Vascular Complications of Central Venous Catheter Placement_ ...
Care and Maintenance of Central Venous Catheter Devices guidelines... · Care and Maintenance of...
Transcript of Care and Maintenance of Central Venous Catheter Devices guidelines... · Care and Maintenance of...
Care and Maintenance of Central Venous Catheter Devices
Printed by The Living Trust
Developed – September 2008 Review date – September 2011
2
CONTENTS PAGE Introduction and Rationale for Guideline Development 3 CHAPTER 1: OVERVIEW OF VASCULAR ACCESS DEVICES 1.1 Peripheral Catheters 5 1.2 Peripherally Inserted Central Catheters 8 1.3 Central Venous Catheters 12 1.4 Tunnelled CVC’s 15 1.5 Dialysis CVC’s 21 1.6 Totally Implantable Ports 23 CHAPTER 2: SELECTION OF CATHETER INSERTION SITE 27 CHAPTER 3: EDUCATION AND TRAINING 28 CHAPTER 4: DEVICE SELECTION 29 CHAPTER 5: INFECTION PREVENTION IN CVC’S 31 CHAPTER 6: CUTANEOUS ANTISEPSIS 36 CHAPTER 7: CATHETER OBSTRUCTION 38 CHAPTER 8: DRESSING SELECTION 47 CHAPTER 9: BLOOD SAMPLING 52 CHAPTER 10: REPLACEMENT OF IV ADMINISTRATION SETS / HUB 53 CHAPTER 11: ASEPTIC TECHNIQUE 55 CHAPTER 12: POWER INJECTION (CONTRAST ADMINISTRATION 56 REFERENCES 57
3
ACKNOWLEDGEMENTS This document was developed by the Vascular Access Service (NHS Greater
Glasgow and Clyde):
Linda Kelly Lead Nurse
Esther Buchan Specialist Nurse
Ann Brown Specialist Nurse
Leanne Criggie Specialist Nurse
This document has been reviewed by senior nurses across NHS GG&C and various
groups and forums across Scotland for an extensive peer review. These groups
included the Scottish Intravenous Access Network (SIVAN) and the West of Scotland
Cancer Nurses Group (WOSCAN).
The final document incorporates the comments of the reviewers.
4
INTRODUCTION AND RATIONALE FOR GUIDELINE DEVELOPMENT CVAD’s are inserted directly or in directly into the superior vena cava or right atrium.
Indications for the use of CVAD‘s include drug and fluid administration, nutrition,
antibiotic therapy, chemotherapy, bone marrow transplantation and renal dialysis.
CVAD‘s are inserted by medical or nursing staff, in theatre areas, radiology
departments, designated clinical areas or at the bedside (Woodrow, 2002).
According to Elliott et al. (1994) there are approximately 200,000 catheters inserted
annually in the UK. Infections are the most serious complication that can result from
the presence and use of a CVAD. The rates for central venous catheter related
bacteraemia (also referred to as catheter – related blood stream infection, or CRBSI)
are 2.1 – 30.2 cases per 1000 catheter – days (Humar et al. 2000). Twenty – five
percent of all hospitalised patients who have standard, non coated central venous
catheters in place for eight days or more will develop colonization at the catheter site,
and 5% of those patients will develop a CRBSI (Saint, 2001). Of the estimated
250,000 children and adults who will develop a CRBSI each year, approximately 12%
to 25% of these patients will die. An additional cost per infection will be lost due to
the extensive treatment and health – care management required (Raad & Hanna
2002). There are therefore, substantial costs associated with the morbidity, mortality,
extended length of hospital stay, and treatment required secondary to central venous
catheter related bacteraemia. Freeman (1990) and Cicalini et al. (2004) agree that
CRBSI’s result in significant morbidity, increased duration of hospitalisation and
increased medical costs.
5
Intravenous therapy is a major component in health care, and appropriate research –
based knowledge is essential to ensure positive patient outcomes. Many changes in
intravenous care have occurred in the last decade and due to these changes current
practice has been affected. To ensure best practice within NHSGG&C this literature
review and subsequent guideline was developed to meet the professional
responsibility of educating healthcare workers about the changes in care. The aim of
these guidelines is to minimise the risk of CRBSI’s and other complications, and to
standardise practice across NHSGG&C. By applying best practice, the rate of CVAD
complications might be reduced with benefits to patients.
A section relating to peripheral catheters has also been included to complete the range
of VAD’s (Vascular Access Devices) available.
