Causes of Lymphadenopathy in Childern
Transcript of Causes of Lymphadenopathy in Childern
-
8/21/2019 Causes of Lymphadenopathy in Childern
1/24
Causes of peripheral lymphadenopathy in children
Last literature review version 18.3: Thu Sep 30 00:00:00 GMT 2010 | This topiclast updated: Thu Sep 30 00:00:00 GMT 2010
Official reprint from UpToDate® www.uptodate.com
©2011 UpToDate®
Authors Kenneth L McClain, MD, PhD Robert H Fletcher, MD, MSc
Section Editors Jan E Drutz, MD Sheldon L Kaplan, MD Donald H Mahoney, Jr, MD
Deputy Editor Mary M Torchia, MD
INTRODUCTION — The causes of peripheral lymphadenopathy in children will be reviewed
here. The approach to the child with peripheral lymphadenopathy, cervical lymphadenitis,
and the causes and evaluation of peripheral lymphadenopathy in adults are discussed
separately. (See "Etiology and clinical manifestations of cervical lymphadenitis in
children" and "Approach to the child with peripheral lymphadenopathy" and "Evaluation of
peripheral lymphadenopathy in adults".)
ANATOMY AND DEFINITIONS — The location of peripheral lymph node groups is shown
schematically in the figures (figure 1 and figure 2). Normal lymph nodes in most regions
usually are less than 1 cm in their longest diameter; normal lymph nodes in the
epitrochlear region usually are less than 0.5 cm in diameter, and normal lymph nodes in the
inguinal region usually are less than 1.5 cm in diameter. Normal lymph nodes tend to be
larger in childhood (ages 2 to 10 years) than later in life. Lymph nodes often are palpable in
the inguinal region in healthy individuals, perhaps because chronic trauma and infection are
so common in the lower extremities. Lymph nodes also may be palpable in the neck
(particularly submandibular lymph nodes) because of previous head and neck infections.
PATHOGENESIS — Lymph node enlargement may be caused by [1]:
Replication of cells within the node in response to antigenic stimuli or as a result of
malignant transformation
Entry of large numbers of cells exogenous to the node (eg, neutrophils or metastatic
neoplastic cells)
Deposition of foreign material within histiocytic cells of the node (as occurs in lipid
storage diseases)
Vascular engorgement and edema secondary to local cytokine release Suppuration secondary to tissue necrosis
EPIDEMIOLOGY — Children frequently have palpable lymph nodes because their immune
systems are being activated by environmental antigens and the common organisms to
which they are exposed. The prevalence of lymphadenopathy in the various lymph node
groups varies with age and site [2,3]. Small occipital and postauricular nodes, for example,
are common in infants, but not in older children [2]. In contrast, cervical and inguinal nodes
are more common after two years of age than in the first six months of life [2,3].
Epitrochlear and supraclavicular adenopathy are uncommon at any age.
Page 1 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
2/24
In one review, 44 percent of children younger than five years who were seen for well-child
visits and 64 percent of those seen for "sick" visits had lymphadenopathy [2]. Most of the
children with adenopathy detected at "sick" visits were between three and five years of age.
Many patients with unexplained lymphadenopathy (and their clinicians) are concerned
about the possibility of malignancy. The prevalence of malignancy among patients seen in
the primary care setting is relatively low [4,5]. In contrast, the prevalence of malignancy inlymph node biopsies performed in pediatric referral centers ranges from 13 to 27 percent
[3,6,7].
In the largest of these series, 239 children underwent peripheral lymph node biopsies for
evaluation of lymphadenopathy [3]. The following etiologies were noted:
Reactive hyperplasia of undetermined etiology — 52 percent
Granulomatous disease (eg, cat scratch disease, atypical mycobacteria,
mycobacterium tuberculosis, fungal infections, or Langerhans cell histiocytosis
(histiocytosis X)) — 32 percent
Neoplastic disease — 13 percent; among these two-thirds had Hodgkin disease
Chronic dermatopathic or bacterial infections — 3 percent
A higher incidence of cancer is expected in patients with certain clinical characteristics,
including weight loss (>10 percent of body weight), abnormal complete blood count (CBC)
or chest radiograph, generalized adenopathy without a clear etiology, fevers, and lack of
upper respiratory tract infection symptoms. We recommend immediate biopsy for patients
who have these findings. In conjunction with the other reasons for biopsy (weight loss,
abnormal CBC, etc), lymph node biopsy also may be indicated in children with persistently
elevated erythrocyte sedimentation rate (ESR) or rising ESR despite antibiotic therapy.
(See "Approach to the child with peripheral lymphadenopathy", section on 'Lymph node
biopsy'.)
OVERVIEW — Lymphadenopathy can be caused by a vast array of diseases (table 1) and
drugs (table 2) [8,9]. Some presentations suggest a specific disease process, whereas a
few diseases present predominantly with lymphadenopathy.
