Cataract: the relation between myopia cataract morphologypresence and absence of either nuclear...
Transcript of Cataract: the relation between myopia cataract morphologypresence and absence of either nuclear...
British Journal of Ophthalmology, 1987, 71, 405-414
Cataract: the relation between myopia and cataractmorphologyNICHOLAS A P BROWN, AND ADRIAN R HILL
From the Nuffield Laboratory of Ophthalmology, University of Oxford, Walton Street, Oxford
SUMMARY The association between high myopia and cataract is already well established and anassociation between simple myopia and cataract has been suggested, but it has not been clear towhat extent the myopia precedes the cataract or is the result of it. The present study compares therefraction of a group of 100 British patients at the time of first presentation with cataract in whomthe refraction was also known four years previously, with a group of matched controls in whom therefraction was also known four years previous to presentation. The study shows that simple myopiadoes not appear to predispose to cataract. It is the development of the cataract itself, in particularnuclear sclerosis, which causes the refractive change towards myopia. The myopic change precedesthe development of cataract, and patients over the age of 55 showing a myopic change in refractionhave a very high probability of developing nuclear sclerotic cataract. The healthy aging eye andeyes with cortical cataract or subcapsular cataract, but without nuclear sclerosis, continue to show agradual hypermetropic change with time.
The relationship of cataract to high (or degenerative)myopia is a well accepted concept.' It has also beenconsidered that this relationship may extend toinvolve simple myopia and attention has been focusedon this recently by Weale,2 Perkins,' and VonKluxen,4 who each examined the refractive state ofpatients presenting at hospital with cataract andfound an excess incidence of myopic refraction inthem. Racz et al, who examined patients withpresenile cataract coming to surgery, found an excessincidence of myopia; the -19 to -21 dioptre groupbeing well represented, which further confirms theassociation of cataract with the higher degrees ofmyopia.Nuclear sclerotic cataract itself causes a change
towards myopia, and so it is not possible to drawconclusions from these previous studies about thebasic refractive states of the patients prior to thedevelopment of cataract. It is the object of thepresent study to make a contribution in this field.
Material and methods
It was decided to study a minimum of 100 patientspresenting with cataract, in whom the refractionCorrespondencc to Nicholas PhcIps Brown, 63 Harlcy Strcet,London WIN 1DD.
was known four years prior to the development ofcataract, and to compare them with the same numberof controls, matched for age, in whom the refractionwas also known four years prior to the time ofpresentation. A period longer than four years wouldhave been preferred but would have severely limitedrecruitment.The patients with cataract and the controls were all
patients attending a central London ophthalmicpractice, with the expectation of a refractive exam-ination and unaware of any eye disease. OnlyCaucasian subjects resident in England wereaccepted, in order to exclude the effects of differingenvironments. They could be admitted to the study ifthey had already attended four years previously.Patients were assigned to the cataract group whenthey had cataract visible by slit-lamp examination inthe undilated pupil and at least minimal interferencewith visual acuity 6/7-5 or worse after refractivecorrection. It was decided to exclude high myopiaand a limit was set at -12 D. Patients and controlswere excluded if they had a recognised potentialcause of cataract, including diabetes. Both thepatients and controls were recruited strictly in orderof their presentation without the exclusion of anycases that satisfied the above criteria. No attempt wasmade to match patients and controls for sex, but a
405
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
NA P Brown, andA R Hill
rig. ia
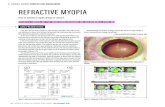
Fig. 1 Slit-image photography oflenses with early cataract.(a) Cortical, (b) nuclear, and (c) subcapsular.
good match occurred spontaneously. The cataractgroup consisted of 110 patients, 71 female and 39male, with 203 affected eyes. There were 110 controls(220 eyes), 74 female and 36 male.
Fig. lb
Fig. IC
The refractions were recorded, and to facilitateanalysis they were simplified to spherical equivalentto the nearest 0125 dioptres (ie., spherical com-ponent plus half cylindrical power in dioptres). Bycomparing the refraction at the time of presentationwith cataract with the refraction four years previouslythe change in refraction could be determined.To simplify the tabulation of the results in respectof age the subjects were grouped into five-year agecategories.The cataracts were classified at the slit-lamp into
cortical, nuclear, and subcapsular (Figs. la, b, and c).Although more than one cataract type may bepresent in an eye, it is possible to assess the refractivechange associated with each cataract type separatelyor in combination by grouping the data as in Fig. 2.By this means it is possible to partition the data in anumber of ways, either by using mutually exclusivecategories or, for example, by comparing all cataractshaving nuclear sclerosis against those without nuclearsclerosis.
