Chest X-rays & Abdominal Plain...
Transcript of Chest X-rays & Abdominal Plain...
Check List
Identify Film: patient name, date and study
Inspiration: 9-10 posterior ribs above right
hemidiaphragm
Position: upright (gastric air-fluid level)
Exposure:bronchovascular structures visible through heart
and diaphragm
Rotation: line through spinous processes bisects line
between clavicular heads
PA vs AP PA: clavicles appear lower, scapulae project more
laterally, posterior elements of vertebral bodies clearer
AP: magnifies heart
PA AP
Chest X-Rays: The Yellow Brick Road
ABC’s…D & E
Air: lungs, including central airways & pulmonary vessels
Bones: ribs, clavicles, spine, shoulders, scapulae
Cardiac: heart & mediastinum
Diaphragm & pleural surfaces
Everything else: lines & tubes, upper abdomen, soft tissues
of chest wall and neck
Air
Air Space vs Interstitial disease pattern
Air Space/alveolar disease pattern: aka consolidation
Fluid density in alveoli
Signs: inhomogenous, patchy opacities, air bronchograms (bronchi surrounded by opaque alveoli)
Causes: usually acute/subacute- bacterial pna, cardiogenic & noncardiogenic pulmonary edema, aspiration, pulmonary hemorrhage
Air
Interstitial Disease pattern: aka
reticular/reticulonodular
Fluid density in interstitium
Signs: diffuse white lines throughout lungs, with or
without tiny white nodules
Causes: usually subacute/chronic- pulmonary fibrosis,
sarcoidosis, Metastatic carcinoma (lymphangitic),
occupational lung dz (abestosis, silicosis)
Exceptions: cardiogenic pulmonary edema & atypical
pneumonia (viral, mycoplasma, miliary TB, histoplasmosis)
Atelectasis
Causes: obstruction (tumor, foreign body), compression
(pneumothorax, pleural effusion, traction (scarring)
Signs: displaced interlobar fissure towards collapsed lobe,
displaced diaphragm or mediastinum towards collapse,
decreased lung volume
Pneumonia
“Silhouette” sign: obscuring of border by lung infiltrate
Heart border = right middle lobe or left lingual
Diaphragm = lower lobe
Air Bronchogram: bronchi surrounded by fluid filled
alveoli
Pneumonia
Lobar Pneumonia
Causes: Streptococcus pneumoniae, Haemophilus influenze,
Klebsiella, Neisseria meningitides…
Signs: lobar opacification/patchy fog, air-bronchograms
Pneumonia
Bronchopneumonia
Involves bronchi, bronchioles and adjacent alveoli with
possible volume loss
Causes: Staphylococcus aureus, Gram negatives, mycoplasma
(also interstitial pattern)
Signs: segmental opacification, no air bronchograms
Pneumonia- considerations
Non- resolving pneumonia:
Wrong antibiotic, lack of compliance, not-absorbing antibiotic, immunocommpromised, intrinsic airway problem (obstruction), not pneumonia => CT
Bacterial pneumonia usually resolves in 6 weeks with treatment (longer if elderly, COPD, ETOH)
Dehydration: hydration will enhance appearance of pneumonia
Neutropenia: increasing white count will enhance appearance of pneumonia
Pneumonia- Considerations
Mimics pneumonia:
Cancer: postobstructive pneumonia from lung CA,
bronchoalveolar, lung CA, pulmonary lymphoma…
Non-neoplastic- aspiration, hemorrhage, pulmonary edema,
sarcoidosis…
PCP pneumonia
HIV: CD4 < 200
Bilateral
symmetric
perihilar
opacities
(however has
variable
appearance)
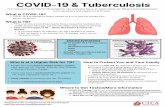
Tuberculosis TB infection
Latent TB infection: Positive tuberculin skin test; no clinical, radiologic, or bacteriologic
evidence of disease
Active TB infection: Clinical, radiologic, or bacteriologic evidence of active disease
Primary TB
Initial infection of nonsensitized patients
Progressive primary TB in 5% of cases
Progressive lung involvement
Tissue necrosis & cavitation
Bronchogenic dissemination of infection
Post-primary TB
Reactivation of TB due to impaired immunity
Exogenous re-infection
Disseminated TB
Primary or post-primary TB
Related to immunosuppression
Sarcoidosis
Stage 0- normal CXR
Stage 1- bilateral symmetric hilar lymphadenopathy
