CELL BIOLOGY Copyright © 2020 Optogenetic stimulation of ... · regulation are not well...
Transcript of CELL BIOLOGY Copyright © 2020 Optogenetic stimulation of ... · regulation are not well...

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
1 of 12
C E L L B I O L O G Y
Optogenetic stimulation of phosphoinositides reveals a critical role of primary cilia in eye pressure regulationPhilipp P. Prosseda1, Jorge A. Alvarado1, Biao Wang1, Tia J. Kowal1, Ke Ning1, W. Daniel Stamer2, Yang Hu1, Yang Sun1,3*
Glaucoma is a group of progressive optic neuropathies that cause irreversible vision loss. Although elevated intra-ocular pressure (IOP) is associated with the development and progression of glaucoma, the mechanisms for its regulation are not well understood. Here, we have designed CIBN/CRY2-based optogenetic constructs to study phosphoinositide regulation within distinct subcellular compartments. We show that stimulation of CRY2-OCRL, an inositol 5-phosphatase, increases aqueous humor outflow and lowers IOP in vivo, which is caused by a calcium- dependent actin rearrangement of the trabecular meshwork cells. Phosphoinositide stimulation also rescues defective aqueous outflow and IOP in a Lowe syndrome mouse model but not in IFT88fl/fl mice that lack functional cilia. Thus, our study is the first to use optogenetics to regulate eye pressure and demonstrate that tight regulation of phosphoinositides is critical for aqueous humor homeostasis in both normal and diseased eyes.
INTRODUCTIONGlaucoma is a group of neurodegenerative diseases of the optic nerve and a leading cause of irreversible blindness. In all forms of glaucoma, the loss of retinal ganglion cells (RGCs) leads to permanent vision loss (1). Lowering intraocular pressure (IOP) is currently the only effective treatment for glaucoma in both children and adults. Identifying the underlying mechanisms for IOP regulation is critical for understanding the pathogenesis of glaucoma.
Regulation of IOP involves a wide range of different signaling molecules, which directly or indirectly control the resistance to out-flow of aqueous humor (2). Increasing evidence suggests that extra-cellular matrix and actin cytoskeleton in the trabecular meshwork (TM) play critical roles in modulating outflow (3, 4). TM cells are specialized cells that are derived from the neural crest and are located in the iridocorneal angle of the eye. Because aqueous humor is pro-duced by the ciliary body of the eye and primarily drained via the TM outflow track, defects in this region cause aqueous humor buildup and a subsequent rise in IOP (5–7).
Primary cilia are conserved solitary organelles that are important mechano- or chemosensors in a number of organ systems, including the brain, kidney, and bone (8, 9). Ciliary signaling can activate intra-cellular pathways that control cellular homeostasis and repair (10). Primary cilia could therefore act as homeostatic sensors in TM cells, and fine-tuning of their signaling would be required to establish basal IOP levels. Primary cilia have been found in TM cells in humans and rodents, suggesting a conserved role across species (11).
Oculocerebrorenal syndrome of Lowe (Lowe syndrome) is a rare X-linked recessive disorder caused by a mutation in the OCRL1 gene, which encodes an inositol polyphosphate 5-phosphatase (12). In addition to brain and kidney defects, Lowe patients frequently develop elevated IOP and congenital glaucoma (13). Our previous work showed that OCRL is localized in the primary cilia of the human TM (HTM) (11) and that phosphatidylinositol 4,5-bisphosphate
[PI(4,5)P2] is increased in cells derived from patients with Lowe syndrome and in OCRL-deficient cells, suggesting that OCRL makes an important contribution to ciliary phosphoinositide regulation (11). Phosphoinositides regulate diverse cell processes, including actin cytoskeleton, cell migration, and ion transport across membranes. Thus, we hypothesized that subcellular activation of phosphoinositides would alter the rate of aqueous outflow and IOP.
To investigate whether regulation of phosphoinositide in the plasma membrane or primary cilium contributes to aqueous humor outflow, we modified an optogenetic protein recruitment system based on two plant proteins, cryptochrome 2 (CRY2) and the transcription factor CIBN. Initially described by Idevall-Hagren et al. (14), the OCRL domain (5-ptaseOCRL), which dephosphorylates the 5-position of the inositol ring of PI(4,5)P2 and PI(3,4,5)P3 (phosphatidylinositol 3,4,5-trisphosphate), is fused to the photolyase homology region domain of CRY2, while CIBN is fused to targeting signals for different cellular compartments. Here, we first show that blue light illumination of mammalian cells expressing optogenetic constructs has differential effects on actin cytoskeleton that depend on the targeting sequence for subcellular phosphoinositide redistribution. We then show that the optogenetic stimulation of 5-ptaseOCRL can increase aqueous outflow facility in mouse models of glaucoma.
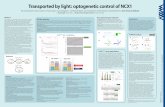
RESULTSLight-induced recruitment of CRY2–5-ptaseOCRL to plasma membrane and primary cilia in vitroTo determine whether subcompartmental distribution of OCRL affects aqueous outflow, we used and then modified a light-inducible system initially described by Idevall-Hagren et al. (14). To analyze the efficiency of this system in ocular hRPE (human retinal pigment epithelial) and HTM cells, we investigated the efficiency of CRY2- OCRL translocation to the plasma membrane. For this assay, the 5-ptase domain of OCRL fused to the optogenetic CRY2 is directed via light in a time/location-specific manner to its dimerizing partner CIBN, which is targeted to a subcellular compartment within the cell (Fig. 1A). We confirmed that hRPE and HTM cells expressed transfected red fluorescent mCherry (mCh–CRY2–5-ptaseOCRL) and a CIBN- EGFP (enhanced green fluorescent protein) fusion protein with a
1Department of Ophthalmology, Stanford University School of Medicine, 1651 Page Mill Road, Rm 2220, Palo Alto, CA 94305, USA. 2Duke Eye Center, Department of Ophthalmology, Duke University, Durham, NC 27710, USA. 3Palo Alto Veterans Administration, Palo Alto, CA 94304, USA.*Corresponding author. Email: [email protected]
Copyright © 2020 The Authors, some rights reserved; exclusive licensee American Association for the Advancement of Science. No claim to original U.S. Government Works. Distributed under a Creative Commons Attribution NonCommercial License 4.0 (CC BY-NC).
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
2 of 12
CAAX-box domain for plasma membrane targeting (CIBN-EGFP-CAAX). Before stimulation with blue light (dark condition), confocal microscopy revealed cytosolic accumulation of mCh–CRY2–5-ptaseOCRL. Expression of CIBN-EGFP-CAAX was enriched at the plasma membrane, with scattered cytosolic aggregates. Induction of CRY2-CIBN dimerization by blue excitation resulted in an accu-mulation of mCh–CRY2–5-ptaseOCRL at the plasma membrane in both hRPE and HTM cells (fig. S1A). The mCh–CRY2–5-ptaseOCRL intensity plot for the peripheral region of light-stimulated hRPE cells indicates that the response to blue light and recruitment to the plasma membrane were almost immediate and coincided with a moderate reduction in the cytosolic mCh–CRY2–5-ptaseOCRL.
The intensity plot shows a gradual reversal of mCh–CRY2–5-ptaseOCRL, with levels returning close to baseline after a 10-min in-cubation period in the dark (Fig. 1B).