Results
The age distributions of patients presenting withcataract and the matched control group are shown inFig 3, from which it will be noted there is very closeagreement. The most frequent age of presentationfor both sample population was between 71-75 years.In patients older than this the prevalence of cataract
406
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
Cataract: the relation between myopia and cataract morphology
Grouping of cataract types for analysis
Subcapsular Cataract
Present Absent
Nuclear Present a bCataract Absent c d
No. of eyes40 1
30 -
20 -
a comprises (N + SC) and (N + SC + C)
b
c
d
" (N) and (N + C)
"1 (SC) and (SC + C)
(C alone)
where N - Nuclear sclerosis
SC a Subcapsular cataract
C - Cortical cataract
eg (N + SC) represents the simultaneous presence
of nuclear sclerosis and subcapsular cataractFig. 2 Contingency matrixfor grouping the data accordingto thepresence or absence ofboth nuclear andsubcapsularcataract.
was ofcourse higher, but the incidence ofpresentationof new cases declined.The incidence of the various types of cataract as a
function of age is shown in Fig. 4. Among those eyespresenting with cataract cortical opacities were themost common, occurring in 63% of eyes, withnuclear cataract in 41% and subcapsular cataract in24%.No. of subjin each gro
40 -
36 -
32 -
28 -
24 -
20 -
16 -
12 -
8
4
0- _
ects)up
41. 46_tLb61 ~ /% ~9 ~k ~9' ~ Age (yrs
* Cataracts
3 Controls
41 '46 -51 '56 '61 '66, 71 '76 '81 '86, 9145 /50 55 6o 65 70 75 80 85 790 95 Age yrs)
Fig. 3 Age distribution ofall cataract patients (n=-O) andnon cataractous controls (n=110).
10 -
0-
,Cortical
il.. "I..
I
.. SubcapsuIar...... % :
40- 45- 56- 55- 66- 65- 70- 7A- 8b- 8§- 90-44 49 54 59 64 69 74 79 84 89 94
AgeFig. 4 Incidence ofthe various types ofcataract, as afunction ofrefractive error (all eyes). In 55 ofthe 202 eyespresenting with cataract more than one morphological type oflens opacity was present (see Table 1).
Slightly more than 70% of all eyes with cataractshowed a single type of cataract. The frequencies ofthese mutually exclusive cataracts and their occur-rence in combination are given in Table 1. Theincidence of the different cataracts occurring singlyor in combination is significantly different fromchance, (x2 RE = 92*91, and x2 LE = 91-98, for df=6have probabilities of occurrence of p < 0-0001). Ahigh correlation of cataract types occurring in theright and left eyes is also evident from Table 1, therebeing only a small number of uniocular cataracts.Such a high positive intereye correlation accords withclinical experience and is present in most ophthalmicdata.67 It precludes the combining of observationsfrom right and left eyes for a single statistical analysis.Separate analysis have therefore been conducted on
Table 1 Frequencies ofthe different cataract typespresenting in isolation or in combination for right and lefteyes
Cataract combination Right Left
Cortical alone (C) 46 46Nuclear alonc (N) 19 16Subcapsular alone (SC) 10 10(Cwith N 13 13C with SC 3 4N with SC 9 9C with N with SC 2 2Totals 102 100
These frequencies are from a total of 1 10 patients presenting withcataract, of which 18 were uniocular (10 right and 8 left).
