Cervical Spine Injury
-
Upload
jhing-rodriguez-borjal -
Category
Documents
-
view
34 -
download
2
Transcript of Cervical Spine Injury

CERVICAL SPINE
INJURY

Common causes:1. MVA (esp major or if head injury),2. sporting 3. diving, 4. falls, 5. assault,

Incidence:
~2% based on sig. spine or cord injuries found in trauma imaging of C-spines.
10-20% HI injury also have a cervical spine injury.
~15% have missed or delayed diagnosis of cervical spine injury, with a risk of permanent neurologic deficit of 29%.

Site: 33% of injuries occur at the level of C2, and 50% occur at the level of C6 or C7.
Pediatric: Most injuries are C1-C2 as relatively heavier head, lax ligaments.
Gender: 4M:1F

Presentation
Cervical spine injury should be suspected if:
· Dangerous mechanism: MVA, fall, diving accident, axial load to head, sporting tackles
· Neck pain: Midline tenderness = vertebral vs lateral tenderness = muscle.

• Neurological signs: Paraesthesiae & weakness/paralysis. Spinal cord injury → various deficits, injury syndromes
• Other trauma: Multi-trauma, significant HI, distracting painful injury
• Elderly – increased fragility.
• ↓LOC – makes assessment difficult – assume an injury

• Injuries to the cervical spine are serious because the crushing, stretching, and rotational shear forces exerted on the cord at the time of trauma can produce severe neurologic deficits
• Edema and cord swelling contribute further to the loss of spinal cord function.



Injury Mechanisms
• Hyperflexion (most common, 80%)o Fractures: Ant wedge #, flexion teardrop #, clay shoveller’s #, peg #o Dislocations: ant subluxation, bilateral interfacet dislocation, antlanto-occipital dislocation, ant atlanto-axial dislocation
• Hyperextension:o Fractures: Hangman's #, extension teardrop #, o Dislocation: ant atlanto-axial dislocation

Injury Mechanisms
• ·Axial compression: Jefferson #, vertebral burst #
• Distraction• Lateral rotation: Unilat interfacet dislocation,
rotatory atlanto-axial dislocation

Atlas (C1) injury
1. Neural arch fracture2. Burst (Jefferson) fracture3. Atlanto-occipital dislocation4. Transverse ligament disruption (ant.
atlantoaxial dislocation)

Neural arch fracture
• Longitudinal # through post. neural arch, usually bilateral caused by hyperextension. Stable.

Jefferson Fracture• Compression fracture of the
bony ring of C1, characterized by lateral masses splitting and transverse ligament tear.
• Best seen on odontoid view

• Signs: Displacement of the lateral masses of vertebrae C1 beyond the margins of the body of vertebra C2.
• CT is required to define the extent of fracture
• Caused by axial compression


Atlanto-occipital dislocation
• Uncommon. Disruption of all ligaments between occiput and atlas with subluxation or complete dislocation of the occipito-atlantal facets.

• Anterior translation of the skull can stretch brainstem → respiratory arrest & death. More common in children due to the larger head.
• Up to 50% of atlanto-occipital dislocations are initially missed.

Transverse ligament disruption (ant. atlantoaxial dislocation)
• Predental space>3mm (child >5mm) as dens moves back compressing spinal cord

Axis (C2) injury
1. Odontoid peg fracture2. Hangman’s fracture (traumatic
spondylolisthesis)

Odontoid Fracture
• Fracture of the odontoid (dens) of C2 (most common)– 3 categories, I-III
• Flexion, extension, and rotation may contribute to the fractures
• Best seen on the lateral view

Type I
• Type I – Fx through superior portion of dens

Type II– Fx through the base of the dens

Type III – Fx that extends into the body of C2

Hangman’s Fracture(traumatic spondylolisthesis)
• Fx through the pars reticularis of C2 secondary to hyperextension; fracture of the pedicles of the axis or second cervical vertebra
• Best seen on lateral view