On the basis of our previous work showing an abnormal increase of ciliary PI(4,5)P2 in Lowe patient cells (15), we decided to modify our optogenetic constructs to specifically target CRY2–5-ptaseOCRL to the primary cilium and study its functional role in modulating phosphoinositide levels. We replaced the CAAX-box in CIBN-EGFP- CAAX with the human rhodopsin ciliary targeting sequence (CTS) (indicated as VAPA). Another ciliary targeting construct was created by replacing the CAAX-box domain with the CTS found within the third intracellular loop of the G protein (heterotrimeric guanine
Fig. 1. Optogenetic modulation of OCRL in subcellular compartments. (A) Schematic model of optogenetic recruitment of mCh–CRY2–5-ptaseOCRL to the plasma membrane or primary cilium after blue light activation. Activation of blue light causes recruitment of cytosolic mCh–CRY2–5-ptaseOCRL to its dimerization partner EGFP-CIBN, which can be targeted to subcellular compartments. (B) Confocal images of the peripheral region of hRPE cells. Cells expressing the mCh–CRY2–5-ptaseOCRL and CIBN-EGFP-CAAX were analyzed via Z-stack to monitor mCh–CRY2–5-ptaseOCRL accumulation before and at intervals 10 min after illumination with 20 × 300–ms blue light pulses, and a respective mCh–CRY2–5-ptaseOCRL intensity data graph was plotted (N = 6). A.U., arbitrary units. (C) Representative images of CIBN-EGFP constructs with ciliary targeting domains. RPE cells were transfected with ciliary targeting constructs CIBN-EGFP-(VAPA/SSTR3) and then fixed and stained with a ciliary marker (ARL13b). (D) Representative images of optogenetic mCh–CRY2–5-ptaseOCRL recruitment to ciliary targeting CIBN constructs, VAPA and SSTR3, and nuclear targeting CIBN control (NLS). (E) Confocal images of HTM cells expressing the mCh–CRY2–5-ptaseOCRL and CIBN-EGFP-SSTR3. mCh–CRY2–5-ptaseOCRL accumulation in the ciliary area was measured before and at intervals 10 min after illumination with 20 × 300–ms blue light pulses, and a respective mCh–CRY2–5-ptaseOCRL intensity data graph was plotted (N = 6).
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
3 of 12
nucleotide–binding protein)–coupled receptor somatostatin recep-tor 3 (SSTR3) (16, 17).
We first verified the proper localization of these targeting sequences to the expected subcellular compartment. The CIBN-EGFP-VAPA or CIBN-EGFP-SSTR3 constructs were transfected into hRPE cells, followed by serum starvation to induce primary cilium formation. We found a distinct overlap of the EGFP fluorescent ciliary CIBN with the ciliary ARL13b marker (Fig. 1C). We next used these two new CTS-containing constructs in combination with mCh–CRY2–5-ptaseOCRL, followed by primary cilium induction by serum starva-tion. Positive CIBN-VAPA or CIBN-SSTR3 cilia had minimal levels of CRY2–5-ptaseOCRL accumulation in the dark condition. Follow-ing activation of CRY2-CIBN dimerization by a train of blue light pulses (detailed in Materials and Methods), a patchy increase of ciliary CRY2–5-ptaseOCRL was detected along the ciliary shaft. These patches varied in strength and location, suggesting that the movement of CRY2–5-ptaseOCRL was more limited inside the ciliary axoneme than in the cytosol (Fig. 1D). In addition, clearance was delayed, and in some instances, CRY2–5-ptaseOCRL accumulation persisted in these primary cilia after 10 min (Fig. 1E). This result suggests that natural transit or clearance of proteins from primary cilia could be considerably slowed at the transition zone.
As a control, we also designed a nuclear targeting CIBN to drive CRY2–5-ptaseOCRL away from the plasma membrane and ciliary membrane. A nuclear localization sequence (NLS) was designed to replace the CAAX-box (18, 19). With this approach, we showed that selective localization of CIBN to subcellular compartments resulted in successful targeted delivery of CRY2–5-ptaseOCRL (Fig. 1D). As expected, recruitment of the enzymatic activity of OCRL via light activation to its membrane target resulted in the local reduction of PI(4,5)P2 levels and conversion into phosphatidylinositol 4-phosphate (PI4P) (fig. S1B). We expected that these changes would not only cause local changes in cytoskeletal and actin organization but also likely affect different pathways involved in regulation of cellular homeostasis.
Viral transduction of CRY2–5-ptaseOCRL via membrane/ciliary-targeted CIBN-EGFP enhances aqueous outflow in vivoTo test whether targeting of CRY2–5-ptaseOCRL to different sub-cellular compartments produces functional changes in aqueous outflow, we used two different vehicles for delivery to the eye: lenti-virus and adeno-associated virus (AAV). Both optogenetic constructs (CIBN/CRY2) were generated in lentivirus and AAV (AAV2-s) and injected into the anterior chamber of the eye of wild-type (WT) C57BL/6J mice. Injection of the viral constructs diluted in Fast Green produced a distinct blue coloration of the injected eye, pro-viding additional visual confirmation of appropriate viral delivery. EGFP labeling demonstrated that both viral deliveries resulted in the expression of CIBN genes in the TM outflow track. Introducing our optogenetic constructs with the AAV2-s–based vector produced in vivo transduction of the TM cells and expression of CIBN/CRY2 in the TM outflow track after an incubation period of 3 to 4 weeks (Fig. 2A). After 4 weeks, one eye of each mouse received 10 min of blue light illumination with a 450-nm, 10-mW laser, while the other remained as a nonilluminated control, followed by eye pressure measurement by tonometer.
Subsequently, the eyes were enucleated and anterior chamber perfusion was performed to determine aqueous outflow (Fig. 2B). Aqueous outflow can be determined from the ratio of fluid inflow
over the corresponding eye pressure. This procedure is described in detail in Materials and Methods with a representative example from WT eyes (fig. S2I). When the IOP is plotted against its correspond-ing stable flow rate, the slope of the curve represents the efficiency of aqueous humor exit in the eye also known as outflow facility, which can be plotted as graphs.
Mice transduced with CRY2–5-ptaseOCRL and CIBN-EGFP-CAAX significantly increased outflow facility in blue light–illuminated eyes as compared to control eyes that did not receive light stimula-tion (Fig. 2C). To confirm that the effect on outflow facility was not caused by a secondary or viral effect that had been activated by blue light illumination, we performed blue light illumination and perfu-sion on animals injected with an AAV2-s–EGFP control vector and observed no differences with or without light stimulation (Fig. 2D). These results suggested that in vivo recruitment of CRY2–5-ptaseOCRL to the plasma membrane was sufficient to increase outflow facility.
We next studied the in vivo effect of directing optogenetic CRY2–5-ptaseOCRL to subcellular compartments within the cell. Subcellular targeting constructs for cilia and nuclei were cloned into AAV2-s vectors, and their transduction efficiency was tested in mice eyes. To test the effect of nuclear targeting of CRY2–5-ptaseOCRL, mice were injected with CRY2–5-ptaseOCRL and the nuclear target-ing AAV2-s. Outflow measurements at variable constant pressures were not significantly altered in eyes illuminated with blue light compared to nonilluminated controls. These results indicate that recruitment of CRY2–5-ptaseOCRL to areas of the cell distant from the cell membrane does not modulate outflow. The results further confirm that neither optogenetic illumination nor dimerization of CRY2-CIBN on its own affects the modulation observed with the membrane-targeting construct (Fig. 2E). To investigate the role of phosphoinositides within the primary cilia in modulating IOP through OCRL, we next packaged the previously designed ciliary targeting CIBN constructs into AAV2-s and lentivirus and injected them with CRY2–5-ptaseOCRL into the anterior chamber. Both light-activated ciliary targeting AAV2-s constructs significantly increased outflow facility compared to the nonilluminated controls (Fig. 2F and fig. S2D). Using a different viral delivery system (lenti-viral delivery) as a control produced similar results (fig. S2C), which supports that ciliary phosphoinositide regulation is critical in mod-ulating outflow facility. Tonometer readings performed on mice after blue light exposure showed a significant decrease in IOP in plasma membrane– or primary cilia–targeted CRY2–5-ptaseOCRL (Fig. 2, G and H, and fig. S2, C and D) compared to the nonilluminated controls, EGFP controls, and nuclear targeting constructs (fig. S2, G and H). A phosphatase dead mutant of OCRL had no effect on outflow facility or IOP (fig. S2, E and F). These results confirm that the effects on aqueous outflow regulation are due to the enzymatic spatial redistribution of functional OCRL to the cell boundaries, including the plasma membrane and primary cilia.