407
4-
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
NA P Brown, and A R Hill
Table 2 Frequencies ofthefour major cataract groups asdefined in Fig. 2
Right eye Left eye
Subscapsular Cataract Subcapsular Cataractpresent absent present absent
Nuclearpresent 11 32 11 29Cataract present 13 46 14 46
single-eye data in a two-eye design, and only thoseresults where the analyses gave consistent findings forright and left eyes are presented.To test several hypotheses on the role of nuclear
cataract and subcapsular cataract on refractive changeover time the data were reorganised into four mutu-ally exclusive cataract groups as defined in Fig. 2.This four-way grouping permits a comparison of thepresence and absence of either nuclear cataract orsubcapsular cataract or both. It will be appreciatedfrom this grouping that the presence of corticalcataract is treated as a random variable, though sinceall the data treated in this way are from the eyes withcataracts those coded into cell D of the contingencytable refer to the presence of cortical cataract alone.When organised in this way, the separate data forright and left eyes are as shown in Table 2. Analysesby x2 on the data for both right and left eyes showthere was no difference in the presence or absence ofnuclear cataract in the proportion of eyes presentingeither with or without subcapsular cataract, (X2 RE =0033, X2 LE = 0 056, with df= 1). At its time of initial
occurrence, therefore, the presence of nuclearsclerosis was unrelated to the presence of subcapsularcataract.The mean refractive error (spherical equivalent)
for the four different cataract categories and thecontrol group, both at presentation and four yearsprior to presentation, are shown in Table 3. Themean refraction of the controls at the initial exam-
ination was one of slight hypermetropia (R+0.90 Dand L+0-72 D to the nearest 0-01 D), which accordsclosely with the most commonly occurring refractiveerror in the general population found by many otherinvestigators.' The distributions of refractive errors
for all cataract patients and controls both at the timeof first cataract presentation and four years previouslyare shown in Figs. 5a, b, c, d. It will be seen that therewas very close agreement between the two samples atfour years prior to cataract presentation. Althoughthe distribution of refractive errors departed slightlyfrom normality (ie., a leptokurtosis with slightskewness towards myopia), this was not sufficient in
the present samples to invalidate the use of para-metric variance analyses.However, the small sample size and related high
variance of some of the cataract categories (notablyC) precludes a useful analysis of the data as presentedin Table 3. For example, the negative mean refractionof the subcapsular group (C) at both examinationtimes is due almost entirely to the occurrence of onepatient with bilateral high myopia as detailed in
the footnote to Table 3. Nevertheless, all analysespresented in this paper include this myopic case,
Table 3 Mean refraction (spherical equivalent in dioptres) among the different cataract categories*
Fouryears preceding At 'cataract' presentation Refractive changepresentation
CataractGroup RE LE RE LE RE LE
A x 0-975 1-102 -0-750 -(0-523 -1-725 -1-625sd 2-071 1-904 2-391 2-404 0(914 1-169
B x 0-277 0(405 -1-121 -0-832 -1-398 -1-237sd 2-690 2-760 2-977 2-938 1-086 0)841
C§ kx -1-886 -1-179 -1-705 1-036 0-182 0(143sd 4-568 3-686 4-365 3-602 0(459 0-373
D x 0-639 0-723 0X-859 0-937 0-220) 0(215sd 199(9 1-794 1-975 1-826 (0-416 ()-438
Controls x 0-902 0-717 1-05() t)-850 (0-147 0-133sd 2-184 2-359 2-255 2-360 0-392 1)395
* For definition of cataract group see Fig 2.t The computed mean values and standard deviations for 'refractive change' (ic., 'presentation' minus 'prior') are based on individualdifferences for all patients. Consequently, where the mean 'refractive change' does not exactly correspond with the difference between themeans for 'presentation' and 'prior' refractive states this is a result of variance in the data.f For details of the number of eyes in each group see Table 1, where x = mean and SD = standard deviation.§ If one high myopic case (R-1 1-625, L-1 1-()() at four years preceding cataract and R - I I *00, R- 10-625 at the presentation of cataract) isexcluded from this group, the mean refractions and corresponding SD values for group C revise to: x: (I) R -0-739, L -0)423 (SD: 2-989,2-409); (11) R -0-573, L 0-298 (SD 3-197, 2-462); (111) R +0- 167, L +() 125 (SD 0-441,(-382).
