Cellular components of mammary secretions and neonatal ...
Transcript of Cellular components of mammary secretions and neonatal ...

HAL Id: hal-00902432https://hal.archives-ouvertes.fr/hal-00902432
Submitted on 1 Jan 1996
HAL is a multi-disciplinary open accessarchive for the deposit and dissemination of sci-entific research documents, whether they are pub-lished or not. The documents may come fromteaching and research institutions in France orabroad, or from public or private research centers.
L’archive ouverte pluridisciplinaire HAL, estdestinée au dépôt et à la diffusion de documentsscientifiques de niveau recherche, publiés ou non,émanant des établissements d’enseignement et derecherche français ou étrangers, des laboratoirespublics ou privés.
Cellular components of mammary secretions andneonatal immunity: a review
C Le Jan
To cite this version:C Le Jan. Cellular components of mammary secretions and neonatal immunity: a review. VeterinaryResearch, BioMed Central, 1996, 27 (4-5), pp.403-417. �hal-00902432�

Review article
Cellular components of mammary secretionsand neonatal immunity: a review
C Le Jan
Unité de pathologie infectieuse et immunologie, Inra, 37380 Nouzilly, France
(Received 18 December 1995; accepted 2 April 1996)
Summary ― Mammary secretions contain viable maternal cells that are mainly lymphocytes,macrophages, neutrophils and epithelial cells. Their biological functions in the neonate, though not yetclearly established, are strongly suggested by experimental data. This paper reviews current knowledgeof the cellular components of mammary secretions: their nature, in vitro properties, and demonstratedin vivo effects in the neonate, and discusses possible future experimental approaches. It is thought thatthe main role of the cellular components from mammary secretions is to interact with the develop-ment of local immunity in the newborn, and to modulate active immunization of the neonatal intestineduring this critical period when the development of adapted responses to antigens (protection/toler-ance/alimentary allergy) is of crucial importance for the future of the young.
colostrum / milk / newborn / mucosal immunity
Résumé - Composantes cellulaires des sécrétions mammaires et immunité néonatale. Synthèse.Les sécrétions mammaires contiennent des cellules maternelles vivantes, qui sont principalementdes lymphocytes, des macrophages, des neutrophiles et des cellules épithéliales. Leur intérêt biolo-gique pour le nouveau-né, s’il n’est pas encore clairement élucidé, est fortement suggéré par les don-nées expérimentales. L’auteur présente les connaissances établies sur les composantes cellulaires dessécrétions mammaires : nature, propriétés in vitro, effets démontrés in vivo chez le nouveau-né, et dis-cute les voies actuelles de recherche dans ce domaine. Le rôle majeur de ces composantes cellulairespourrait être d’interagir sur le développement de l’immunité locale du nouveau-né, et de moduler l’im-munisation active de l’intestin néonatal dans cette période critique où le développement de réponsesadaptées aux antigènes (protectionltolérancelallergie alimentaire) est d’une importance cruciale pourle devenir du jeune.
colostrum / lait / nouveau-né / cellules / immunité des muqueuses

INTRODUCTION
Mammary secretions are a link between themother and neonate after birth. Their func-tions extend beyond their nutritional aspects.The first days of life for a neonate corre-spond to a period of extremely intenseorganic growth, with high levels of cellularactivity mostly relating to cell division andto the establishment of various physiological
functions. These activities occur in an envi-
ronment where the first contacts with largequantities of foreign antigens are occurringand where it is necessary to quickly estab-lish appropriately adapted responses. It has
to be emphasized that the neonatal intes-tine, in addition to its role in nutrition physi-ology, is a major lymphoid organ and theprincipal site of antigenic contacts. An appro-priate level of immediate defenses, genuine

or resulting from mammary secretions, is
therefore essential for survival in the neona-tal period. The development of local immu-nity during the neonatal period concerns notonly the acquisition of immunity againstpathogens, but also the maturation of thelocal immune system and the establishmentof adapted responses (tolerance/activeimmunity). The transmission of passiveimmunity by mammary secretions is wellknown. In species such as swine, where thetype of placenta prevents the passage ofmacromolecules from maternal blood to the
foetus, the young is agammaglobuiinemicat birth and must form a pool of sericimmunoglobulins from the colostral maternalIg. There is a continuous supply of secre-tory IgA in the milk that is induced by intesti-nal sensitization of the mother during preg-nancy and mammogenesis, and which givespassive protection to neonatal intestine(Salmon, 1987; Berthon et al, 1993).Another aspect of lactogenic immunity isthe link between mammary secretions andthe active immunity of the neonate. Theproblem is complex, and at this time remainsa field under investigation. Mammary secre-tions have been shown to contain a largevariety of components that are immunolog-ical or that have the capacity to interact withthe immune system: lymphoid and non-lym-phoid cells, cytokines, immunomodulatingsubstances such as casein derivatives,growth factors and hormones. All these com-ponents could contribute to the cellulardefenses of the neonate, and could alsointeract with the development of the localimmune system in the newborn and withthe induction and orientation of active
responses to foreign antigens (Bernard etal, 1983; Chernishov and Sluvkin, 1990).The interactions between the maternal com-
ponents and the maturation of an activeimmunity in the neonate are as yet poorlyunderstood, and many questions remain tobe answered. This report, which focusesmainly on cells and cytokines (excludinggrowth factors, hormones and immunomod-
ulating substances), attempts to provide anoverview of the nature and roles of cellular
mammary secretion components for new-borns, and the different approaches cur-rently under investigation.
NATURE AND IN VITRO PROPERTIES
OF CELLULAR MAMMARY SECRETIONCOMPONENTS
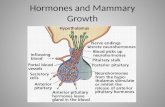
Nature of mammary secretion cells
For any mammalian species, there are morethan 1 x 106 cells mL-1 in colostrum and
milk. Global cellularity and cell types varyaccording to species, time of lactation andphysiological and individual conditions, butthe point is that the newborn receives a sig-nificant number of cells through mammarysecretions. For example, piglets ingest500-700 million viable maternal cells daily.Four cell types characterize mammarysecretions: lymphocytes, macrophages,neutrophils and epithelial cells. Lympho-cytes represent 5-9% of mammary secre-tion cells in humans, 20-25% in sheep,more than 30% in cows and 40% in rodents
and, during the colostral phase, 15-25% inswine (Crago et al, 1979; Ouzrout et al,1991; Park et al, 1992; Na et al, 1992; Evanset al, 1982; Schollenberger et al, 1986a;Magnusson et al, 1991; Le Jan, 1993).Based on the results obtained so far, it is
accepted that most mammary gland andmammary secretion lymphocytes originatefrom the mesenteric lymph nodes (Parmelyand Beer, 1977; Kumar et al, 1989).Macrophages and neutrophils predominatein the mammary secretions of most species,except in swine where they are outnum-bered by epithelial cells. Epithelial cells arepresent in low numbers during the colostraland involution phases, when the mammarygland is undergoing architectural recon-struction (Taylor-Papadimitriou and