• Signs:– Prevertebral soft tissue swelling– Avulsion of anterior inferior corner of C2
associated with rupture of the anterior longitudinal ligament.
– Anterior dislocation of the C2 vertebral body. – Bilateral C2 pars interarticularis fractures.
• MOI: extreme hyperextension during a diving accident or motor vehicle collision– Hanging or hitting a dashboard


C2-C7 Injury
• Anterior wedge compression fracture• Teardrop flexion fracture• Teardrop extension fracture• Burst fracture• Unilateral (locked) facet joint dislocation• Bilateral (locked) facet joint dislocation• Spinous process fracture• Whiplash (Cervical Sprain)• Hyperflexion Strain• Hyperextension Strain

• Hyperflexion # with reduced ht (<3mm) of vertebral body only anteriorly.
Anterior wedge compression fracture
• Compression fracture resulting from flexion.
• Mechanism: hyperflexion and compression

• Signs: – Buckled anterior
cortex.
– Loss of height of anterior vertebral body.
– Anterosuperior fracture of vertebral body.

Flexion Teardrop Fracture• Posterior ligament
disruption and anterior compression fracture of the vertebral body which results from a severe flexion injury.
• Best seen on lateral view

• Signs: – Prevertebral swelling associated with anterior
longitudinal ligament tear.– Teardrop fragment from anterior vertebral body avulsion
fracture.– Posterior vertebral body subluxation into the spinal
canal.– Spinal cord compression from vertebral body
displacement.– Fracture of the spinous process.
Mechanism: hyperflexion and compression (e.g. diving into shallow water)

• Neurologic injury is very common. The result is often the anterior cord syndrome, manifesting as quadriplegia and loss of pain and temperature sensation. The most common level for a teardrop fracture is C5.

Teardrop extension fracture
• Hyperextension causes a triangular fragment to be avulsed off the anteroinferior corner of the vertebral body.
• C2 is most commonly involved.
• Only rarely assoc with neurological deficit.

Burst Fracture• results from axial
compression.
• Axial compression → comminuted fracture ± fragment surface driven back into spinal canal
• CT is required for all patients to evaluate extent of injury.

• Injury to spinal cord, secondary to displacement of posterior fragments, is common.

Facet Joint Dysfunction
• Cervical instability • MOI - from acute trauma
(whiplash) or repetitive motions
• S&S – posterior neck pain in paraspinal region, pain with A and PROM during extension and rotation of the c-spine, clicking or catching; referred pain but no radicular pain

Unilateral Facet Dislocation• Facet joint dislocation and
rupture of the apophyseal joint ligaments resulting from rotatory injury of the cervical vertebrae. (vertebra being displaced anteriorly by up to 25% on the lateral film.)
• Best seen on lateral or oblique views
• Mechanism: simultaneous flexion and rotation

• Signs:
– Anterior dislocation of affected vertebral body by less than half of the vertebral body AP diameter.
– Discordant rotation above and below involved level.
– Facet within intervertebral foramen on oblique view.
– Widening of the disk space.
– "Bow tie" or "bat wing" appearance of the overriding locked facets.

Bilateral Facet DislocationComplete anterior dislocation of the vertebral body resulting from extreme hyperflexion injury. It is associated with a very high risk of cord damage. (displaced ant by 50%on lateral view.)
• Best seen on lateral view

• Mechanism: extreme flexion of head and neck without axial compression.
• most severe form of anterior subluxation
• Neurologic injury is common.

• Signs: – Complete anterior
dislocation of affected vertebral body by half or more of the vertebral body AP diameter.
– Disruption of the posterior ligament complex and the anterior longitudinal ligament.
– "Bow tie" or " bat wing" appearance of the locked facets.

Spinous process fracture
• Hyperflexion causes avulsion of the spinous process by the supraspinatous ligament, usually C6 or C7 (Clay shoveller’s).

• This is caused by flexion as the body rotates relative to the head and neck. Usually undisplaced, stable and seen on lateral film.