408
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
Cataract: the relation between myopia and cataract morphology
Number ofpat i e nts
30
28
26
24-
22
20 -
18 -
16 -
14 -
1 2 -
10 -
8-
6
4-
2-
O-
Number ofpatients
C ATA RACT at 4 yrs priorto presentation
m-F ThC) COCD CD CD Co CD4C CO
cQC; 00 %d vO C CD CQqO- , , , , + + +
Spherical Equivalent Refraction ( dioptres)Fig. Sa
Fig. 5 Distribution ofrefractive errors for-1 Ocataractpatients (a) four years prior to thepresentation ofcataractand (b) at the time ofinitial cataractpresentation;compared with the distribution ofrefractive errorsfor 110age matched controls (c)four years prior to presentation and(d) at time ofpresentation for a refractive examination. Righteye data. *
since it did not exceed the exclusion criteria estab-lished at the outset of the study. Consequently, to testthe hypothesis that nuclear cataract is associated witha myopic shift over time, the cataract data wereregrouped into two categories at presentationcomprising all those eyes possessing nuclear cataractversus all eyes without nuclear cataract. The meanrefractions for these regrouped data are shown inTable 4. The analysis of variance for right eye data issummarised in Table 5. It shows a highly significantdifferent change of refraction over four years in thenuclear compared with non nuclear cataract groupsand controls. This interaction term is due to arelatively large mean myopic change in the presenceof nuclear cataract (R -1-47 D, L -1-34 D), whereasthere is a slight hypermetropic change both in the
3028 -
26 -
24 -
22 -
20 -
1 8 -
16 -
14 -
1 2 -
1 0 -
8-
6-
4-
2-
O-4
SphericalFig. 5b
CATARACT at "Presentation"
6 od , m oj CD c-, -t
, I + + +
Equivalent Refraction ( dioptres)
non-nuclear cataract group and in controls. Apost-hoc Newman-Keuls test shows the change inrefraction over four years in each of the three groups(i.e., nuclear cataract, non-nuclear cataract, andcontrol) to be highly significant, as also were thedifferences in mean refraction between cataractcategories and controls at each examination time(p <0.01). (The differences between mean refractionsat four years prior to cataract presentation becomeinsignificant if the single case of high myopia isremoved. For details of this case see footnote toTable 3.) The distribution of the change in refractiveerror over time for the nuclear and non-nuclearcataract groups is shown in Figs. 6 a, b.To test the hypothesis that the myopic shift occur-
ring in nuclear cataract is independent of the initialametropic state the data were structured for furtheranalysis according to whether an eye was myopic orhypermetropic at four years prior to cataract presen-tation. Separate analyses of variance on right and lefteye data were conducted on the change in refractiveerror occurring over the four-year interval betweenexaminations. A summary of the variance analysisfor right eye data is given in Table 6, from which it
. . . . . . . . . . . . . .ITr
409
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
NA P Brown, andA RHill
Number ofpatients
30 -
28 -
26 -
24 -
22 -
20 -
18 -
16 -
14 -
12 -
10 -
8-
6-
4-
2
0-
CONTROLS at 4 yrs priorto presentation
Number ofpat e n t s
30
28
26
24
22
20
18
16
14
12
10
8
6
4
2
0 r
CONTROLS at "Presentation"
I
Ii 14ii i ___--4--q--Il
CD ) CD
CMI I I I + + +
+ + +
Spherical Equivalent Refraction (dioptres)Fig. 5c
will be seen that there was neither a significantinteraction of refractive change between ametropiaand cataract type, nor was there a significant maineffect due to ametropic state. This implies that themean refraction for the sample of myopes and thesample of hypermetropes did not differ between thecataract group and the controls. The data were
examined further to determine whether there was a
greater proportion of myopes than of non-myopes in
Spherical Equivalent Refraction (dioptres)Fig. 5d
the cataract group at four years prior to presentation.Table 7 shows there was no difference between thecataract group and controls in the proportion ofmyopes to non-myopes. A X' test gives the probabilityassociated with these proportions being the same
in each group as p>08, (X2 RE=0-028, and X2
LE=0-058, each with df= 1). The myopic shiftobserved in nuclear cataract was therefore inde-pendent of whether an eye started out as beingrefractively myopic or hypermetropic.
Analyses of variance conducted on the data when
Table 4 Mean refraction error (spherical equivalent in dioptres) for eyes with and without nuclear cataract
(I) (11) (111)Fouryears preceding At 'cataract' presentation Refractive change t (11- 1)presentation
CataractGroup* RE LE RE LE RE LE
(A+B) x 0-439 0-597 -1-035 -0-747 -1.474 -1-344nuclear sd 2-554 2-549 2-828 2-775 1-048 0-943cataract(C+D)non- x 0-168 0(279 0(381 (0477 0-213 0-198nuclear sd 2-745 2-471 2-731 2-472 0(421 (-422cataractControls x 0902 0-717 1 05( 0-85( 0- 147 0 133
sd 2-1X4 2-359 2-255 2.36(0 (1392 0-395
* and t see footnotes to Table 3.