Stage 2- stage 1 & reticulonodular parenchymal opacities
Stage 3- increased opacities but decreased lymphadenopathy
Stage 4- pulmonary fibrosis, bullae (usually in upper lobes)
Emphysema
Chronic obstruction
leading to destruction
of alveoli and
hyperinflation,
bullae, decreased
lung density,
decreased
vasculature,
flattened diaphragms
Asthma
Hyperinflated lungs
(>10 ribs on
inspiration),
peribronchial
cuffing (also seen in
chronic bronchitis,
bronchiectasis,
pulmonary edema &
cystic fibrosis)
Cavities
Abscess, fungal
pneumonia,
granulomatous
disease, tumors
(squamous cell
carcinoma)
“air crescent”
sign- fungal
ball/aspergilloma
Air Crescent sign
Pulmonary Embolism
80-90% with abnormal CXR
Findings: non-specific (subsegmental atelectasis, ill-defined
opacities)
Hamptom’s Hump: peripheral, pleural-base cone shaped
opacity from post-obstructive infarct of lung tissue
Westermarks’ sign: abrupt tapering of a vessel with focal
oligemia
Lung Cancer
In 10% of heavy smokers (>35 pack years)
1. squamous cell carcinoma. 2. adenocarcinoma
92% of Lung CA with history of smoking
Bronchogenic carcinoma:
Adenocarcinoma 45%
Squamous cell carcinoma 35%
Small cell carcinoma 15%
Large cell carcinoma 1-5%
Lung Cancer
Nodules < 3cm; Mass > 3cm Malignant: large nodules, lobulated/spiculated
margins, older patient, enhances with iv contrast, cavitary lesion with wall thickness > 16mm (95% malignant)
Benign: calcification (diffuse, central, “popcorn”, laminar), very fast growth (double volume < 1mo), very slow growth (stable for > 2 yrs), smooth margins, cavitary lesion with wall thickness < 4mm (>95% benign)
Pathologic lymph nodes: > 1cm
Lung Cancer
Squamous cell CA: central mass with atelectasis or postobstructive pneumonia, cavitation (30%)
Adenocarcinoma- peripheral nodule/mass, pneumonia that fails to resolve
Bronchoalveolar CA- multiple nodules, chronic airspace consolidation or interstitial pattern
Small cell CA: extensive mediastinal lymphadenopathy without other findings or central mass, distant metastasis at diagnosis
Large cell CA: central or peripheral mass
Pulmonary metastasis: multiple, lung bases (perfusion), peripheral (90% outer third)
Pancoast tumor
Usually Squamous cell or adenocarcinoma
At lung apex with invasion causing horner’s syndrome (miosis, ptosis, anhydrosis) & atrophy of muscles ipsilaterally
Reverse S sign of Golden
Convex bulge in
medial aspect of
minor fissure in
patient with right
upper lobe
atelectasis from
obstructing
central mass
Bones
Ribs, Clavicles, Spine, Shoulders, Scapulae
Rib Fracture
Child abuse:
posterior rib fractures, calluses, multiple stages of healing
Cardiac
Heart
Congestive Heart Failure
Cardiomegaly
Pulmonary Edema
Pericardial Effusion
Mediastinum
Anterior Mediastinum
Paraspinal bulge
Pneumomediastinum
Aorta
Cardiomegaly
Causes: pericardial disease, valvular heart disease,
cardiomyopathy, hypertension, congenital…
Cardiothoracic ratio
Heart size vs chest width:
25-50% nl, 50-60% ?, > 60% abnormal
Considerations: upright vs supine CXR, PA vs AP, inspiration
Cardiomegaly
Left Ventricular Heart failure
CXR relation to PCWP
15 mmHg- normal CXR
15-20 mmHg- pulmonary venous hypertension
cephalization (can look normal in chronic disease)
>20 mmHg- pulmonary edema
Blurring margins of central pulmonary vessels, Kerley lines,
thickening of bronchi walls
To be continued…
Pulmonary Edema
Non-cardiogenic Pulmonary Edema Findings: normal heart size, perihilar
opacification, rare air bronchograms
Pulmonary injury Patchy opacification (mostly alveolar injury), air
bronchograms, normal heart size/pulmonary vessels, rare kerley b lines or pleural effusions
Pulmonary Edema
Causes:
Increased hydrostatic pressure- LVH, mitral stenosis,
anomalous pulmonary return, high altittude disease)
Decreased plasma oncotic pressure- nephrotic syndrome
Impaired capillary integrity- infection, acid aspiration, toxic
inhalation