Stampfer, 1991). In swine, however, theseepithelial cells represent 20-40% of the totalnumber of colostral cells, and 60-90% ofmilk cells. All these cell types are potentiallyinteresting from a biological point of view.
T lymphocytes
T lymphocytes outnumber B lymphocytes inmammary secretions. Early studies haveindicated that they may represent a popu-lation of functional cells that selectivelymigrate in mammary secretions. Richie et al(1980) suggested that human colostrum Tlymphocytes are mostly activated lympho-cytes, as 50% of them form thermostablerosettes with sheep red blood cells, as com-pared with 3% of peripheral blood T cells. Awide range of functional properties wasestablished for these cells: the proliferativeresponse of sow colostral T cells to oval-
bumin (Evans et al, 1982), of rat and humancolostral T cells to mitogens, allogeneiccells, bacterial and viral antigens (Ogra etal, 1983; Parmely et al, 1976), the responseto transplantation antigens and the pro-duction of chemotactic factors (Nair et al,1985). However some contradictory obser-vations, such as the lower response ofthese cells to phytohaemagglutinin (PHA)and their reduced capacity to mediate anti-body-dependent cell cytotoxicity (ADCC)(Kohl et al, 1980), have made a clear-cutconsensus on their functions difficult: are
they functional cells, or are they simplybeing eliminated in the mammary secre-tions?
It is now clearly established that T lym-phocytes from mammary secretions areselected cells, with phenotypes differingfrom those encountered in peripheral blood,and that they are able to express in vitrofunctional capacities. In human mammarysecretions, 83% of the secreted lympho-cytes are T lymphocytes, with a CD4/CD8ratio significantly lower than that found in
peripheral blood. The main characteristic ofthis group of cells is the predominance ofmemory-activated T cell phenotypes. Themarkers of activation CDw29+, UCHL1+,LFA1+, 2H4CD45R-. HLA-DR and CD25(IL2-receptor) are expressed on 85% of milkT cells. This proportion is only 10% in periph-eral blood. Almost all CD4+ and CD8+ milkcells are CD45RO+RA-, indicating that theyrange from unprimed CD45RA+RO-T cellsto antigen-primed, memory T cells. Theexpression of CD2 (T11 ) and CD54 (ICAM-1) is twice as high in colostral lymphocytesas in blood lymphocytes (Bertotto et al,1990a, 1991; Eglinton et al, 1994; Wirt etal, 1992). There are twice as many lym-phocytes expressing the 7-6 T cell receptor(TCR) in human milk as in blood. These 7-6T cells in milk express non covalently boundy-6 chains, while in the blood most 7-6 Tcells express the disulphide-linked form ofTCR (Bertotto et al, 1991 The expressionof non covalently bound chains has beenshown to be associated with actin rear-
rangement and motility capacity after lym-phocyte activation (Grossi et al, 1989).These phenotypic characteristics are in cor-relation with the in vitro established func-tions of colostral T lymphocytes. They pre-sent a low proliferative response to
stimulation by PHA, respond to a wide rangeof bacterial and viral antigens and producesignificant amounts of gamma interferonwhen stimulated by mitogens or Newcastledisease virus. Similar to blood lymphocytes,milk lymphocytes proliferate and produce yinterferon in response to anti-CD2 and anti-
CD3. The phenotype and functional reper-toire of milk T lymphocytes are the sameas those of peripheral blood memory T cells(Bertotto et al, 1990b, 1991 It is clearlyestablished that T lymphocytes are antigen-pulsed cells, able to develop a secondaryimmune reponse, and that a directed andnot a random passage of T lymphocytesexists in human mammary secretions. Thesame conclusions have been obtained inother species.

The proportions of T lymphocytes amongmammary secretion cells and the T4/T8 ratioin secretions and in blood are respectively23, 1.0 and 2.3% in rat (Na and Seelig,1993; Na et al, 1992). In sheep, 67% of milklymphocytes are T lymphocytes with a T4/T8ratio of 0.36 (Ouzrout et al, 1991). In
bovines, the proportion of T lymphocytesvaries from 16% in the colostrum to 62% inlate lactation, with a T4/T8 ratio of 0.85 incomparison to 1.5 in blood (Park et al,1992). T Lymphocytes of bovine mammarysecretions express predominantly TCR a-[3and have a twofold higher level of CD2 andfivefold lower level of CD45R+ expression incomparison with peripheral blood lympho-cytes (Taylor et al, 1994). In swine, 10-25%of colostral cells are lymphocytes, of which70-90% are T cells, with a T4/T8 ratio (0.57)significantly lower than that of blood (0.80).In sow milk, less than 1 % of total cells are T
lymphocytes (Evans et al, 1982; Schollen-berger et al, 1986b; Le Jan, 1993, 1994).Sow colostral T lymphocytes do not expressinterleukin 2 receptors (IL2-R), but respondto mitogenic stimulation by proliferating andexpressing IL2-R (Le Jan, 1994).
B lymphocytes
Initial in vitro studies on the B lymphocytes inmammary secretions gave contradictoryresults in different experimental systems. Forexample, Crago and Mestecky (1984) didnot obtain immunoglobulin production afterstimulation of human colostral B lymphocyteswith pokeweed mitogen (PWM) or theEpstein-Barr virus, and suggested that, unlikeT lymphocytes, the colostral B lymphocyteswere non functional cells that were beingeliminated in mammary secretions. These
negative results could have been related tobackground contamination by macrophages,which could have masked the in vitro pro-duction of small quantities of IgA by the Bcells. Slade and Schwartz (1989), inducingautolysis of macrophages using a leucine-
O-methyl ester, demonstrated that humanmilk lymphocytes respond to in vitro stimu-lation by producing IgA. The in vitro func-tional capacities of B lymphocytes are estab-lished (Mestecky et al, 1991 After beingtransformed by the Epstein-Barr virus, celllines producing IgA, IgG and IgM have beenestablished from human milk B lymphocytes(Alvital et al, 1985; Shinmoto et al, 1992).
Neutrophils and macrophages
The functional capacity of neutrophils iso-lated from mammary secretions is uncer-
tain. The normal functions of phagocytosis,motility, respiratory burst and polymor-phonuclear (PMN)-mediated killing aredecreased in mammary secretion neu-
trophils, in comparison with those of theperipheral blood. They contain IgA, but donot release it during the phagocytosis oflatex particles (Kohl et al, 1980; Nair et al,1985; Schollenberger et al, 1986c;Ozkaragoz et al, 1988). In contrast, mam-mary secretion macrophages have estab-lished in vitro functional activities. They haveenhanced levels of motility and a greatercapacity to invade collagen gels in com-parison with blood monocytes (Okaragozet al, 1988). They contain IgA, which they lib-erate during the phagocytosis of latex par-ticles or opsonized bacteria by a mecha-nism that can be blocked by actin filamentinhibitors (Weaver et al, 1982, 1984). Theyexpress Class II antigens, and this expres-sion is enhanced by y interferon (Rivas etal, 1994). Mammary secretion macrophagesexpress in vitro characteristics of functional
phagocytic and antigen presenting cells.
Epithelial cells
In most species, epithelial cells representa minor component of the colostral cell pop-ulation. The capacity of these cells to grow