Nutrition, renal and paediatric medicine
*These specialities have specific guidelines that should be referred to and used in
conjunction with this document.
6
CHAPTER 1 - OVERVIEW OF VASCULAR ACCESS DEVICES 1.1 PERIPHERAL CATHETERS
Peripheral catheters are the most commonly inserted catheters with the numbers being
inserted annually in the United Kingdom being too great to quantify. Waghorn (1994)
estimated that in a 500 bedded district general hospital, 18,000 peripheral catheters
were inserted in a single year.
1.1.2 Indications
Peripheral catheters are used for treatments including IV administration,
administration of antibiotics and administration of certain cytotoxic drugs.
1.1.3 Contraindications
They are contraindicated for long - term treatment, certain cytotoxic drugs, total
parenteral nutrition (TPN) and medications with a PH of less than 5 or greater than 9.
7
1.1.4 Insertion
Peripheral cannulation is a procedure that many nurses are now performing regularly
and routinely as part of their role. Training and competences must be kept up to date.
∞ Collect all necessary equipment include correct catheter size for purpose
∞ Confirm patients identity and explain the procedure
∞ Perform hand washing technique
∞ Cleanse skin for at least 30 seconds with an alcohol impregnated wipe and
allow to dry
∞ Wear clean gloves
∞ Position patient and select most appropriate site
∞ Facilitate accurate insertion
(ICNA, 2001)
1.1.5 Potential complications
Potential complications of peripheral IV therapy include disconnection, dislodgement,
infiltration, extravassation and phlebitis. Inadequate fixation of peripheral cannula
contributes to the occurrence of these complications (Wood, 1997). Optimal
securement of the device is therefore a key nursing consideration (Callaghan et al,
2002). In the past cannulas, were often secured with non - sterile tape and gauze, this
practice is no longer satisfactory as peripheral cannulae provide a direct route into the
patients blood stream breaching the body’s defences and is therefore a potential route
of contamination. In a study performed by Oldman (1991) it was found that the use of
non-sterile adhesive tape resulted in bacterial contamination.
1.1.6 Implications for practice
∞ The selection of a peripheral catheter should be dependent on the length of
therapy, type of medication, the patients’ condition and preference (Hamilton
and Ferno 1998; Dolan and Doughery 2000; Hamilton 2000; ICNA 2000). If
treatment is required for more than 3 weeks, consider alternative device
selection.
∞ Use a transparent dressing to allow continual visualisation of site (Kiernan,
1997, Fuller and Winn, 1999).
∞ Change dressing if moist or no longer intact (ICNA 2001; RCN 2006)
8
∞ Cannula should be replaced every 72 – 96 hours, or sooner if complications
are suspected (Bregenzer 1999; Holmer and Holmes 1998; Carlson 2001; Frey
2001; CDC 2002)
∞ A peripheral catheter inserted in an emergency situation where aseptic
technique has been compromised should be replaced within 24 hours (RCN,
2006).
∞ Remove as soon as possible if no longer required.
9
1.2.1 PERIPHERALLY INSERTED CENTRAL CATHETER - PICC
PICC’s are frequently used to obtain central venous access for patients in seconary
and primary care. PICC’s are a reliable alternative to short - term central venous
catheters, with a lower risk of complications. They first gained popularity in the
1980’s, and their use has continued to grow steadily since then. The reason they have
grown in popularity is because of their reduction in potential complications and cost
compared to short - term central venous catheters, and because PICC’s can be inserted
by registered nurses who have been trained in the procedure.
A vein in the arm is the most common point of insertion with the distal tip of the
catheter terminating in the superior vena cava or proximal right atrium. These
catheters can be inserted for treatment that is required for 3 weeks to 6 months.
1.2.2 Indications for use
As well as the delivery of antibiotic therapy, IV fluids, TPN, Blood sampling and the
administration of irritants / vesicants, PICC’s have become an important venous
access device for patients receiving chemotherapy (Bunting, Slaughter, Masel et al.
2000). This is largely due to the fact that inpatient stays are greatly reduced if
treatment is delivered in the community instead of peripherally in the ward area.
1.2.3 Advantages of PICC’s
∞ Preserves venous access
∞ One cannula only
∞ Easy to insert
∞ Less skin flora (than Hickman line site)
∞ Fewer complications on insertion
10
∞ Allows rapid haemodilution of thrombophlebogenic agents reducing the risk
of venous intimal damage, and thus reducing the potential for thrombosis
formation and thrombophlebitis.