410
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
Cataract: the relation between myopia and cataract morphology
Table 5 Summary analysis of variance ofrefractive error asaJunction ofexamination time (presentation versus Jouryears prior) and cataract group (nuclear versus non-nuclearversus controls). Right eye data*
Source of variation SS DF F p
Cataract group (C) 110-36 2 4 58 0(0113Error 2517-08 209Examinationtime(T) 1257 1 71 85 <0(0001C x T 46 41 2 132 60 <0(0001Error 36 58 209
* Anova for left cyc shows similar results with a comparabledistribution of variances.
grouped according to the patients' sex showed thereto be no difference in the refractive change in thenuclear and non-nuclear cataract groups for malescompared with females.
Discussion
The application of the findings of this study, may belimited by the restrictive nature of the sampling,which has been confined to a group of CaucasianBritish patients attending a central London practice.However, this is a good place in which to make astudy of the relationship of simple myopia to cataract
Nuclear * and non-nuclear0 cataract
Refractive change in 0.50D categories
Fig. 6 Refractive change overfouryears ofeyes with (a)nuclear cataract and non-nuclear cataract and (b) controls(right eve data).
Table 6 Summary analysis ofvariance offour-year changein refraction as afunction ofinitial ametropic state (myopiaversus hypermetropia) and cataract group (nuclear versusnon-nuclear versus controls). Right eve data*
Source of variation Ss DF F p
Amctropia (A) 0(1691 1 0(49 0(4845Cataractgroup(C) 87 240)5 2 126-53 <0(0)001AxC 1 4768 2 2 14 0(1201Error 71 0185 2t)6
* Anova for Icft cyc shows similar results with a comparabledistribution of variances.
since environmental factors in the causation ofcataract are minimal.The finding of an excess incidence of cataract in
the female is similar to that found by Perkins.3 It isinteresting that the same ratio of female to maleoccurs in the controls. Although the study deals withage groups in which females predominate, since thesex ratio is the same in the cataract group and in thecontrols it cannot be stated that the female is moreprone to cataract.The present study differs from previous studies in
that the refractive state of eyes were obtained at thetime offirst presentation with cataract and comparedwith the refractive state of these same eyes before the
Number ofs u b j ec t s
68 -
6466hI-
R6
24-
22-
20-18-16-14-12-10
8-
6-
4-
2- ~'I-5 -4 3 -2 1 0 +1I
R ef rac t ive cha nge i n .50D categories+2
Fig. 6b
Number ofs u b j ec t s
26 -
24 -
22 -
20 -
18-
1 6 -
14
1 2 -
1 0 -
8-
6-
4-
20
-5
Fig. 6a
41
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
NA P Brown, andA R Hill
Table 7 Frequency ofpatients having myopia and thosewithout myopia (ie., emmetropia and hypermetropia) atfouryears prior to presentation, for the cataract group and thecontrols. Right eye data
Right eye Left eye
Cataract Controls Cataract Controlsgroup group
Myopes 29 30 26 27Non-myopcs 73 80 74 83Ratio myopes/non-myopcs 0-397 0-375 0-351 0.325
development of cataract. The cataracts were seen atthe time of their first presentation. They can there-fore be presumed to be earlier in their natural historythan would be the case in those patients beingexamined at hospital after referral with cataract, ashave been considered in other studies.A tendency to myopia was confirmed at the time of
diagnosis of cataract, which corroborates the work ofWeale,2 Perkins,3 Von Kluxen.4 In particular, it isshown that a marked myopic shift (Fig. 5) hadoccurred in the four years preceding the presentationof cataract only in those eyes with nuclear cataract.Furthermore, there is no evidence in the data that themyopic shift is any different among eyes which weremyopic or hypermetropic before the presentationwith cataract. From these results it is possible tospeculate that the increased prevalence of myopiaamong eyes with cataract is entirely due to thecataract and did not precede it. This is furthersubstantiated by the extremely close agreement ofmean refractive error between the cataract group andcontrols at the four-year stage preceding cataractpresentation.When the mean refractions for both ophthalmic
examinations for the cataracts and the controls areplotted graphically (Fig. 7), it can be seen that theyrepresent two diverging groups of individuals.By the application of Darwinian theory9 it can be
suggested that each group has evolved from onecommon group of individuals, which is shown in thegraph by the extrapolated dotted line. It is reasonableto conclude, therefore, that simple myopia does notpredispose to cataract, but is the product of cataractswhich include the element of nuclear sclerosis.There is also a suggestion in the data that the
combination of nuclear and subcapsular cataract(group A) produces the largest refractive change, (R-1-725 D, L -1-625 D in four years; Table 4).Although this is not significantly different from theeffects of nuclear cataract alone, it has been notedpreviously"' that lenses with nuclear sclerosis andsubcapsular cataract are liable to have a thinned