Pulmonary Edema
Increased hydrostatic pressure (ie CHF) Findings: Grade I- cephalization
Grade II- peribronchial cuffing, pleural effusions, kerley b lines
Grade III- alveolar opacification, air bronchograms
Kerley lines
A- multiple arcuate lines radiating from hila
B- multiple short horizontal linear densities perpendicular
to pleural space
C- cobweb mesh of linear opacities in middle portion of
lungs
Can also represent interstitial fibrosis, pulmonary
hemorrhage, lymphangitic spread of tumor
Pericardial Effusion
Causes: infection, immune reactions, trauma, neoplasm,
inflammation…
CXR
Frontal: Cardiomegaly
Lateral:
“oreo cookie” sign- vertical opaque stripe between anterior heart
border (epicardial fat) and pericardial fat
Follow-up with Echo, CT or MRI
Mediastinum
Anterior Mediastinum Four T’s
Thyroid mass
Thymoma
Teratoma
“Terrible Lymphoma”
Cervicothoracic sign: “neck” mass
Anterior mediastinum if lateral margins of mass above clavicles are blurred (four T’s)
Posterior mediastinum if lateral margins of mass above mediastinum are sharp (ie... Paraspinal bulge)
Mediastinum Paraspinal Bulge:
90% neurogenic tumor:
neurofibromas,
neuroganglioneuromas
Traumatic spine fracture
with hematoma
Aortic Issues
Aortic Laceration
Usually from MVA
Findings: Wide mediastinum (>8cm at level of aortic arch),
blurred aortic arch, blood over apex of lung as a white
crescent (apical cap), hematoma pushing trachea right and
left main bronchus down, NGT pushed right
Aortic Issues
Aortic Aneurysm fusiform/saccular & focal
Aortic Dissection Fusiform/normal, diffuse Debakey classification
I – ascending & descending aorta II- ascending aorta to origin of great vessels III- disttal to left sublacvian artery
Stanford classification A- involves ascending aorta (5% survive 1 year without surgery) B- spares ascending aorta (70% survive without surgery)
Tx: Surgery for I, II, A & Medical (BP control) for III, B
CXR signs: wide mediastinum, increased size of aorta, medial displacement of intimal aortic calcifications Further evaluation with CT, TEE, MRI, angio
Diaphragm & Pleural surfaces
Pneumothorax
Spontaneous
Tension
Pleural Effusions
Diaphragm
Rupture
Hiatal hernia
Pleural Mass
Pneumothorax
Spontaneous: Primary: associated with apical blebs
Secondary: to COPD, pulmonary fibrosis, langerhans cell histiocytosis, neoplasm…
Hospitalized patients: thoracentesis, mechanical ventilation, central lines
Tension: Cause: usually positive pressure mechanical ventilation or
penetrating chest trauma
Clinical signs: rapid hemodynamic/respiratiory deterioration, hyperresonant ipsilateral hemithorax, decreased breath sounds, contralateral displacement of trachea & cardiac apex
Treat first, CXR later
Pneumothorax
CXR signs:
Upright CXR
End expiratory film
Decreased lung volume relatively increases ptx volume
Increased density of lung vs ptx
Sharp line of visceral pleura
Supine CXR
Hyperlucency of lung base, deep sulcus sign, double diaphragm
sign
Lateral decubitus CXR: ptx side up
Pleural Effusions
Plasma ultrafiltrate, empyema, hemothorax, urine, bile... Transudative vs exudative
Common causes: cardiogenic/noncardiogenic pulmonary edema, pneumonia, neoplasm, autoimmune disease
Upright CXR: blunt costophrenic angles >150-300 ml of fluid
Lateral decubitus CXR: Affected side down- layering of effusion Check for loculation
Supine CXR: Blunt costophrenic angle, loss of hemidiaphragm definition, general
increase in hemithorax density May obtain lateral decubitus CXR, cross table lateral, CT or U/S
Subpulmonic Effusion
Effusion between lung & diaphragm
Signs: lateral displacement of diaphragm apex, no visible
bronchovasculature behind “pseudodiaphragm”,
increased distance between left diaphragm & gastric
bubble (nl < 2cm), posterior meniscus on upright lateral
CXR
Everything else
Tubes, Lines & Catheters
Endotracheal tube
NG tube
Central Venous Catheter
Swan-Ganz catheter
Why care?