Phosphoinositide modulation influences calcium regulation and the cytoskeletal framework of TM cellsWe hypothesized that rearrangement of the actin cytoskeleton due to an increase in PI(4,5)P2 hydrolysis and conversion to PI4P could account for the reduction of IOP in light-stimulated eyes. Several groups have shown that actin regulation alters aqueous outflow (20). To determine the role of CRY2–5-ptaseOCRL in modulating the actin cytoskeleton, we cotransfected the actin marker LifeAct and the optogenetic constructs CRY2–5-ptaseOCRL and CIBN-EGFP-CAAX
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
4 of 12
Fig. 2. Outflow facility measurement of optogenetically treated mice. (A) Schematic design of optogenetic constructs CRY2–5-ptaseOCRL and CIBN-EGFP were pack-aged into AAV2-s or lentiviral vectors and injected at day 0 into the anterior chamber of C57BL/6J WT mice. Ocular injection was visualized by dilution in Fast Green blue dye. The anterior chamber was punctured with a 32-gauge needle horizontally, injected with air to create a small air bubble, and infused with 2 l of virus (>1010 plaque-forming units). Days 1 to 28: Viral expression of optogenetic constructs with lentivirus or AAV2-s was allowed for a period of 4 weeks, at which time positive cell transduction in the mouse anterior segment, including the TM, was achieved. The vehicle control expressed no fluorescence. (B) Schematic design of in vivo optogenetic activation. The right eye of each animal was exposed to 10-mW blue light (450-nm laser) for 10 min followed by outflow facility measurement. (C) Perfusion plots of mouse eye injected with AAV2-s–CIBN–EGFP–CAAX and CRY2–5-ptaseOCRL with and without blue light exposure. Eyes with illumination demonstrate higher outflow facility than those without exposure, as represented by a significant difference between slopes (N = 10 eyes). (D) No significant difference was observed in AAV2-s–CIBN–EGFP control (N = 10 eyes) or (E) AAV2-s–CIBN–NLS nuclear targeting constructs (N = 8 eyes). (F) Outflow facility measurement of eyes injected with ciliary targeting CIBN via AAV2-s intraocular delivery shows a significant increase in outflow facility (N = 9 eyes). (G) Membrane targeting: Decrease in IOP compared to nonilluminated control eyes (H). Ciliary targeting: Decrease in IOP compared to nonilluminated control eyes. Statistical analysis: Paired sample t test, where P < 0.05 was considered statistically significant. Error bars represent SEM. (I) Representative eye pressure tracing of light-stimulated WT mice eye treated with AAV2-s–CIBN and CRY2–5-ptaseOCRL.
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
5 of 12
in hRPE and HTM cells. After light stimulation, actin stress fibers gradually diminished, which coincided with a significant decrease in cell size. These results suggest that PI(4,5)P2 breakdown at the membrane influences cytoskeletal organization and cell plasticity. Cell contraction was more prominent in HTM cells than in hRPE cells (Fig. 3A). The same light activation protocol did not affect the size of cells that had not been transfected with CIBN-CAAX or that were transfected with phosphatase dead mutant of OCRL (D523G). Similarly, transfection of control nuclear targeting construct CIBN-EGFP-NLS in combination with LifeAct and CRY2–5-ptaseOCRL did not affect cytoskeleton organization or cell size (fig. S3A). The ciliary targeting construct produced a moderate, but not significant, change in cell size in HTM after the first 10 min (Fig. 3A).
We next studied the effect of optogenetic regulation on cell con-traction with a collagen-based cell contraction assay using HTM cells. HTM cells treated with the contraction-inducing 3-butanedione monoxime as a positive control demonstrated significant contraction. In HTM cells transfected with membrane-localizing CRY2–5-
ptaseOCRL, a significant contraction already occurred by 10 min after blue light illumination (Fig. 3B). Analysis of the ciliary localizing OCRL revealed that although only a moderate contraction was measured initially, contraction became significant during a longer incubation period. It is possible that the cytoskeletal effect of OCRL in primary cilia might be additionally regulated and enhanced by flow in vivo, thus explaining the delayed or reduced effect in vitro. Cell contraction is known to be mediated through intracellular calcium. Because previous studies have shown that OCRL binds to the ciliary transient receptor potential vanilloid 4 (TRPV4) calcium channel, possibly modulating its activity (11), we next tested if modulation of intracellular calcium could affect contraction. We found that, in HTM cells, intracellular calcium induced by TRPV4 agonist (GSK1016790A) or thapsigargin (an inhibitor of the endo-plasmic reticulum calcium adenosine triphosphatase) produced different degrees of cell contraction (fig. S3, B and C). To determine whether the contraction affected by CRY2–5-ptaseOCRL localization was calcium dependent, BAPTA AM was used as a cell-permeant
Fig. 3. Phosphoinositide modulation influences calcium regulation and the actin cytoskeleton of TM cells. (A) Representative image of LifeAct actin and CRY2–5-ptaseOCRL distribution in hRPE and HTM cells. After expression of the CIBN and CRY2–5-ptaseOCRL constructs, the cells were stimulated with a train of pulses of 488-nm light and the cytoskeletal reorganization was measured. Cell outline was indicated before and 10 to 20 min after CRY2–5-ptaseOCRL recruitment. A significant decrease in cell size parallel to contraction of the internal actin arrangement was detected in plasma membrane–targeted CRY2–5-ptaseOCRL. (B) Cell contraction assay of CRY2–5-ptaseOCRL and CIBN-SSTR3/CAAX–transfected HTM cells after blue light illumination. (C) LifeAct actin CRY2–5-ptaseOCRL and CIBN-CAAX–transfected cells pretreated with BAPTA AM before and after blue light optogenetic activation. Representative image and quantification are shown. (D) Fluorescence intensity graph of BAPTA AM after blue light optogenetic activation. (E) CRY2–5-ptaseOCRL recruitment to plasma membrane, followed by 10-min incubation and phalloidin staining in 4% paraformalde-hyde fixation. Recruitment to plasma membrane was associated with increased actin stress fiber fragmentation compared with non–light-activated control. Statistical analysis for cell size change (N = 6), where six treated cell sizes were compared with untreated cell sizes that are normalized to 1, unpaired t test, where P < 0.05 was considered statistically significant. Error bars represent SEM (*P ≤ 0.05 and **P ≤ 0.01).
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
6 of 12
calcium chelator. We found that pretreatment with BAPTA AM followed by optogenetic recruitment of OCRL to the plasma mem-brane prevented the cell contraction observed previously (Fig. 3C). Intracellular BAPTA AM increased in fluorescence upon binding and chelating calcium, and we recorded a significant increase in BAPTA AM fluorescence shortly after optogenetic CRY2–5-ptaseOCRL re-cruitment to the plasma membrane, suggesting that light-induced recruitment increased intracellular calcium (Fig. 3D). Perfusion analysis of mice eyes injected with either TRPV4 agonists or antagonists showed a differential effect on outflow facility, further support-ing the role of calcium in regulating TM contraction/outflow facility (fig. S3D). Calcium was postulated to contribute to cyto-skeletal actin organization decades ago (21). To examine in detail the cytoskeletal changes, we compared the actin cytoskeleton in nonactivated and light-activated CRY2–5-ptaseOCRL and CIBN-EGFP-CAAX–transfected cells. Optogenetic CRY2–5-ptaseOCRL recruited to the plasma membrane significantly decreased and fragmented linear actin stress fibers (Fig. 3E). Therefore, we conclude that the IOP and outflow facility change resulted from calcium- dependent actin cytoskeletal reorganization.
OCRL modulation of a Lowe syndrome mouse modelPrevious analyses of the oculocerebrorenal syndrome of Lowe showed that OCRL was critical in its pathogenesis, but no detailed studies in mouse eye are available. Recent technical advances now allow eye pressure and aqueous outflow measurement in the mouse (22). Bothwell et al. (23) showed that mice deficient only in Ocrl (Ocrl−/−) exhibited few, if any, abnormalities, while those lacking both Ocrl and Inpp5b (Ocrl−/−:Inpp5b−/−) died on embryonic day 9.5. INPP5B, a paralog of OCRL, is another inositol 5-phosphatase. Introduction of the human INPP5B to double-knockout mice (Ocrl−/− Inpp5b−/− INPP5B+/+, hereafter referred to as the IOB mouse), however, induced renal abnormalities seen in Lowe syndrome. This result prompted us to examine the ocular phenotype of IOB mice; we found it to be simi-lar to the ocular pathology in human Lowe syndrome. Dilated fundoscopic examination showed retinal thinning in vessel images of both the right (OD) and left (OS) eyes of IOB mice (Fig. 4A), which is also similar to the phenotype in humans (Fig. 4B). In addition, flat mounts and cross sections of retinas from both strains consistently showed a marked reduction of the number of ganglion cells in IOB mice (Fig. 4, C and D).