1.2.4 Disadvantages
∞ Not always suitable for blood transfusion / sampling
∞ Migration possible if not adequately secured.
1.2.5 Insertion technique
A clear understanding of vascular anatomy and certain principles of physiology are
important, as these catheters are threaded many inches into the veins. The ability to
apply this knowledge to a patient is important in successful placement.
The PICC line is inserted using a strict aseptic technique. Topical or local anaesthesia
is used at insertion site. The patient then lies in the supine position with the arm
positioned at a right angle to the trunk.
The skin is cleaned using a single patient use application of alcoholic chlorhexidine
2% gluconate in 70% alcohol, and the area draped with sterile towels. The operator
dons a sterile gown and gloves. When the prepared area is dry, venous access is
obtained using an introducer needle. Once the vein is cannulated and good blood flow
obtained, the catheter is advanced through the cannula to the desired point using depth
markings on the catheter guide. Catheter placement within a vein is confirmed by
aspirating blood and irrigating with normal saline before the guidewire is removed.
The PICC is secured using a securing device and a transparent dressing. A chest x-ray
is then performed to confirm the position of the catheter tip.
1.2.6. Mid line catheter
A soft flexible tube made from silicone or polyurethane that is inserted using the same
technique as the PICC. They provide venous access in a large peripheral vein
extending up to 20 cms. Midline catheters do not enter the central venous system.
Midline catheters are used for therapy of moderate duration. They are neither cuffed
nor sutured and are held in place by a transparent dressing.
11
1.2.7 Ultrasound guidance (USG) for PICC placement
Ultrasound imaging has been found to greatly assist vascular access, in particular the
insertion of peripherally inserted central catheters. USG has been shown to increase
success rates and avoid associated complications such as thrombosis and stenosis
(Moureau, 2003). Real-time ultrasound studies have reported a greater percentage of
successful cannulations, fewer venepuncture attempts and a decreased time required
for cannulation (Slama, Novara, Safavian et al.1996 and Rothschild, 2001).
Several studies have now been carried out to determine the need for USG in placing
PICC’s. A recent study by Bunting et al. (2000) concluded that the success rate of
USG PICC insertion is extremely high, in particular with patients who have very poor
peripheral venous access. In this study there was a 100% success rate with the use of
ultrasound guidance. A further study by Moureau (2003) found that successful PICC
insertion increased to over 90% with the use of USG in comparison to 80% with
traditional non-ultrasound PICC insertion.
Therefore, as concluded from the research, PICC insertion is greatly aided by the use
of ultrasound guidance. The National Institute for Clinical Excellence (2002) further
reiterates this by stating, “The use of two-dimensional (2-D) imaging ultrasound
guidance should be considered in most clinical circumstances where CVC insertion is
necessary either electively or in an emergency situation”.
As the use of ultrasound guidance to place central venous catheters requires a
competent and experienced operator (Bunting et al, 2000), training for all nurse
specialists is paramount. Current guidelines state “It is recommended that all those
involved in placing CVC’s using two-dimensional (2-D) imaging ultrasound guidance
should undertake appropriate training to achieve competence” (National Institute for
Clinical Excellence, 2002).
1.2.8 PiCC line removal
Universal precautions must be maintained to avoid contamination of the health care worker
through exposure of blood bourne pathogens.
12
PiCC lines can be removed by registered nursing staff who have undergone training and are
competent in the procedure.
Procedure
Don sterile gloves
Remove dressing from bottom upward
Clean site using 2 % chlorhexidine gluconate in 70% isopropyl alcohol
Place swab at exit site
Gently withdraw catheter
Apply pressure to exit site for 5 minutes
Tip may be sent for sensitivity and culture if infection is suspected
Apply mepore dressing
13
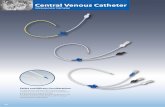
1.3. CENTRAL VENOUS CATHETERS
A central venous line is a catheter which is placed directly via of one of the large
veins of the body (jugular, subclavian or femoral) and whose tip lies in one of the
central veins (superior vena cava or inferior vena cava). These lines can have up to
five lumens and are held in place by a suture or catheter securement device. They are
commonly used for the measurement of central venous pressure, the administration of
fluids and /or toxic drugs, in patients who have limited peripheral access and for
short-term haemodialysis (Hocking, 2000).