in vitro has been demonstrated in humansand bovines, where colostrum is a source ofcells for mammary gland epithelial cell cul-tures (Taylor-Papadimitriou and Strampfer,1991; Buehring, 1990). Genomic DNA andmRNA for P-casein have been isolated andamplified from human colostral epithelialcells (Lindquist et al, 1994). In contrast,epithelial cells represent a major compo-nent of the cells from mammary secretionsin swine. In sow milk, large epithelial cells,laden with fatty globules, secretory compo-nents and secretory IgA, represent morethan 60% of the total cell contents (Evans etal, 1982; Schollenberger et al, 1986a; LeJan, 1993). These cells do not grow in vitro,and have the characteristics of totally dif-ferentiated alveolar epithelial cells. Swinecolostrum contains more than 20% epithe-lial cells; these cells are small in size, with lit-tle or no cytoplasmic [gA, and have low lev-els of secretory component expression.They are able to grow in vitro for more thanthree passages. When cultivated in the pres-ence of lactating sow serum or an aqueousextract of sow colostrum, these cellsundergo differentiation and produce oc-lact-albumin. In culture, these cells are sensi-tive to the porcine coronavirus transmissiblegastroenteritis (TGE). They produce infec-tious virus particles and express viral anti-gens (Le Jan, 1993; Le Jan and Chevaleyre,1996b). They may also express Class II anti-
gens, depending on their degree of differ-entiation. Their in vitro capacity to processantigens is under investigation. We hypoth-esize that the epithelial cells from sowcolostrum can produce cytokines and canact as antigen-presenting cells.
Cytokines
It appears that free cytokines form an inte-gral part of mammary secretions, but to dateonly a limited amount of data is available.These data relate to some species and somecytokines. However, whenever a particularly
biologically important cytokine was lookedfor, it was found in the mammary secretionsin a biologically active form. In vitro, thecapacity of colostral, milk and mammarygland epithelial cells to produce cytokineshas been established. Human milk contains
y interferon at levels four times higher thanmaternal blood (Eglinton et al, 1994; Bocciet al, 1993), and significant amounts of inter-leukin 6 (IL-6) (Rudloff et ai, 1993; Bocci et al,1993). Tumour necrosis factor (TNF) is alsopresent in human milk (Rudloff et al, 1992). Inbovine mammary secretions, TNF-a is notpresent in the colostrum but is present in themilk throughout the lactation period, with adecrease in quantity four to six weeks beforeparturition (Rewinski and Yang, 1994; Sor-dillo et al, 1991 Transforming growth fac-tor (TGF)-p has been found in high concen-trations in early bovine colostrum, and itslevel decreases from the 12th hour after par-turition to reach a negligible level at the 30th(Tokuyama and Tokuyama, 1993). In
humans, TGF-# is present at a concentra-tion near 1 300 ng/mL in colostrum and 900ng/mL in milk (Saito et al, 1993). Humancolostrum contains high levels of interleukin1 (IL 1) (3, but no IL-1 a (Munoz et al, 1990).Epithelial cells from human and bovine mam-mary glands have been shown to produce,during in vitro cultures, IL-6, interleukin 8 (IL-8) and TNF (Palkowetz et al, 1994; Basolo etal, 1993). Mononuclear cells from humanmilk produce in vitro IL1 a and (3, IL-6, IL-8and TNF a (Skansen-Saphir et ai, 1993).Cells from rat milk, after in vitro non-specificstimulation by concanavalin A (ConA) or spe-cific stimulation by an antigen, produce TNF,interleukin 2 (IL-2) and IL-6 (Na and Seelig,1993).
DEMONSTRATIONSOF IN VIVO FUNCTIONSOF MAMMARY SECRETION CELLS
We present here the established informa-tion concerning the interactions between

mammary secretion cells and the newborn:the fate of colostral cells after ingestion, theeffects of cellular components on immunedefenses and immunological parameters.
Fate of colostral cells in the newborn
It is clearly established in many speciesincluding mice (Weiler et al, 1983), ovines(Schnorr and Pearson, 1984; Tuboly et al,1995), primates (Jain et al, 1989) and swine(Tuboly et al, 1988; Williams, 1993; Le Janet al, 1995) that colostral cells are able tocross the neonatal intestinal barrier. All theabove studies, using cell labelling by fluo-rochromes or radioactive markers, were per-formed during a short period (up to 60 hafter ingestion). This is too short a timeperiod for an evaluation of the duration ofthe persistence of maternal cells in the new-born; however, semi-allogeneic maternalcells are accepted by neonatal intestinalmucosa. After ingestion, maternal cells havebeen detected in intestinal mucosa, mesen-teric lymph nodes, blood, lungs, liver andspleen. In pigs this absorption is restricted tothe duodenum and jejunum, with preferen-tial passage in the duodenum (Le Jan et al,1995). The mechanism of entry of colostralcells into the intestinal mucosa is not estab-
lished. However, specific recognition ofmaternal cells has been established in the
pig during in vivo and ex vivo experiments(Tuboly et al, 1988; Williams, 1993). Onlymaternal colostral cells can pass throughthe intestinal barrier; maternal peripheralblood leukocytes (PBL) and colostral cellsfrom a different sow cannot. No similar donorrestriction exists in primates, as Jain et al(1989) have shown in the trans-intestinalabsorption of human colostral cells in new-born baboons. The duodenal epithelium ofpiglets does not express Swine leukocyteantigens (SLA) Class 1 antigens during thefirst four days following birth. The level ofexpression is lower on the jejunal epithe-
lium of piglets than in adult pigs (Le Jan andChevaleyre, 1996a). This reduced expres-sion of SLA Class 1 relates to its ability toaccept maternal cells, but is more likely anindication of the immaturity of the neonatalintestinal epithelium. In humans, major his-tocompatibility complex (MHC) Class 1 anti-gens are fully expressed by the neonatalintestinal epithelium (Rognum et al, 1992).
Established protection in experimentalmodels
There are few experimental demonstrationsof in vivo protective effects of cells frommammary secretions, but those that do existare clearly conclusive. There are many dif-ficulties in evaluating the effects of cellularcomponents on neonatal diseases. In lethaldiseases of newborns, such as transmissi-ble gastroenteritis in piglets, the evolutiontime of the disease is short, and it is believedthat in order for a defence to be effective it
must act quickly. The immune exclusion bysecretory IgA is likely to be more efficientthan a specific cellular immunity. In orderfor a disease to be an effective model for
assessing the contribution of cellulardefence, one must be able to quantify thisdefensive response. Up to now, establishedmodels have concerned parasitic and viraldiseases. The reference model demon-
strating cellular protection by cells frommammary secretions is the infestation of
newborn rats by Trichinella spiralis. In thisdisease, it is established that the inflam-
matory events leading to the expulsion ofthe parasites from the intestine is due tospecific T lymphocytes. Female rats immu-nized against Trichinella spiralis are able totransfer immunity to the suckling newborns.The degree of protection is quantified bythe number of parasites harboured in theintestine after a challenge. Cross-fosteringexperiments have established that the pro-tection is conferred by the milk of the immu-