We next examined the eye for defects in aqueous outflow, which underlie glaucoma development. Examination of the average outflow facility of perfused eyes revealed that the outflow rate was decreased at different IOP levels in IOB mice than in IOB+/Y control mice (Fig. 4E). Measurement of eye pressure with a re-bound tonometer confirmed an abnormally elevated pressure in IOB mice compared to IOB+/Y (control) (Fig. 4F). We conclude that a defect in aqueous outflow may underlie the glaucomatous phenotype observed in IOB mice. Together, these data show that the IOB mouse expresses ocular defects and decreased aqueous outflow facility, similar to those of patients with Lowe syndrome. These defects may be directly linked to the known modulatory role of OCRL on phosphoinositides and actin cytoskeleton regulation (fig. S4) (24, 25). These findings led us to propose that abnormal regulation of phosphoinositides in the eye can result in aqueous outflow defects.
We have shown that optogenetic recruitment of CRY2–5-ptaseOCRL to the plasma membrane or primary cilia could modulate outflow
facility. To determine whether CRY2–5-ptaseOCRL recruitment has the same beneficial effect in pathological conditions, we tested plasma membrane and ciliary optogenetic recruitment in the IOB Lowe syndrome mouse model. IOB mice were injected with AAV2-s–CRY2–5-ptaseOCRL and AAV2-s CIBN-EGFP-CAAX or AAV2-s CIBN-EGFP-SSTR3, and after an incubation period of 4 weeks, opto-genetic translocation was induced with blue light as previously de-scribed. Tonometer readings showed a significant decrease of IOP in the optogenetically stimulated eye compared to the nonstimulated eye with both the membrane and ciliary targeting constructs. Outflow perfusion analysis of the respective enucleated eyes corroborated the IOP data (Fig. 4, G and H), suggesting that IOP decreased with both optogenetically activated constructs due to a local increase of aqueous outflow through the TM.
PI(4,5)P2 and primary cilia play a critical role in outflow facility regulationTo determine whether 5-phosphatase enzymatic activity is required for outflow regulation, we blocked OCRL activity by injecting a selective inhibitor against OCRL1 (YU142670) into the anterior chamber of the eye. After an incubation period of 30 min, we per-formed a perfusion analysis of the treated and untreated control eyes, which showed that pharmacological inhibition markedly re-duced outflow facility (Fig. 5A). OCRL deficiency has previously been associated with an abnormal increase in intracellular PI(4,5)P2 levels. PI(4,5)P2 is a known regulator of actin polymerization. To further confirm that the reduction in outflow facility by OCRL was primarily due to abnormal accumulation of PI(4,5)P2 rather than to changes in other metabolites such as PI4P or PI(3,4,5)P3, we applied two additional pharmacological PI(4,5)P2 regulators that control conversion of PI(4,5)P2 to PI(3,4,5)P3 (Fig. 5B). Perfusion analysis revealed that phosphatidylinositol 3-kinase (PI3K) inhibition sig-nificantly reduced outflow facility, whereas PI3K activation caused a moderate increase (Fig. 5C). Although these results do not ex-clude that upstream or downstream alterations of PI4P or PI(3,4,5)P3 might also influence outflow facility, they show that different enzymatic manipulations that decrease PI(4,5)P2 levels are suffi-cient to exert a positive influence on outflow facility and IOP (Fig. 5, C and D).
To investigate whether the OCRL-dependent PI(4,5)P2 reg-ulation in primary cilia or plasma membrane plays a mutual or in-dependent role in modulating outflow facility, we next performed perfusion analysis on IFT88fl/fl mice that had received a lentiviral CRE injection to the anterior chamber to abolish the ability of TM cells to form primary cilia (Fig. 5E and fig. S5). We measured no difference in outflow facility between IFT88fl/fl mice injected only with CRE and IFT88fl/fl mice coinjected with CRE and either AAV2-s–CRY2–OCRL + AAV2-s–CIBN–CAAX or SSTR3 but without light stimulation. Upon light activation, injection of only the plasma membrane–targeting AAV2-s significantly increased outflow facility, whereas injection of the ciliary targeting AAV2-s had no effect (Fig. 5F). These results show that the effect of CRY2–5-ptaseOCRL on the plasma membrane is independent of primary cilia, while in a cilia-ablated model CRY2–5-ptaseOCRL is unable to exert or initiate its positive effect on outflow facility. Analysis of IOP supports this conclusion (fig. S5B). Using an optogenetic model, we show that functional primary cilia play a pivotal role in phosphoinositol regulation and adaptive modulation of IOP in a healthy eye.
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
7 of 12
DISCUSSIONPhosphoinositide signaling has been implicated in a wide range of biological processes. In this study, we provide evidence for a new role of phosphoinositides in the regulation of eye pressure. We used in vivo optogenetic stimulation of the CRY2-CIBN interaction to show that subcellular targeting of inositol phosphatase OCRL in the mouse eye can differentially regulate aqueous outflow and IOP. We also present evidence that the underlying mechanism is based on calcium-dependent actin cytoskeletal rearrangement and primary cilia regulation in TM cells, which cause cellular contraction, in-creased aqueous drainage, and lowered IOP (Fig. 5G). This report is the first to use optogenetics to study eye pressure. Direct exposure
to blue light at 450-nm wavelength penetrates and illuminates the eye, which activates the dimerization of CRY2-CIBN in vivo. Previous studies of outflow facility relied primarily on either pharmacological or genetic manipulations (knockdown and overexpression) in animals. Use of the CIBN/CRY2 system enabled us to demonstrate a direct effect of enzyme activation (OCRL) on outflow in vivo.
The important breakthrough of this study is the discovery that phosphoinositides in TM cells can regulate eye pressure. The main enzymatic activity of the 5-phosphatase domain of OCRL (CRY2–5-ptaseOCRL) is directed toward PI(4,5)P2 (26). OCRL and INPP5B are the only phosphatase variants currently known to be involved in the dephosphorylation of PI(4,5)P2 to PI4P at the apical surface
Fig. 4. OCRL modulation of a Lowe syndrome mouse model. (A) Left: Retinal imaging and optical coherence tomography of right (OD) and left (OS) eyes of IOB mouse. Right: Vessel imaging of an IOB mouse with severe cataracts. (B) Optic nerve images of human patients with Lowe syndrome and glaucomatous optic nerve cupping. (C) Flat mount and (D) cross sections of normal and IOB mice retinas, which were stained with an RGC marker, RBPMS, and hematoxylin and eosin stain, respectively. A marked decrease in the RGCs layer and number of RGCs is detected in 4-month-old IOB mice compared to the same age WT control. IPL, inner plexiform layer; INL, inner nuclear layer; OPL, outer plexiform layer; ONL, outer nuclear layer. (E) Average outflow facility of perfused eyes in IOB−/− mice (N = 14) or IOB+/Y mice (control, N = 12) and comparison performed with unpaired t test. (F) IOP measurements using TonoLab tonometer. IOP measurements of IOB−/− mice (N = 10) versus IOB+/Y (control) mice (N = 8) are obtained, and comparison was performed with unpaired t test. (G) Perfusion plots of IOB model eyes injected with AAV2-s–CIBN–CAAX and mCh–CRY2–5-ptaseOCRL with and without blue light exposure. Eyes with illumination demonstrate a higher outflow facility and lower IOP than those without exposure, as represented by a significant difference between slopes (N = 4, comparison between left and right eye). Statistical analysis was performed using paired sample t test. (H) Perfusion plots of IOB model eyes injected with AAV2-s–CIBN–SSTR3 and mCh–CRY2–5-ptaseOCRL with and without blue light exposure. Eyes with illumination demonstrate a higher outflow facility and lower IOP than those without exposure, as represented by a significant difference between slopes (N = 4, comparison between left and right eye). Statistical analysis was performed by paired sample t test, where P < 0.05 was considered statistically significant. Error bars represent SEM (*P ≤ 0.05 and **P ≤ 0.01).
