit infrequently, in nursing homes all over the United States. However, due to the relative lack of success using this medication in patients with anorexia and weight loss unrelated to HIV or cancer treat-ments, along with its expense, its use has not become common. The FDA is fast-tracking a cannabinoid oromuco-sal spray to treat pain in patients with advanced cancer. But delta-9 tetrahy-drocannabinol (THC) remains illegal. Federal “Just Say No” policies date to
the Reagan Administration and seem unlikely to change, despite changes at the state level.
A Long History The plant genus Cannabis has been cul-tivated by humans since antiquity, both for the strength of its stalks (hemp) and the bioactive properties of its seeds, leaves, flowers, and buds. Medicinal uses for cannabis, and particularly the sativa species, were widely described in ancient medical texts since the pharma-copoeia of Emperor Shen-Nung in 2737 B.C. It was considered a fundamental treatment in many herbal medication systems, along with extracts from opium poppies and ephedra plants. Its use is described on Egyptian papyri and was apparently used topically to treat hem-orrhoids, including those of at least one Pharaoh. Cannabis preparations were used by Indian, Greek, and Arab physi-cians. A shaman from the Uighur region was buried 2700 years ago with bowls of cannabis at his head and feet, which have been confirmed to contain THC. And some scholars have suggested that the kaneh bosem described in Exodus 30:23 as one major ingredient of holy anointing oil (later used by Jesus and his followers to heal the sick – see Mark 6:13) – and which is variably translated as reeds, sweet cane, calamus, or other plants – is actually cannabis.
Cannabis for both medical and recre-ational use was legal in the United States until 1937. Extracts of cannabis were routinely sold in pharmacies for both ingestion and topical use. Nevertheless, it was not commonly prescribed nor – despite the miraculous properties ascribed by some enthusiasts – regarded as particularly effective for the treatment of common conditions. The analgesic properties of cannabis were known and explored in ancient times, when its numbing properties were used for anesthesia, but cocaine was considered a much more effective topical anesthetic for mucosal pain than cannabis smoke. There was little opposition from orga-nized medicine when marijuana was outlawed, nor has there been any par-ticular pressure from major medical societies for its legalization.
Limited DataMedical use of marijuana is legal in many countries, but utilization is not very extensive. Although potential uses have been described for many different conditions, including glaucoma, neu-ropathic pain, cancer, multiple sclero-sis, and seizure disorders, for most of these conditions the use of cannabis
derivatives appears likely to be of symp-tomatic relief for a limited group of patients with refractory conditions rather than a routine or preferred treat-ment. Of course, anything that might relieve suffering should be seriously examined, and potentially useful treat-ments should not be denied to those who may benefit. Unfortunately, use-ful data to evaluate the risks and ben-efits of marijuana for the treatment of any of the proposed conditions are extremely limited. Although more than 200 researchers have been approved to use marijuana for research purposes, many of these studies relate to detec-tion and evaluation of abuse potential. Only 16 researchers are conducting trials on smoked marijuana in human beings. Most published studies on therapeutic potential or adverse effects to date have been small in scale and poorly designed to answer clinicians’ questions.
A 2007 study in the British Journal of Pharmacology (Br J Pharmacol 2007;152:655-62) raised the exciting pros-pect that cannabis might be an effective treatment for Alzheimer’s disease. The authors noted that THC and other can-nabinoids have been shown to have neuro-protective effects against beta-amyloid aggregation, inhibit the phosphorylation of tau protein, and decrease inflamma-tory and oxidative damage to neurons. Furthermore, THC may be a cholines-terase inhibitor in the brain, thus offer-ing a trifecta for Alzheimer’s in a single drug. The brain has an entire cannabi-noid system with binding sites present on a variety of neurons. Unfortunately, a recent review article of cannabis for the treatment of a variety of neurodegen-erative diseases, and a Cochrane review specifically aimed at Alzheimer’s disease, both concluded that there is insufficient evidence to draw conclusions regarding the efficacy of cannabis for long-term treatment. But there is no doubt that the acute use of inhaled cannabis preparations inhibits short-term memory and that the potential for cannabis-induced sensory alterations and hallucinations repre sents a severe risk for dementia patients who already are susceptible to delirium.
Different Smokes for Different Folks Understanding medical marijuana is complicated by the simple fact that there are many different strains of marijuana and that THC is only one of at least 468 compounds present in a typical Cannabis sativa plant (not counting possible pes-ticides or other substances used in its growth and preparation). The concen-trations and ratios of these substances
vary from plant to plant and certainly between C. sativa and C. indica, which may be more sedating and also contain more of the nonpsychoactive elements believed to control seizures and muscle spasms. States that have legalized medi-cal marijuana have generally allowed physicians to prescribe it on an as-needed basis and allowed patients to adjust the amount ingested – whether eaten or smoked – based on their symptoms. Because there is no standardization, with sale currently by product weight alone, and even the ratio of seeds to leaves or buds varying from sale to sale (not to mention twigs, soils, and bugs frequently present as well), consumers have only limited control over purchased products. (The Denver Post currently employs a pot critic to review locally available strains, comparable to their wine critic.)
Some strains are known or believed to have much higher THC concentrations, and some plants grown primarily for hemp production have been bred to have very low THC concentrations to protect agricultural laborers from having contact with the plants. Some strains produce oilier THC, which may be present on the exterior of the plant. Dosage also varies with the route of administration as does the onset of biological action, which is much more rapid when absorbed directly across pulmonary membranes than through the gastrointestinal tract. Obviously, all this makes actual prescrib-ing by a physician or nurse practitioner for administration by licensed nursing staff in specific doses at specific intervals virtually impossible. Also, vendor phar-macies in most states are not licensed to distribute cannabis, which is generally sold through specialized outlets. New York state has proposed an integrated license from production through trans-port and sale, which would effectively exclude standard pharmacy supply sys-tems from involvement with medical marijuana. Reimbursement through standard insurance mechanisms is also effectively impossible.
Too Much To Overcome Given all these barriers, most facili-ties would be unwise to use medi-cal marijuana as such in the nursing home. The early experience in states that have legalized marijuana for medi-cal purposes has suggested that only a few physicians write the majority of prescriptions and that the typical user of medical marijuana is a 41-year-old male using marijuana for a chronic pain
By Jeffrey Nichols, MD
high in the nursing home
Dear Dr. Jeff
See Nursing Home • page 5

4 • CARIng FoR The AgeS JAnuARy 2015
Nicole Brandt, PharmD, MBA, CGP, professor, geriatric pharmaco-therapy, pharmacy practice and sci-ence, University of Maryland School of Pharmacy, Baltimore:
▶▶ There will continue to be this trans-formation to value-based health care and this will impact how the care is delivered in the PA/LTC market. Hopefully, we will see an integration of health information exchange dur-ing care transitions, especially in light of impact on reimbursement due to readmissions.
▶▶ Medication management and man-aging high cost medications will con-tinue to be areas that need attention. Expensive specialty medications for conditions such as hepatitis C, cancer, and multiple sclerosis will continue to impact drug spending and the burden both on PA/LTC facilities and payers, as well as patients.
▶▶ There needs to be a concerted effort to look at how to effectively integrate or communicate with health care sys-tems and providers to improve the delivery of care and minimize transi-tions in care. There needs to continue to be a collaborative, interprofessional approach to meeting the increasingly complex medical and medication needs of the patients served in the PA/LTC setting.
Janet K. Feldkamp, RN, BSN, LNHA, JD, partner, Benesch Friedlander Coplan & Aronoff LLP, Columbus, OH:
▶▶ The Office of Inspector General and other state and
federal fraud-fighting entities will continue to vigorously investigate and prosecute health care fraud, includ-ing violations of the false claims act, Stark law, and other fraud statutes. The focus will be across all types of health care entities, including skilled nursing facilities, home health, and hospice.
▶▶ Elsewhere, [violations] related to infection control in the SNF setting will continue to be actively cited. Expect to see more citations and increasing scope and severity citations because of the prevalence of multi-drug resistance organisms and the recent focus on Ebola in the United States.
▶▶ Additionally, we likely will see liti-gation related to the use and enforce-ment of arbitration agreements in SNFs in states that do not have a statutory or regulatory prohibition on their use with admission agree-ments. This litigation continues in many jurisdictions.
Robert M. Gibson, PhD, JD, senior clinical psychologist, Edgemoor DP SNF, Santee, CA:
▶▶ There is clearly a great deal happen-ing with funding and growing financial
pressures in long-term care. At the same time, I expect continued pressure on LTC facilities to cope with higher acuity, both medically and in terms of psycho-logical and psychiatric issues. As place-ment pressures continue, we will likely see continued growth in the numbers of younger adults in long-term care, as well as a continued shift of medically impaired persons in the correctional system to the community and, in many cases, to long-term care. With declining mental health resources and a lack of resources for persons with brain injury or neurodegenerative conditions, these segments of the LTC population will also continue to grow, thus increasing the need for effective behavior man-agement and mental health services. In general, I anticipate the need to be increasingly flexible and to do more with less.
Daniel Haimowitz, MD, FACP, CMD internist, Levittown, PA:
▶▶ There has defi-nitely been a trend towards expansion of services out of
institutions and toward home- and com-munity-based care. Partly this is due to expectations of baby boomers, but it ties into financial pressures. It certainly provides an opportunity for practitio-ners outside of the traditional PA/LTC setting (assisted living, PACE, house call practices, etc.).
▶▶ Financial drivers are always key issues. Medicare and Medicaid are in the midst of potentially very radical changes – bundled payments, ASOs, combined Medicare-Medicaid man-aged care programs for LTC patients, etc. These are driving real changes in the marketplace. Already, hospitals are making it clear to nursing homes that quality metrics (and clearly the related financial implication) will drive referral patterns. As a result, nursing homes will try moving up the acuity chain into more Medicare post-acute care and fewer chronic LTC patients.
▶▶ I hope medical directors will help the nursing homes step up their game and play a major role in help-ing staff understand and implement the Quality Assurance and Performance Improvement (QAPI) process and INTERACT. Elsewhere, the role of non-physician health care professionals in the PA/LTC world will continue to expand.
▶▶ I hope that the coming year brings more recognition of the Choosing
Wisely campaign, and I think we’ll see more interest in genomic medicine, specifically targeting individuals and their personalized medication use. The concept is interesting, and I believe this issue will continue to expand.
Linda Handy, MS, RD, Commission on Dietetic Registration, San Marcos, CA:
▶▶ I predict that long-term care will be impacted by the recently completed Centers for Medicare
& Medicaid Services Hospital Patient Safety Pilot Initiative that includes detailed surveyor worksheets developed to challenge surveyors as they assess hos-pitals’ compliance with QAPI and infec-tion control. This impact has already started and will carry over into LTC surveys as surveyors ask for more doc-umentation of performance improve-ment and criteria (What residents are screened for weight variance meetings? How are nutrition interventions fol-lowed for effectiveness? What has been evaluated for the root causes of weight loss?). [Facilities will have to] follow through on weaknesses identified and show how effective corrective actions and staff competency are demonstrated. Facilities also will be expected to show how they demonstrate that the infection control officer designee is involved in preventing foodborne illness. I believe that we would benefit from studying these surveyor worksheets and apply them to long-term care to ensure our own compliance.
Jeffrey Nichols, MD, president, New York Medical Directors Association, New York:
▶▶ The top issues will be related to finances, as they always are. Although many
facilities are dependent on Medicare Part A reimbursement – or managed care equivalents – to cover inadequate Medicaid rates and declining private pay census, there will be a serious squeez-ing of these referrals. Instead, providers and insurers are increasingly looking at intensive home care as a cheaper alterna-tive to SNF care, especially for many of the standard orthopedics cases that have been the bread and butter of most sub-acute programs. As a result, facilities will need to refocus their rehab programs and align their services to the needs of referral sources and a sicker resident population to survive.
▶▶ At the same time, 2015 will be the year when electronic health records finally reach many LTC providers. Most sys-tems designed for use in nursing homes perform well on the finance/care plan-ning/[Minimum Data Set] side but are
poorly designed for clinical care or link-age to acute care and home care partners in the care continuum. Progress in this area will depend on whether medical directors and other practitioners are able to unite and insist that these problems are addressed as paper charts disappear.
Dan Osterweil, MD, CMD, profes-sor of medicine and associate director, multicampus pro-gram in geriatrics and gerontology, the Borun Center, Sherman Oaks, CA:
▶▶ The pressures to meet the value-based purchasing propositions will increase both on nursing home providers and hospitals. As a consequence, medical providers will feel this pressure as well.
▶▶ The demand for quality will spill over to the post-acute space with increased demand for accountability that will come out of National Committee for Quality Assurance standards, delineating the responsibilities for post-acute complica-tions between the hospitals and skilled nursing facilities. SNFs may join the crowd and be subject to financial penal-ties and rewards just as hospitals are.
▶▶ Last, but not least, the care coordina-tion codes and PA/SNF coordination codes in fee-for-service medicine may shift the burden for care coordination between settings from institutions to practitioners. The next year will provide an opportunity to improve on cross-sys-tem coordination. Practitioners will be wise to consider hiring a care coordina-tor for their practice, especially those practices with more than 200 patients who have two or more chronic condi-tions and qualify for the per-member-per month fee.
Barbara Resnick, PhD, CRNP, FAAN, FAANP, professor and Sonya Ziporkin Gershowitz chair in gerontology, University of Maryland School of Nursing, Baltimore:
▶▶ There will be a continued separa-tion and differentiation in long-term care between subacute and post-acute care patients and long-stay patients. Increasingly, there will be a growth in specific buildings and units for these different types of patients. In my crys-tal ball, I see that this will have many positive outcomes. Designated units that focus on rehabilitation and recov-ery will work on training staff to have the skills to provide rehabilitation nurs-ing and medicine, and will facilitate the discharge in the most cost-effective and efficient manner. I further hope that this rehabilitation philosophy will translate to long-stay patients as well, and we will all begin to incorporate a
experts Predict: What’s Ahead for PA/LTC in 2015?Caring for the Ages asked its editorial advisers to predict, from their distinct perspectives, the major issues they expect to arise in the field of post-acute/long-term
care during 2015. Predictions coalesced on the topics of quality outcomes, workforce issues, and finances and reimbursement.

CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 5
function-focused care approach, regard-less of setting.
▶▶ Another prediction (or at least a dream) includes a stronger focus on prevention, with immunizations that go beyond just flu and pneumonia vaccines and include zoster and tetanus-diphtheria-pertussis as routine vaccinations. Likewise, we will focus more on prevention of pressure areas and contractures, even at what is thought of as the end of life (as one never knows what might happen to or with our quite resilient older individuals during this time). Elsewhere, as more individuals live to 100 years or older, we may need to put more emphasis on pre-vention so that those years can be lived comfortably and with some quality.
Karl Steinberg, MD, CMD, editor in chief, Caring for the Ages, Oceanside, CA:
▶▶ We will see more of a move toward value-based pay-ment and population
health in the PA/LTC setting in 2015, and this trend will continue in years to come. With some of the new models, includ-ing later generations of accountable care organizations, many of our patients will be able to go directly from emergency department (or doctor’s office) to skilled care in an SNF without a required hos-pital stay – just as our Medicare+HMO
patients have been able to do for decades. That is a very good thing, because the hospital is not a good place to be when patients don’t need to be there (with all due respect to our hospital and hospital-ist colleagues). At the same time, it will be possible for a long-term custodial SNF resident to be bumped up to a skilled level without having to go to the hospital, which is also a very positive change.
▶▶ I also predict that the pilot programs for dual eligibles (Medicare/Medicaid)will be expanded, and we will see a continuing exodus of less functionally impaired SNF residents into residential
care (assisted living, board-and-care facil-ities, etc.). This is another good devel-opment and a better way to spend our Medicaid tax dollars.
▶▶ Meanwhile, as desperately as the assisted living industry tries to cling to the “we are not medical” mantra, we’ll see movement for increasing regulation in this arena – maybe even federal regu-lations at some point – as the level of chronic illness continues to increase in that setting.
▶▶ From the clinical side, I think we will continue to see less unnecessary use of antipsychotics, less use of sliding-scale
insulin, better antibiotic stewardship (with less checking of urine studies for isolated single-symptom situations like cloudy or foul-smelling urine, a fall, or mental status changes, and thus less inappropriate treatment of asymptom-atic bacteriuria), and more access to palliative care services and appropriate, informed advance care planning in our buildings. CfA
Compiled by senior contributing writer Joanne Kaldy, a freelance writer in Harrisburg, PA, and a communications consultant for AMDA.
With CancerCare, the difference comes from: • Professional oncology social workers• Free counseling • Education and practical help• Up-to-date information • CancerCare for Kids®
For needs that go beyond medical care, refer your patients and their loved ones to CancerCare.
CancerCare’s free services help people cope with the emotional and practical concerns arising from a cancer diagnosis and are integral to the standard of care for all cancer patients, as recommended by the Institute of Medicine.
makes all the difference
®
1-800-813-HOPE (4673)
www.cancercare.org
Help and Hope
syndrome, far different from the pro-file of a typical nursing home resident. Nursing homes with significant hospice or AIDS populations should consider the use of currently available FDA-approved preparations.
The issues presented by legalized rec-reational possession and use are totally different. Regardless of risks of carcino-gens or tars that may be present in mari-juana, or the supposed “gateway” nature of its use leading down the slippery slope to addiction, nursing home residents with decisional capacity should have the right to make or repeat the dumb deci-sions of any other citizen of your state. Because of the risk of fire in an institu-tional setting, plus the risk of exposure to secondhand smoke for employees and other residents (contact high), it seems reasonable to use all the same restric-tions used for tobacco smoking, includ-ing complete restriction if necessary. However, oral ingestion using supplies bought and maintained individually for the resident should be accepted. Indeed, perhaps as a tribute to the late Jerry Garcia, you might name one nursing unit Panama Red. Unit birthday parties with brownies should be very mellow. CfA
Dr. Nichols is president of the New York Medical Directors Association and a member of the Caring for the Ages Editorial Advisory Board. Comment on this and other columns at www.caringfortheages.com under “Views.”
Nursing Homefrom page 3

6 • CARIng FoR The AgeS JAnuARy 2015
family was taking him for prostate tests. Dr. Karlawish asked what they were looking for and what they expected to gain from these tests, and discovered the family didn’t really have an answer. “It led to a dialogue about the value of what we propose to do and what will maximize quality of life and dignity for the patient,” he said.
Prognosis and Life Expectancy Prognosis and life expectancy should inform how elders live and the inter-ventions practitioners recommend for them. “We should be recommending whether or not to pursue tests or treat-ments based on meaningful future risk,” said Dr. Karlawish. “We should know about this so that we can be savvy in our recommendations. There are a whole host of risk calculators available,
but we need to scrutinize them care-fully and determine their value.” He cautioned that practitioners shouldn’t just rely only on calculators and risk-benefit data. “Don’t discount your solid clinical judgment about a prognosis,” he said.
One consideration regarding progno-sis is fairly simple, Dr. Karlawish said. “If, a year from now, you were told that your patient died, would you be sur-prised?” He added, “I use that when I communicate with patients or families, and they want a prognosis.” However, he added, “When people ask for a prog-nosis, I seek to determine what it is that they want to know, especially in the case of people with dementia. It’s presumptuous to think that they mean life expectancy.” For example, he said, they may want to know how long it will be before a loved one doesn’t recognize them or until he or she is no longer able to live alone.
If the family actually wants to know how long someone will live, said Dr. Karlawish, “I talk about how sur-prised – or not – I would be to hear in a year that the person had died. That is a more meaningful qualitative response than a number that may or may not be accurate.”
Mining for Gold in Conversations Practitioners should take full advan-tage of opportunities to communicate
with family members and to learn from these interactions. “A useful con-versation is to say, ‘Tell me how things have gone for your family member? How has he gotten to this place in his life? What does he – and you – see for the future?’ Ask the family to share what they see as the person declines and what they expect to happen in the future,” Dr. Karlawish said. He explained that these narratives can uncover interesting and even surpris-ing information.
For example, “They may see the dis-ease differently than you do,” he said. “Or they may have a narrative that is full of conflict and emotion and views that reflect this. You may discover that they don’t trust the health care system or that they have guilt or anger because they don’t think a loved one has been cared for adequately.”
He recalled, “I remember one inci-dent where my perspective was that the patient had advanced dementia, while the family’s view was that the cognitive impairment was only a recent development. My perspective of advanced dementia with limited time left was different than their view.” Once the practitioner knows the fam-ily’s perspective, he or she can seek to find some common ground. “Once you have a common understanding, you have some reasonable grounds to make plans to care for the patient,” Dr. Karlawish said.
Dr. Karlawish stressed that AMDA members and other post-acute/
long-term care practitioners play a key role in creating and perpetuating “plea-sure panels” for their patients. “They are on the front lines of caring for people who are among the most vulnerable in our society,” he said. “In this unique position, they are the keepers of the culture and values that will shape what society does – and does not do – for these people.”
Dr. Karlawish said that he is look-ing forward to speaking at the AMDA annual conference. His presentation at the AMDA annual conference, “How Are We Going To Live with Alzheimer’s Disease,” is scheduled for Friday, March 20, from 8:00-10:30 a.m. CfA
Senior contributing writer Joanne Kaldy is a freelance writer in Harrisburg, PA, and a communications consultant for AMDA and other organizations.
Pleasurefrom page 1
Balancing Bedside Manner With Desktop Medicine
In 2010, Dr. Karlawish coined the term “desktop medicine,” describing a model of care in which computer networks and big databases transform medical practice. In this model, disease is defined based on risk, and practitioners and patients alike seek information about these diseases and their treatment, and they share information with others.
Desktop medicine is transforming health care, including post-acute/long-term care, a setting where technology traditionally has lagged behind. “Many practitioners pursue work in this setting because they want to care for sick peo-ple, and long-term care is seen as the last bastion of bedside medicine. These patients are sick; they have a number of problems and need personalized atten-tion,” said Dr. Karlawish.
Nonetheless, there is a role for desktop medicine in this care setting. “Long-term care patients are loaded with risks, and desktop medicine can be thought of as an actuarial exercise. We can use technology to help assess patients, to communicate to them and to families, and to devise and communicate a coher-ent, effective, real-time care plan,” he said.
Although technology has advantages for the PA/LTC practitioner, one chal-lenge for these individuals will be taking advantage of it without losing the art of bedside manner. Dr. Karlawish cautioned against using technology, such as electronic health records [EHRs], as an “endless data dump.” He shared the story of a physician who had a serious injury and, on recovery, reviewed his records. “He determined that the notes in the record were useless with little attention [given] to anything anyone was saying, particularly him.
“EHRs discourage writing,” Dr. Karlawish said. “Instead, there are ‘drop downs’ and check boxes for complaints, symptoms, concerns, and so on. These aren’t in the patient’s words. It’s not information about what the patient says or feels.” He added that certain aspects of EHRs, such as the ability to easily transfer information, are good if they are integrated effectively and organized in a way that practitioners don’t have to “flip through endless data” to find the information they need.
To supplement data input into the EHR, Dr. Karlawish uses voice recognition technology to dictate his notes and capture his conversations. “This helps me document what is really happening with the patient – what is their typical day.”
For more information about desktop medicine, see Dr. Karlawish’s original article ( JAMA 2010;304:2061-2).
Take Part I of AMDA’s Core Curriculum on Medical Direction in LTC online save money,
earn credits at your convenience.
core curriculumon medical direction in long-term care
PART I ONLINE—REGISTRATION NOW OPEN
™
S E S S I O N 1January 5, 2015 – March 2, 2015
Registration now open! Closes February 16.
S E S S I O N 2April 6, 2015 – June 1, 2015
Registration opens February 9, 2015.
R E G I S T E R N O W AT
www.amda.com/cmedirect/core-part-1.cfm
For information on the full live course, and part II visitwww.amda.com/education/core/index.cfm
Register NowIf you haven’t registered for the AMDA – The Society for Post-Acute and Long-Term Care Medicine Annual Conference in Louisville, KY, March 19-22, don’t put it off any lon-ger. Visit www.paltcmedicine.org/register-now/ to register. To book your hotel, visit www.paltcmedicine.org/travel-and-hotel/. You won’t want to miss this one-of-a-kind educational forum designed for PA/LTC professionals.
‘When people ask for a prognosis, I seek to determine what it is that they want to know, especially in the case of people with dementia.’

CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 7
sodium excretion of 3-5 g per day, and the next largest segment, 44%, had a sodium excretion of more than 5 g per day.
“This suggests that, at present, human consumption of extremely low amounts of sodium for prolonged periods is rare,” the investigators noted.
The investigators found, after mul-tivariate adjustment, that for each 1-g increment in sodium excretion, there was an increment of 2.11 mm Hg in systolic BP and 0.78 mm Hg in diastolic BP (P < .001 for both) for all areas of the globe.
However, this correlation was non-linear. The association between sodium and BP was weak in the largest subset of participants who had an excretion of 3-5 g per day, and was nonsignificant in those who had an excretion of less than 3 g per day.
The association between sodium intake and BP was stronger in people who had an excretion of more than 5 g per day and in those who already had hypertension at baseline. It also increased with increasing patient age.
Taken together, these findings indicate that sodium’s effect on BP is nonuniform and depends on the background diet of the population as well as the individual’s age and hypertension status, Dr. Mente and his associates said (N Engl J Med 2014;371:601-11).
PURE CVD SubstudyThe second report also was a sub-study of the PURE study, this time headed by Martin O’Donnell, PhD, of the Population Health Institute and McMaster University. The researchers performed a prospective cohort study involving 101,945 PURE participants to assess the association between baseline urinary sodium and potassium excre-tion, again as a surrogate for intake, with mortality and incident cardio-vascular events during 3.7 years of follow-up.
The primary composite outcome of death or a major CV event occurred in 3,317 participants (3.3%). The mean 24-hour sodium excretion was 4.9 g.
Surprisingly, the lowest risk of death and CV events was seen not in
people with the recommended lev-els of sodium excretion but in those whose sodium excretion was much higher, at 3-6 g per day. Risks actually increased at levels of sodium excretion that were lower than 3 g per day, as is recommended, as well as at levels that were higher than 6 g per day. Moreover, the association between high sodium excretion and high CV and mortal-ity risk was significant only among adults who already had hypertension at baseline.
“The projected benefits of low sodium intake ... are derived from models ... that assume a linear relationship between sodium intake and BP and between BP and cardiovascular events. Implicit in these guidelines is the assumption that there is no unsafe lower limit of sodium intake,” Dr. O’Donnell and his associates wrote (N Engl J Med 2014;371:612-23).
The findings from both of these PURE studies call those assumptions into question.
Sodium and Cardiovascular Mortality: NUTRICODE The third report was a review of the lit-erature regarding sodium intake’s effect on CV mortality worldwide; the gath-ered data then served as the basis for a complex statistical model that estimated how many deaths could be attributed to sodium consumption in excess of a ref-erence level of 2.0 g per day. This study was performed by the Global Burden of Diseases, Nutrition, and Chronic Diseases Expert Group (NUTRICODE) and was headed by Dariush Mozaffarian, MD, PhD, MPH, a cardiologist and epi-demiologist with Tufts University and the Harvard School of Public Health, both in Boston.
These investigators quantified sodium intake in 66 countries (accounting for 74% of adults throughout the world) by age, sex, and country of residence, and correlated these data first with find-ings from their meta-analysis of 107 ran-domized trials of interventions to curb sodium intake and then with the results of two large international trials linking the effects of various BP levels on CV mortality.
They estimated that the mean level of sodium intake worldwide is 3.95 g per day and that those mean levels varied by
geographic region from a low of 2.18 g to a high of 5.51 g. “Overall, 181 of 187 countries – 99.2% of the adult popula-tion of the world – had estimated mean levels of sodium intake exceeding the World Health Organization recommen-dation of 2.0 g/day,” Dr. Mozaffarian and his associates said.
Contrary to the findings of the two PURE analyses, these data showed “strong evidence of a linear dose-response relationship” between sodium intake and BP, such that each reduction of 2.30 g per day of sodium was sig-nificantly linked with a reduction of 3.82 mm Hg in systolic BP, as well as a direct correlation between increasing BP and increasing CV mortality.
Extrapolating from these data, “we found that 1.65 million deaths from CV causes worldwide in 2010 were attribut-able to sodium consumption above the reference level” of 2 g per day. “Globally, 40.4% of these deaths occurred pre-maturely, i.e. in persons younger than 70 years of age,” Dr. Mozaffarian and his associates said (N Engl J Med 2014;371:624-34).
“In sum, approximately [one] of every 10 deaths from CV causes worldwide and nearly [one] of every [five] prema-ture deaths from CV causes were attrib-uted to sodium consumption above the reference level,” they said.
In an editorial accompanying this report, Suzanne Oparil, MD, said,
“The NUTRICODE investigators should be applauded for a herculean effort in synthesizing a large body of data regarding the potential harm of excess salt consumption” (N Engl J Med 2014;371:677-9).
“However, given the numerous assumptions necessitated by the lack of high-quality data [in the literature], cau-tion should be taken in interpreting the findings of this study,” said Dr. Oparil, of the vascular biology and hyperten-sion program, University of Alabama at Birmingham.
The PURE studies were supported by the Heart and Stroke Foundation of Ontario, the Population Health Research Institute, the Canadian Institutes of Health Research, several pharmaceutical companies, and various national or local organizations in 18 participating coun-tries. These funders played no role in the design or conduct of the studies, in collection or analysis of data, or in pre-paring the manuscript. Dr. O’Donnell reported ties to Boehringer Ingelheim, Bayer, Bristol-Myers Squibb, and Pfizer, and his associates reported ties to Sanofi-Aventis, AstraZeneca, and Cadila. The NUTRICODE study was funded by the Bill and Melinda Gates Foundation. CfA
Mary Ann Moon is a Frontline Medical News freelance reporter based in Clarksburg, MD.
More Fuelfrom page 1
PA/LTC Perspective“There have been a number of previous studies that found that lower sodium is not necessarily good for you. The first two studies prove lowering
salt to an excessive level is bad, and show that anything below 3 g of sodium is bad. There is no evidence to go below 3 g. The optimal level of sodium is probably about 3-4 g a day.
“The third study only focused on blood pressure. In the nursing home, lowering blood pressure by a few points is not paramount, particularly if people are starving because they’re not eating the unpalatable – and unsalted – food being served to them. This paper makes little sense as it relates to our population.
“We have a tendency in medicine to want to get some-thing to an optimal level, and if we get there, we want to try to go lower. This should not be the case with sodium restriction.”
—John Morley, MD, BChSt. Louis University Medical Center
Announcing AMDA’s 2015 Webinar BundleAMDA is pleased to announce the 2015 webinar bundle, with new discounts. Sign-up now to receive access to 9 live webinars, as well as their recordings following the live event. Topics will include: Person-centered Care, Resident Rights, Hospice Care, Pitfalls of EMRs, CMS 5-Star System, Cardiology Issues in PA/LTC, Cultural Diversity in PA/LTC, Skilled Services/Medical Necessity, and Infectious Diseases.
New in 2015, AMDA members will receive an additional discount on both single webinars and the webinar bundle – almost a 50% discount off of non-member prices, and close to 30% off from previous costs.
SINGLE WEBINARS: AMDA Members - $55
Non Members - $99
AMDA 2015 WEBINAR BUNDLE:AMDA Members - $425Non Members - $825
Visit www.amda.com/cmedirect/#web for more information and to register.
Join Us for AMDA’s Next Live Webinar:J A N U A R Y 2 8 , 2 0 1 5Title: Infection Control in PA/LTCPresenter: Karyn Leible, MD, CMDwww.amda.com/cmedirect/#web
™
online education
e-University PROVIDED BY
™
Not an AMDA Member?www.amda.com/membership/

8 • CARIng FoR The AgeS JAnuARy 2015
Post-acute care facilities, including some skilled nursing facilities, con-tinue to struggle with consistent
initiation of cardiopulmonary resuscita-tion for residents who have chosen to elect CPR in the event of cardiac arrest. The failure of SNFs to appropriately implement CPR continues to result in an immediate jeopardy citation by state survey agencies and in civil money pen-alties and other sanctions for facilities receiving citations. Facility management, including the physicians and medical directors, should review the policies and procedures related to CPR to ensure that their facility is well-prepared to imple-ment a CPR intervention determined by the physician orders and the applicable legal requirements.
Despite the fact that the effectiveness of CPR is reduced for individuals outside of the acute care setting, and also reduced as individuals age, the decision regarding a resident’s code status is a legally binding determination that must be documented by a physician. Each resident or his/her legal decision maker has the right to make medical choices, including the determina-tion of code status, in consultation with the attending physician. A study from the Archives of Internal Medicine published in 2000 found that despite previous con-tradictory study results, individuals older than 80 years survive to hospital discharge at a lesser rate than do younger individu-als. In the SNF setting, even with dimin-ished survival rates, the legal decision for the implementation of CPR or that of a no code or limited code status still must be issued as a physician order.
To highlight some of the confusion in the area, the Centers for Medicare & Medicaid Services issued guidance to the state survey agencies in October 2013 regarding CPR services in nurs-ing facilities. “Survey & Certification: 14-01-NH” requires SNFs to implement policies to provide for at least basic CPR, in accordance with or in the absence of advance directives, before the arrival of
emergency medical services (EMS), in the event a resident experiences cardiac arrest. CMS cited past policies and prac-tices of some SNFs that did not provide all residents experiencing cardiac arrest with CPR prior to the arrival of EMS. The issuance of the guidance followed news reports about concerns over CPR implementation in a California continu-ing care community. The policy at the California community was not to per-form CPR on residents, but to simply contact local EMS for resuscitation at the time of the community’s response to the cardiac arrest. Now, CMS has clarified that all Medicare and Medicaid certified nursing facilities must have a policy for at least basic CPR, yet facilities across the country continue to receive regula-tory citations due to failure to initiate CPR or failure of adequate performance of CPR.
Penalties Add Up A CMS regional manager recently told me at least eight facilities in the coun-try were cited for immediate jeopardy for improper implementation of CPR in the second quarter of 2014. Historically, citation penalties often have been the retrospective imposition of civil money penalties back dated to the date of the failure to implement CPR, even when the identification of lack of action was not determined until a later date through a complaint or standard survey.
A December 2010 departmental appeals board (DAB) appellate division case upheld a citation at F309 (quality of care) cited at Woodland Oaks, KY, for inappropriately withholding CPR from a resident with end-stage renal disease who did not show signs of irreversible death and did not have a do-not-resusci-tate (DNR) order in the medical record. The facility was cited for immediate jeop-ardy and received a civil money penalty ($4,550 per day for 23 days) for placing this resident and other residents at risk of death or serious harm for failing to implement timely resuscitative measures.
The facility argued that its policy was supported by the Kentucky Board of Nursing advisory opinion statement. This advisory opinion statement indi-cates that CPR is inappropriate, even when the resident had no DNR order, when a person exhibits obvious signs of irreversible death. However, the DAB found that the resident did not show signs of irreversible death when the resi-dent was found cool to the touch and without vital signs. The DAB case discus-sion indicated that the signs of irrevers-ible death listed by the Kentucky Board of Nursing include lividity, rigor mortis,
and algor mortis, and that the resident, according to the facility’s own nursing notes, did not display these signs prior to the pronouncement of death. After-the-fact handwritten statements by several nurses were determined by the court to be self-serving and unreliable evidence.
A Michigan facility was cited in May 2012 with multiple immediate jeopardy and actual harm citations by failing to resuscitate a full code resident. The resident had a recent change of con-dition related to pneumonia and was having increasing respiratory distress. When a licensed practical nurse found the resident without a pulse or respira-tion, she tried to arouse the resident and performed “sternal percussions.” The facility did not undertake appropriate resuscitation efforts or summon EMS personnel, and the resident died at the facility without receiving CPR. The cita-tions included failure to appropriately notify the physician with all the pertinent information; failure to follow appropri-ate standards of nursing care by failing to implement CPR and summon EMS, per policy; and failure to provide necessary care and services by not assessing, moni-toring, and providing prompt interven-tion for an acute condition change. The citations resulted in a fine of $101,000 and the imposition of other sanctions.
These cases illustrate that following the facility’s policies and understanding the state laws related to resuscitation are vital to the management of the facility. Failing to implement the level of resus-citation ordered for residents, despite the resident’s current clinical condition and multiple complicating disease states, can create significant risk for facilities.
Document, Educate, Review Good practices for CPR policies and actions at a nursing home include:
▶▶ Periodic review by the management and the medical director of all policies related to emergency response requiring staff to initiate CPR.
▶▶ Distribution of information on advance directives as required by the Patient Self-Determination Act of 1990, as well as education of residents, families, and staff regarding advance directives.
▶▶ Education of staff, including periodic drills, to ensure that the staff can compe-tently perform the needed resuscitation processes.
▶▶ Documentation in resident records of timely CPR initiation and documentation confirming that CPR was efficiently and timely performed until the resident was transferred into the care of EMS provid-ers or otherwise handed off to other appropriate health care professionals.
▶▶ Clear documentation in the resident’s medical record of the advance directive related to resuscitation that complies with state law and federal certification requirements. Clear identification of the resident’s code status per the facility’s policy.
▶▶ Periodic review of the resident’s advance directive with the resident or the resident’s legal decision-maker, as resident choices may change over time.
▶▶ Periodic quality assurance audits of the accuracy of documentation related to identification of facility residents’ code status.
Nursing facilities have a responsibil-ity to have and implement policies that provide for immediate CPR intervention for residents who do not have a cur-rent DNR order in place (i.e., indicating no CPR). Staff education and training are key components of a successful CPR policy. Facilities must ensure that all residents have accurate, up-to-date code status documented according to policy. Staff must know how to deter-mine resident code status, and when and how CPR is indicated for residents who are full code status. A clear and well-communicated CPR policy can prevent serious state survey citations and, most importantly, ensures that resident prefer-ences at the end of life are appropriately addressed and honored. CfA
This column is not to be substituted for legal advice. The writer, Janet K. Feldkamp, practices in various aspects of health care, including long-term care survey and certification, certificate of need, health care acquisitions, physician and nurse practice, managed care and nursing related issues, and fraud and abuse. She is affiliated with Benesch Friedlander Coplan & Aronoff, LLP of Columbus, OH. You can comment on this and other columns at www.caringfortheages.com, under “Views.”
Facilities at Risk When CPR Isn’t Implemented
By Janet K. Feldkamp, JD, RN, LNHALegal Issues
C.A.S.T. Program
AMDA’s Companion and Spouse Travelers Program allows AMDA – The Society for Post-Acute and Long-Term Care Medicine meet-ing attendee spouses and guests to explore the Louisville area. Visit the Wild Turkey Distillery, the Louisville Slugger Museum, and the Muhammad Ali Center just to start. Pre-registration for C.A.S.T. members ends Feb. 25, so don’t delay. Visit www.paltcmedicine.org/c-a-s-t-registration/.
Nursing facilities have a responsibility to have and implement policies that provide for immediate CPR intervention for residents who do not have a current DNR order in place.

CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 9
PHILADELPHIA – A combination drug of dextromethorphan and quinidine sig-nificantly reduced aggression and agita-tion in patients with Alzheimer’s disease.
Associated with those improvements were significant reductions in measures of caregiver strain and distress, Erik Pioro, MD, said at the Clinical Trials Conference on Alzheimer’s Disease.
“These were very clear, stable, and statistically and clinically meaningful dif-ferences,” when compared with patients who received placebo, said Dr. Pioro, director of the Section of Amyotrophic Lateral Sclerosis and Related Disorders at the Cleveland Clinic.
The drug, Nuedexta, is already approved for pseudobulbar affect and is being investigated as AVP-923 for several other indications, including depression, migraine, neuropathic pain, autism, and Parkinson’s disease dyskinesia.
This phase II trial comprised 220 patients with moderate Alzheimer’s who displayed clinically significant agi-tation or aggression as measured by the Neuropsychiatric Inventory (NPI) and the Clinical Global Impressions Scale.
Most (87%) were living at home, about 5% were in nursing homes, and the remainder were in assisted living facili-ties. At baseline, 74% were taking cho-linesterase inhibitors; 50%, memantine;
56%, an antidepressant (including trazo-done); 21%, an antipsychotic; and 8%, a benzodiazepine.
As measured by scores on the NPI, 92% displayed clinically significant aggression; 70%, irritability/lability; 52%, apathy/indifference; and 47%, anxiety and aberrant motor behaviors. About a third of the group had night-time behavioral disorders, depression, dysphoria, delusions, disinhibition, ela-tion, and hallucinations.
They were randomized to dextro-methorphan hydrobromide and quini-dine sulfate (20 mg/10 mg) or placebo for 10 weeks. Patients in the active group stayed on the study drug for the entire time. Those in the placebo group were assessed for response; 30 of these had improved on placebo. These were reran-domized to active and placebo groups. Placebo nonresponders were also reran-domized to the drug or placebo.
By the end of the first 5-week phase, patients in the active group experienced a mean improvement of 3.3 points on the NPI aggression subscale, which was signif-icantly better than the 1.7-point improve-ment seen among those taking placebo.
After the placebo nonresponders had been rerandomized and treated for another 5 weeks, those taking the study drug had a mean 2-point improvement, compared with a 0.8-point improvement among those taking placebo.
In the group that been on their origi-nally assigned treatment for the entire 10 weeks, those taking the study drug again fared significantly better (a mean improvement of about 4.5 points vs. 1.5 points with placebo).
In all randomization schemes, the clinical and physicians’ global impres-sion improved significantly more in the active group than in the placebo group.
The total NPI score improved signifi-cantly more in the active group (13.5 vs.
8.5 points for those who had been on the same treatments for 10 weeks). NPI symp-tom clusters showed the same pattern of improvement favoring the study drug.
Measurements of caregiver response based on the Caregivers Strain Index and the NPI Caregiver Distress Score significantly improved for caregivers of patients taking the study drug for 10 weeks. CfA
Michele G. Sullivan is with the Mid-Atlantic bureau of Frontline Medical News.
Combination Drug Quells Anxiety, AggressionBy MICHele G. SUllIVan
Editor’s NoteMany of us have already tried dex-tromethorphan/quinidine off-label for our agitated dementia patients, and in my experience it works some-times, maybe a little better in people with vascular dementia. It’s great to see that there is now actual research showing statistically significant improvement in a well-designed, if small, phase II study. This drug is generally well tolerated – certainly with less significant adverse effects than antipsychotics – and I think we will all welcome more options to treat agitated behavior in challenging patients with dementia.
—Karl Steinberg, MD, CMD Editor in Chief
Both patients and their caregivers benefited from the combination drug.
©is
to
cK
Ph
ot
o.c
om
/ge
be
r8
6
After Hours OpportunityUse your clinical skills from your home!
eSNF, Inc. has an exciting opportunity for great physicians experienced in the fields of:
❖ Internal Medicine ❖ Geriatrics ❖ Family Practice
The benefits of working for our physician group are:
❖ Generous supplemental income ❖ No billing ❖ Clinically challenging❖ No overhead ❖ State-of-the-art technology ❖ Work from home
eSNF, Inc. is a telemedicine practice focusing on the institutionalized medically frail. Due to tremendous growth we need more great physicians, with availability on nights and weekends, preferably licensed in:
❖ New York ❖ Pennsylvania ❖ New Jersey❖ Illinois ❖ Connecticut ❖ Florida
Successful candidates will possess strong clinical, communication and consultation skills, a patient-first focus, and an aspiration to drive improvements in health care well into the future.
For More Information Please Call:(855) 376-3669 x702

10 • CARIng FoR The AgeS JAnuARy 2015
We continue with our series exploring long-term care pro-vider organizations that serve
people in facility-based settings and home- and community-based settings. This month, we’ll look at Golden Living through the eyes of its chief medical officer, Michael Yao, MD, CMD.
Golden Living, headquartered in Plano, TX, is one of the largest providers of reha-bilitation and skilled nursing care in the country, with just under 300 facilities in 21 states. This family of companies includes Golden LivingCenters, Aegis Therapies (third largest provider of therapy services in the United States), 360 Staffing, Ceres Purchasing Solutions (a purchasing, con-tract services company), and AseraCare Hospice. Golden LivingCenters alone serve more than 26,000 patients, with a collective staff of more than 40,000.
Most of its services and individu-als served are in facility-based set-tings, except for AseraCare and Aegis Therapies. Between 50% and 60% of its
hospice services and its palliative medi-cine program, PRIME, are provided in the patient’s home.
Dr. Yao has been with Golden Living in a variety of roles for the past 10 years. For the past 2 years, he has served as chief medical officer for Golden Living and is responsible for overseeing and support-ing the medical directors and attending physicians working within Golden Living Centers and AseraCare agencies. He also assists in the evaluation of leading-edge, evidence-based medical practices through the development and expansion of clinical specialty programs, according to the Golden Living website. Dr. Yao is board certified in family medicine and geriatric medicine, and has more than 20 years of experience in long-term care.
Care Across the ContinuumThe rise of vertically connected organiza-tions, such as accountable care organiza-tions, is affecting service delivery across the health care industry. Fragmentation
in health care delivery is well-known. There are more than 15,000 nursing facil-ities and approximately 16,000 licensed home health and hospice agencies in the United States, and that does not include private duty agencies and the vast amount of informal in-home caregivers. An emphasis on connection, coordina-tion, and integration across providers is only natural and makes sense.
So how does Golden Living balance the unique opportunities and challenges of facility-based care with community- or home-based care and services? For Dr. Yao, the health care delivery environ-ment for facility-based and home-based care is similar. Whether you work in a skilled nursing facility or in home- and community-based services, the desired goal is the same: to deliver quality care to the patient over time. “If you’re round-ing on a patient in an SNF setting, you have to think about how care is delivered postdischarge,” Dr. Yao said. It is a grow-ing challenge to view the patient holisti-cally and over time. With the increasing number of hospitalists, SNF specialists, and office-only physicians, mitigating this challenge will become greater and take intentionality to overcome.
Is there a different skill set for the attending physician who follows patients in a facility-based setting rather than in a home-based setting? Dr. Yao would say that it’s not so much a matter of skill set as it is attitude. Home-based care requires the physician to be overtly intent on lis-tening and paying attention to what on-site caregivers report. The physician has to listen closely to what visiting nurses and other staff identify because they see the patient more often than the physi-cian. And that takes time, which is at a premium for physicians across the board. Although the importance and legitimacy of special providers like hospitalists and SNF specialists should not be overlooked, Dr. Yao’s experience is that physicians who do the best with home-based care are those who also follow patients in their facility-based care as well.
Golden Living anticipates growth in vertically integrated organizations, perhaps sooner in metropolitan areas than in rural settings. Increasingly, this includes not just provider networks but also insurance companies. Golden Living is actively participating in Centers for Medicare & Medicaid Services bun-dled payment projects, in which pro-vider partnerships are key.
Physicians as Employees A concurrent development is the chang-ing nature of physician employment status. More and more, physicians are employees of provider networks, rather than being solely independent practitio-ners. At least conceptually, this should
simplify the development process for ver-tically connected organizations because it streamlines the number of parties involved in the negotiations.
Support and communication are essen-tial parts of Golden Living’s corporate strategy to prepare its physicians for the future. In addition to Dr. Yao being at the helm, four regional medical direc-tors interface directly with facility medi-cal directors, who, in turn, interface with local attending physicians. A dedicated newsletter targeted to medical directors and attending physicians covers topics that may range from facility operations to those of specific clinical focus, such as infection control and medication steward-ship. Golden Living also actively encour-ages its physicians to pursue a medical director certification and promotes atten-dance at the annual AMDA conference.
Golden Living will continue to explore ways that leverage technology to support physicians and other caregivers. Two things of growing importance to the com-pany: centering dialog about quality of care and quality of life around metrics of care, and how to increase active involve-ment of physicians in quality assurance and performance improvement.
The transition from primary care physi-cian and educator to a 100% administra-tive role has been a significant change for Dr. Yao. The challenges are many: work-ing daily to improve care and systems of care in the face of reimbursement, regula-tion, and increasingly complex care issues. However, Dr. Yao said, “In the end, it still comes down to quality of care and hav-ing a heart for the populations we serve.” Surely Dr. Yao, his work, and his leader-ship at Golden Living, are a great example for others to model and admire. CfA
Mr. Kubat is director of mission integration for the Evangelical Lutheran Good Samaritan Society. He is an editorial adviser for Caring for the Ages and coordinates the work of various authors for this column. You can comment on this and other columns at www.caringfortheages.com, under “Views.”
Community LTC, golden Living, and Michael yao
Community LTC
By Bill Kubat, LNHA
Experience AMDA’s 2015 Annual Conference sessions anytime, anywhere! Create a username and password, browse sessions, stream or download the entire session! All sessions are synchronized with the audio and presentation materials. CME/CMD credits available for 2015 sessions!
Experience AMDA’s 2015 Annual Conference sessions from the comfort of your own home. All DVD-ROM sessions are synchronized with the audio and presentation materials.
Get both the online library & DVD-ROM of the AMDA’s 2015 Annual Conference sessions. CME/CMD credits available for 2015 sessions on the online library.
Missed any of the previous AMDA Meetings? No Problem! Digitell has over 600 educational sessions from the 2004-2015 Meetings! CME/CMD credits are available for the 2012, 2013, 2014 and 2015 sessions. Experience the sessions anytime,anywhere! Create a username and password, browse sessions, stream or download the entire session!
$199.00Post Conference: $395
$495.00Post Conference: $595
$199.00Post Conference: $395
$249.00Post Conference: $445
Pre-order your online library subscription to the session recordings by March 2, 2015 and take advantage of the special pre-conference rates!
To Pre-Order Online Library visit: www.prolibraries.com/amdaTo Pre-Order DVD-ROM call: 1-800-679-3646
on
KENTUCKY INTERNATIONAL CONVENTION CENTER
Pre-Order &
Save! CME/CMD
Credit Available!
™
Michael Yao, MD, CMD

CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 11
An estimated 690,000-plus adults in the United States suffer an ischemic stroke annually, and an
additional 240,000 experience a transient ischemic attack.
The good news is that the cur-rent estimated annual rate of future stroke (3%-4%) is historically low, thanks to preventive measures, accord-ing to the new “Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic
Attack: A Guideline for Healthcare Professionals.” The updated guide-line (Stroke 2014;45:2160-236), gives evidence-based recommendations on secondary stroke prevention as well as primary prevention in those who have suffered a TIA.
In the guideline, the American Heart Association and the American Stroke Association address scenarios ranging from general risk factor modification to specific circumstances, such as myocar-dial infarction and thrombus, cardiomy-opathy, and arterial dissection.
One recommendation is to consider adding clopidogrel 75 mg/day to aspi-rin for 90 days in patients with a recent (within 30 days) stroke or TIA attribut-able to high-grade stenosis (70%-99%) of a major intracranial artery, an alternative therapy to statins and antiplatelet ther-apy. Other new recommendations stress nutrition. One item suggests perform-ing a nutritional assessment for patients with a history of ischemic stroke or TIA.
After having experienced an acute neurologic event, many patients and their families are highly motivated to
make whatever changes are necessary to prevent a future, potentially catastrophic stroke. Reduction of sodium from 3.3 g/day to 2.5 g/day or less is reasonable, according to the guidelines, although lowering intake to less than 1.5 g/day will lower blood pressure even further.
The new guideline also suggests coun-seling patients to follow a Mediterranean-type diet – emphasizing whole grains, fruits, vegetables, nuts, olive oil, legumes, fish, poultry, and even low-fat dairy products – instead of the traditional low fat diet. CfA
A. Maria Hester, MD, is a hospitalist with Baltimore-Washington Medical Center.
SAN DIEGO – Although doctors in recent years have done a good job catch-ing severe sepsis, lesser cases are falling through the cracks and ultimately prov-ing fatal, according to a retrospective database study.
That’s probably the main reason inves-tigators at Kaiser Permanente Northern California found that up to half of hos-pital deaths are sepsis-related. Of 14,206 adult inpatient deaths at KPNC hospi-tals between 2010 and 2012, 36.9% had sepsis-related codes. When the team included patients without sepsis codes but with evidence of both infection and acute organ failure – implying sepsis – the number rose to 55.9%.
Most patients had indications of sepsis at admission, and patients with initially less severe sepsis made up the majority of sepsis deaths. About 56% of sepsis-related deaths were in peo-ple with normal blood pressure and normal or intermediate serum lactate levels (< 4 mmol/L) on admission. Patients who met the criteria for early goal-directed therapy at admission, but for whatever reason did not get it, accounted for 21% of the deaths ( JAMA 2014;312:90-2).
The story was similar when the team looked at 143,312 deaths in the 2010 Healthcare Cost and Utilization Project Nationwide Inpatient Sample, which captures about 20% of U.S. community hospitals: 34.7% had sepsis codes, and 52% had codes or evidence of both infection and acute organ failure.
Sepsis could have been the final com-mon pathway in already-ill patients, but the numbers hint that, at least in some cases, sepsis that could have been extin-guished early got out of hand before it was recognized.
The Surviving Sepsis Campaign and other efforts “have had a huge impact on how we treat the most severely ill sepsis patients. We’ve seen about a halving of mortality in the past 15 years. Now we need to broaden our perspective to focus intervention on the less severely ill, who tend to be less severe up front and under identified,” said lead investigator Vincent Liu, MD, with the KPNC division of research, Oakland, CA.
Based on the results, KPNC has started applying its sepsis bundle to patients with intermediate-lactate lev-els, “but there is very limited data about the benefit of bundle care in less severe sepsis patients, so we are still tracking
our outcomes,” he said. There’s also a culture shift involved, which includes heightening clinician awareness, updat-ing communication protocols, and other measures, Dr. Liu said, in pre-senting the results at an international conference of the American Thoracic Society.
There is a role for more research dol-lars as well, and education efforts to make the public aware of sepsis and the need for early intervention, similar to what’s been done for stroke, he said.
The work was funded by the Kaiser Foundation, the Department of Veterans Affairs, and others. One author disclosed personal fees from Pfizer, MedImmune, Eli Lilly, Ferring Pharmaceuticals, and Roche Diagnostics. Dr. Liu and the other authors said they had no financial disclosures. CfA
M. Alexander Otto is with the Seattle bureau of Frontline Medical News.
Stroke guidelines Worthwhile
Less-Than-Severe Sepsis not Recognized in Time
By a. MaRIa HeSTeR, Md
By M. aleXandeR oTTo
Advance, Inspire and Educate the Caregivers of Tomorrow
Your donation to help educate and inspire our PA/LTC providers will benefit our aging population for years to come. It’s only with your support that the AMDA Foundation can continue to recognize and uplift our future leaders and caregiving facilities that exemplify excellence. So please, donate today to the AMDA Foundation’s Annual Giving Campaign for a better future!
Visit www.amdafoundation.org and donate today.
Support the AMDA Foundation’s Annual Giving Campaign
Make a Donation to the AMDA Foundation Today
The AMDA Foundation is a non-profit organiza-tion recognized as a public charity, an exempt or-ganization under Section 501(c)(3) of the Inter-nal Revenues Code. Gifts or contributions to the AMDA Foundation are deductible as charitable contributions for federal tax purposes to the full-est extent of the law.
Editor’s NoteThis 50-plus-page set of guidelines is very comprehensive and does add a lot of practical, nuts-and-bolts guid-ance for those of us who look after stroke and TIA patients. But I would reiterate that the most important guideline in nursing homes is to be sure that acute neurological symp-toms are considered an emergency – by all staff and all clinicians.
Unless your patient is definitely not a candidate for thrombolysis, the 911 system should be activated immedi-ately. This is one situation where it’s not acceptable to wait 20 minutes for a doctor to call back. We should educate and remind our personnel about the importance of time in a “brain attack” and empower them to use whatever avenues are neces-sary to ensure prompt attention in a stroke-protocol emergency department.
—Karl Steinberg, MD, CMD Editor in Chief
There is a role for ... education efforts to make the public aware of sepsis and the need for early intervention, similar to what’s been done for stroke.

12 • CARIng FoR The AgeS JAnuARy 2015
Vascular dementia, which is much more common than Alzheimer’s disease in patients with chronic kid-
ney disease, impairs executive function and is associated with anatomic white matter brain disease. Executive function is the cognitive domain concerned with attention, processing speed, reasoning, planning, and problem solving. Clinicians tend to miss the presence of cognitive impairment in patients with CKD because they typically rely upon the Mini-Mental State Examination (MMSE) to screen for impaired cognition. And the MMSE focuses on memory difficulties, which are more common in Alzheimer’s disease, rather than the more subtle domain of executive function, he explained.
“We’re trying to teach [CKD patients] about complex topics such as fluid restriction, medication management, and salt intake, and you wonder if it just goes in one ear and out the other
because they’re not able to process these complicated issues,” observed Daniel Weiner, MD, a nephrologist at Tufts University, Boston.
Dr. Weiner was coauthor of a recent cross-sectional cohort study in which 314 hemodialysis patients at six Boston-area hemodialysis units completed a comprehensive battery of neuropsy-chological tests assessing memory and executive function. The patients scored markedly worse than general popula-tion norms on executive function, but not on memory performance. Moreover, impaired executive function was highly prevalent even in patients with a nor-mal MMSE of 24 or more. The take-home message: be cautious in using an MMSE score of less than 24 to screen for cognitive impairment in dialysis patients (Neurology 2013;80:471-80).
Moderate to severe cognitive impair-ment is also prevalent in patients on peritoneal dialysis, as shown by investi-gators at the University of Minnesota.
They gave a battery of nine validated neuropsychological tests to 51 perito-neal dialysis patients, 338 hemodialy-sis patients, and 101 controls without CKD who were matched for age and comorbid conditions. Of the peritoneal dialysis cohort, 31% had severe cognitive impairment, as did 37% of the hemodi-alysis group and 13% of controls. In an adjusted logistic regression model, peri-toneal dialysis was associated with a 2.5-fold increased risk of moderate to severe global cognitive impairment, compared with the no-CKD controls. Hemodialysis patients had a similar 3.16-fold increased risk (Am J Kidney Dis 2011;57:612-20).
“That’s a remarkably high prevalence: one-third of dialysis patients in a moder-ately well educated Minnesota population with access to medical care performed poorly enough on a neurocognitive bat-tery to be classified as severely cognitively impaired, meaning they flubbed on two different domains of cognitive function,” Dr. Weiner commented.
The effect of dialysis itself upon cog-nition is a matter of continuing con-troversy. Although some nephrologists posit that a more intensive dialysis regi-men would result in improved cognitive performance, that hasn’t been borne out in analyses to date (Kidney International 2011;79:14-22).
“This suggests that the cognitive impairment we see in dialysis patients isn’t related to the dialysis dose. It’s not related to retained solutes, but is more related to the – for lack of a better word – bad humors patients have been exposed to for many years and which have put them into a situation where they require dialysis,” according to Dr. Weiner.
“We have patients that drop their sys-tolic blood pressure by 20, 30, 40, even unfortunately 80 mm Hg during dialysis. You can’t imagine that this is good for you. We’re inducing transient micro-vascular ischemia, which is ultimately manifest structurally: in the kidney we get fibrosis, in the brain we get white matter disease,” he said.
Cognitive dysfunction is associated with increased mortality risk even in CKD patients who are not dialysis depen-dent. In an analysis of National Health and Nutrition Examination Survey III data, non-dialysis dependent CKD patients in the lowest quartile in terms of cognitive score had a twofold increased risk of mortality, compared with those in the highest quartile (Am J Nephrol 2012;35:49-57).
Chronic kidney disease as defined by an estimated glomerular filtration rate below 60 mL/min/1.73 m is also a cardiovascular disease risk equivalent for stroke. Dr. Weiner and coworkers showed that the stroke rate in patients with CKD but no known CVD is ele-vated to roughly the same extent as in patients with known CVD but no CKD (Am J Kidney Dis 2006;48:392-401).
More recently, Dr. Weiner and his col-leagues showed in a brain MRI study that hemodialysis patients not only have far more white matter disease and cerebral atrophy than controls without kidney disease, they also have a high prevalence of previously unrecognized strokes. The cross-sectional study involved 45 hemodialysis patients and 67 controls, all without a history of stroke. Impressively, 18% of the hemodialysis patients had evidence of a small-vessel infarction on MRI and another 8% had a large-vessel infarction (Am J Kidney Dis 2013;61:271-8).
The high rate of often subtle cogni-tive impairment among dialysis patients points to the need for alternative patient education strategies. In order to reinforce his educational messages, Dr. Weiner makes an effort to convey the same extensive information to fam-ily members and other primary care-givers that he provides to the patients themselves.
He reported having no financial conflicts. CfA
Bruce Jancin is with the Denver bureau of Frontline Medical News.
NEW YORK – Valproic acid might be effective for treating hyperactive delir-ium, results of a small, retrospective study suggest.
Among 16 patients with hyperactive delirium, 13 had complete resolution of delirium according to the DSM-IV-TR criteria, reported Yelizaveta I. Sher, MD, an instructor in psychiatry and behav-ioral science at Stanford University, CA.
“You should definitely consider this medication where antipsychotics are
ineffective or there are concerns about side effects from antipsychotics, and you need rapid control of agitation,” Dr. Sher said at the annual meeting of the American Psychiatric Association.
Antipsychotic agents are usually first-line pharmacological therapies for delirium, but these agents are associated with adverse events such as prolongation of the QT interval, extrapyramidal side effects such as akathisia, tremors, and, less frequently, the neuroleptic malig-nant syndrome, Dr. Sher said.
Antipsychotics also are less-than-ideal agents for treatment of agitation associ-ated with acute delirium after traumatic brain injury or from alcohol withdrawal, she added.
Valproic acid is approved in the United States for seizures, migraine prophy-laxis, and acute manic or mixed bipolar episodes. It often is used off-label for treatment of agitation, neuropathic pain, and personality disorder, accord-ing to Dr. Sher. In addition, its use has been explored in agitated patients with dementia, agitation in traumatic brain injury, and corticosteroid-induced mania.
The use of valproic acid has been associated with mild blood dyscrasias, abnormal liver function tests, and, in patients with urea-cycle enzyme defi-ciencies, symptomatic hyperammo-nemia. Medication interactions with valproic acid include a decrease in blood levels of up to 80% when it is used with meropenem, and an increase in war-farin levels when valproic acid is used with the anticoagulant. Valproic acid also can decrease clearance of carbam-azepine, lamotrigine, nortriptyline, and amitriptyline.
Dr. Sher and her colleagues con-ducted a retrospective study of charts
for patients with episodes of hyperac-tive delirium who were treated with adjunct valproic acid by a consulting or liaison psychiatrist on the psychosomatic medicine service at their center from Aug. 1, 2011, through Aug. 31, 2012. All the patients had hyperactive or mixed delirium as defined by Dr. Benjamin Liptzin’s criteria (Am. J. Psychiatry 1991;148:454-7).
Dr. Sher and her associates reviewed daily notes from the primary intensive care unit team; daily mental status examination results; daily medication use and doses of psychotropic medica-tions, sedatives, and related medications; daily lab data; descriptions of agitation; and important clinical events such as the use of restraints and extubation.
They identified 16 patients (14 men and two women) treated for hyperac-tive delirium, all but three of whom were treated in the ICU. Of this group, 15 patients had received multiple drug treatments for delirium and/or agitation prior to valproic acid use.
The average dose of valproic acid used on days 2-5 was 1,133-1,258 mg per 24 hours in divided daily doses.
Thirteen patients had complete res-olution of delirium, at an average of 7.2 days from the start of valproic acid. Two patients had resolution of delirium within 2 days, four within 3 days, two within 4 days, one within 5 days, and the remaining four patients at 10, 12 (two patients), and 31 days.
In all patients, agitation was mark-edly decreased as rated by mental status examination, agitation scale ratings, and reduced need for sedatives. CfA
Neil Osterweil is a Frontline Medical News freelance writer based in Boston.
By BRUCe JanCIn
By neIl oSTeRWeIl
Chronic Kidney Disease Linked to Cognitive Impairment
old Standby Valproic Acid effective Against hyperactive Delirium
Editor’s NoteAlthough this was a tiny, retrospec-tive study in which it’s not clear why valproate was used in place of anti-psychotics (the standard treatment for delirium) in the first place, it is very intriguing. We all know that delirium is really bad, and most of us aren’t fond of antipsychotics, so it’s certainly worth considering valproic acid (or its better tolerated version, divalproex) for agitated delirium as we await the results of larger and better-designed studies.
The drug is available in intrave-nous as well as oral formulations. It is pretty sedating in the elderly, and many of us have used it in the past for dementia-related agitation (a use that has no real evidence to support it and has fallen out of favor). But delirium is a different animal, and it would be great to have something quick, easy, and inexpensive in our armamentarium. Better yet would be if it were also evidence-based.
—Karl Steinberg, MD, CMD Editor in Chief

CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 13

14 • CARIng FoR The AgeS JAnuARy 2015
no program or concept has had a deeper, more positive impact on care transitions in skilled
nursing facilities than the Interven-tion to Reduce Acute Care Transfers (INTERACT) initiative. The goal of INTERACT is to improve care and reduce the frequency of potentially avoidable transfers to the acute hospital. Such transfers can result in numerous complications of hospitalization and billions of dollars in unnecessary health care expenditures.
INTERACT was conceived as a qual-ity improvement program, although it is often implemented as a readmis-sion reduction program in the long-term care clinical environment. There are three basic types of INTERACT tools: communication tools, care paths or clinical tools, and advance care planning tools. The first steps in the INTERACT process are designed to improve the early identification of resident problems, promote systematic resident assessment for those changes, and guide efficient documentation of the work of the bedside nursing team. Next, scripted communication about resident status changes in skilled nurs-ing facilities encourages an efficient, accurate, clinical interchange with the attending clinician. These steps allow caregivers to intervene in acute resident change of conditions, resulting in on-site care that reduces the frequency of acute hospital transfer.
Joe Ouslander, MD, PhD, professor of clinical biomedical science and senior associate dean for geriatric programs, and
his INTERACT team at Florida Atlantic University, including Jill M. Shutes, GNP-BC, and Janelle Miller, RN, clinical product line manager at PointClickCare have strived to expand the availability and impact of INTERACT. Here, Ms. Shutes and Ms. Miller, the authors of this col-umn, describe a recent innovation to integrate the program into the electronic medical record.
INTERACT Is a HITA substantial reduction in hospitaliza-tion rates has been associated with implementation of the INTERACT quality improvement program using the paper-based clinical practice tools (INTERACT 3.0). There is a compel-ling opportunity to further increase the impact of INTERACT by embedding INTERACT 3.0 tools into nursing home health information technology (HIT) via standalone or integrated clinical decision support systems. This article highlights the process of embedding INTERACT 3.0 tools from paper to nursing home HIT.
INTERACT is an example of a qual-ity improvement intervention designed to support clinical decision making, as well as to facilitate the identification, evaluation, documentation, and com-munication about changes in resident status. This is accomplished by collect-ing information about baseline care plan goals and condition-specific clini-cal information when a change in status occurs. The INTERACT 3.0 (origi-nally II) care paths and other tools, incorporate information from various
sources including best practices, clini-cal practice guidelines, and input from front line nursing home providers and national experts in long-term care.
Saves Time, Streamlines ProcessesMany LTC facilities using electronic health records have already obtained a license agreement with Florida Atlantic University to embed INTERACT within their HIT. Some of the reported chal-lenges associated with using paper-based INTERACT 3.0 tools may be improved when these tools are incor-porated into nursing home HIT. Use of an electronic format will enable staff to spend less time updating data, provide greater access to automated information, reduce the time needed to track down information from differ-ent sources, minimize the time spent performing manual calculations, and keep tasks on track through remind-ers or prompts noting when specific actions should be taken. Simply put, it will make it easier for front line staff to do the right thing at the right time when a patient’s clinical condition has changed.
Translating INTERACT 3.0 clinical decision support tools from paper to HIT in the nursing home has spotlighted steps along the way: the process of inte-grating these tools; the discovery that paper-based tools don’t always translate (in their current form) into HIT; and the team approach that is critical in the implementation phase.
Embedding INTERACT within HIT will:
▶▶ Trigger and document a response to a change in condition (CIC) noted by a “stop and watch” warning.
▶▶ Provide real-time decision support to nurses performing evaluation of a CIC.
▶▶ Incorporate alerts for nurses about notifying clinicians based on decision support.
▶▶ Link INTERACT compatible patient order sets.
▶▶ Efficiently use data to generate trans-fer information when needed.
▶▶ Track key outcomes over time and benchmark results.
▶▶ Summarize root cause analyses over time.
▶▶ Track specific core process measures.
Turning Paper to Data To refine the process, the INTERACT team analyzed paper tools at the data-element level to gain understand-ing of each element’s use; these were compared against same or similar ele-ments already available in the system. Redundancies and inconsistencies were
highlighted during this process. The goal was to minimize additional documenta-tion burden and to leverage existing doc-umentation to the extent possible. This process was very enlightening for the INTERACT team, as the original tools were developed independently of each other. They were developed by obtaining input from different team members and experts, with different “language” used to describe the same sign, symptoms, or process. Each tool was mapped onto an Excel spreadsheet. Inconsistencies in the paper-based program were identified and corrected. After the data elements from paper tools were refined, the next step was to translate the clinical decision support tools from paper to HIT for use in actual practice. This included develop-ing the content, formatting the informa-tion, and establishing the algorithms or rules that will produce alerts, reminders, and reports.
The INTERACT quality improve-ment intervention and related paper-based tools have demonstrated the potential to enhance the detection, management, and communication of acute change in condition among nurs-ing home residents. For example, unlike standalone paper-based tools that rely on employees to follow proper policy when notifying the clinician about a subtle change in condition, INTERACT automatically sends an alert to the nurse when a subtle change has been detected by a nursing assistant, which prompts the nurse to react to that alert within the system.
Developing INTERACT 3.0 clinical decision support tools in an interopera-ble format that would enable widespread dissemination and integration into vari-ous nursing home HIT products, could lead to sustainable improvement in resident and clinician process and out-come measures, including a reduction in unplanned transfers and potentially avoidable hospital admissions.
For information on how to obtain a license for INTERACT please visit the website at http://interact.fau.edu/. CfA
Jill Shutes, GNP, is a research associate at Florida Atlantic University. Janelle Miller, RN, BSN, is clinical product line manager at PointClickCare. Patient Order Sets has provided support through FAU for Dr. Ouslander and Ms. Shutes.
Dr. James Lett II, MD, CMD, chairman of the AMDA Transitions of Care Committee, coordinates this column. You can comment on this and other columns at www.caringfortheages.com, under “Views.”
InTeRACTing With the electronic Medical Record
By James Lett II, MD, CMDCaring Transitions
Tools for TransitionsImproving care transitions has long been a priority for PA/LTC practitioners, as they have sought to enhance communication between care settings and support patients and families as individuals move through the care continuum. AMDA has several tools, developed by interdisciplinary teams and based on clinical evi-dence, to support care teams and facilities as they improve care transitions:
▶▶ Acute Change of Condition Clinical Practice Guideline. This document details a person-centered approach to recognition, assessment, treatment, and monitor-ing of acute condition changes designed to result in better management of these events and fewer transfers to hospitals and other acute-care settings. For more information, go to www.amda.com/tools/guidelines.cfm#acoc.
▶▶ Transitions of Care Clinical Practice Guideline. This guideline offers an array of steps, tools, and resources to enable smooth and effective care transitions as patients move from setting to setting. This guideline is available as a free down-load. For more information, go to www.amda.com/tools/guidelines.cfm#toc.
▶▶ The Know-It-All-Series includes several tools to encourage communication, documentation, and support that improve transitions and care as patients move between the PA/LTC facility and the hospital, home, or other setting. Included in the series are: Caregiver’s Communication Guide – Caring for the Older Adult in the Community; Know-It-All Series: Tools to Reduce Unnecessary Transitions to Hospitals; Know-It-All Before You Call Data Collection System; Know-It-All When You’re Called Diagnosing System; and Know-It-All Set (includes both data cards and diagnosing system). For more information, go to www.amda.com/tools/kia.cfm.

CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 15
Fecal incontinence is a devastating and isolating condition. Sales of adult diapers are a $7 billion global
market and the fastest-growing house-hold products business. Which is where a lot of our patients with this condition remain – at home.
Fecal incontinence (FI) is characterized by continuous or recurrent uncontrolled passage of fecal material. The preva-lence may be as high as 15%. Risk factors include physical disabilities, dementia, diabetes, urinary incontinence, chronic diarrhea, and multiparity. One-third of patients will talk to us about it. Which for some of us may be suitable, given our inability to offer good treatments.
If patients do mention it, evaluation involves taking a good history. We need to differentiate incontinence from fecal urgency and frequency. Anorectal exam-ination should look for a bilateral anal wink (absence suggests nerve damage). Some form of endoscopic examination should be performed in most patients. Further evaluation and referral will be based upon findings.
Treatment includes improving stool consistency (e.g., fiber for loose stool) and reducing frequency (e.g., loperamide for diarrhea). Hyoscyamine may be help-ful for post-meal leakage. Scheduled defecation and amitriptyline may be of
benefit to some patients. However, sig-nificant anticholinergic effects may limit the utility of these medications in the geriatric population.
Henri Damon, MD, of Hospices Civils de Lyon, France, and colleagues conducted a multicenter study of peri-neal retraining for FI (Dig Liver Dis 2014;46:237-42). The standardized inter-vention included perineal retraining
and biofeedback. The protocol was based upon 20 sessions of 30 minutes performed within a 4-month period. Eighty patients were included in the control group, with 77 in the biofeed-back group.
The success rate was significantly higher in the biofeedback group (57% vs. 37%; P < .021). Stool frequency, leak-age, and urgency significantly decreased.
Perineal retraining was significantly associated with a higher chance of self-rated improvement.
The take-home message is that peri-neal retraining is an effective compo-nent of FI treatment. Combining it with improved perianal skin hygiene, bowel habit ritualization, and the addi-tion of fiber as a bulking agent and loperamide for diarrhea offers the best hope for patients with this challenging condition. CfA
Jon O. Ebbert, MD, is professor of medicine, a general internist at the Mayo Clinic in Rochester, MN, and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. The opinions expressed in this article should not be used to diagnose or treat any medical condition.
By Jon o. eBBeRT, Md
gaining Control over Fecal Incontinence
AMDA Foundation’s2015 Caring Canines Calendar
is here!
Our 12-month, full-color calendar features dogs and other furry friends with their human friends selected from long-term care facilities from across the country. It’s a perfect holiday gift and a great way to support the Foundation’s long-term care research and education projects.
*Discounts available when purchasing multiple copies
Order Now!Only
$16.95*(plus shipping)
Find out more at www.amdafoundation.org/canines
PA/LTC Perspective“Many staff and caregivers think fecal incontinence is just a result of aging, which is incorrect,” said T.S. Dharmarajan, MD, vice chair of the department of medicine at Montefiore Medical Center’s Wakefield Campus and clinical director of the division of geriatrics of Montefiore in New York. “The older the patient and the longer the stay in the nursing home, the more likely the preva-lence of fecal incontinence is,” he told Caring for the Ages.
He emphasized the need for staff to be aware of and knowledgeable about risk factors. “They also must understand the importance of the ability to trans-fer between bed and chair (and the toilet), as data suggests that the inability to transfer correlated with occurrence of more fecal incontinence,” he said. Dr. Dharmarajan added that prompted defecation helps as a conservative approach in ambulatory and responsive residents. “While dietary modification, such as increased fiber and fluids intake, as well as increased activity, are the best means of addressing chronic constipation, these measures are less effective in [the frail elders] in long-term care,” he said.
Ultimately, he said, “The best means to address the issue are to assess every resident individually using a multifactorial and interdisciplinary approach including assessing mental and physical capacity and [to] initiate a care plan to address the predisposing factors in each individual.”
For more information, see Dr. Dharmarajan’s AMDA webinar, “A Practical Approach to Incontinence and Constipation” at AMDA’s e-University. Visit www.amda.com/cmedirect/#web.
[Perineal training] combined with improved perianal skin hygiene, bowel habit ritualization, and the addition of fiber and loperamide is an effective option.