Clay Shoveler’s Fracture
• Fracture of a spinous process C6-T1
• Best seen on lateral view
• Mechanism: powerful hyperflexion, usually combined with contraction of paraspinous muscles pulling on spinous processes (e.g. shoveling).

• Signs: – Spinous process
fracture on lateral view.
– Ghost sign on AP view (i.e. double spinous process of C6 or C7 resulting from displaced fractured spinous process).

Whiplash (Cervical Sprain)• Sprain – injury to a ligament
or non-contractile tissue• Sudden deceleration of the
body, with flexion and extension movements of the cervical spine usually results in sprain or intervertebral disc injury without fracture or dislocation.

• The commonest radiographic appearance is straightening of the cervical spine due to severe muscle spasm, with the normal curvature reduced or reversed. Usually MVA. May be increased with seat belts. Reduced by proper head rests.

Whiplash injury• Sudden hyperextension and flexion• Increasing neck pain for the first 24hours • Associated headache, pain radiating to both
shoulders and paraesthesia in hands• Reduced lateral flexion• Anterior longitudinal ligaments are torn causes
dysphagia • Forward flexion against resistance is painful• 90% are asymptomatic after 2years• 10% still have pain



Hyperflexion Strain
• Anterior subluxation occurs with disruption of posterior longitudinal ligament, interspinous ligament and intervertebral disc.
• Lat film shows localised kyphotic angulation with increase in height of intervertebral disc posteriorly and associated fanning of the spinous processes.

Hyperextension Strain
• The converse of hyperflexion strain; the anterior longitudinal ligament is disrupted as evidenced by widening of the intervertebral disc space anteriorly.
• The facet joints are disrupted and the interspinous distance is narrowed.

Anterior Subluxation
• Disruption of the posterior ligamentous complex resulting from hyperflexion.
• It may be difficult to diagnose because muscle spasm may result in similar findings on the radiograph. Subluxation may be stable initially, but it associates with 20%-50% delayed instability. Flexion and extension views are helpful in further evaluation.
• Mechanism: hyperflexion of neck

• Signs:– Loss of normal cervical
lordosis.– Anterior displacement of
the vertebral body.– Fanning of the
interspinous distance.

Brachial Plexus / Neuropraxia Commonly called burners, stingers,
pinched nerves
MOI: stretch or compression
S/S: burning or stinging neck/arm/hand, muscle weakness, supraclavicular tenderness (Erb’s Point), neck painchronic: numbness ,tingling, and weakness lasts longer

Brachial Plexus Injury• Compression force – nerve roots pinched between
adjacent vertebrae– Increased risk if spinal stenosis (narrowing of
intervertebral foramen) exists• Distraction force – tension or “stretch” force on
nerve roots– Most common at C5/C6 levels but may involve
any cervical nerve root– Erb’s point – 2-3 cm above clavicle anterior to C6
transverse process, most superficial passage of brachial plexus

Other Pathology
1. Spondylosis2. Metastatic disease3. Congenital fusion4. Hanging

Spondylosis
• Refers to OA of the spine. Disc space narrowing and osteophyte formation. The associated osteophytes may impinge on the nerve root foramina. May obscure underlying injury.
• A common injury mechanism in these patients (often elderly) is a fall directly onto forehead → C2 #.

Spinal Stenosis• can be congenital• S&S:– can be asymptomatic– Neurological pain– Increased leg pain with
standing that resolves by sitting (increases available space in spinal canal)
– Can be ipsilateral (foramen) or bilateral (canal)

Metastatic disease
• Primary tumours can metastasise to vertebral bodies demonstrating a lucent, moth-eaten, permeative appearance. There is often subsequent collapse.

Congenital fusion
• It is not unusual to see a congenital fusion within the cervical spine, usually at C2/C3 with fusion of the vertebral bodies and posterior elements.
• This is associated with a hypoplastic odontoid peg.