1.3.1 Advantages
The advantages of central venous lines are that they can be inserted relatively easily
and quickly and used immediately once tip position has been ascertained. As they can
also be used for several therapies at the same time and can be used for critically ill
patients this makes them highly advantageous. These lines can be placed in a variety
of settings and can be placed by most senior medics making their use relatively
common (Dougherty, 2006). Another advantage of the central venous line is their use
for blood sampling, thus decreasing venepuncture cannulations.
1.3.2 Disadvantages
There are many disadvantages in the use of the central venous line. There are many
complications associated with their insertion including, pneumothorax/haemothorax,
arterial injury and haemorrhage, infection, air embolism and thrombosis. The use of
central venous lines in emergency situations for the treatment of critically unwell
patients further exposes patients to these complications (Dougherty, 2006).
14
Central venous lines should only be used as a temporary measure due to the high rates
of infection associated with these devices (Centers for Disease, Control and
Prevention, 2002). Some research suggests the routine replacement of these catheters
should take place in order to reduce incidence of infection (Centers for Disease,
Control and Prevention, 2002). However, statistics show that routine replacement of
central venous lines does not significantly reduce the incidence of infection (Centers
for Disease, Control and Prevention, 2002). Therefore, these lines should only be used
as a temporary measure for a short duration.
1.3.3 Insertion of Central Venous Lines
Insertion of central venous lines is commonly undertaken by medical practitioners,
although specialist nurse-led units are now developing key roles in the insertion of
these devices (Dougherty, 2006). Research shows, however, that these catheters
should be placed by experienced operators who have been appropriately trained in the
procedure (British Committee for Standards in Haematology (BCSH), 2006).
There are several different methods of central venous line placement, however, in all
cases the vein of choice is directly punctured and the skin entry site dilated to allow
easy insertion of the device. Research shows that in all cases of insertion, the use of
ultrasound is beneficial, decreasing the risk of complications on insertion (BCSH,
2006).
Following insertion of the central venous line the catheter should be anchored using a
skin suture or securement device (Dougherty, 2006). The patient should then have a
check chest x-ray prior to use to ensure that the catheter tip is in satisfactory position
(Dougherty, 2006).
15
1.3.4 Care of Central Venous Lines
The care of central venous lines should always be carried out using a strict aseptic
technique. In order to maintain patency of the catheters lumens should be flushed
before and after use (Moureau, 2004). There is still some debate as to whether central
venous line lumens should be locked with heparin. The research is inconclusive;
therefore, we would recommend adhering to your local policy regarding this matter.
In order to prevent infection dressings should also be changed every seven days or
sooner if no longer intact or soiled. A transparent dressing should be used to allow
visual inspection of insertion site (Scales, 1999).
1.3.5 Removal of Central Venous Lines
Although removal of central venous lines is fairly straightforward, complications can
still occur. The main risk is that of air embolus. Once the sutures or securement
device has been removed, the patient should be placed in a 30% head down tilt while
and after the catheter is removed, thus decreasing the risk of air embolus. A bioclusive
dressing should then cover the site for at least 24 hours (Scales, 1999).
Removal should be performed using strict aseptic technique as the risk of
contamination is present until the site is fully healed.
1.3.6 Recommendations for Practice
∞ Central Venous Lines should be for short-term use only
∞ Central Venous Lines should be placed and cared for using an aseptic
technique
∞ Central Venous Lines should never be used without confirming line tip on a
chest x-ray
∞ Central Venous Lines should be flushed before and after each use
16
1.4 TUNNELLED CENTRAL VENOUS CATHETERS
Hickman type catheter
1.4.1 Description A soft, flexible tube made from various materials including silicone and polyurethane.
It is inserted via the large veins of the neck or chest (jugular and subclavian using a
guide wire Seldinger technique). The femoral vein should be avoided. The tip rests
in the lower third of the superior vena cava or the upper right atrium. It is tunnelled
subcutaneously and many are equipped with a fibrous (Dacron) cuff, which sits in the
skin tunnel. This enables the patient's tissue to bond with the line, to create a secure
fix, and will act as a mechanical barrier to prevent infection traversing the line. They
are usually sutured or secured in place for three to six weeks until the bonding process
is complete. These lines may be open-ended or valved and are available in single,
dual or triple lumen. They are available in various gauges the most commonly used
being 6.6 French to 14 French.
1.4.2 Indications
There are many indications for tunnelled central venous access including:
∞ Poor venous access - this may have a variety of causes, including drug abuse
and obesity.