16 • CARIng FoR The AgeS JAnuARy 2015
CNA Scope of PracticeCertified nurse aides (CNAs) in nurs-ing homes have an expanded scope of practice in 11 states, according to a study led by Tara L. McMullen, MPH, of the University of Maryland in Baltimore. Researchers looked at state-by-state differences in tasks that nurses may delegate to CNAs.
“By law, some of what is required must be currently performed by a nurse (LPN or RN). With the increasing complexity of care needs of older adults, there will not be a sufficient number of registered nurses to provide one-on-one care, nor is that practical,” said fellow researcher Barbara Resnick, PhD, CRNP, FAAN, FAANP, of the university’s school of nursing.
Using data from all 50 states’ regu-latory offices or health care services agencies, the researchers compared the tasks each state allows CNAs to perform against the Code of Federal Regulations (42 CFR § 483). The code lists tasks that CNAs may perform in nine areas: per-sonal care skills, safety/emergency pro-cedures, basic nursing skills, infection
control, communication and interper-sonal skills, care of cognitively impaired residents, basic restorative care, mental health and social service needs, and resi-dents’ rights.
All 50 states allowed CNAs to perform the nine basic nursing care tasks from the 42 CFR § 483, whereas 11 states allowed for what could be considered expanded scope of practice for CNAs, the researchers found. Specifically:
▶▶ Two states let CNAs participate in medication management, such as docu-menting a resident taking medications, and assisting with the placement of pills and medication into the resident’s mouth.
▶▶ Nine allowed CNAs to manage wound care and to reposition residents to facili-tate wound care and healing.
▶▶ Nine allowed CNAs to manage cathe-ter care tasks and catheter and tube care, such as cleaning and replacing catheters.
▶▶ Three allowed CNAs to manage medi-cal information, such as communicating medical information given from one pro-vider to another or to a family member.
“There is no reason to believe patients are in jeopardy and that is exactly what we were trying to demonstrate; in states in which expanded care is provided there is no evidence of harm,” Dr. Resnick said.
▶▶ Source: Certified Nurse Aide Scope of Practice: State-by-State Differences in Allowable Delegated Activities – McMullen TL, et al.
Frailty CostsA 12-month multifactorial intervention in frail individuals provided better value for its cost than usual care, especially for those who were very frail, according to a cost-effectiveness study.
Using data from the Frailty Intervention Trial (FIT), Nicola Fairhall, PhD, of the University of Sydney, Australia, and col-leagues compared the cost effectiveness of an interdisciplinary intervention with usual care in community-dwelling indi-viduals aged 70 years and older who met the Cardiovascular Health Study (CHS) frailty criteria. Dr. Fairhall and her col-leagues found that such an approach reduced degree of frailty and decreased disability in older people.
The researchers randomized partici-pants to receive usual care, or a 12-month intervention in which professionals from different health disciplines treated vari-ous components of frailty. Among the 216 individuals who completed the study, the prevalence of frailty was 14.7% lower in the intervention group vs. the control group at 12 months. The team found that there was a 30% probability that the inter-vention was both cost-saving and effective in all groups, and a 63% probability in the very frail subgroup.
▶▶ Source: Economic Evaluation of a Multifactorial, Interdisciplinary Intervention Versus Usual Care to Reduce Frailty in Frail Older People – Fairhall N, et al. CfA
Jeffrey S. Eisenberg, a freelance writer in the Philadelphia area, compiled this report.
The coming senior tsunami brings with it a wave of hepatitis C. According to the Centers for Disease Control and Prevention, people born between 1945 and 1965 are five times more likely than other adults to be infected with the hepatitis C virus. In fact, 75% of adults with hepatitis C were born during those baby boom years.
The CDC recommends hepatitis C testing for people in this age group. Early diagnosis and treatment can help prevent liver damage, cir-rhosis, and even liver cancer. The CDC estimates that one-time blood testing for everyone born between 1945 and 1965 could prevent more than 120,000 deaths.
Why should you care about this? Hepatitis C is a bloodborne contagious liver disease that is potentially fatal. It can be mild and last weeks, or serious and last a lifetime. It can also be cleared from your body with appropriate treatment.
People with this disease often have no symptoms and can live for decades without feeling sick. Symptoms one might experience soon after they’ve been infected include fever, fatigue, and poor appetite. Other signs include nausea and vomiting, stomach pain, muscle or joint pain, abnormal urine or bowel movements, and yellowing in the skin or eyes. Some people may have symptoms within 2 weeks of infection; others may not notice signs of the disease for 10 years or more.
Various blood tests are used to test for hepatitis C. Generally, the first step is a screening test to show if a person has developed hepatitis C antibodies, substances in the blood the body produces in response to a virus. A positive antibody test means that a person has been exposed to hepatitis C, not necessarily that a person has it. However, if an antibody test is positive, the doctor likely will order a second test to confirm whether the virus is still present and if the person has chronic hepatitis C.
There are two types of hepatitis C – acute and chronic. Acute hepatitis C clears on its own with-out treatment in about 25% of people. Treatment reduces the risk that the illness will go from acute to chronic for the other 75%. Chronic hepatitis C is long-term and can lead to serious problems, such as liver cancer or cirrhosis. Both types are treated with the same medications, although some individuals have fewer side effects than others. There are several drugs now available to treat hepatitis C, and most are combined with ribavirin and interferon.
People with chronic hepatitis C should see a health care practitioner regularly. For most people, peri-odic blood work and ultrasound studies of the liver should be done.
▶▶ Questions to Ask Your Practitioner• Should I be tested for hepatitis C? • How could I have it and not know it?• Can I live a normal life with this disease? How is it treated? What lifestyle changes may be necessary?
▶▶ What You Can Do:• Talk to you practitioner about getting tested for hepatitis C.• Make any lifestyle changes (e.g., reduce alcohol intake) your practitioner recommends.• If you have the disease, alert individuals who you might have infected and urge them to get tested.• If you have chronic hepatitis C, tell all of your practitioners; check with them before taking any over-the-counter or complementary/alternative medications because some can damage the liver.
Caring for consumers
Testing helps Baby Boomers navigate Threat of hep CEric Tangalos, MD, CMD, professor of medicine at the Mayo Clinic in Rochester, MN, talks about the importance for baby boomers to be tested for Hepatitis C and what it means to have the illness.
™
Caring for thE agEs is the official newspaper of AMDA – The Society for Post-Acute and Long-Term Care Medicine and provides post-acute and long-term care professionals with timely and relevant news and commentary about clinical developments and about the impact of health care policy on long-term care. Content for Caring for thE agEs is provided in part by Frontline Medical News and by writers, reporters, columnists, and editorial advisory board members under the editorial direction of Elsevier and AMDA.
The ideas and opinions expressed in Caring for thE agEs do not necessarily reflect those of the Association or the Publisher. AMDA – The Society for Post-Acute and Long-Term Care Medicine and Elsevier Inc., will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services mentioned herein.
©2015 AMDA – The Society for Post-Acute and Long-Term Care Medicine.
▶▶ For More Information:• Hepatitis C Information for the Public: www.cdc.gov/hepatitis/c/cfaq.htm• Hepatitis C: http://www.who.int/mediacentre/factsheets/fs164/en/
From the January Issue of JAMDAJournal Highlights

CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 17
BOSTON – An automated system for monitoring the symptoms of patients in home hospice and supporting their care-givers with coaching can both improve patient comfort and relieve at least some of the stress on the caregiver, said inves-tigators in a pilot program.
In a prospective, randomized con-trolled trial, caregivers assigned to symptom care by phone, in which they received automated coaching tailored to the specific situation, had better over-all vitality, and the patients they cared for had less fatigue and anxiety than caregiver-patient pairs assigned to usual care, reported Kathi Mooney, RN, PhD, professor of nursing at the University of Utah College of Nursing, Salt Lake City.
“The family inclusion in hospice care, the philosophy around that, offers the opportunity to extend PROs [patient-reported outcomes] to FCROs [family caregiver reported outcomes]. We call that an opportunity to use electronic monitoring to monitor a family,” she said at the Palliative Care in Oncology Symposium.
Dr. Mooney and her colleagues have previously reported on the use of auto-mated symptom monitoring for sup-port of patients undergoing ambulatory chemotherapy. In the current study, she described its application in home-based end-of-life care to support both the patient and the caregiver.
The investigators recruited 319 cancer patient/caregiver dyads from 12 hos-pices in Illinois, Massachusetts, Oregon, and Utah. The mean age of the patients was 72 years, and the mean age of care-givers was 59 years.
The caregivers were randomly assigned either to the symptom care by phone (SCP) system or to usual care. The SCP system is an automated sys-tem in which caregivers phone in to report the patient’s symptoms and their own levels of stress, anxiety, etc., and receive automated responses based on the severity of symptoms and number of days reported without relief. The sys-tem offers both patient care and self-care strategies and identifies and reinforces issues that should be addressed by con-tacting the hospice team. At the end of the call, the data are sent to the nurse, including alerts to matters that require prompt attention.
Caregivers in each group made daily automated monitoring calls to report one or more of 11 patient symptoms and five caregiver symptoms on a 0-10 scale and to report the patient’s and their own distress about the symptoms. “We have developed algorithms to pro-vide just-in-time, tailored suggestions related to the pattern that they have reported,” Dr. Mooney said.
Data reported by caregivers in the con-trol (usual care) group were recorded but not acted upon, whereas data reported by those in the SCP intervention group
triggered the automated coaching and hospice nurse alerts for moderate to severe symptoms.
“People in the usual care group under-stood that they were just contributing symptom information, and they were told on every call and at consent that if they had any concerns to call their hos-pice nurse,” Dr. Mooney said.
For clinicians, the automated system triggers an alert at preset thresholds of severity (4-10), as well as trend alerts. Hospice nurses have online and mobile access to the alert website, where they can view a report of symptoms over the previous 24 hours, and review graphs of symptoms over time to see trends. The nurses were instructed to log that they had seen the alert and what their planned action was, which was left to their professional judgment.
The average length of the calls was 7 minutes, 4 seconds for the usual care group, and 7 minutes, 59 seconds for the intervention group. Control group care-givers completed 59% of expected calls, and those in the intervention group completed 64%.
Reported symptoms present in more than 50% of patients included fatigue (88.8%), pain (60.2%), eating/drink-ing problems (76.6%), difficulty think-ing (69.6%), anxiety (67.6%), negative mood (67.3%), bowel problems (61%), and trouble sleeping (58.3%).
Among caregivers, 73.3% reported fatigue, 66.7% anxiety, 61% trouble sleeping, and 57.1% negative mood.
In a mixed-effects model looking at caregiver vitality – a composite of care-giver symptoms – the authors found that the severity of symptoms in the usual care group increased steadily over the course of hospice care, out to at least 91 days. In contrast, the sever-ity of symptoms among caregivers in the SCP group rose only slightly. The between-group difference was signifi-cant (P < .001).
Similarly, among patients the overall symptom severity scores were lower for those in the intervention group than for controls (P =.03). Additionally, the onset of benefit, defined as time to the first symptom-free day, was significantly earlier among patients in the SCP group (P < .02)
Patterns of patient fatigue during the last 8 weeks of life also favored the symptom-care intervention, Dr. Mooney noted.
The symposium was cosponsored by the American Academy of Hospice and Palliative Medicine, American Society of Clinical Oncology, American Society for Radiation Oncology, and Multinational Association of Supportive Care in Cancer.
The study was supported by the National Cancer Institute. Dr. Mooney reported having no relevant disclosures. CfA
Neil Osterweil is a Frontline Medical News freelance writer based in Boston.
By neIl oSTeRWeIl
Automated Support eases Patient, Caregiver Burden
onIN LONG-TERM CARE
M A RC H 1 9 -22 LOUISVILLE, KY KENTUCKY INTERNATIONAL
CONVENTION CENTER
AMDA
Save by registering under the Best Value Rate now — available for a limited time!
www.PALTCmedicine.org
201
5The 2015 Annual Conference will offer two special ticketed events that incur an additional fee. You MUST pre-register for these as space is limited. To register for one or both of these events, check the box next to the session title on the registration form.
Meet the Expert Breakfast Session – Movement Disorders in the Older AdultAward winning neurologist Pratap Chand, MD, DM, FRCP, will discuss the recognition, clinical features, and management of common movement disorders in the older adult including Parkinson’s disease, Chorea, Hemiballismus, Myoclonus, Asterixis, and Tardive dyskinesia.For more information, visit www.bit.ly/meethexperts.
Navigating Mood & Behavior Challenges in Long-Term Care: Strategies for Optimal OutcomesBack by popular demand, this workshop will pursue an evidence-based approach to effective interventions, utilizing case-based presentations, panel discussions, and participant handouts and practical tools including 3 AMDA CPGs.For more information, visit www.bit.ly/moodbehavior.
THE SOCIETY FOR POST-ACUTE AND LONG-TERM CARE MEDICINE ANNUAL CONFERENCE
™