Hanging
• 3rd most popular method of suicide. More common in young adult males & indigenous pop.
• Cervical spine injury in only 1% (Hangman’s fracture) only if drop>patient height. Death less likely from tracheal obstruction as from venous obstruction → suffusion, venous cerebral infarction, carotid sinus reflex bradycardia & ¯CNS → asphyxia. May have petechial/sub conj haemorrhages, hyoid #, laryngeal #or thyroid/cricoid cartilages. 75% intact if survive to ED.

Assessment
• History: Details of trauma. When neck pain/neuro symptoms developed (usually delayed with whiplash). Prior spinal injuries. AMPLE history.
• Examination: Palpate for tenderness, swelling, gap or step, muscle spasm. Neuro. (sensation, motor fn, reflexes, rectal tone, perianal sensation), other injuries.
• Investigation: Decision to image based on NEXUS criteria or Canadian C-spine rule.

CERVICAL SPINE IMAGING
National Emergency X-radiography Use Study (NEXUS) Low Risk Criteria (NLC)
• Aim: Criteria for clearing a patient of any or significant C-spine injury without imaging.
• Included: All who had trauma imaging of C-spine
• Excluded: Penetrating trauma

• Criteria:· No midline posterior tenderness· No focal neurological deficit· Alert· Not intoxicated· No distracting painful condition – e.g. long bone #, large lac, degloving, crush injury, burns
• Performance: Sensitivity 99% (any) or 99.6% (sig). Specificity 12.9% (any) or 12.9% (sig)
• Validated: in elderly (have a higher prevalence of odontoid fx) & children>9 y

Canadian C-Spine Rules
• Aim: Rules for detecting C-spine injuries in blunt trauma
• Included: All who had blunt head or neck trauma, GCS15, stable (BPsys>90mmHg & RR 11-23)
• Excluded: Penetrating trauma, age<16, pregnant, minor injuries only, GCS<15, >48h since injury, acute paralysis, known spinal disease, return for same injury.
• Performance: Sensitivity 100%. Specificity 42.5%


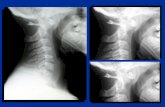
Imaging Modalities
• Plain radiography typically includes 3 views: anteroposterior, lateral, and odontoid.
• This imaging modality is falling out of favor because its false-negative rate is higher than that associated with CT Shows skeletal #s, alignment

CT imaging
• to evaluate patients for injury. • CT allows easy imaging of the cervical spine
when clinically indicated. • A CT scan is best for detecting bony
abnormalities; it can detect 97% of osseous fractures.
• shows skeletal #s, sublux/disloc injuries, disc spaces, alignment,

MRI
• shows ligamentous, disc & cord injuries well, less good view of #s. Controversy over use.

Primary Assessment

• Any person with a head, neck, or back injury or fractures to the upper leg bones or to the pelvis should be suspected of having a potential spinal cord injury until proven otherwise

• Provide immediate immobilization of the spine while performing assessment.
• Airway.
• Breathing.
–Intercostal paralysis with diaphragmatic breathing indicates cervical spinal cord injury.

Primary interventions

1. Immobilize the cervical spine.

The protocol for spinal immobilization is as follows:1. Maintain the head in neutral in-line position with a cervical collar in place2. Logroll the patient onto the backboard3. Secure the torso with spider straps or buckle straps4. Secure the head to the backboard with foam blocks or towel rolls5. Secure the legs to the backboard.


2. Open the airway using the jaw-thrust technique without head tilt.
3. If the patient needs to be intubated, it may be done nasally.
Recommendations for managing the airway of a trauma patient are:1. Rapid-sequence intubation (RSI): When managing an unconscious patient, standard drugs should be used for paralysis and induction

2. Manual in-line stabilization: An assistant firmly holds both sides of the patient’s head, with the neck in the midline and the head on a firm surface throughout the procedure, to reduce cervical spine movement and minimize potential injury to the spinal cord3. Orotracheal intubation is preferred in trauma patients requiring intubation4. Use a tracheal tube introducer such as a Bougie or stylet5. Have a selection of blades ready: evidence supports the use of a Macintosh blade6. A laryngeal mask airway (LMA) can be used as a temporary device.