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
8 of 12
Fig. 5. Phosphoinositides and primary cilia regulate aqueous outflow facility. (A) Anterior chambers of WT mice eyes were injected with 100 M (YU142670) OCRL inhibitor, and perfusion analysis was performed after 30-min incubation. Perfusion analysis of related, untreated control mice was performed under the same conditions, and outflow comparison is shown as a whisker plot of outflow facility C for YU142670. (B) Schematic representation of drug targets. (C) Perfusion plots of eye anterior chamber injected with 1 l of 10 M PI3K inhibitor (GSK1059615) or 50 M PI3K activator (740-Y-P) per eye. (D) Eye pressure tonometer analysis of GSK1059615- and 740-Y-P–treated mice after 2-hour incubation. (E) Analysis of IFT88fl/fl mice intraocularly injected with CRE lentivirus for primary cilia removal in combination with AAV2-s–CRY2–OCRL + AAV2-s–CIBN–CAAX/SSTR3. (F) Relevant whisker plot of outflow facility C for optogenetically treated IFT88fl/fl/CRE eyes (blue dots, light activated) (N = 4 eyes). Statistical analysis was performed by independent samples t test and paired t test, where P < 0.05 was considered statistically significant. Error bars represent SEM. (G) Schematic representation of 5-ptaseOCRL–dependent optogenetic modulation of IOP in the TM of mouse eye. (*P ≤ 0.05 and **P ≤ 0.01).
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
9 of 12
(23, 27, 28). The role of various channels and receptor subtypes that might be affected by lipid-regulated cross-talk is unknown (29, 30). The available data support the specific role of OCRL in degrading PI(4,5)P2 and PI(3,4,5)P3, which causes cytoskeletal changes that affect outflow facility and lower IOP. Cell morphology alterations and cell contraction are primarily driven by the actin cytoskeleton, and we show that inositol 5-phosphatase recruitment to the plasma membrane can reorganize the cytoskeleton. This finding is consistent with previous studies showing that the TM has smooth muscle–like properties and a variety of smooth muscle receptors and channels that regulate actin and are important in contractility (31, 32, 33). Moreover, it has been shown that TM cells in bovine eyes could be induced pharmacologically to contract to an extent to reduce outflow and that this contraction was associated with a rise of intracellular calcium (31).
We show that calcium regulation induces TM contraction to a similar extent as optogenetic CRY2–5-ptaseOCRL recruitment, sug-gesting that OCRL-induced contraction might be mediated through intracellular calcium regulation. In support of this notion, previous studies in our laboratory showed a functional interaction between OCRL and TRPV4 calcium channel, suggesting that OCRL could directly modulate its function (11). Therefore, regulation of ciliary or plasma membrane phosphoinositides could be a critical influence on various calcium channel activities. We show that blocking the intracellular calcium pathway can prevent cell contraction caused by light-stimulated CRY2–5-ptaseOCRL, which provides strong evidence that CRY2–5-ptaseOCRL–derived cell contraction is calcium dependent.
Notably, our data support earlier reports that modulation of spe-cific pools of intracellular PI(4,5)P2, involved in regulating actin can influence cytoskeletal reorganization, which, inversely, is a known regulator of ciliogenesis (24). Previous studies have shown that a range of different OCRL1 knockdown cell types are characterized by a decreased ability to assemble primary cilia and a reduction in the overall length of their cilia (34), suggesting that OCRL deficiency might impede normal primary cilia formation and function through defective actin organization.
The results from this study support a model in which abnormal accumulation of PI(4,5)P2 in different areas of OCRL-deficient cells causes local actin disorganization and therefore breakdown of normal cellular function, including primary cilium regulation and cell plasticity. Our data suggest that PI(4,5)P2 levels must be tightly regulated in two critical areas to positively influence IOP: the plasma membrane and the primary cilium. Both sites are likely to converge in a common intersecting pathway that regulates the derived cytoskeleton organi-zation and actin buildup, which provides resistance to further deformation by outside pressure. The importance that our findings attribute to cilia is consistent with the clear linkages established be-tween 5-ptases, such as INPP5E and OCRL1, and different types of ciliopathies, including Joubert/MORM (mental retardation, truncal obesity, retinal dystrophy and micropenis) syndromes and Lowe syndrome. We show that the presence of functional primary cilia is important for the normal functioning of the TM and that phos-phoinositides play a critical role in synthesizing different mecha-nisms involved in the regulation of aqueous outflow.
MATERIALS AND METHODSReagentsAnti-ARL13b mouse antibody was purchased from University California Davis/National Institutes of Health (NIH) NeuroMab
Facility (Davis, CA). Alexa Fluor 488 and Alexa Fluor 594 goat anti- mouse immunoglobulin G secondary antibodies were obtained from Life Technologies. Alexa Fluor 568 Phalloidin and ProLong Gold Antifade Mountant with DAPI (4′,6-diamidino-2-phenylindole) were purchased from Invitrogen. The OCRL inhibitor YU142670 (custom made) and the ROCK inhibitor Y-27632 dihydrochloride were from Tocris. Anti- RBPMS (RNA-binding protein with multiple splicing) guinea pig (1832-RBPMS), anti-PI4P (Z-P004), and PI(4,5)P2 (Z-P045) antibodies were obtained from PhosphoSolutions (Aurora, CO) and Echelon (Salt Lake City, UT). Latrunculin B, Oregon Green 488, BAPTA-1, AM (A1076), and thapsigargin (T9033) were obtained from Sigma- Aldrich. Anti-fibronectin was purchased from Abcam (ab2413). GSK1059615 [3.33 mg/ml in dimethyl sulfoxide (DMSO)], 740-Y-P (1 mg/ml in water), GSK1016790A (10 mg/ml in DMSO), and HC 067047 TRPV4 agonist (10 mg/ml in DMSO) were purchased from Tocris.
AnimalsAll animal experiments followed the guidelines of the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research and were approved by the Institutional Animal Care and Use Committee of Stanford Uni-versity School of Medicine. WT (C57BL/6) mice were purchased from The Jackson Laboratory. Ocrl−/− Inpp5b−/− INPP5B+/+ mice were a gift from R. L. Nussbaum (University of California, San Francisco). IFT88fl/fl mice (B6.129P2-Ift88tm1Bky/J) were obtained from The Jackson Laboratory. Animals were housed under a 12-hour light/12-hour dark cycle with free access to water and food. For viral injections, mice were anesthetized with ketamine based on their body weight [ketamine (100 mg/kg)]. For blue light exposure and tonometer readings, mice were anesthetized using isoflurane. Oxygen flow was set to 2 liters/min and isoflurane at 1% under a nose cone. All mice studied were within the same age range to avoid age-related variability.
Cell cultureControl human fibroblast cultures (NHF558), human hRPE cell cultures, and Lowe 1676 fibroblast cell lines were previously described (35). HTM cells were obtained from cadaveric corneas (Indiana Lions Eye Bank), and characterization and culturing protocols were based on previous reports (36, 37). In experiments requiring ciliogenesis, specific culture conditions were applied to ensure primary cilia formation (10).
DNA plasmid and transfectionCIBN-EGFP-CAAX and mCh-CRY2-OCRL were gifts from P. de Camilli (Yale University). mRhodopsin CTS (312KQFRNCMLTTL- CCGKNPLGDDDASATASKTETSQVAPA348) was cloned to generate CIBN-VAPA-EGFP. SSTR3 CTS from pEGFPN3-Sstr3 (16) was cloned to generate CIBN-EGFP-SSTR3. SV40 NLS (124PPKKKRKVA133) was cloned to generate CIBN-EGFP-NLS. Optogenetic constructs were either directly transfected using Lipofectamine 3000 (Invitrogen) or polyethylenimine (Sigma) or subcloned separately into Flag- and Myc-tagged lentiviral constructs, and AAV2-s tdTomato–LifeAct-7 and LV-Cre were from Addgene.
ImmunofluorescenceSlides of cells in culture were treated with 488-nm blue laser for 10 min before 4% paraformaldehyde fixation for 10 min at room temperature, followed by permeabilization with 0.5% Triton X-100.
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
10 of 12
Samples were then blocked with phosphate-buffered saline (PBS)/0.5% bovine serum albumin (BSA)/10% normal goat serum for 30 min at room temperature. Primary antibodies were applied at 4°C overnight, followed by secondary antibodies at room temperature for 1 hour.
Confocal microscopy and live-cell imagingImaging was performed with a Zeiss LSM880 confocal microscope and a Zeiss Axio Observer 5 inverted microscope. Z-stack pictures were performed with confocal microscope; a single 488-nm (for CIBN- EGFP) channel pulse activation was followed by time series Z-stack scanning of 568 nm (for the mCh-CRY) channel for at least 10 min. Intensity of mCh-CRY2-OCRL in various experiments was quanti-fied with ImageJ (v1.47v, NIH). Area and total fluorescence intensity were measured in a selected region around the area of interest.