It is clinically useful to classify the causes of lymphadenopathy according to whether the
lymphadenopathy is localized (in only one region, such as the neck or axilla) (table 3) or
generalized (occurring in more than one noncontiguous region) (table 4A-B) [9].
Conditions that can mimic lymphadenopathy are discussed below. (See 'Mimics of
lymphadenopathy' below.)
LOCALIZED LYMPHADENOPATHY — Localized lymphadenopathy is present in only one
region, such as the neck or axilla.
Cervical — The anterior cervical lymph nodes are enlarged in a variety of infections of the
head and neck and in systemic infections such as toxoplasmosis, Epstein-Barr virus (EBV),
or cytomegalovirus (CMV) infection. Only one-quarter of patients with enlarged cervical
nodes have another serious disease, which most often is mycobacterial. Upper posterior
cervical lymphadenopathy rarely is associated with significant diseases in children [8,9].
In considering the causes of cervical lymphadenopathy, it is helpful to distinguish between
acute (develops over a few days) and subacute/chronic (develops over weeks to months)
Page 2 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
3/24
lymphadenopathy and whether the adenopathy is unilateral or bilateral. (See "Etiology and
clinical manifestations of cervical lymphadenitis in children".)
Inflamed cervical nodes that develop over a few days and progress to fluctuation, especially
in children, typically are caused by staphylococcal (picture 1) and streptococcal infection
[10]. The source of infection may be unapparent even after careful examination. Treatment
typically begins first with a course of antibiotics, but incision and drainage may be
indicated. Antimicrobial treatment of cervical lymphadenitis is discussed separately.(See "Diagnostic approach to and initial treatment of cervical lymphadenitis in children",
section on 'Initial treatment'.)
Fluctuant cervical nodes that develop over weeks to months without significant
inflammation or tenderness suggest infection with Mycobacterium tuberculosis, atypical
mycobacteria, or Bartonella henselae, the agent of cat scratch disease. Cat scratch disease
is discussed separately. (See "Microbiology, epidemiology, clinical manifestations, and
diagnosis of cat scratch disease".)
Mycobacterial infections can present with lymphadenopathy alone, especially in the neck
(scrofula). M. avium complex and M. scrofulaceum account for most cases in children
[11,12]. Nodes typically are nontender, enlarge over weeks to months without prominent
systemic symptoms, and can progress to matting and fluctuation (picture 2). (See "Etiology
and clinical manifestations of cervical lymphadenitis in children", section on 'NTM infection'.)
Hard nodes, often associated with cancer in adults, are found infrequently in children. The
nodes involved with Hodgkin disease are rubbery and difficult to differentiate from
hyperplastic nodes or nodes caused by granulomatous disease. (See "Overview of Hodgkin
lymphoma in children and adolescents".)
Less common causes of cervical adenopathy, which are discussed below, include
malignancy, Kawasaki disease, Langerhans cell histiocytosis, autoimmune
lymphoproliferative disease, Rosai-Dorfman disease, sarcoidosis, and Kikuchi disease.(See 'Uncommon but important causes' below and "Clinical manifestations and diagnosis of
Kawasaki disease" and "Langerhans cell histiocytosis, Juvenile xanthogranuloma, and
Erdheim-Chester disease".)
Supraclavicular — Supraclavicular (or lower cervical) (figure 1) lymphadenopathy is
associated with a high risk of malignancy (up to 75 percent) in children [7,9]. Right
supraclavicular adenopathy is associated with cancer of the mediastinal lymph nodes. Left
supraclavicular adenopathy ("Virchow's node") suggests intraabdominal malignancy, most
often lymphoma.
Axillary — The axillary nodes receive drainage from the arm, thoracic wall, and breast.
Infections, including cat scratch disease, are common causes of axillary lymphadenopathy.In one series of 31 children who underwent axillary node biopsies, 11 (35 percent) had
reactive hyperplasia, and five (16 percent) had cat scratch disease [3]. (See "Microbiology,
epidemiology, clinical manifestations, and diagnosis of cat scratch disease".)
Inguinal — Inguinal lymphadenopathy in children usually is not associated with a specific
etiology unless the nodes are very large (>3 cm).
Epitrochlear — Palpable epitrochlear nodes (figure 2) are often pathologic in children.
However, many biopsied nodes show only hyperplasia if they are associated with cuts or
Page 3 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
4/24
abrasions and there are no other signs suggestive of malignancy. The differential diagnosis
for epitrochlear lymphadenopathy includes infections of the forearm or hand, leukemia,
lymphoma, and atypical mycobacterial infections. (See "Overview of the presentation and
classification of acute lymphoblastic leukemia in children".)
GENERALIZED LYMPHADENOPATHY — Generalized lymphadenopathy is present in two
or more noncontiguous regions. It may be a feature of numerous systemic diseases, many
of which are recognized by other clinical findings (table 4A-B). Several of these diseases arediscussed below.