4. If respirations are shallow, assist with a bag-valve mask.
5. Administer high-flow oxygen to minimize potential hypoxic spinal cord damage.

Subsequent assessment

1. Assess the position of the patient when found; this may indicate the type of injury incurred.
2. Hypotension and bradycardia accompanied by warm, dry skin (hypothermia)—suggests spinal shock.
3. Neck and back pain/extremity pain or burning sensation to the skin.
4. History of unconsciousness.

5. Total sensory loss and motor paralysis below level of injury.
6. Loss of bowel and bladder control; usually urinary retention and bladder distention.
7. Loss of sweating and vasomotor tone below level of cord lesion.
8. Priapism—persistent erection of penis.

9. Hypothermia—due to the inability to constrict peripheral blood vessels and conserve body heat.
10. Loss of rectal tone.

General interventions

NURSING ALERT
• A spinal cord injury can be made worse during the acute phase of injury, resulting in permanent neurologic damage.
• Proper handling is an immediate priority.

1. Insert an NG tube.
2. Keep the patient warm.
3. Initiate I.V. access.
4. Insert an indwelling urinary catheter to avoid bladder distention.
5.Monitor for hypotension, hypothermia, and bradycardia.
6. Continue with repeated neurologic examinations to determine if there is deterioration of the spinal cord injury.

7. Be prepared to manage seizures.
8. Pharmacologic interventions: high-dose steroids (methylprednisolone).
The standard regimen is 30 mg/kg I.V. loading dose over 15 minutes, followed by a 5.4 mg/kg/hour infusion to be initiated 45 minutes later.
Continue the infusion for 23 hours.

Cord-Level Findings
Neurologic deficits correlate with the level of the injury, resulting in weakness or paralysisbelow the lesion. There are 8 pairs of spinal nerves in the cervical spine.
From C1 to C7, the nerve root exits above the level of the vertebra; from C8 and below, the nerveroot exits below the level of the vertebra.

Myotome and Dermatome TestingNerve Root
LevelSensory Testing Motor Testing Reflex Testing
C1-C2 Front of face Neck flexion N/AC3 Lateral face and skull Lateral flexion N/aC4 Supraclavicular Shoulder shrug N/AC5 Lateral shoulder/upper arm Shoulder
abductionBicipital (musculocutaneous)
C6 Lateral lower arm and hand (thumb and index finger)
Elbow flexion and wrist extension
Brachialradial (musculocutaneous)
C7 Palmar aspect of hand – middle 3 fingers
Elbow extension and wrist flexion
Triceps (radial)
C8 Medial lower arm and hand Finger flexion and thumb extension
N/A
T1 Medial elbow and upper arm Finger abduction N/A

The presentation of incomplete cord injuries depends on the level and location of the lesion.
The anterior column conveys motor function, pain, and temperature, and the posterior column conveys impulses related to fine touch, vibration, and proprioception.

Partial Cord Syndromes
• Anterior cord syndrome results from compression of the anterior spinal artery, direct compression of the anterior cord, or compression induced by fragments from burst fractures.
• Anterior cord syndrome manifests as complete motor paralysis, with loss of pain and temperature perception distal to the lesion.
• Posterior cord syndrome is very rare; involvement of the posterior column is most often seen in Brown-Se´ quard syndrome.

Brown-Se´ quard syndrome
• Brown-Se´ quard syndrome is characterized by paralysis, loss of vibration sensation, and proprioception ipsilaterally, with contralateral loss of pain and temperature sensation.
• These signs and symptoms result from hemisection of the spinal cord, most often from penetrating trauma or compression from a lateral fracture.

Central cord syndrome, induced by damage to the corticospinal tract, is characterizedby weakness in the upper extremities, more so than in the lower extremities. The weakness is more pronounced in the distal portion of the extremities. This injury is usually caused by hyperextension in a person with an underlying condition such asstenosis or spondylosis.
Central cord syndrome