∞ Irritating agents - many drugs are caustic and can irritate veins, which may
lead to clotting and inflammation. Infusates with an osmolarity greater than
280-300 mOsm require dilution within a central vein.
∞ Prolonged intravenous therapy, such as chemotherapy and antibiotics.
∞ Dialysis, either for acute renal failure or while awaiting permanent access.
17
∞ Plasmaphereis.
∞ Conditions requiring multiple punctures, such as daily blood withdrawals in
patients with coagulopathy.
∞ Total parenteral nutrition.
1.4.3 Advantages
∞ More comfortable and discreet than the non – tunnelled catheters.
∞ Can remain insitu for over 2 years.
∞ Patients can be nursed at home with these devices in place.
1.4.4 Disadvantages
∞ Requires a minimally invasive surgical procedure for placement.
∞ Potential complications on insertion
.
1.4.5 Insertion Technique
The procedure of tunnelled central venous catheter insertion is a minimally
invasive surgical procedure that carries risks of complication. These complications
can be serious or potentially fatal (Hamilton, 2006; McGee and Gould, 2003;
Polderman and Girbe, 2002). Complications include; pneumothorax,
haemothorax, haemorrhage, carotid puncture, air embolism and infection (Maklin
and Chernecky, 2004)
∞ The procedure should take place in a clean environment (Theatre, radiology
suite or dedicated treatment room). Bedside placements should only be
performed in emergencies.
∞ Experienced operators should perform catheter insertions and supervision and
assessment programs should be in place.
∞ Ultrasound guidance is recommended for all central venous access insertions
(NICE, 2002)
∞ Imaging facilities (fluoroscopy) should be available for tunnelled catheter
insertion (BCSH guidelines, 2006).
18
∞ Maximum sterile barrier precautions should be used for catheter insertion
including: gown, sterile gloves, hat and mask (Mermel et al, 1991)
∞ Clean site using 2 % chlorhexidine gluconate in 70% isopropyl alcohol and allow to
dry.
∞ A large sterile drape should be used to completely cover the patient.
∞ Procedure should be performed using a strict aseptic technique and following
the local standard operating procedure.
∞ The patient should be monitored throughout (blood pressure, pulse, oxygen
saturation).
∞ Tip placement should be checked by performing a chest x-ray.
∞ The procedure should be document in the patients’ notes.
∞ Paediatric specialists should insert catheters in children.
∞ Sedation or general anaesthesia should be used where appropriate.
1.4.6 Post procedure care
∞ Do not used catheter until x-ray checked and deemed satisfactory
∞ Change dressing after 24 hours – weekly thereafter (INCA, 2001; RCN, 2006).
∞ Check for signs of pneumothorax
∞ Follow local protocol for post procedure care
1.4.7 Removal of tunnelled central venous catheters
∞ Tunnelled lines are removed for the following reasons:
∞ Systemic infection.
∞ Thrombosis.
∞ Obstruction
∞ Fistula maturity
∞ End of treatment
Although this is a relatively straightforward procedure, it is essential this
should only be carried out by appropriately trained personal, as impropriate
removal technique could result in catheter damage, fracture or both. (Macklin
& Chernecky 2004). Potential Complications include: infection, line
dissection, air embolus and bleeding. If catheter removal is required urgently
19
and the vascular access service is not available the procedure detailed below
should be followed.
1.4.7 Local procedure for removal of cuffed tunnelled catheter
Check the patients’ anticoagulation status. If the patient has been receiving
anticoagulants it should be ensured the INR is 1.5 or below.
Set trolley using a sterile technique
Explain procedure to patient and obtain consent
Remove heparin lock by aspirating all lumens.
Prepare patient, and expose area
Don sterile gloves
Clean skin using chlorhexidine 2%
Drape patient with sterile covers
Infiltrate lidocaine 1% (approx. 10mls) locally at entry site, along the line tract
and beyond the cuff, care being taken not to puncture catheter.
Using forceps carefully separate tissue from around the line to expose the cuff.
Care must be taken to avoid line dissection, therefore the use of blades or
scissors is not advised.
If the line accidentally gets cut, grab the line beyond it with forceps and
contact a member of medical staff/ Vascular Access Service immediately.
When the cuff is free, put the trolley or bed on a head down tilt (If this is not
possible place a pillow or other type of support under the knees).
Place a swab over the entry site, and ask the patient to breathe in, then out, and
then to hold their breath (this will prevent air entry) Again if this is not
possible wait until the patient is breathing on inspiration and using one quick
movement pull the line out.