nized mother; non-immune mothers receiv-ing intravenously mesenteric T lymphocytesfrom immunized syngeneic rats, can protecttheir sucklings through their milk, as well asthe direct per os administration of sensitizedT lymphocytes to the newborn (Kumar et al,1989, 1990; Na et al, 1992). In another par-asitic model, infestation of mice byHymenolepis nana, suckling neonates areprotected after the inoculation of lactatingmothers with lymph-node cells from immu-nized mice, or by direct ingestion of thesecells. This transfer of protection is abrogatedby pre-treatment of the cells with anti-Thy-1.2monoclonal antibody and complement(Asano and Okamoto, 1992). In newborncalves, colostral lymphocytes contribute tothe protection against an experimental infec-tion by a rotavirus (Archambault et al, 1988).Protection after the challenge is quantifiedby the duration of the virus excretion in thefeces. The protection is complete, that is,there is no virus excretion, after the admin-istration of immune colostrum without cells.There is no difference between the controlcalves and calves receiving colostral lym-phocytes from non-immunized mothers.There is, however, a significant decrease inthe duration of the viral excretion and thelevel of virus titers in feces, after a challengebetween calves receiving immune-mothercolostral lymphocytes and control calves orcalves receiving colostral lymphocytes fromnon-immunized mothers. This establishesthe fact that colostral immunized lympho-cytes reduce the disease course.
Effects on immunological parametersof newborn
Cases where cellular immunity has beentransmitted by mammary secretions havebeen observed. In humans, delayed-typereactions can be transmitted by breast-feed-ing against schistosomal antigens (Eissa etal, 1989) and tuberculin (Mohr, 1972). Ograet al (1977) have shown a transient sensi-
tivity of blood lymphocytes from infantsbreast-fed from an immunized mother to the
purified protein derivative of Mycobacteriumtuberculosis; however, their conclusion that’at the moment, it is difficult to determinewhether such reactivity represents uptakeof antigen-sensitized intact cells or a sim-ple absorption of pharmacological media-tors released by T lymphocytes during theirpassage through the intestinal tract of thenewborn’ remains valid and illustrates theneed for caution in the interpretation of invivo-measured effects of colostral cellular
components.
Mycobacterium-reactive y/8 T cells arepresent in the colostrum of tuberculin-posi-tive mothers (Bertotto et al, 1993). This cor-relates well with the presence of sensitized
lymphocytes in the newborn, but does notimply that delayed-type skin sensitivity isnecessarily due to these maternal cells.Pabst et al (1989) have shown an enhancedlymphoblastic response to BCG vaccina-tion in breast-fed infants, in comparison withinfants reared on milk formulae, and thiswas not related to the immune status of themother. This result indicates that a non-spe-cific enhancement of cellular responses tocertain antigens by mammary secretionscan exist. This could be due to the cellular oracellular components of mammary secre-tions.
In mice (Zhang and Miller, 1993), thereis a cellular and humoral hypoimmuneresponse to non-inherited maternal MHC
antigens. After the ingestion of maternal milk,maternal cells are present in the lymphnodes of newborn. The observation thatthere is a prolonged survival of maternal skingrafts suggests that the transferred maternalT cells selectively inactivate host T cellscapable of recognizing them. Cross-fosteringexperiments in mice have also shown thatmilk-feeding modifies the recognition ofMHC, even though the mechanism for this(cells or other factors) is not yet established(Nepomnaschy et al, 1988).

In calves (Riedel-Caspari, 1993), com-parisons of the effects of different diets(colostrum with or without cells, milk sub-stitutes with or without a colostral cell sup-plement) have shown that following colostralcell ingestion there is a higher response ofblood lymphocytes to non-specific mitogensand a higher level of seric antibody forma-tion. This is in agreement with observationsby Brenner et al (1986), that breast-fedinfants have a higher level of lymphocyteresponse in the early weeks after birth. Inpiglets (Williams, 1993) there is a signifi-cant augmentation of the PBL response toPHA, ConA and PWM after colostral cellshave been ingested by the newborn. Tubolyet al (1995), using tetanus anatoxin as anantigen, demonstrated that maternalcolostral lymphocytes remain immunologi-cally active after trans-intestinal absorptionacross the newborn intestinal mucosa, andthat these cells transfer an immunologicalmemory.
RESEARCH NEEDSAND DEVELOPMENTS
It is clearly established that mammary secre-tions contain a wide range of factors poten-tially able to interact with the immatureneonatal local immune system, at a timewhen this system is confronted with contactwith various antigens simultaneously. It is
therefore probable that the newborn’s intesti-nal immune system must be capable of rec-ognizing the type of response to develop(humoral or cellular immune exclusion, ortolerance), and that the maternal cells,cytokines, growth factors, hormones andimmunomodulatory substances of colostrumand milk may influence the stages in theprocess of recognition of self and of foreignantigens during this critical neonatal period.It is also clear that the topic of neonatalactive immunity is poorly understood. Trans-mission of passive immunity by lactogenic
immunity and active immunity of the youngafter weaning have been much more clearlyelucidated in their fundamental and practicalaspects.
The questions can be defined in verysimple terms: How do colostrum and milkreduce neonatal pathology? What are theroles of the immune components ofcolostrum and milk in the establishment ofthe local immunity of neonate? How couldthese effects be modulated? The answersto these questions would involve: (i) improv-ing the understanding and control of atopicdiseases and alimentary allergies, particu-larly in humans; (ii) reducing neonatalpathology in animal production; (iii) improv-ing zootechnical potentialities in intensiveproduction systems where losses due topathology are mostly due to the effect ofan inadequate balance between oppor-tunistic, or occasionally pathogenic, ubiq-uitarious germs and organisms; and (iv)elaborating neonatal vaccination strategiesand manufacturing improved milk substi-tutes. This implies an integrated experi-mental approach, which should includeimmunology, physiology and developmen-tal biology.
Migration patterns of colostral cellsin newborn
Semi-allogeneic maternal colostral cells areaccepted by the newborn intestinal mucosa,and the experimental data suggest thatthese cells persist in newborn organismslong enough to exert their functions. Manyquestions remain to be resolved about thismigration; regarding the mechanisms oftransepithelial crossing, their persistence inthe newborn, and the phenotype and local-ization of migrating cells. It is established
that in mice primates, ruminants, rabbitsand pigs, colostral cells cross the intestinalbarrier and persist during the time period ofthe experimental surveys, which have not