Intraocular injectionIntraocular injections were performed according to Wang et al. (38). Briefly, AAV2-s or lentivirus with optogenetic constructs was injected into the anterior chamber of the eye of C57BL/6 mice anesthetized with ketamine (100 mg/kg) in ddH2O. In addition, one drop of 0.5% proparacaine hydrochloride (Bausch & Lomb, Tampa, FL) was applied to each eye as a local anesthetic. The cornea was punctured with a sterile 33-gauge needle (STERiJECT) under observation through a dissection microscope (Nikon) to create a small aperture to the anterior chamber. The needle was removed, and a fine borosilicate glass capillary (World Precision Instruments, 1B150-4) connected to a Hamilton syringe by polyethylene tubing was passed through the same hole to introduce a small air bubble. The capillary was slowly removed and filled with 2 l of viral constructs (1010 infectious units/l) diluted in Fast Green blue dye to facilitate and monitor the injection through the same puncture site. After introduction of the diluted virus, the anterior chamber was filled with a distinct blue tint, and the glass capillary was left in position for an additional minute to monitor the pattern of the staining. The air bubble was then gently moved to the insertion site to seal off the puncture and prevent leaking of vector. After the procedure, neomycin was applied to each eye to prevent infection.
Measurement of IOPIOP was measured with the TonoLab tonometer TV02; mice received topical anesthesia. The device recorded six valid rebound measure-ments from the eye; the mean of the middle five readings was used as one summary measurement.
Mouse eye perfusion apparatusThe mouse eye perfusion apparatus was designed according to pre-vious research (22, 39). As shown in the schematic representation (fig. S2I), a 5-mm-long 33-gauge needle (TSK Laboratory, Japan) attached to a micromanipulator was introduced into the anterior chamber through the cornea under microscopic guidance, avoiding damage to the iris and lens. The needle was connected to a rigid, noncompliant, Lectro-Cath tube attached to a three-way stopcock, which was connected on one hub to an MLT1199-BP transducer (AD Instruments, CO) and on a second hub to a calibrated glass Hamilton syringe driven by a New Era syringe pump (Syringe Pump, NY). The MLT1199-BP transducer was connected to an amplifier by the Transducer Cable Kit (AD Instruments, CO). The pump (flow range of 0.001 l/hour to 2120 ml/hour) was controlled
by customized pumping software programmed to integrate with LabChart 8 software (AD Instruments, CO) in a computer connected to the Amplifier/PowerLab system (AD Instruments, CO). Modified software controlled the pumping flow rate to maintain stabilized pressure settings. The perfusion apparatus was filled with sterile Dulbecco’s PBS and calibrated before each experiment. Pressure was zero-referenced before cannulation. The pressure in the anterior chamber was transduced to the pressure transducer after cannulation. High-speed flow rate was used to reach a desired pressure in the anterior chamber; low-speed flow rate was controlled by the syringe pump and automatically adjusted according to the feedback between LabChart and pumping software. Outflow from the anterior cham-ber was determined and recorded according to the low-speed flow rate when each pressure had achieved a stable constant number. Each eye was pumped at a constant pressure (Y value) from 10 to 35 mmHg and corresponding flow rate (X value) to maintain this constant IOP reading and allowed to stabilize over 10 min at each pressure value. Representative perfusion tracings show flow rate (left y axis in red) and IOP (right y axis in black) for WT mouse eye as a function of time. Each flattened tracing of flow rate and pres-sure was marked as the constant outflow rate under different IOPs. X1 and Y1 indicate a paired perfusion pressure and its correspond-ing IOP (10, 15, 20, 25 mmHg). The IOP was then plotted against its corresponding stable flow rate, where slope indicates conventional outflow facility and the y intercept indicates the uveoscleral outflow independent of IOP. Average outflow facility of perfused eyes with flow rate (ml/min) on the y axis plotted against IOP (in mmHg) on the x axis represents the perfusion plot of IOP versus flow rate (fig. S2, A and B). Before measurement with this system, mice were anesthetized and sacrificed by cervical dislocation. Eyeballs were enucleated within 10 min of death and perfused immediately with the perfusion apparatus. We perfused eyes over 60 min at increments of IOP. To determine the outflow facility of each sample, we drew the dependent relationship of IOP and conventional outflow facility rate (C) using the modified Goldmann equation: f = C × IOP + U. In this equation, f is the low-speed flow rate at each corresponding stable IOP and U is the unconventional outflow. The conventional outflow rate C of each sample was determined as the slope of the equation plotted using multiple recorded pumping flow rates and the corre-sponding IOPs in GraphPad Prism.
AAV vector construction and productionAAV2 were capsid-mutated according to Bogner et al. (40) (referred here as AAV2-s). AAV2-s viral particles were prepared by the triple plasmid transfection method following the protocol of Wang et al. (38). Briefly, AAV cis, AAV trans, and adenovirus helper plasmid (2:1:1 ratio) were transfected using PolyJet In Vitro DNA Transfection Reagent in human embryonic kidney (HEK) 293 cells. Viral purifi-cation was performed by protocols from Lock et al. (41). Viral particles were subsequently resuspended in PBS. AAV2-s was titrated by TaqMan quantitative polymerase chain reaction amplification using primers and probes detecting the promoter, and transgene of the transgene cassette with deoxyribonuclease I–resistant vector genome copies as reference. Viral preparation purity was evaluated by SDS–polyacrylamide gel electrophoresis gel electrophoresis.
Lentivirus construction and productionHEK293TT cells were cultured and transfected to generate lentivirus of CIBN-EGFP and mCh-CRY2-OCRL or CRE according to adapted
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
11 of 12
protocols from Protocol Exchange (42) Briefly, reverse transfection was used for the generation of lentiviral particles. The transfection is done in suspended 293T cells using 20 g of lentiviral vector, 10 g of pVSV-G, 20 g of pCMV-dR8.91, and 100 l of PolyJet (SignaGen) or Lipofectamine 2000 (Life Technologies) in 10-cm dishes. The plasmid/transfection reagent complex and the 293T cell suspension were mixed in 50-ml centrifuge tubes and incubated for 30 min on a shaker. The suspension was then applied to the 10-cm dishes. After an incubation period of 72 hours, the virus was harvested and Lenti-X (Clontech) concentrator was used to concentrate virus into the desired small volume. Concentrated virus (500 to 2000 l) was used to infect 1 × 106 cells in 500 l of culture medium in the presence of polybrene (4 g/ml; Sigma-Aldrich), followed by gentle pipetting 25 times and shaking for 10 min in the hood.
Collagen-based cell contraction assayHTM cell contraction after optogenetic stimulation was performed using the Collagen-based Cell Contraction Assay from Cell Biolabs, and experiments were set up according to the manufacturer’s specifi-cation. Briefly, HTM cells were transfected with optogenetic con-structs, and after overnight incubation, cells were resuspended and diluted in medium at 2 × 106 to 5 × 106 cells/ml. The cell suspension was then mixed with the cell-collagen mixture and seeded in 24-well plates. After incubation at 1 hour at 37°C to allow collagen poly-merization, 1.0 ml of culture medium was added to each well and incubated for 24 hours following optogenetic stimulation and mea-surement of contraction.
Statistical analysisAll statistical analysis was performed using GraphPad8 (Prism) software. Results are expressed as mean values ± SEM. Statistical analysis was performed using linear regression analysis for outflow facility measurement and unpaired t test to compare the means of two independent groups, such as outflow facility and IOP between control versus treated and disease mice in vivo or cell cultures transfected and treated with different compounds in vitro.
Paired t test was used for comparison of blue light–illuminated versus nonilluminated eyes of each mouse transduced with opto-genetic viruses as indicated. P < 0.05 was considered statistically significant. Distinct and clear statistical results were commonly abbreviated with stars (*P ≤ 0.05, **P ≤ 0.01, and ***P ≤ 0.001). To highlight statistical changes outside the normal range, P values were spelled out in some cases.
SUPPLEMENTARY MATERIALSSupplementary material for this article is available at http://advances.sciencemag.org/cgi/content/full/6/18/eaay8699/DC1
View/request a protocol for this paper from Bio-protocol.