Systemic infection — Systemic bacterial or viral illnesses are the most common causes of
generalized adenopathy [12]. Common viral causes of generalized lymphadenopathy
include EBV or CMV mononucleosis, rubella, and measles (in parts of the world where
rubella and measles are endemic).
Mononucleosis — Classic infectious mononucleosis is characterized by the triad of
moderate to high fever, pharyngitis, and lymphadenopathy. A characteristic distribution of
lymph node involvement occurs; typically it is symmetric and involves the posterior cervical
more than the anterior cervical chain. The posterior cervical nodes are deep to the
sternocleidomastoid muscles (figure 1). Lymphadenopathy also may be present in the
axillary and inguinal areas, which helps to distinguish infectious mononucleosis from other
causes of pharyngitis. The lymph nodes are kidney-shaped and may be large.
Lymphadenopathy peaks in the first week and then gradually subsides over two to three
weeks. (See "Infectious mononucleosis in adults and adolescents".)
HIV — Lymphadenopathy is common in primary human immunodeficiency virus (HIV)
infection. Nontender adenopathy primarily involving the axillary, cervical, and occipital
nodes develops in the majority of individuals during the second week of acute symptomatic
HIV infection, concomitant with the emergence of a specific immune response to HIV [12].
The nodes decrease in size after the acute presentation, but a modest degree of
adenopathy tends to persist. (See "Natural history and classification of pediatric HIV
infection", section on 'Clinical manifestations'.)
Miliary tuberculosis — Miliary tuberculosis is an important consideration in patients
with generalized lymphadenopathy. Miliary tuberculosis can be mistaken for malignancy.
(See "Clinical manifestations; diagnosis; and treatment of miliary
tuberculosis" and "Pathogenesis and epidemiology of miliary tuberculosis".)
Systemic lupus erythematosus — Enlargement of lymph nodes occurs in approximately
50 percent of patients with systemic lupus erythematosus (SLE). The nodes typically are
soft; nontender; discrete; varying in size from 0.5 to several centimeters; and usually
detected in the cervical, axillary, and inguinal areas. Lymphadenopathy is noted more
frequently at the onset of disease or in association with an exacerbation. Lymph node
enlargement also can be caused by infection or a lymphoproliferative disease in SLE; when
infections are present, the enlarged nodes are more likely to be tender. (See "Hematologic
problems in children and adolescents with systemic lupus erythematosus".)
Medications — Numerous medications may cause serum sickness that is characterized by
fever, arthralgias, rash, and generalized lymphadenopathy (table 3). Phenytoin can cause
generalized lymphadenopathy in the absence of a serum sickness reaction. (See "Serum
sickness and serum sickness-like reactions" and "Pharmacology of antiepileptic drugs",
Page 4 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
5/24
section on 'Phenytoin' and "Drug eruptions", section on 'Hypersensitivity syndrome'.)
UNCOMMON BUT IMPORTANT CAUSES — Lymphadenopathy is a central feature of
numerous less common systemic diseases that are important to consider because they are
life-threatening or require specific treatment (table 1).
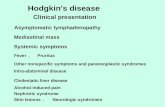
Malignancy — Neoplastic causes of lymphadenopathy include Hodgkin disease, non-
Hodgkin lymphoma, neuroblastoma, acute lymphocytic leukemia, acute myeloid leukemia,and rhabdomyosarcoma.
The prevalence of malignancy among patients seen in the primary care setting is relatively
low [4,5]. In contrast, the prevalence of malignancy in lymph node biopsies performed in
pediatric referral centers ranges from 13 to 27 percent [3,6,7]. (See 'Epidemiology' above.)
As discriminant features of malignancy versus other etiologies, fever, duration of
adenopathy, and tenderness are not particularly helpful.
However, a higher incidence of cancer is expected in patients with certain clinical
characteristics, including weight loss (>10 percent of body weight), abnormal CBC or chest
radiograph, generalized adenopathy without a clear etiology, fevers, and lack of upper
respiratory tract infection symptoms. We recommend immediate biopsy for patients who
have these findings. In conjunction with the other reasons for biopsy (weight loss,
abnormal CBC, etc.), lymph node biopsy also may be indicated in children with persistently
elevated ESR or rising ESR despite antibiotic therapy. (See "Approach to the child with
peripheral lymphadenopathy", section on 'Lymph node biopsy'.)
Kawasaki disease — Kawasaki disease, though an uncommon illness, is the most frequent
cause of childhood vasculitis. This syndrome is associated with fever, cervical
lymphadenopathy, and a variety of other manifestations, including conjunctivitis, mucositis,
rash, and coronary artery aneurysms. (See "Clinical manifestations and diagnosis of
Kawasaki disease".)