exceeded 60 h up until now. The migrationmechanism has not been elucidated. Spe-cific recognition of colostral maternal cellshas been established in swine (Tuboly etal, 1988; Williams, 1993), during both in vivoand ex vivo experiments. The results indi-cate that an active process, which presum-ably implies colostral cells and mucosalepithelium, occurs. The enhanced mobility ofhuman colostral macrophages (Ozkaragozet al, 1988), and the predominance ofhuman colostral y-6 T cells expressing non-covalently linked TCR chains (Bertotto etal, 1991) support the hypothesis of an activemigration of colostral cells in humans. Thedegree of maturation of the neonatal intes-tine could also be a determining factor, assuggested by the decreased levels of SLAClass 1 antigens expressed by the intestinalepithelium of newborn piglets (Le Jan andChevaleyre, 1996a). It can be hypothesizedthat colostral lymphocytes migrate to thelymph nodes and the macrophages andepithelial cells to the mucosal surfaces, assuggested by the fact that the same mem-brane determinants are shared by colostraland pulmonary human macrophages (Biondiet al, 1984). The model of in vitro interac-tion between colostral cells and neonatalintestine explants established by Williams(1993) in pigs offers a useful methodologicalapproach for the study of colostral cell migra-tions. A technique is being developed in ourlaboratory which labels pig-blood lympho-cytes and colostral cells with PKH26, analiphatic fluorochrom (Horan et al, 1990).Maternal blood lymphocytes intravenouslytransferred to histocompatible piglets weredetected in the recipient blood with this newtechnique during a 15-day survey, and thelabelling did not impair the in vitro functionsof the colostral cells (transformation of Tlymphocytes in response to mitogenic stim-ulation, and in vitro growth of epithelial cells).This method could be used for trackingcolostral cells in piglets and for phenotypiccharacterization.
Functions of mammary secretion cells
Lymphocytes
T lymphocytes are both the most prevalentand the most active of the lymphocytes pre-sent in mammary secretions. B lymphocytesselectively accumulate in the mammarygland during gestation (Chabaudie et al,1993). Their primary established function isto synthesize dimeric IgA, which will thenbe translocated and excreted in the milk
throughout lactation. Since the B lympho-cytes would secrete the same IgA in thenewborn as they already have been shownto secrete in the mammary gland, the new-born does not really need these maternalB lymphocytes. Depending on the pheno-typic and in vitro functional characteristics ofcolostral T lymphocytes, these T cells prob-ably transfer immune functions to theneonate and also secrete cytokines. Theestablished immunoprotective functions ofmammary secretions, such as the transfer ofcellular immunity and protection againstinfectious disease, suggest mediationassumed by CD4 and CD8 cells. Based onthe in vitro results it could be expected thatCD4 cells would produce INF-y, TNF-# andIL-2 cytokines in the newborns. In fact, inter-feron y levels are increased in human milk
(Eglinton et ai, 1994; Wirt et al, 1992). It is
possible that immunoregulatory factors inmammary secretions maintain activated T
lymphocytes in a latent phase and delay thesecretion of soluble factors by these cells.Since the CD8/CD4 ratio is higher in mam-mary secretions than in the blood and sincethe CD8 have been shown to be activated in
humans, it is expected that they produceIL-4 and TGF (3, which is known to be animmunosuppressor factor. This role is sus-pected in TNF (3 knock-out mice, whoremain free of spontaneous inflammationduring the suckling period (Kulkarni andKarlsson, 1993). The enhanced proportionof T8 lymphocytes in mammary secretionscould contribute to the natural immunosup-

pressive properties of breast milk, allowinga controlled activation of the immune systemduring weaning. Two research directionsneed to be explored: the analysis of the cel-lular immunity transfer and helper functionsof T4 cells, and the study of the control ofimmune activation by T8 cells.
Phagocytes and epithelial cells
Since polymorphonuclear neutrophils iso-lated from mammary secretions havereduced functional capacities such as motil-ity and phagocytosis, it seems likely thattheir role is essentially devoted to thedefense of the mammary gland. This sup-position is supported by the author’s obser-vations that most neutrophils from sowcolostrum are destroyed during the wash-ing steps used for cell preparations, and fur-ther supported by the fact that in instancesof subclinical mammary gland inflammation,colostral and milk cell preparations are con-taminated by high numbers of live neu-trophils. Macrophages from mammarysecretions are active in vitro and could con-
tribute to neonatal immune defenses byphagocytosis and IgA excretion (Weaver etal, 1982, 1984). As proposed by Ozkaragozet al (1988), they could invade the intesti-nal mucosa and interact with intestinal
epithelium. Their expression of Class II anti-gens is enhanced by y interferon (Rivas et al,1994), and the internalization of the anti-gens present in the mammary gland by themacrophages could in fact be enhanced byIgA. Their principal role in the newbornshould be to act as cytokine-producing (Poli-tis et al, 1991) and antigen-presenting cells.
Epithelial cells are a major componentof mammary secretions in swine. In sow
milk, they represent 60-90% of the totalnumber of cells, and it has been concluded(Le Jan, 1993) that they are exfoliated fromthe alveolar epithelium and that they con-tribute to the transfer of secretory IgA to theneonatal intestine. The IgA that is normally
present in mammary secretions has passedthrough a classic trans-mammary epithe-lium translocation. If, however, the IgA isliberated from the epithelial cells by cell lysisin the gastric or intestinal lumen, it will have
a non-cleaved secretory component, and,as a result, different properties (mucus adhe-sion, resistance to proteolysis). In sowcolostrum, epithelial cells can grow and dif-ferentiate in vitro, and can express viral anti-
gens after in vitro infection. This capacitysuggests that they could interact with thelocal immune system of the piglet bycytokine secretion and antigen presenta-tion after passage through the intestinal bar-rier.
It may be of significant interest for theneonate immune system that maternal cells,which have already processed foreign anti-gens, can pass through the neonate intesti-nal barrier. These processed antigens wouldinduce an immunity in the neonate that it
might not otherwise have been able tomount for itself, because for example: (i)the antigen had been captured by IgA; (ii) alocal immune response was rendered diffi-
cult by the rapid cell division occurring inthe neonate intestine or the lack of receptorson neonate cells; or (iii) epitopes might bepresented that are different from those thatthe newborn antigen-presenting cells wouldhave processed. Mammary secretionscould, by way of antigen presentation, directand modulate the newborn response to spe-cific antigens, and could act on the balancebetween immune response, tolerance and
allergy. This aspect is being studied in ourlaboratory. A model of in vitro culture ofcolostral epithelial cells is being developedto analyse the processing of antigens bysecretory component and IgA. Antigens ofTGE coronavirus are being used. Possiblefurther developments are the analysis oflocal piglet immune response after theadministration of antigen-presenting colostralcells. Another suggested role for
macrophages and epithelial cells is a local