REFERENCES AND NOTES 1. H. A. Quigley, Open-angle glaucoma. N. Engl. J. Med. 328, 1097–1106 (1993). 2. W. D. Stamer, T. S. Acott, Current understanding of conventional outflow dysfunction
in glaucoma. Curr. Opin. Ophthalmol. 23, 135–143 (2012). 3. M. Montecchi-Palmer, J. Y. Bermudez, H. C. Webber, G. C. Patel, A. F. Clark, W. Mao, TGF2
induces the formation of cross-linked actin networks (CLANs) in human trabecular meshwork cells through the smad and non-smad dependent pathways. Investig. Ophthalmol. Vis. Sci. 58, 1288–1295 (2017).
4. C. Luna, G. Li, J. Huang, J. Qiu, J. Wu, F. Yuan, D. L. Epstein, P. Gonzalez, Regulation of trabecular meshwork cell contraction and intraocular pressure by miR-200c. PLOS ONE 7, e51688 (2012).
5. T. Carreon, E. van der Merwe, R. L. Fellman, M. Johnstone, S. K. Bhattacharya, Aqueous outflow - A continuum from trabecular meshwork to episcleral veins. Prog. Retin. Eye Res. 57, 108–133 (2017).
6. D. WuDunn, Mechanobiology of trabecular meshwork cells. Exp. Eye Res. 88, 718–723 (2009).
7. R. F. Ramos, G. M. Sumida, W. D. Stamer, Cyclic mechanical stress and trabecular meshwork cell contractility. Investig. Ophthalmol. Vis. Sci. 50, 3826–3832 (2009).
8. N. F. Berbari, A. K. O’Connor, C. J. Haycraft, B. K. Yoder, The primary cilium as a complex signaling center. Curr. Biol. 19, R526–R535 (2009).
9. D. A. Hoey, S. Tormey, S. Ramcharan, F. J. O’Brien, C. R. Jacobs, Primary cilia-mediated mechanotransduction in human mesenchymal stem cells. Stem Cells 30, 2561–2570 (2012).
10. O. V. Plotnikova, E. N. Pugacheva, E. A. Golemis, Primary Cilia and the Cell Cycle. Methods Cell Biol. 94, 137–160 (2009).
11. N. Luo, M. D. Conwell, X. Chen, C. I. Kettenhofen, C. J. Westlake, L. B. Cantor, C. D. Wells, R. N. Weinreb, T. W. Corson, D. F. Spandau, K. M. Joos, C. Iomini, A. G. Obukhov, Y. Sun, Primary cilia signaling mediates intraocular pressure sensation. Proc. Natl. Acad. Sci. U.S.A. 111, 12871–12876 (2014).
12. O. Attree, I. M. Olivos, I. Okabe, L. C. Bailey, D. L. Nelson, R. A. Lewis, R. R. Mclnnes, R. L. Nussbaum, The Lowe’s oculocerebrorenal syndrome gene encodes a protein highly homologous to inositol polyphosphate-5-phosphatase. Nature 358, 239–242 (1992).
13. A. Bökenkamp, M. Ludwig, The oculocerebrorenal syndrome of Lowe: An update. Pediatr. Nephrol. 31, 2201–2212 (2016).
14. O. Idevall-Hagren, E. J. Dickson, B. Hille, D. K. Toomre, P. De Camilli, Optogenetic control of phosphoinositide metabolism. Proc. Natl. Acad. Sci. U.S.A. 109, E2316–E2323 (2012).
15. P. P. Prosseda, N. Luo, B. Wang, J. A. Alvarado, Y. Hu, Y. Sun, Loss of OCRL increases ciliary PI(4,5)P2 in Lowe oculocerebrorenal syndrome. J. Cell Sci. 130, 3447–3454 (2017).
16. N. F. Berbari, A. D. Johnson, J. S. Lewis, C. C. Askwith, K. Mykytyn, Identification of ciliary localization sequences within the third intracellular loop of G protein-coupled receptors. Mol. Biol. Cell 19, 1540–1547 (2008).
17. M. V. Nachury, E. S. Seeley, H. Jin, Trafficking to the ciliary membrane: How to get across the periciliary diffusion barrier? Annu. Rev. Cell Dev. Biol. 26, 59–87 (2010).
18. N. Freitas, C. Cunha, Mechanisms and signals for the nuclear import of proteins. Curr. Genomics 10, 550–557 (2009).
19. S. Chatterjee, M. Javier, U. Stochaj, In vivo analysis of nuclear protein traffic in mammalian cells. Exp. Cell Res. 236, 346–350 (1997).
20. B. Tian, B. T. Gabelt, B. Geiger, P. L. Kaufman, The role of the actomyosin system in regulating trabecular fluid outflow. Exp. Eye Res. 88, 713–717 (2009).
21. H. L. Yin, Gelsolin: Calcium- and polyphosphoinositide-regulated actin-modulating protein. Bioessays 7, 176–179 (1987).
22. M. K. Ko, A. Yelenskiy, J. M. Gonzalez Jr., J. C. H. Tan, J. M. Gonzalez, Feedback-controlled constant-pressure anterior chamber perfusion in live mice. Mol. Vis. 20, 163–170 (2014).
23. S. P. Bothwell, E. Chan, I. M. Bernardini, Y. M. Kuo, W. A. Gahl, R. L. Nussbaum, Mouse model for Lowe syndrome/Dent Disease 2 renal tubulopathy. J. Am. Soc. Nephrol. 22, 443–448 (2011).
24. H. L. Yin, P. A. Janmey, Phosphoinositide regulation of the actin cytoskeleton. Annu. Rev. Physiol. 65, 761–789 (2003).
25. D. Dambournet, M. Machicoane, L. Chesneau, M. Sachse, M. Rocancourt, A. El Marjou, E. Formstecher, R. Salomon, B. Goud, A. Echard, Rab35 GTPase and OCRL phosphatase remodel lipids and F-actin for successful cytokinesis. Nat. Cell Biol. 13, 981–988 (2011).
26. A. Kühbacher, D. Dambournet, A. Echard, P. Cossart, J. Pizarro-Cerdá, Phosphatidylinositol 5-phosphatase oculocerebrorenal syndrome of Lowe protein (OCRL) controls actin dynamics during early steps of Listeria monocytogenes infection. J. Biol. Chem. 287, 13128–13136 (2012).
27. N. Luo, A. Kumar, M. Conwell, R. N. Weinreb, R. Anderson, Y. Sun, Compensatory role of inositol 5-phosphatase INPP5B to OCRL in primary cilia formation in oculocerebrorenal syndrome of Lowe. PLOS ONE 8, e66727 (2013).
28. S. P. Bothwell, L. W. Farber, A. Hoagland, R. L. Nussbaum, Species-specific difference in expression and splice-site choice in Inpp5b, an inositol polyphosphate 5-phosphatase paralogous to the enzyme deficient in Lowe Syndrome. Mamm. Genome 21, 458–466 (2010).
29. U. Schlötzer-Schrehardt, M. Zenkel, R. M. Nüsing, Expression and localization of FP and EP prostanoid receptor subtypes in human ocular tissues. Invest. Ophthalmol. Vis. Sci. 43, 1475–1487 (2002).
30. D. A. Ryskamp, A. M. Frye, T. T. Phuong, O. Yarishkin, A. O. Jo, Y. Xu, M. Lakk, A. Iuso, S. N. Redmon, B. Ambati, G. Hageman, G. D. Prestwich, K. Y. Torrejon, D. Križaj, TRPV4 regulates calcium homeostasis, cytoskeletal remodeling, conventional outflow and intraocular pressure in the mammalian eye. Sci. Rep. 6, 30583 (2016).
31. M. Wiederholt, H. Thieme, F. Stumpff, The regulation of trabecular meshwork and ciliary muscle contractility. Prog. Retin. Eye Res. 19, 271–295 (2000).
32. K. Steinhausen, F. Stumpff, O. Strauß, H. Thieme, M. Wiederholt, Influence of muscarinic agonists and tyrosine kinase inhibitors on L-type Ca2+ channels in human and bovine trabecular meshwork cells. Exp. Eye Res. 70, 285–293 (2000).
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

Prosseda et al., Sci. Adv. 2020; 6 : eaay8699 29 April 2020
S C I E N C E A D V A N C E S | R E S E A R C H A R T I C L E
12 of 12
33. H. Thieme, K. Steinhausen, A. Ottlecz, G. N. Lambrou, O. Strauss, M. Wiederholt, R. Rosenthal, Effects of unoprostone and endothelin 1 on L-type channel currents in human trabecular meshwork cells. Ophthalmic Res. 37, 293–300 (2005).