Tularemia — Patients with tularemia typically present with fever and a single
erythematous papulo-ulcerative lesion with a central eschar (picture 3) that is accompanied
by tender regional lymphadenopathy (picture 4). The majority of cases in the United States
occur in Arkansas, Missouri, and Oklahoma. Sources of infections in humans include vectors
(eg, ticks, biting flies, and mosquitoes), handling of infected animals (rodents and rabbits),
ingestion of inadequately cooked meat, drinking contaminated water, cat scratches or bites,
or splashing infected material into the eye or rubbing eyes with contaminated fingers.
(See "Microbiology, pathogenesis, and epidemiology of tularemia" and "Clinical
manifestations, diagnosis, and treatment of tularemia".)
Langerhans cell histiocytosis — Langerhans cell histiocytosis may present with unilateralor bilateral cervical lymph nodes. Sometimes there is massive enlargement similar to those
seen in Rosai-Dorfman disease. (See 'Rosai-Dorfman disease' below and "Langerhans cell
histiocytosis, Juvenile xanthogranuloma, and Erdheim-Chester disease".)
Hemophagocytic lymphohistiocytosis — Hemophagocytic lymphohistiocytosis patients
have diffuse adenopathy in one-third of cases. (See "Hemophagocytic lymphohistiocytosis".)
Chronic granulomatous disease — Chronic granulomatous disease (CGD) encompasses
a heterogeneous group of disorders characterized by genetic defects in the ability of
Page 5 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
6/24
phagocytes to generate reactive oxygen intermediates from molecular oxygen. These
defects manifest primarily as an immunodeficiency resulting in frequent, severe infections,
including pneumonia, abscesses, suppurative adenitis, osteomyelitis, bacteremia/fungemia,
and superficial skin infections (cellulitis/impetigo). (See "Primary disorders of phagocytic
function: An overview".)
Castleman's disease — Castleman's disease is an uncommon lymphoproliferative disorder
characterized by massive lymphadenopathy and systemic features such as fever,hepatomegaly, splenomegaly, and polyclonal hypergammaglobulinemia. (See "Castleman's
disease".)
Autoimmune lymphoproliferative disease — Patients with autoimmune
lymphoproliferative disease (ALPS), also known as the Canale-Smith syndrome or
autoimmunity/lymphoproliferation syndrome, usually present in the first year of life with
massive cervical adenopathy that may obscure the angle of the jaw [13]. Splenomegaly
also can occur. Frequent associations with autoimmune diseases, including hemolytic
anemia, neutropenia, immune thrombocytopenic purpura, glomerulonephritis, and Guillain-
Barré syndrome, have been reported. The syndrome appears to be caused by a defect in
lymphocyte apoptosis (programmed cell death). (See "Apoptosis and autoimmune disease",section on 'Autoimmune lymphoproliferative syndrome'.)
Rosai-Dorfman disease — Rosai-Dorfman disease (sinus histiocytosis with massive
lymphadenopathy) often presents in children with markedly enlarged, nontender cervical
adenopathy of massive proportions, similar to patients with ALPS [14-18]. However, other
nodal sites, including the mediastinum, retroperitoneal, axillary, and inguinal sites, also
may be involved. Other manifestations include involvement of the nasal cavity, salivary
gland tissue and other regions of the head and neck, lytic bone lesions, pulmonary nodules,
or rash. Patients often are febrile when massive lymphadenopathy is present. Laboratory
evaluations show leukocytosis, polyclonal hypergammaglobulinemia, a hypochromic or
normocytic anemia, and elevated ESR. Treatment is uncertain; spontaneous resolution isfrequently observed [19].
Kikuchi disease — Kikuchi disease is a rare, benign condition of unknown cause usually
characterized by cervical lymphadenopathy (although it may be more generalized) and
fever. It is discussed in detail separately. (See "Kikuchi's disease".)
Inflammatory pseudotumor — Inflammatory pseudotumor of lymph nodes is a syndrome
of lymphadenopathy in one or more node groups, often with systemic symptoms. Nodes
show a fibrosing and inflammatory process [20].
Churg-Strauss syndrome — Massive lymphadenopathy in children with asthma may be a
rare manifestation of the Churg-Strauss syndrome (asthma, tissue and peripheral blood
eosinophilia, and granulomatous vasculitis). A case report of a boy with this triad plus a
mediastinal mass suggesting Hodgkin disease has been reported [21]. (See "Epidemiology,
pathogenesis, and pathology of Churg-Strauss syndrome (allergic granulomatosis and
angiitis)".)
Sarcoidosis — Children with sarcoid may present with impressive cervical adenopathy,
similar to ALPS or Rosai-Dorfman disease patients. Lymphadenopathy is present in 50
percent of patients with sarcoidosis, who often have weight loss, cough, fatigue, lethargy,
bone and joint pain, anorexia, and headache [22]. African-Americans represent two-thirds
Page 6 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
7/24
to three-fourths of patients. (See "Clinical manifestations and diagnosis of sarcoidosis".)