secretion of cytokines, which would inter-act with the local immunity of the newborn.This can now be studied through the detec-tion of secreted cytokines and also theexpression of specific mRNA using labelledcolostral cells in newborn intestinal mucosa.
CONCLUSION
It is established that mammary secretionsconstitute a cellular link between the motherand newborn. The information presentedhere seems to indicate that these cells exert
biological functions. Experimental modelshave demonstrated the protective proper-ties of these cells. It can be considered that,under natural conditions, specific cellularprotection is not the major role of colostrumand milk lymphocytes. If, for a givenpathogen, there is specific T lymphocyte inthe colostrum or milk, it can be assumedthat a specific secretory IgA will also be pre-sent, and that the immune exclusion mech-anisms acting during lactation will be moreefficient than cellular cytotoxicity. Trans-mission of immune memory has beendemonstrated by mammary secretion cellsand could be of primary importance to thenewborn. Many factors other than specificmemory T lymphocytes could enhance pri-mary antigenic stimulation, for example thepresence of immunomodulatory substancesin mammary secretions and the possibleeffects of anti-idiotypic antibodies (Telemo etal, 1991). The immunoregulatory effect ofcells from mammary secretions is stronglysupported by the predominance and char-acteristics of T8 lymphocytes in the
colostrum and milk. It is clearly establishedthat breast-feeding reduces atopic diseasesin humans (Saarinen and Kajoosaari, 1995),although the intervention of cellular com-ponents has not yet been demonstrated.
Antigenic stimulation and orientation ofimmune responses of the neonatal intes-tine may be one of the most important func-
tions of mammary secretion cells. Theneonatal intestine represents a unique sys-tem. It consists of an immature mucosa,untouched by previous antigen contacts,that receives adult antigen-presenting cellswhich are not recognized as foreign cells.This is the case for macrophages, and pre-sumably for colostral epithelial cells in swine.Further investigations are necessary toassess the capacity of mammary secretionmacrophages, and colostral epithelial cellsin swine, to induce local immune responsesin the newborn. This is a critical period forthe neonate and the orientation of its
adapted responses to various antigens isof crucial importance for the survival anddevelopment of the young.
ACKNOWLEDGMENTS
The author thanks F Guiguen for many fruitfuldiscussions and E Thompson for her English revi-sion of the manuscript.
REFERENCES
Alvital A, Tamir S, Steimeitz M (1985) Continuous invitro production of IgA by a human colostral immor-talized cell line. fmmunof Left 9. 23-27
Archambault D, Morin G, Elazhary T, Roy RS, Joncas JH(1988) Immune response of pregnant heifers andcows to bovine rotavirus inoculation and passiveprotection to rotavirus infection in newborn calvesfed colostral antibodies or colostral lymphocytes.Am J Vet Res 49, 1084-1091
Asano K, Okamoto K (1992) Transfer of T-cell medi-ated immunity of Hymenolepis nana from mothermice to their neomates. Experientia 48, 67-71
Basolo F, Conaldi PG, Fiore L, Calvo S, Toniolo A (1993)Normal breast epithelial cells produce interleukins6 and 8 together with tumor-necrosis factor: defectiveIL6 expression in mammary carcinoma. Int J Cancer55, 926-930
Bernard S, Aynaud JM, Salmon H (1983) Le lait de truie :composantes humorales et cellulaires de la protec-tion pour le jeune porcelet. J Rech Porc Fr 15, 401-412
Berthon P, Salmon H, Martinet J, Houdebine LM (1993)Immunological factors in mammary secretions. In:

Biologie de la lactation (J Martinet, ed), INRA Ver-sailles, 389-141
Bertotto A, Castellucci G, Fabietti G, Scalise F, VaccaroR (1990a) Lymphocytes bearing the T cell receptorin human breast milk. Arch Dis Child 65, 1274-1275
Bertotto A, Gerli R, Fabietti F, Crupi S, Arcangeli C,Scalise F, Vaccaro R (1990b) Human breast milk Tlymphocytes display the phenotype and functionalcharacteristics of memory T cells. Eur J Immunol
20, 1877-1880
Bertotto A, Gerli R, Castellucci G, Scalise F, Vaccaro R(1991) Human milk lymphocytes bearing the y/8 T-cellreceptor are mostly 6 TCS1-positive cells. Immunol-ogy 74, 360-363
Bertotto A, Gerli R, Castellucci G, Crupi S, Scalise F,Spinozzi F, Fabietti G, Forenza N, Vaccaro R (1993)Mycobacteria-reactive y/2i T cells are present inhuman colostrum from tuberculin-positive, but nottuberculin-negative nursing mothers. Am J ReprodImmunol29, 131-134
Biondi A, Rossing TH, Bennett J. Todd RF (1984) Sur-face markers heterogeneity among human mononu-clear phagocytes. J lmmunol 132, 1237-1243
Bocci V, von Bremen K, Corradeschi F, Franchi F, LuzziE, Paulesu L (1993) Presence of interferon-y andinterleukin-6 in colostrum of normal women. Lym-phokine Cytokine Res 12, 21-24
Brenner MK, Duffy SW, Lakhani PK, Kennedy CR. Far-rant J (1986) The effect of breast-feeding on prolif-eration by infant lymphocytes in vitro. Pediatr Res20, 227-231
Buehring GC (1990) Culture of mammary epithelial cellsfrom bovine milk. J Dairy Sci 73, 956-963
Chabaudie N, Le Jan C, Olivier M, Salmon H (1993)Lymphocyte subsets in the mammary gland of sows.Res Vet Sci 55, 351-355
Chernishov VP, Sluvkin II (1990) Mucosal immunity of themammary gland and immunology of mother/new-born interrelation. Arch Immunol Ther Exp 38, 145-164
Crago SS, Prince SJ, Pretlow TG, McGhee JR, MesteckyJ (1979) Human colostral cells. I. Separation andcharacterization. Clin Exp lmmunol 38, 585-597
Crago SS, Mestecky J (1984) Human colostral cells. II.
Response to mitogens. Celllmmunof 86. 222-229
Eglinton BA, Robertson DM, Cummins AG (1994) Phe-notype of T cells, their soluble receptor levels, andcytokine profile of human milk. Immunol Cell Biol72, 306-313 3
Eissa AM, Saad MA, Abdel-Ghaffar AK, el-SharkawayIM, Kamal KA (1989) Transmission of lymphocyteresponsiveness to schistosomal antigens by breast-feeding. Trop Geogr Med 41, 208-212 2
Evans PA, Newby TJ, Stokes CR, Bourne FJ (1982) Astudy of cells in the mammary secretions of sow.Vet Immunol Immunopathol3, 515-527
Grossi CE, Ciccone E, Migone N, Bottino C, ZarconeD, Mingari MC (1989) Human T cells expressing the!1-6 T-cell receptor (TcR-1 ): y 1 and C y encodedforms of the receptor correlate with distinctive mor-phology, cytoskeletal organization and growth char-acteristics. Proc Natl Acad Sci USA 86, 1619-1623
Horan PK, Melnicoff MJ, Jensen D, Slezak SE (1990)Fluorescent cell labeling for in vivo and in vitro celltracking. In: Methods in Cell Biology, Volume 33:Flow Cytometry (Z Darzynkiewicz, HA Crissman,eds), Academic Press, New York, 469-490
Jain L, Vidyasagar P, Xanthou M, Ghal V, Shimada S,Blend M (1989) In vivo distribution of human milkleucocytes after ingestion. Arch Dis Child 64/S, 930-933
Kohl S, Pickering LK, Cleary TG, Steinmetz KD, Loo LS(1980) Human colostral cytotoxicity. 11. Relative
defects in colostral leukocyte cytotoxicity and inhi-bition of peripheral blood leukocyte cytotoxicity bycolostrum. J Infect Dis 142, 884-891
Kulkarni AB, Karlsson S (1993) Transforming growthfactor p 1 knockout mice. A mutation in one cytokinegene causes a dramatic inflammatory disease. AmJ Pathol 143, 3-9
Kumar SN, Steward GK, Steven WM, Seelig LL (1989)Maternal to neonatal transmission of T-cell medi-
ated immunity to Trichinella spiralis during lactation.Immunology 68, 87-92
Kumar SN, Stewart GL, Steven WM, Seelig LL (1990)Role of T cell subsets in the maternal-to-neonatal
transmission of immunity against Trichinella spiralisduring lactation in rats. J Reprod Immunol 17, 69-78
Le Jan C (1993) Secretory component and IgA expres-sion by epithelial cells in sow mammary gland andmammary secretions. Res Vet Sci 55, 265-270
Le Jan C (1994) A study by flow cytometry to lympho-cytes in sow colostrum. Res Vet Sci 57, 300-304
Le Jan C, Chevaleyre C (1996a) Reduced expression ofSLA Class 1 antigens by intestinal epithelium ofnewborn piglets. Vet Immunol Immunopathol, inpress
Le Jan C,Chevaleyre C (1996b) Cellules 6pith6liales ducolostrum de truie : sensibiiite au virus GET et pro-priétés in vitro. J Rech Porc Fr28, 303-306
Le Jan C, Le Dividich J, Chevaleyre C, Hulin JC (1995)Devenir des cellules colostrales chez le porc nou-veau-né. J Rech Porc Fr27, 91-96
Lindquist S, Hansson L, Hernell 0, Lonnerdal B, Nor-mak J, Stromquist M, Bergstrom S (1994) Isolation ofmRNA and genomic DNA from epithelial cells inhuman milk and amplification by PCR. Biotechniques17, 692-496
Magnusson U, Rodriguez-Martinez H, Einarsson S(1991) A simple, rapid method for differential cellcounts in porcine mammary secretions. Vet Rec 30,485-488