N e w s F r o m t h e s o c i e t y™
18 • CARIng FoR The AgeS JAnuARy 2015
AMDA’s Choosing Wisely recom-mendations were featured promi-
nently in a recent Consumer Reports health special publication, “Advice for Caregivers: Treatments and Tests for Seniors,” a roundup of medical issues and tips to help patients and families make decisions about health care.
The report stated, “If you are caring for an aging relative or friend, you want to help all you can. You may urge the doctors to try every possible treatment. But the experts who care for older adults say you should be cautious.” In addition to AMDA’s Choosing Wisely recommendations, the report highlights other groups’ suggestions of interest to seniors and their family caregivers.
Access the Consumer Reports special publication at http://consumerhealthchoices.org/wp-content/uploads/2014/10/Choosing WiselyCaregiversRoundup-ER.pdf.
AMDA partnered with the ABIM Foundation in 2013 to participate in the Choosing Wisely campaign
to encourage con-versations among physicians, patients, and other health care stakeholders about medical tests and procedures that
may be unnecessary and could be harmful. AMDA has produced a list of five items (www.amda.com/tools/ChoosingWisely_5Things.pdf), including associated tools and resources. CfA
Consumer Reports highlights Choosing Wisely Recommendations
The countdown to AMDA’s 2015 annual conference is on, and
March 19-22 is quickly approaching. The 2015 program features leading experts and hot topics, including:
▶▶ Jason Karlawish, MD, will deliver the keynote address on Friday, March 20, entitled “How Are We Going to Live with Alzheimer’s Disease?” Dr. Karlawish is professor of medicine, medical ethics and health policy at the University of Pennsylvania and director of Penn’s Neurodegenerative Disease Ethics and Policy Program and associate director of the Penn Memory Center.
▶▶ Physician and author Louise Aronson, MD, MFA, will deliver the Anne-Marie Filken Lecture on Sunday, March 22. She will discuss and demonstrate how stories and data can be used for narrative advocacy,
bearing witness, teaching, and improving PA/LTC. She will provide examples and offer simple tips to help participants translate their exper-tise and experience into stories that inspire and persuade.
▶▶ Saturday’s General Session will focus on AMDA’s top policy issues for 2015. The program will also feature an update on AMDA’s competencies for attending physicians and a presen-tation about the impact of health care reform on post-acute/long-term care.
▶▶ The acclaimed day-long program, “Navigating Mood and Behavior Challenges in Long-Term Care Strategies for Optimal Outcomes” is scheduled for Thursday, March 19. Program Chair Eric Tangalos, MD, CMD, will lead a panel of experts who will discuss evidence-based approaches
Countdown to AMDA Annual Conference
Two General Session speakers at AMDA’s 2015 annual conference
are talented authors whose books have received rave reviews. Con-ference participants will have the opportunity to obtain signed books by keynote speaker Jason Karlawish, MD, and Anne-Marie Filkin lecturer Louise Aronson, MD, MFA, as part of the AMDA Foundation’s book auction. However, the Foundation needs you
to ensure the auction’s success. If you have signed or rare volumes or other interesting or unique books, please consider donating them to the Foundation for the auction. Other items, including works of art, toys and games, and DVDs, are also welcome.
To arrange your donation, contact the AMDA Foundation at [email protected] or 410-992-3134. CfA
Leave your Literary Legacy Through the Foundation
in action
If you don’t want to wait until July or travel to Baltimore, MD, to at-
tend the AMDA Core Curriculum on Medical Direction in Long-Term Care, you can complete part 1 of the course online between now and March 2 (register by Feb. 16) or be-tween April 6 and June 1 (register by May 18). Registrants must complete all 13 modules – including self-assess-ment questions and evaluations – dur-ing that time.
The program features an experi-enced faculty, including AMDA past presidents Alva S. Baker, MD, CMD, Karyn Leible, MD, CMD, and Matt Wayne, MD, CMD; as well as promi-nent society volunteer leaders Robert
G. Kaplan, MD, CMD, Jeffrey B. Burl, MD, CMD, and J. Kenneth Brubaker, MD, CMD. Topics include a variety of issues that practitioners must master to be effective PA/LTC medical directors, including medical information man-agement, financial issues, employee health and safety, the regulatory envi-ronment, emerging challenges and industry trends, and infection control.
After completing the 13 modules, registrants must participate in one of three scheduled live Q&A telecon-ference sessions. Part 2 must still be completed at the live program.
For more information about the online core program, visit www.amda.com/cmedirect/core-part-1.cfm. CfA
Late last year, the AMDA Foun-dation kicked off its fall giving
campaign, and Paul Katz, MD, CMD, board of directors chair, is focused on the organization’s strategic goals. “These goals frame our board calls and conversations, and are the corner-stone of our efforts as we plan pro-grams and projects moving forward.”
The four goals are: educate, mentor, inspire, and recognize future and cur-rent long-term care health professionals; promote financial stewardship; advance quality and improve care through the application of long-term care research; and enhance the global awareness of excellence in long-term care.
“When you make a donation to the Foundation, you help expand and enhance our Futures program to include an even richer curriculum and involve more participants, includ-ing nurse practitioners and physician assistants. You enable visionary facility teams to complete innovation quality improvement projects that improve care and maximize quality of life,” Dr. Katz said. “You also recognize innovative leaders through our awards program and inspire others to follow their example. And you help facilitate
international collaboration, such as the participation of a Korean delegation at last year’s annual conference and the appearance of [Jos] Schols, MD, PhD, from Maastricht University in the Netherlands at this year’s meeting.”
And there is more to come. For example, the Foundation is focusing on public education and is sponsoring a town hall meeting for consumers in Louisville.
“AMDA is about the nuts and bolts of post-acute/long-term care medicine. The AMDA Foundation is the heart and soul,” said Dr. Katz. “The Foundation’s programs inspire careers, encourage creative projects and research that addresses the most inventive of ‘what ifs,’ validate and honor practitioners’ tireless efforts to make a difference, bring together veteran and new prac-titioners as colleagues and friends, and touch lives in many ways every day.”
Visit www.amdafoundation.org/content/view/419/254/ to donate. Watch future issues of the Weekly Roundup for opportunities to con-tribute to the Foundation, including the Wall of Caring, the Auction at the Wall, and other initiatives at AMDA’s annual conference in March. CfA
AMDA Foundation Kicks off Fall giving Campaigns
More Chances To Complete online Core
to effective behavioral interventions and provide practical strategies and solutions to navigate mental health challenges in this care setting. (A 4-day registration and additional $55 pre-registration fee are required for participation.)
▶▶ Nationally known speaker and author Pratap Chand, MD, DM, FRCP, professor and director of movement dis-orders in the department of neurology and psychiatry at the St. Louis University School of Medicine in Missouri, will
address “Movement Disorders in the Older Adult” at the Meet the Expert Breakfast Session. The program is set for Saturday, March 21, 6:00-7:45 a.m.
Go to the conference’s dedicated web-site at www.paltcmedicine.org for more information about the program or to register. The Best Value Rate is available until January 20 or when hotel rooms sell out – whichever comes first. The rate applies at one of four AMDA conference hotels, described on the website. CfA

N e w s F r o m t h e s o c i e t y ™
CARIngFoRTheAgeS.CoM CARIng FoR The AgeS • 19
January 5-March 2, 2015AMDA Online Core Curriculum on Medical Direction in Long-Term Care: Part I Session 1Contact: AMDA Registrar Phone: 410-992-3116Email: [email protected]: www.amda.com/ cmedirect/core-part-1.cfm
January 28, 2015AMDA Live Webinar: Infection Control in LTC Contact: AMDA Registrar Phone: 410-992-3116Email: [email protected]: www.amda.com/cmedirect/#web
January 31, 2015ALMDA Mid-Winter MeetingBirmingham, ALContact: Jennifer HayesPhone: 334-954-2513 Email: [email protected]: www.almda.org/new-events/
March 19, 2015Navigating Mood and Behavior Challenges WorkshopIn Conjunction with AMDA’s Annual ConferenceContact: AMDA Registrar
Phone: 410-992-3116Email: [email protected]: www.bit.ly/moodbehavior
March 19-22, 2015AMDA – The Society for Post-Acute and Long-Term Care Medicine 2015 Annual ConferenceLouisville, KYContact: AMDA Registrar Phone: 410-992-3116Email: [email protected] Website: www.paltcmedicine.org
March 21, 2015Meet the Expert Breakfast Session: Movement Disorders in the Older Adult Louisville, KYContact: AMDA RegistrarPhone: 410-992-3116Email: [email protected]: http://bit.ly/meethexperts
March 27-28, 2015GAPNA: Contemporary Pharmacology and Prescribing in Older AdultsPhiladelphia, PAContact: Jill BrettPhone: 866-355-1392Email: [email protected]: www.gapna.org
April 1, 2015AMDA CMD Initial and Recertification DeadlineContact: AMDCP Program ManagerPhone: 410-992-3117Email: [email protected] Website: www.amda.com/certifica-tion/overview.cfm
April 6-June 1, 2015AMDA Online Core Curriculum on Medical Direction in Long-Term Care: Part I Session 2Contact: AMDA RegistrarPhone: 410-992-3116Email: [email protected]: www.amda.com/cmedirect/
core-part-1.cfm
April 24-25, 20152015 CALTCM Annual MeetingLos Angeles, CAContact: Barbara HulzPhone: 888-332-3299Email: [email protected]
Website: www.caltcm.org
May 15-17, 2015American Geriatrics Society 2015 Annual Scientific MeetingNational Harbor, MDWebsite: www.americangeriatrics.org/annual_meeting/
June 6-10, 2015NADONA 28th Annual ConferenceAtlanta, GAWebsite: www.nadona.org
July 18-24, 2015AMDA Core Curriculum on Medical Direction in Long-Term CareBaltimore, MDContact: AMDA RegistrarPhone: 410-992-3116Email: [email protected]: www.amda.com/education/core
September 30-October 3, 2015GAPNA: Annual ConferenceSan Antonio, TXContact: Jill BrettPhone: 866-355-1392Email: [email protected]: www.gapna.org
March 17-20, 2016 AMDA – The Society for Post-Acute and Long-Term Care Medicine 2016 Annual ConferenceKissimmee, FLContact: AMDA Registrar Phone: 410-992-3116Email: [email protected]: www.paltcmedicine.org
ImportantDates
There is still time to support the 2015 AMDA Foundation Futures
Program. Individuals who receive a scholarship to participate in this program not only gain insights into career opportunities in PA/LTC medicine but also make friends and contacts and learn about topics that inspire their passions. Just ask Futures alumnus Ken Konchilja, MD.
“It was interesting to meet people who practice in different areas – aca-demia, community settings, nursing homes, etc. I didn’t know much about the medical director’s role, and I really enjoyed learning more about that. It also was nice to have a chance to bond with people my own age who share some of my professional interests,” Dr. Konchilja said of his Futures expe-rience. He also was pleased to learn how many practicing physicians also are involved in research. “That was interesting to me because people often think that primary care physicians can’t or don’t do research. As someone who wants to do research and practice medi-cine, I found that enlightening,” he said.
The Futures program itself was “amazing,” Dr. Konchilja said, adding
that the speakers were excellent. He particularly liked presentations by Cari Levy, MD, CMD, about options for career paths, and by Steven Handler, MD, CMD, who spoke about PA/LTC research.
Beyond Futures, Dr. Konchilja found the AMDA conference, the program sessions, and networking with people from around the country to be music to his ears. “It was like an orchestra with all kinds of sights and sounds – people from various backgrounds, practice settings, and areas of interest,” he said. “You listen to all of the stories and best practices, and you take them back and use them with your team at home.”
The Futures Program is funded through donations to the Foundation, Caring Canines calendar purchases, and grassroots contribu-tions from state chapters, physician practices, and other organizations and individuals. For more informa-tion about the Futures Program and how you can support the class of 2015, contact the AMDA Foundation at [email protected] or 410-992-3134. CfA
It’s not Too Late To Inspire young Practitioners
Don’t Miss These events
In response to member feedback and a commitment to provide afford-
able, cutting-edge, and convenient education, AMDA has announced a 2015 member discount for webinar programs. Single webinars for AMDA members will be discounted to $55 – almost a 50% savings.
You can take advantage of this discount to register for the webinar on infection control, presented by AMDA past-president Karyn Leible, RN, MD, CMD. “A great deal has been happening in the infection con-trol area in recent months,” she said, noting that the idea for this webinar arose from a request by her organiza-tion to develop policies and proce-dures to address Ebola. The program will present an update on infection control and infectious diseases includ-ing the various organisms practitio-ners need to be aware of, what is known and what the literature says about treatment and prevention, and misconceptions on the part of staff and others. For example, she said, “People often think that drug-resis-tant organisms make people sicker. In fact, they don’t, but they are more
difficult to treat.” Dr. Leible also will discuss challenges regarding the over-use of antibiotics and their implica-tions for managing infections in the PA/LTC setting.
Dr. Leible perhaps understands the challenges of addressing infec-tious disease better than many, as she was on the forefront of treating patients with AIDS and HIV back in the early ‘80s, when these illnesses were largely unknown. “I was a nurse at Mass General when we got the first AIDS patients. We used draco-nian precautions, such as the use of gowns, masks, and strict isolation. We learned over time not only how to treat AIDS and other infectious diseases but also how to provide per-son-centered care for the people with these conditions.” She noted, “We have to realize in post-acute and long-term care that our patients’ rooms are their homes. We need a better way than to just isolate them there when they get sick or show signs of an infectious disease.”
For more information about the program or to register, go to http://www.amda.com/cmedirect/#web. CfA
Sign up for Infection Control Webinar: get Member Discount