MIMICS OF LYMPHADENOPATHY — Conditions that can mimic an enlarged lymph node
include [23-25]:
Infection or stones in any of the salivary glands
Congenital anomalies: branchial cleft cyst, cystic hygroma, thyroglossal duct cyst
Thyroid nodule Soft-tissue swelling from trauma or an insect bite or sting
Hematoma
Inguinal hernia
Hemangioma, lymphangioma
Lipoma
Dermoid
Rheumatoid nodules
SUMMARY
Normal lymph nodes in most regions usually are less than 1 cm in their longest
diameter; normal lymph nodes in the epitrochlear region usually are less than 0.5 cm,
and normal lymph nodes in the inguinal region usually are less than 1.5 cm.
(See 'Anatomy and definitions' above.)
Lymphadenopathy can be caused by a vast array of diseases and drugs (table 1). It is
clinically useful to classify the causes of lymphadenopathy according to whether the
lymphadenopathy is localized or generalized. (See 'Overview' above.)
Localized lymphadenopathy is present in only one region. Causes of localized
lymphadenopathy are listed in the table (table 2). (See 'Localized
lymphadenopathy' above.)
Generalized lymphadenopathy is present in two or more noncontiguous regions.
Causes of generalized lymphadenopathy are listed in the table (table 3).
(See 'Generalized lymphadenopathy' above.)
Uncommon but important causes of peripheral lymphadenopathy in children include
malignancy, Kawasaki disease, tularemia, Langerhans cell histiocytosis,
hemophagocytic lymphohistiocytosis, autoimmune lymphoproliferative disease, Rosai-
Dorfman disease, Kikuchi disease, inflammatory pseudotumor, and Churg-Strauss
syndrome. (See 'Uncommon but important causes' above.)
Malignancy should be considered in children with peripheral lymphadenopathy and
weight loss, abnormal complete blood count (CBC) or chest radiograph, generalizedadenopathy without a clear etiology, fever >1 week, and lack of upper respiratory
tract infection symptoms. Immediate biopsy is indicated in such children. In
conjunction with the other reasons for biopsy (weight loss, abnormal CBC, etc.),
lymph node biopsy also may be indicated in children with persistently elevated
erythrocyte sedimentation rate (ESR) or rising ESR despite antibiotic therapy.
(See 'Malignancy' above and "Approach to the child with peripheral
lymphadenopathy", section on 'Lymph node biopsy'.)
Page 7 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
8/24
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
1. Jackson, MA, Chesney, PJ. Lymphatic system and generalized lymphadenopathy. In:
Principles and Practice of Pediatric Infectious Diseases, 2nd ed, Long, SS, Pickering,LK, Prober, CG (Eds), Churchill Livingstone, New York 2008. p.135.
2. Herzog, LW. Prevalence of lymphadenopathy of the head and neck in infants andchildren. Clin Pediatr (Phila) 1983; 22:485.
3. Knight, PJ, Mulne, AF, Vassy, LE. When is lymph node biopsy indicated in children withenlarged peripheral nodes? Pediatrics 1982; 69:391.
4. Ferrer, R. Lymphadenopathy: differential diagnosis and evaluation. Am Fam Physician1998; 58:1313.
5. HEINRICH, WA, JUDD ES, Jr. A critical analysis of biopsy of lymph nodes. Mayo ClinProc 1948; 23:465.
6. Lake, AM, Oski, FA. Peripheral lymphadenopathy in childhood. Ten-year experiencewith excisional biopsy. Am J Dis Child 1978; 132:357.
7. Soldes, OS, Younger, JG, Hirschl, RB. Predictors of malignancy in childhood peripherallymphadenopathy. J Pediatr Surg 1999; 34:1447.
8. Barton, LL, Feigin, RD. Childhood cervical lymphadenitis: a reappraisal. J Pediatr 1974;84:846.
9. Williamson HA, Jr. Lymphadenopathy in a family practice: a descriptive study of 249cases. J Fam Pract 1985; 20:449.
10. Lai, KK, Stottmeier, KD, Sherman, IH, McCabe, WR. Mycobacterial cervicallymphadenopathy. Relation of etiologic agents to age. JAMA 1984; 251:1286.
11. Spark, RP, Fried, ML, Bean, CK, et al. Nontuberculous mycobacterial adenitis of
childhood. The ten-year experience at a community hospital. Am J Dis Child 1988;142:106.
12. Gaines, H, von Sydow, M, Pehrson, PO, Lundbegh, P. Clinical picture of primary HIVinfection presenting as a glandular-fever-like illness. BMJ 1988; 297:1363.