Check for complications of tubes, lines and catheters
Avoid mistaking them for pathology
TLC placement
ET tube: 4 cm above carina
because flexion/extension may move tip up to 4 cm (~ level of clavicular head)
TLC placement
NG tube: Between esophageal-
gastric junction and pylours
Central venous catheter: Over shadow of SVC
between 1st rib/clavicle and right atrium (above R atrium to avoid arrythmias) Right Subclavian central line
TLC complications Device Complication Inappropriate position
Endotracheal tube Aspiration (parenchymal opacities),
pharyngeal perforation (subc
emphysema, pneumomediastinum)
Esophageal intubation, selective
mainstem bronchus intubation, too high,
balloon too big (> 2-3 cm)
Nasogastric tube Aspiration, intracranial perforation, ptx Intratracheal intubation,
intraesphophageal, intraduodenal
Chest tube Lung perforation (mediastinal opacity) Extrathoracic, apical (Horner’s syn)
Central Venous Catheter Ptx, bleeding (mediastinal, pleural), air
embolism
Extravascular, peripheral, intracardiac
Swan-Ganz catheter Ptx, bleeding, air embolism Proximal, distal (pulmonary infarction)
Directions
Free ABDO Free fluid
Air Outside bowel- free intraperitoneal air, retroperitoneal air,
branching air in liver, abcess, air in bowel wall
Inside bowel- dilated bowel, air fluid levels
Bowel wall thickening inflammation & ischemia
Densities bone, calcifications, other…
Organs outlines of liver, spleen, kidney & bladder
Free Fluid
Supine KUB: free fluid if…
distance between colon and flank fat stripe greater than the
width of a pinky finger
Large amounts of free fluid will cause a diffuse increased
opacification in the abdomen
Air outside
Why? Perforations!
Peptic ulcer disease, diverticulitis, colon ca, obstruction…
Normal after abdominal surgery- about 10 days for reabsorption
Upright CXR
Free air under diaphragm
Chilaiditi’s Syndrome: incorrect diagnosis of free air from large bowel between liver and diaphragm
Left Lateral Decubitus film: free air above liver
Air Outside… again
Abdominal Film: Rigler’s sign: bowel wall outlined by air inside and outside
bowel Retroperitoneal Air: Perforation from parts of duodenum, ascending/descending colon
Air outline kidneys, iliopsoas muscle, abnormal air streaks extending into iliopsoas
Branching air in Liver: Pneumobilia: bile duct manipulation (sphincterotomy) or
emphysematous cholecystitis
Portal venous air (ominous): massive bowel infarction
Abscess: local collection of air not in bowel Abnormal bowel location, no haustra or plicae circulares, air in stable
location
Pneumatosis Intestinalis (air in bowel wall): bowel ischemia/infarct
Air- Inside
Small vs Large Bowel: Small bowel: central, plicae circulares
(circumferential)
Large bowel: framing, haustra (non-circumferential)
Air Fluid levels: line with air above and fluid below
Dilated bowel… size and loss of lines Small bowel > 3cm
Large bowel > 6 cm
Cecum > 9 cm
Air Inside- Nuts’n Bolts
Ileus: paralyzed bowel
Localized- inflammation
Generalized- drugs, surgery, pain
Bowel obstruction
Adhesions, hernia, bowel CA, intussusception,
ischemia, volvulus, Crohn’s, Meckel’s
diverticulum, gallstone ileus…
Proximal dilation, distal collapse
Complete vs partial: check for distal air (rectum)
Air Inside- more Nuts’n Bolts
Volvulus
Sigmoid
More common
Coffeebean or inverted U shape dilation in lower abdomen
Cecal
Like a stomach bubble in middle of abdomen
Acute Pancreatitis
“Sentinel loop”: focal small bowel ileus in ULQ
“Colon cutoff sign”: distended transverse colon with no gas
distal to splenic flexure
Left pleural effusion
Bowel wall thickening
Sign of bowel inflammation or ischemia
Narrowed lumen, thickening folds, “thumb printing”,
loop separation
Densities
Bone: vertebral column, pelvis
Appendicitis: Appendicolith: seen in 10% of appendicitis Other findings: RLQ ileus, blurred right psoas shadow, extraluminal soft-
tissue mass, pneumoperitoneum, scoliosis of lumbar spine- convex to left
Stones: Gallstones: RUQ Renal/Ureteric stones: 80-90% visible on plain abdominal film
Pancreatic Calcifications: chronic pancreatitis
Abdominal Aortic Aneurysm (AAA): calcified aorta > 3cm width
Uterine Fibroids, Phleboliths, Dermoids, foreign objects, lines & tubes…
Remember
CXR
ABCDE
Air
Bones
Cardiac
Diaphragm & pleura
Everything Else
Abdominal Films
Free ABDO
Free air
Air inside/outside
Bowel wall thickening
Densities
Organs
Credits
Douglas S. Katz, MD, et al. Radiology Secrets.
Hanley and Belfus, Inc. Philidelphia, PA, 1998
Hague Ouellette, MD, et al. Clinical Radiology
made ridiculously simple. Medmaster Inc.
Miami, FL, 2000.
Ryan W Davis, et al. Blueprints in Radiology.
Blackwell Publishing, Inc. Mass, CT, 2003.
And many thanks to the internet for images