Mestecky J, Moldoveanu Z, Prince SJ, Kutteh WH, Kul-havy R, McGhee JR, Moro 1, Crago SS (1991)Immunological properties and differentiation poten-tial of human colostral lymphocytes of B cell lineage.Adv Exp Med Biol 310, 123-129
Mohr JA (1972) Colostrum and delayed hypersensitivity.Am Rev Resp Dis 105, 985-986
Munoz C, Endres S, van der Meer J, Schlesinger L,Arevalo M, Dinarello C (1990) Interleukin-1 (1 inhuman colostrum. Res Immunol 141, 505-513 3
Na HR, Hiserodt JC, Seelig LL (1992) Distribution oflymphocyte subsets in rat milk from normal andTrichinella spiralis-infected rats. J Reprod Immunol22, 269-279
Na HR, Seelig LL (1993) In vitro TNF, IL-6 and IL-2 pro-duction by rat milk cells following Trichinella spiratisinfection. J Reprod Immunol25, 119-131 1
Nair MPN, Schwartz SS, Slade HB (1985) Comparisonof cellular cytotoxic activities of colostral lympho-cytes and maternal peripheral blood lymphocytes.J Reprod Immunol7, 199-207
Nepomnaschy I, Deroche A, Pasqualini CD, Piazzon I
(1988) Maternal influence on the immune response:SMLC reactions between identical and reciprocalF1 hybrids and the role of lactation Immunol Lett18, 19-25
Ogra SS, Weintraub D, Ogra PL (1977) Immunologicalaspects of human colostrum and milk. III. Fate and
absorption of cellular and soluble components in thegastrointestinal tract of the newborn. J /mmuno/119,245-248
Ogra PL, Losonki GA, Fishaut M (1983) Colostrum-derived immunity and maternal-neonatal interac-tion. Ann N YAcad Sci 409, 82-87
Ozkaragoz F, Rudloff HB, Rajaraman S, Mushtaha AA,Schmalstieg FC, Goldman AS (1988) The motilityof human milk macrophages in collagen gels. Pedi-atr Res 23, 449-452
Ouzrout R, Guiguen F, Lerondelle C (1991) Evolutiondes sous-populations lymphocytaires dans le lait debrebis au moment de !’excretion du virus Maedi. AnnRech Vet 22, 379-386
Pabst HF, Godel J, Grace M, Cho H (1989) Effect ofbreast-feeding on immune response to BCG vacci-nation. Lancet8633, 295-297
Palkowetz KH, Royer CL, Garofalo R, Rudloff HE,Schmalstieg FC, Goldman AS (1994) Production ofinterleukin-6 and interleukin-8 by human mammarygland epithelial cells. J Reprod Immunol26, 57-64
Park YH, Fox LK, Hamilton MJ, Davis WC (1992) Bovinemononuclear leukocyte subpopulations in periph-eral blood and mammary gland secretions duringlactation. J Dairy Sci75, 998-1006
Parmely MJ, Beer AE (1977) Colostral cell-mediatedimmunity and the concept of a common immune sys-tem. J Dairy Sci 60, 655-665
Parmely MJ, Beer AE, Billingham RE (1976) In vitrostudies on the T lymphocytes population in humanmilk. J Exp Med 144, 358-362
Politis, McBride BW, Burton JH, Zhao X, Turner JD
(1991) Secretion of interleukin-1 by bovine milkmacrophages. Am J Vet Res 52, 858-862
Rewinski MJ, Yang TJ (1994) Lactation stage-depen-dent changes in levels of tumor necrosis
factor/cachectin in milk. Am J Reprod Immunol 31, 1 ,170-176
Richie ER, Steinmetz KD, Meistrich ML, Ramirez I,Hilliard JK (1980) T lymphocytes in colostrum andperipheral blood differ in their capacity to form ther-mostable rosettes. J Immunol 125, 2344-2346
Riedel-Caspari G (1993) The influence of colostral leuko-cytes on the course of an experimental Escherichiacoli infection and serum antibodies in neonatal
calves. Vet Immunollmmunopatho/35, 275-288
Rivas RA, el Mohandes AA, Katona IM (1994) Mononu-clear phagocytic cells in human milk: HLA-DR and Fcgamma R ligand expression. Biol Neonate 66, 195-204
Rognum TO, Thrane PS, Stoltenberg L, Vege A,Brandtzaeg P (1992) Development of intestinalmucosal immunity in fetal life in the first postnatalmonths. Pediatr Res 32, 145-149
Rudloff HB, Schmalstieg FC, Mushtaha AA, PalkowetzKH, Liu SK, Goldman AS (1992) Tumor necrosisfactor-a in human milk. Pediatr Res 31, 29-33
Rudloff HE, Schmalstieg FC, Palkowetz KH,Paszkiewicz, Goldman AS (1993) Interleukin-6 inhuman milk. J Reprod Immunol23, 13-20
Saarinen UM, Kajoosaari M (1995) Breastfeeding at pro-phylaxis against atopic disease: prospective follow-up study until 17 years old. Lancet 346, 1065-1069
Saito S, Ichijo S. Ishizaka S, Tsujii T (1993) Transform-ing growth factor-13 (TGF-!) in human milk. Clin ExpImmunol94, 220-224
Salmon H (1987) The intestinal and mammary immunesystem in pigs. Vet Immunol Immunopathol 17, 367-388
Schnorr KL, Pearson LF (1984) Intestinal absorption ofmaternal leucocytes by newborn lambs. J ReprodImmunol6, 329-337
Schollenberger A, Frymus T, Degorski A, SchollenbergerA (1986a) Cells of sow mammary secretions. I. Mor-
phology and differential counts during lactation. JVet Med 33, 31-38
Schollenberger A, Frymus T, Degorski A, SchollenbergerA (1986b) Cells of sow mammary secretions. 11.Characterisation of lymphocyte populations. J VetMed 33, 39-46
Schollenberger A, Frymus T, Degorski A, SchollenbergA (1986c) Cells of sow mammary secretions. 111.
Some properties of phagocytic cells. J Vet Med 33,353-359

Shinmoto H, Dosako S, Tanaka S (1992) Transformationof human colostrum lymphocytes with Epstein-Barrvirus. Tokai J Exp Clin Med 17, 129-132
Skansen-Saphir U, Lindfors A, Andersson U (1993)Cytokine production in mononuclear cells of humanmilk studied at the single-cell level. Pediatr Res 34,213-216 6
Slade HB, Schwartz SA (1989) Antigen-drivenimmunoglobulin production by human colostral lym-phocytes. Pediatr Res 25, 295-299
Sordillo LM, Redmond MJ, Campos M, Warren L,Babiuk-LA (1991) Cytokine activity in bovine mam-mary gland secretions during the periparturientperiod. Can J Vet Res 55, 298-301
Taylor BC, Dellinger JD, Cullor JS, Stott JL (1994) Bovinemilk lymphocytes display the phenotype of memoryT cells and are predominantly CD8+. Cell lmmunol156, 245-253
Taylor-Papadimitriou J, Stampfer MR (1991) Culture ofhuman mammary epithelial cells. In: Culture of
Epithelial Cells (RI Freshney, ed), Wiley-Liss, NewYork, 107-133
Telemo E, Bailey M, Miller RG, Stokes CR, Bourne FJ(1991) Dietary antigen handling by mother and off-spring. Scand J Immunol34, 689-696
Tokuyama Y, Tokuyama H (1993) Purification and iden-tification of TGF J3 2 related growth factor from bovinecolostrum. J Dairy Res 60, 99-109
Tuboly S, Bernath S, Glavits R, Medveczy I (1988)Intestinal absorption of colostral lymphoid cells innewborn piglet. Vet Immuno//mmunopatho/20, 75-85
Tuboly S, Berath S, Glavits R, Kovacs A, Megyeri Z(1995) Intestinal absorption of colostral lymphocytesin newborn lambs and their role in the developmentof immune status. Acta Vet Hung 43, 105-115 5
Weaver EA, Tsuda H, Goldblum AS, Davis CP (1982)Relationship between phagocytosis and immunoglob-ulin release from human macrophages. Infect Immun38, 1073-1077
Weaver EA. Rudloff HE, Goldblum RM, Davis CP, Gold-man AS (1984) Secretion of immunoglobulin A byhuman milk leukocytes initiated by membrane stim-ulation. J Immunol 132, 684-689
Weiler IJ, Hickler W, Sprenger R (1983) Demonstrationthat milk cells invade the suckling neonatal mouse.Am J Reprod Immunol4, 95-98
Williams PP (1993) Immunomodulating effects of intesti-nal absorbed maternal colostral leukocytes by neona-tal pigs. Can J Vet Res 57, 1-8
Wirt DP, Adkins LT, Palkowetz KH, Schmalstieg FC,Goldman AS (1992) Activated and memory T lym-phocytes in human milk. Cytometry 13, 282-290
Zhang L, Miller RG (1993) The correlation of prolongedsurvival of maternal skin grafts with the presence ofnaturally transferred maternal T cells. Transplantation56, 918-921