13. Sneller, MC, Wang, J, Dale, JK, et al. Clincal, immunologic, and genetic features of anautoimmune lymphoproliferative syndrome associated with abnormal lymphocyteapoptosis. Blood 1997; 89:1341.
14. McAlister, WH, Herman, T, Dehner, LP. Sinus histiocytosis with massivelymphadenopathy (Rosai-Dorfman disease). Pediatr Radiol 1990; 20:425.
15. Horneff, G, Jürgens, H, Hort, W, et al. Sinus histiocytosis with massivelymphadenopathy (Rosai-Dorfman disease): response to methotrexate and
mercaptopurine. Med Pediatr Oncol 1996; 27:187. 16. Pulsoni, A, Anghel, G, Falcucci, P, et al. Treatment of sinus histiocytosis with massive
lymphadenopathy (Rosai-Dorfman disease): report of a case and literature review. AmJ Hematol 2002; 69:67.
17. Lee, KY, Yeon, YH, Lee, BC. Kikuchi-Fujimoto disease with prolonged fever in children.Pediatrics 2004; 114:e752.
18. La Barge DV, 3rd, Salzman, KL, Harnsberger, HR, et al. Sinus histiocytosis withmassive lymphadenopathy (Rosai-Dorfman disease): imaging manifestations in thehead and neck. AJR Am J Roentgenol 2008; 191:W299.
Page 8 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
9/24
19. Payne, JH, Evans, M, Gerrard, MP. Kikuchi-Fujimoto disease: a rare but importantcause of lymphadenopathy. Acta Paediatr 2003; 92:261.
20. Moran, CA, Suster, S, Abbondanzo, SL. Inflammatory pseudotumor of lymph nodes: astudy of 25 cases with emphasis on morphological heterogeneity. Hum Pathol 1997;28:332.
21. Casey, M, Radel, E, Ratech, H. Lymph node manifestations of limited Churg-Strausssyndrome. J Pediatr Hematol Oncol 2000; 22:468.
22. Pattishall, EN, Strope, GL, Spinola, SM, Denny, FW. Childhood sarcoidosis. J Pediatr1986; 108:169.
23. Torsiglieri AJ, Jr, Tom, LW, Ross AJ, 3rd, et al. Pediatric neck masses: guidelines forevaluation. Int J Pediatr Otorhinolaryngol 1988; 16:199.
24. Margileth, AM. Sorting out the causes of lymphadenopathy. Contemp Pediatr 1995;12:23.
25. Yaris, N, Cakir, M, Sözen, E, Cobanoglu, U. Analysis of children with peripherallymphadenopathy. Clin Pediatr (Phila) 2006; 45:544.
Page 9 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
10/24
GRAPHICS
Lymph nodes of the head and neck
This drawing schematically depicts the major lymph nodes in the head and neckarea that are likely to be enlarged on physical examination in patients withvarious local or systemic diseases. The major nodal groups are shown here inbold, with the areas draining into these nodal groups noted when appropriate.While enlargement of both the left and right supraclavicular lymph nodes mayreflect disease in the thorax, left supraclavicular nodal enlargement, because ofits drainage pattern, may also reflect the presence of abdominal involvement (ie,Virchow's node).
Page 10 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
11/24
Lymph node regions in the body
Page 11 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
12/24
Causes of peripheral lymphadenopathy
Cause Examples
Infections
Bacterial
Localized Streptococcal pharyngitis; skin infections; tularemia; plague; catscratch disease; diphtheria; chancroid; rat bite fever
Generalized Brucellosis; leptospirosis; lymphogranuloma venereum; typhoid fever
Viral Human immunodeficiency virus; Epstein-Barr virus; herpessimplex virus; cytomegalovirus; mumps; measles; rubella;hepatitis B; dengue fever
Mycobacterial Mycobacterium tuberculosis; atypical mycobacteria
Fungal Histoplasmosis; coccidioidomycosis; cryptococcosis
Protozoal Toxoplasmosis; Leishmaniasis
Spirochetal Secondary syphilis; Lyme disease
Cancer Squamous cell cancer head and neck; metastatic; lymphoma;leukemia
Lymphoproliferative Angioimmunoblastic lymphadenopathy with dysproteinemia
Autoimmune lymphoproliferative disease
Rosai-Dorfman disease
Hemophagocytic lymphohistiocytosis
Immunologic Serum sickness; drug reactions (phenytoin)
Endocrine Hypothyroidism; Addison's disease
Miscellaneous Sarcoidosis; lipid storage diseases; amyloidosis; histiocytosis;chronic granulomatous diseases; Castleman's disease; Kikuchi'sdisease; Kawasaki disease; inflammatory pseudotumor;systemic lupus erythematosus; rheumatoid arthritis; Still'sdisease; dermatomyositis; Churg-Strauss syndrome
Page 12 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
13/24
Drugs that cause lymphadenopathy
Data from Pangalis, GA, Vassilakopoulos, TP, Boussiotis, VA, Fessas, P, Semin Oncol 1993;
20:570.