34. B. G. Coon, V. Hernandez, K. Madhivanan, D. Mukherjee, C. B. Hanna, I. Barinaga-Rementeria Ramirez, M. Lowe, P. L. Beales, R. C. Aguilar, The lowe syndrome protein OCRL1 is involved in primary cilia assembly. Hum. Mol. Genet. 21, 1835–1847 (2012).
35. N. Luo, C. C. West, C. A. Murga-Zamalloa, L. Sun, R. M. Anderson, C. D. Wells, R. N. Weinreb, J. B. Travers, H. Khanna, Y. Sun, OCRL localizes to the primary cilium: A new role for cilia in Lowe syndrome. Hum. Mol. Genet. 21, 3333–3344 (2012).
36. K. E. Keller, S. K. Bhattacharya, T. Borrás, T. M. Brunner, S. Chansangpetch, A. F. Clark, W. M. Dismuke, Y. du, M. H. Elliott, C. R. Ethier, J. A. Faralli, T. F. Freddo, R. Fuchshofer, M. Giovingo, H. Gong, P. Gonzalez, A. Huang, M. A. Johnstone, P. L. Kaufman, M. J. Kelley, P. A. Knepper, C. C. Kopczynski, J. G. Kuchtey, R. W. Kuchtey, M. H. Kuehn, R. L. Lieberman, S. C. Lin, P. Liton, Y. Liu, E. Lütjen-Drecoll, W. Mao, M. Masis-Solano, F. McDonnell, C. M. McDowell, D. R. Overby, P. P. Pattabiraman, V. K. Raghunathan, P. V. Rao, D. J. Rhee, U. R. Chowdhury, P. Russell, J. R. Samples, D. Schwartz, E. B. Stubbs, E. R. Tamm, J. C. Tan, C. B. Toris, K. Y. Torrejon, J. A. Vranka, M. K. Wirtz, T. Yorio, J. Zhang, G. S. Zode, M. P. Fautsch, D. M. Peters, T. S. Acott, W. D. Stamer, Consensus recommendations for trabecular meshwork cell isolation, characterization and culture. Exp. Eye Res. 171, 164–173 (2018).
37. J. T. Morgan, J. A. Wood, N. J. Walker, V. K. Raghunathan, D. L. Borjesson, C. J. Murphy, P. Russell, Human trabecular meshwork cells exhibit several characteristics of, but are distinct from, adipose-derived mesenchymal stem cells. J. Ocul. Pharmacol. Ther. 30, 254–266 (2014).
38. Q. Wang, Z. Wu, J. Zhang, J. Firrman, H. Wei, Z. Zhuang, L. S. Liu, L. Miao, Y. Hu, D. Li, Y. Diao, W. Xiao, A robust system for production of superabundant VP1 recombinant AAV vectors. Mol. Ther. Methods Clin. Dev. 7, 146–156 (2017).
39. A. Boussommier-Calleja, J. Bertrand, D. F. Woodward, C. R. Ethier, W. D. Stamer, D. R. Overby, Pharmacologic manipulation of conventional outflow facility in ex vivo mouse eyes. Investig. Ophthalmol. Vis. Sci. 53, 5838–5845 (2012).
40. B. Bogner, S. L. Boye, S. H. Min, J. J. Peterson, Q. Ruan, Z. Zhang, H. A. Reitsamer, W. W. Hauswirth, S. E. Boye, Capsid mutated adeno-associated virus delivered to the anterior chamber results in efficient transduction of trabecular meshwork in mouse and rat. PLOS ONE 10, e0128759 (2015).
41. M. Lock, M. Alvira, L. H. Vandenberghe, A. Samanta, J. Toelen, Z. Debyser, J. M. Wilson, Rapid, simple, and versatile manufacturing of recombinant adeno-associated viral vectors at scale. Hum. Gene Ther. 21, 1259–1271 (2010).
42. X. L. Xu, D. Cobrinik, S. Jhanwar, Producing Lentivirus in 293T Cells with Polyjet. Protoc. Exch. 10.1038/protex.2014.038 (2014).
43. C. Cao, E. Zakharian, I. Borbiro, T. Rohacs, Interplay between calmodulin and phosphatidylinositol 4,5-bisphosphate in Ca 2+-induced inactivation of transient receptor potential vanilloid 6 channels. J. Biol. Chem. 288, 5278–5290 (2013).
44. Y. Kwon, T. Hofmann, C. Montell, Integration of phosphoinositide- and calmodulin-mediated regulation of TRPC6. Mol. Cell 25, 491–503 (2007).
Acknowledgments: We thank J. L. Goldberg for thoughtful comments during the preparation of this manuscript, R. Nussbaum for the gift of Lowe syndrome mouse model, C. Wells for the phosphoinositide fluorescent protein constructs, and P. de Camilli for CIBN-EGFP-CAAX and mCh-CRY2-OCRL constructs. Funding: This work was supported by NIH/NEI [K08-EY022058 (to Y.S.), R01-EY025295 (to Y.S.), and VA merit CX001298 (to Y.S.)], Ziegler Foundation for the Blind (to Y.S.) [R01-EY-023295 (to Y.H.), R01-EY024932 (Y.H.), and R01-EY022359 (to W.D.S.)], Children’s Health Research Institute Award (to Y.S.), Research for Prevention of Blindness Unrestricted grant (Stanford Ophthalmology), American Glaucoma Society (to Y.S.), Lowe Syndrome Association (to Y.S.), Knights Templar Eye Foundation (to Y.S.), and P30 Vision Center grant to Stanford Ophthalmology Department. Y.S. is a Laurie Kraus Lacob Faculty Scholar in Pediatric Translational Medicine. Author contributions: P.P.P. designed and carried out all experiments and wrote the manuscript. J.A.A. assisted with in vivo studies. B.W., T.J.K., and K.N. contributed to the experimental design and reviewed the manuscript. W.D.S. and Y.H. provided valuable advice and experimental suggestions for this study. Y.S. supervised the whole project. Competing interests: The authors declare that they have no competing interests. Data and materials availability: All data needed to evaluate the conclusions in the paper are present in the paper and/or the Supplementary Materials. The Ocrl−/− Inpp5b−/− INPP5B+/+ mice can be provided by corresponding author pending scientific review and a completed material transfer agreement. Requests for the Ocrl−/− Inpp5b−/− INPP5B+/+ mice should be submitted to Y.S. ([email protected]). Additional data related to this paper may be requested from the authors.
Submitted 25 July 2019Accepted 11 February 2020Published 29 April 202010.1126/sciadv.aay8699
Citation: P. P. Prosseda, J. A. Alvarado, B. Wang, T. J. Kowal, K. Ning, W. D. Stamer, Y. Hu, Y. Sun, Optogenetic stimulation of phosphoinositides reveals a critical role of primary cilia in eye pressure regulation. Sci. Adv. 6, eaay8699 (2020).
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from

pressure regulationOptogenetic stimulation of phosphoinositides reveals a critical role of primary cilia in eye
Philipp P. Prosseda, Jorge A. Alvarado, Biao Wang, Tia J. Kowal, Ke Ning, W. Daniel Stamer, Yang Hu and Yang Sun
DOI: 10.1126/sciadv.aay8699 (18), eaay8699.6Sci Adv
ARTICLE TOOLS http://advances.sciencemag.org/content/6/18/eaay8699
MATERIALSSUPPLEMENTARY http://advances.sciencemag.org/content/suppl/2020/04/27/6.18.eaay8699.DC1
REFERENCES
http://advances.sciencemag.org/content/6/18/eaay8699#BIBLThis article cites 43 articles, 10 of which you can access for free
PERMISSIONS http://www.sciencemag.org/help/reprints-and-permissions
Terms of ServiceUse of this article is subject to the
is a registered trademark of AAAS.Science AdvancesYork Avenue NW, Washington, DC 20005. The title (ISSN 2375-2548) is published by the American Association for the Advancement of Science, 1200 NewScience Advances
License 4.0 (CC BY-NC).Science. No claim to original U.S. Government Works. Distributed under a Creative Commons Attribution NonCommercial Copyright © 2020 The Authors, some rights reserved; exclusive licensee American Association for the Advancement of
on Septem
ber 7, 2020http://advances.sciencem
ag.org/D
ownloaded from