cortex, with reduced radius of curvature of theanterior surface, so that a greater change in thisgroup may be explained by the combination ofrefractive index change (nuclear) and curvaturechange (cortical).The relation of hypermetropia to cataract has been
considered by Bourdon-Cooper," who observed thatcataract was more common in ametropia, especiallyin hypermetropia. The contrary was reported by VonKluxen,4 who found cataract to be common inmyopia and emmetropia but rare in hypermetropia.In the present study, which used a random samplingprocedure for the inclusion of all eligible patients atthe time of first presentation with cataract, there wasno evidence from the refractions of four yearspreviously (when cataract was not present) thatmyopia or hypermetropia were more prevalent thanamong a sample of age matched non cataractouscontrols. Hence, excluding the special condition ofthe degenerative myopias in excess of -10-00 D, a
CHANGE IN REFRACTION OVER 4 YEARS FOR CATARACTSWITH AND WITHOUT NUCLEAR SCLEROSISCOMPARED WITH CONTROLS
RIGHTEYE
Presentationof cataract -
Yearsprior tocataract 4presentation
8-
Non-Nuclear nuclear
-2.0
Controls
I0+.I I
-1.0 0 +1.0 +2.0Refractive change (dioptres)
Horizontal bars indicate ± 1 SEMNote: the values for the non-nuclear cataracts are the corrected
means following the removal of the high myopic caseFig. 7 The change in refraction with timefor eyes withnuclear cataract and non-cataractous eyes (right eye data).The broken line is extrapolated to aproposed common meanrefractive status prior to the onset ofcataractous changes,which, it is suggested, occurat aboutsix years before theclinical appearance ofa cataract by slit-lamp examination.The horizontal bars indicate ± I standard error ofthe mean.The mean valuesfor the non-nuclear cataracts exclude thecase ofhigh myopia (seefootnote to Table 4).
412
I
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
Cataract: the relation between myopia and cataract morphology
refractively myopic eye is at no greater risk ofdeveloping cataract than one with hypermetropia.
It has been suggested that stress induced in the lensfibres by the change in the shape of the lens onaccommodation is a cause of cataract. Bourden-Cooper" suggested that the greater need to accom-modate by the hypermetropic eye might be causative.The theory of accommodative cause can alternativelybe applied to account for a greater incidence ofcataract in myopia. Weale quoted Fisher's work')on lens fibre stress to show that the latently accom-modated lens of the hypermetrope would be relaxed,whereas in the myopic eye the lens would be stressedby a continually unrelaxed zonule.The refractive change through life was studied in
detail by Slataper, who showed that a hypermetropicchange was normal up to the age of 64, after whichrefraction levelled out and then changed in thedirection of myopia. His series of subjects did notexclude those developing cataract. Since cataractbecomes very prevalent after the age of 60,'- '8Slataper's subjects would have included a high pro-portion of cataract patients in the older age groups.Indeed Slataper himself considered that the myopicchange which he recorded in old age was due tocataract, a deduction which is confirmed by thepresent study. When cases with cataract are excluded,it is seen that a continuing hypermetropic refractivechange is found in the healthy eye in old age (Table 3and Fig. 5). The finding of a myopic refractive changein a seemingly healthy eye in a middle aged orolder person should therefore be considered as anindication of impending cataract.The incidence of the different types of cataract-
cortical, nuclear, and subcapsular (Table 1 and Fig.4) - appears similar to that observed by Foster andBenson" in patients presenting with reduced visualacuity due to cataract at a hospital in Leeds. Directcomparisons cannot be made because they classifiedmixed types of opacities separately and did not relatethe incidence to age. In the present- study it isnoteworthy that subcapsular cataract is the first toappear, presenting in the 40-44 year age group, sinceit is in the younger age groups that the ophthal-mologist is most often asked to determine whether acataract is spontaneous or due to exposure to drugs,irradiation, or other cause. Thus the identification ofa cataract as subcapsular is not in itself evidence of aprobable external cause. Perkins recorded a higherincidence of subcapsular cataract at 40% comparedwith 24% in the present study. The difference can beaccounted for by his patients having more advancedcataract than those in the present study. A patientpresenting with cortical or nuclear cataract will oftendevelop subcapsular cataract later, which will bringthem to hospital because of its more disabling effect
on visual acuity. The reported incidence of sub-capsular cataract is still lower in other series: 6% inFoster and Benson's series,'9 10% in Kirby's series,'and only 1-8% in Chatterjee's series."