Allopurinol
Atenolol
Captopril
Carbamazepine
Cephalosporins
Gold
Hydralazine
Penicillin
Phenytoin
Primidone
Pyrimethamine
Quinidine
Sulfonamides
Sulindac
Page 13 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
14/24
Causes of localized lymphadenopathy in children
Lymph nodegroup
Area ofdrainage
Causes
Occipital Posterior scalp, neck Common: Scalp infections (including tinea
capitis, lice), insect bites, seborrhea,roseola (human herpes virus 6, HHV6)
Less common: Rubella, acute lymphoblasticleukemia
Posterior auricular Temporal and parietalscalp
Rubella, roseola (HHV6, HHV7)
Anterior auricular(preauricular)
Anterior and temporalscalp, anterior earcanal and pinna,lateral conjunctivaand eyelids
Common: Eye or conjuctival infections (eg,adenovirus, oculoglandular syndrome)
Less common: Cat scratch disease,tularemia, listeriosis
Submental Central lower lip,floor of mouth
Tongue, gum, buccal mucosal, and dentalinfections (eg, gingivostomatitis), group Bstreptococcal infection (in infants
-
8/21/2019 Causes of Lymphadenopathy in Childern
15/24
Data from: Segal, GB, Hall, CB. Lymphadenopathy. In: Primary Pediatric Care, 4th ed, Hoekelman,
RA (Ed), Mosby, St. Louis 2001. p.1192. Perkins, SL, Segal, GH, Kjeldsberg, CR. Work-up of
lymphadenopathy in children. Semin Diagn Pathol 1995; 12:284. Malley, R. Lymphadenopathy. In:
Textbook of Pediatric Emergency Medicine, 5th ed, Fleisher, GR, Ludwig, S, Henretig, FM (Eds),
Lippincott Williams and Wilkins, Philadelphia 2006. p.421.
rat-bite fever, toxoplasmosis,rheumatologic disease of the hand or wrist
Epitrochlear Hand, forearm, elbow Common: Viral diseases, sarcoidosis,tularemia, infection of hands
Less common: Cat scratch disease,tularemia, secondary syphilis,
rheumatologic disease of the hand or wrist
Inguinal Leg and genitalia Common: Genital herpes, primary; syphilis,gonococcal infection, lymphoma
Less common: Yersinia pestis, chancroid,lymphogranuloma venereum
Popliteal Posterior leg andknee
Local infection
Page 15 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
16/24
Infectious causes of generalized lymphadenopathy in children
InfectiousSelected clinical features that may be
present
Viral
Epstein-Barr virus Tonsillopharyngitis, splenomegaly (>50 percent), fever,malaise, fatigue; periorbital edema
Cytomegalovirus Fever, malaise, fatigue, occasional hepatosplenomegaly
Herpes simplex virus Grouped vesicles; gingivostomatitis
Varicella zoster virus Generalized vesicular rash appearing in crops
Adenovirus Respiratory tract symptoms, pharyngitis, conjunctivitis
Rubella Fever and rash; may be asymptomatic
Hepatitis B virus High-risk sexual behavior, exposure to blood products
Rubeola (measles) Maculopapular rash with cranial to caudal progression
Humanimmunodeficiencyvirus
Recurrent bacterial infection, opportunistic infection, fever,diarrhea, encephalopathy, failure to thrive,hepatosplenomegaly
Fungal
Coccidioidomycosis(valley fever)
Pneumonia; travel to or residence in endemic area (eg,southwestern United States)
Blastomycosis Pneumonia; travel to or residence in an endemic area (eg,southeastern and south central United States, Africa)
Bacterial
Group A streptococcaldisease
Rash followed by desquamation
Brucellosis Fever, sweats, malaise, fatigue, weight loss, ingestion ofunpasteurized milk; exposure to cattle, sheep, or goats
Tularemia Fever, chills, headache; ingestion of undercooked meats,exposure to rabbits, rodents, biting flies, or mosquitoes
Leptospirosis Fever, rigors, myalgia, headache, conjunctival injection, rash,hepatosplenomegaly
Spirochetal
Syphilis Rash, fever, malaise, anorexia, and weight loss,heptaomegaly
Lyme disease Erythema migrans, fever, headache, myalgia, malaise,arthralgia
Parasitic
Toxoplasmosis Most infections in immunocompetent hosts areasymptomatic; myalgia, fatigue, fever, splenomegaly, andmaculopapular rash may be present; exposure to cats
Page 16 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
17/24
Data from: Malley, R. Lymphadenopathy. In: Textbook of Pediatric Emergency Medicine, 5th ed,
Fleisher, GR, Ludwig, S, Henretig, FM (Eds), Lippincott Williams and Wilkins, Philadelphia 2006.
p.421.
Leishmaniasis Cutaneous lesions, organomegaly, fever, cachexia; exposureto sandflies
Malaria Fever, travel to or residence in an endemic area
Page 17 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
18/24
Noninfectious causes of generalized lymphadenopathy in children
NeoplasticSelected clinical features that
may be present
Primary
Hodgkin lymphoma Usually manifests as cervicallymphadenopathy; adenopathy may beunilateral; respiratory distress can occur
Non-Hodgkin lymphoma Rapidly enlarging diffuse adenopathy,abdominal pain, vomiting; adenopathy isusually bilateral; respiratory distress canoccur
Metastatic
Acute lymphocytic or myelogenousleukemia
Ill appearance, bleeding,hepatosplenomegaly, anemia,thrombocytopenia; occipital nodes often
prominent
Neuroblastoma Abdominal mass; opsoclonus-myoclonus,proptosis, periorbital echymoses, nasalobstruction, Horner syndrome, subcutaneousnodules, secretory diarrhea
Rhabdomyosarcoma Proptosis; nasal, aural, or sinus obstruction;hematuria; urinary obstruction; constipation
Immunologic
Vasculitis syndromes (systemic lupuserythematosus, rheumatoid arthritis)
Patients may have generalized adenopathyduring the acute phase of illness
Serum sickness Rash, splenomegaly, myalgia, arthritis
Autoimmune hemolytic anemia Lymphadenopathy coincides with hemolysis
Chronic granulomatous disease Recurrent infection, skin abscesses,suppurative adenitis
Metabolic
Gaucher disease Hepatosplenomegaly, anemia,thrombocytopenia, osteopenia
Niemann-Pick disease Hepatosplenomegaly, loss of neurologicfunction
Drugs
Phenytoin, phenobarbitol,carbamazepinem, isoniazid, aspirin,barbiturates, penicillin, tetracycline,iodides, sulfonamides, allopurinol, andphenylbutazone.
Severe maculopapular rash, fever,hepatosplenomegaly, jaundice, anemia,leukopenia, and plasmacytosis occurringduring or after the lymphadenopathy
Miscellaneous
Sarcoidosis Multisystem granulomatous disease;generalized adenopathy with prominent
Page 18 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
19/24
Data from: Malley, R. Lymphadenopathy. In: Textbook of Pediatric Emergency Medicine, 5th ed,
Fleisher, GR, Ludwig, S, Henretig, FM (Eds), Lippincott Williams and Wilkins, Philadelphia 2006.
p.421.
cervical involvement
Hemophagocytic lymphohistiocytosis Fever, hepatosplenomegaly, neurologicsymptoms, rash
Castleman's disease Fever, hepatosplenomegaly, polyclonalhypergammaglobulinemia
Langerhans cell histiocytosis Rash (brown to purplish papules), mucosallesions, lytic bone lesions, proptosis, diabetesinsipidus
Rosai-Dorfman disease (sinushistiocytosis with massivelymphadenopathy)
Chronic bilateral cervical adenopathy ischaracteristic; other nodal groups areinvolved in most cases; fever, anemia,leukocytosis, elevated ESR, andhypergammaglobulinemia
Hyperthyroidism Tachycardia, hypertension, diaporesis, weightloss, goiter, hyperreflexia
Papular acrodermatitis (Gianotti-Crosti
syndrome)
Rash on face, buttocks, limbs, palms, and
soles; hepatomegaly
Page 19 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
20/24
Staphylococcus aureus adenitis
Acute unilateral cervical adenitis caused by S. aureus.Submandibular nodes are affected in more than 50 percent ofcases. The lymph node is usually 3 to 6 cm in diameter, tender,warm, erythematous, nondiscrete, and poorly mobile.
Page 20 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
21/24
Mycobacterium avium adenitis
Mycobacterium avium cervical lymphadenitis in the parotid andsubmandibular regions. The parotid node underwent incompleteexcision and began to relapse. The submandibular node beganto spontaneously drain and formed an overlying scab.
Page 21 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
22/24
Tularemia eschar
Courtesy of Todd M. Pollack, MD.
Page 22 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
23/24
Tularemia adenitis
Ulceroglandular tularemia involving the submental nodecharacterized by a papular lesion in the drainage field of theinflamed lymph node.
Page 23 of 24Causes of peripheral lymphadenopathy in children
05-01-2011http://www.uptodate.com/online/content/topic.do?topicKey=gen_pedi/6167&view=print
-
8/21/2019 Causes of Lymphadenopathy in Childern
24/24
© 2011 UpToDate, Inc. All rights reserved. | Subscription and License Agreement | Support Tag:[ecapp1103p.utd.com-146.83.118.10-55F5675C57-348330]Licensed to: Universidad Catolica del Norte
Page 24 of 24Causes of peripheral lymphadenopathy in children