Conclusion
This study shows that simple myopia does not appearto predispose to cataract. It is the development of thecataract itself, in particular nuclear sclerosis, whichcauses the refractive change towards myopia. Themyopic change precedes the development of recog-nisable cataract, and it can be shown by usingBayesian statistics22 that the probability of a personover the age of 55 having nuclear sclerosis, given arefractive change of at least -1-00 D over four years,is 0-99. The healthy aging eye continues to show agradual hypermetropic change.
We are grateful to Dr B C Reeves for computing assistance.
References
I Duke-Elder S. System of ophthalmology. London: Kimpton,197(); 11:225.
2 Weale R. A note on a possible relation between refraction and adisposition for senile nuclear cataract. Br J Ophthalmol 1980;64:311-4.
3 Perkins ES. Cataract: refractive error, diabetes, andmorphology. Br J Ophthalmol 1984; 68: 293-7.
4 Von Kluxen G. Klinische und experimentelle Untersuchungenan Alterskatarakten. Fortschr Med 1985; 103: 243-6.
5 Racz P. Koszoras L, Ordogh M. Investigations on bilateralpresenile cataracts. Lens Res 1984; 2: 13-21.
6 Rosner B. Statistical methods in ophthalmology: an adjustmentfor the intraclass correlation between eyes. Biometrics 1982; 38:1t)5.
7 Ray WA, O'Day DM. Statistical analysis of multi-eye data inophthalmic research. Invest Ophthalmol Vis Sci 1985: 26:1 186-8.
8 Duke-Elder S. System of ophthalmology. London: Kimpton,197t); 5: 234.
9 Darwin C. The origin of species by means of natural selection.London: Murray, 1859.
1t) Brown N, Tripathi R. Loss of the anterior subcapsular clear zoneof the lens. Prognostic significance in cataract formation. TransOphthalmol Soc UK 1974; 94: 29-45.
11 Bourdon-Cooper J. Aetiology of cataract. Br J Ophthalmol1922; 6: 385-412.
12 Fisher RF. Senile cataract: a comparative study between lensfibres stress and cuneiform opacity formation. Trans OphthalmolSoc UK 1970; 90: 93-1t)9.
13 Fisher RF. In: The human lens in relation to cataract. CibaFoundation symposium No. 19. Amsterdam: AssociatedScientific Publishers, 1973: 307-8.
14 Slataper FH. Age norms of refraction and vision. Arch Ophthal-mnol 1950; 43: 466- 81.
15 Gradle H. Study of lenticular change with age. Ophthalmic Sci1926; 62:255.
16 Fisher FP. Ueber Altersveranderungen des Auges. Ophthal-mnologica 1941; 102: 226-32.
17 Shafer RN, Rosenthal G. Comparison of cataract incidence innormal and glaucomatous populations. Am J Ophthalmol 1970;69: 368-70.
18 Gibson JM, Rosenthal AR, Lavery J. A study of the prevalence
413
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from
414 NA P Brown, andA R Hill
of eye disease in the elderly in an English community. Trans 21 Chattcrjec A, Milton RC, Thylc S. Prevalence and aetiology ofOphthalhnol Soc UK 1985; 104: 196-20)3. cataract in Punjah. BrJ Ophthalmnol 1982; 66: 35-42.
19 Foster J, Benson J. The percentage incidence and surgical 22 Aspinall PA, Hill AR. Clinical inferences and decisions- 1.significance of the different forms of senilc cataract. Trans Diagnosis and Bayes' theorem. Ophthalmic PhYssiol OptOphthalmol Soc UK 1934; 54: 127-36. 1983; 3: 295-304.
20 Kirby DB. Pathogenesis of senile cataract. Arch Ophthalmol1932; 8: 96-119. Accepted for publication 25 June 1986
on February 15, 2020 by guest. P
rotected by copyright.http://bjo.bm
j.com/
Br J O
phthalmol: first published as 10.1136/bjo.71.6.405 on 1 June 1987. D
ownloaded from