Apply digital pressure until bleeding stops.
If necessary the site should be stitched by medical staff or competent
registered nurse. Remove the stitches after 7 to 10 days.
The site should be covered with a transparent dressing, which can remain in
place until the site has healed.
The patient is advised to take mild analgesia for localised pain, and advised
that they may experience bruising at the site.
20
If the patient is being discharged, they should be given extra dressings to take
home, and advised to speak to their district nurse or practice nurse if they are
worried about the site.
1.4.6 Implications for practice
∞ Only staff competent in CVC care and maintenance should carry out
care and treatment in CVC’s (RCN, 2006)
∞ Use a dedicated lumen for TPN
∞ Use a tunnelled catheter for patients whose anticipated duration of
treatment is more than 3 – 4 weeks.
∞ Dress catheter with a transparent dressing that should be changed every
7 days or sooner if loosened or moist. A gauze dressing should be
replaced by a transparent dressing as soon as possible.
∞ Use a single patient application of alcoholic chlorhexidine gluconate
solution (preferably 2% chlorhexidine gluconate in 70% isopropyl
alcohol) to cleanse area during dressing change. The area should be left
to dry.
∞ Do not apply antimicrobial ointment to catheter insertion sites as part
of routine catheter site care.
∞ Antibiotic locks should not be routinely used.
∞ In – line filters should not be routinely used for infection prevention
purposes.
∞ Preferably, sterile 0.9% sodium chloride for injection should be used to
flush and lock catheter lumens that are in frequent use.
∞ When recommended implanted ports or open – ended catheters should
be flushed and locked with heparin (See section on flushing and
locking)
∞ Change needle free devices every 7 days or as per manufacturer’s
instructions.
∞ Administrations sets in continuous use need not be replaced more
frequently than at 72 hours unless they become disconnected or a
central access device is replaced.
21
∞ Administration sets for blood and blood components should be
changed when transfusion complete or every 12 hours (Whichever is
sooner)
∞ TPN administration sets should be changed every 24 hours.
(Pratt, 2007)
1.4.7 Statlock catheter securing device
Advantages
1. Studies have proved that to reduce the incidence of CRBSI (1, 2)
2. Reduces the risk of accidental needle stick injuries (3)
The centre for Disease Control and Prevention Guidelines for the prevention of
intravascular catheter – related infections (2002), state that these devices can be
advantageous over sutures in the prevention of catheter related blood stream
infections. BCSH guidelines on the insertion and management of central venous
access device’s (2006) also recommend that securing devices, for example, statlock
are preferable to stitches.
Two recent studies document a 2% needle stick rate among clinicians who secure
catheters with sutures. Using a securing device drops this risk to zero (Sheppard,
LeDesma, O’Connor, 1999; Yamamoto, Solomon, Soulen, 2002).
Most securing devices require changing once a week.
1.5 TUNNELLED DIALYSIS CATHETER (PERMCATHS)
22
Tunnelled dialysis catheters are used as a bridge to a more permanent form of access
or in patients with no remaining access sites.
Cuffed venous catheters are the chosen method for temporary access lasting longer
than three weeks, and are also acceptable for shorter durations. They may also be used
in patients who have exhausted all other means of access, or in those patients waiting
for a fistula to mature.
1.5.1 Advantages
∞ No maturity time.
∞ Possibility to insert into multiple sites.
∞ Venepuncture not required for dialysis.
∞ Long-term access to allow maturity of A V fistulae.
∞ Applicable universally
∞ Venepuncture not required for dialysis
∞ No haemodynamic consequences
∞ Ease of catheter placement and replacement
∞ Ease of correcting thrombotic complications.
1.5.2 Disadvantages
∞ Thrombosis
∞ Infection
∞ Risk of permanent central venous stenosis or occlusion
∞ Discomfort and cosmetic problems associated with external placement
∞ Shorter expected use life than other types of access
∞ Lower blood flow rates which require longer dialysis times
∞ 1.5.3 Insertion Technique
As per Hickman type catheter insertion, although requires the use of large dilators to
aid placement. X-ray screening is recommended for placing these catheter unless twin
catheters with small dilators are used.
23
1.6 TOTALLY IMPLANTABLE PORTS (TIPS)
An implantable port or port-a-cath is a venous access device comprised of a portal
body and attaching catheter which are implanted under the skin (Dougherty, 2006).
The port, made of stainless steel, titanium or plastic is a hollow reservoir with a latex
septum and a side outlet which connects to a silicone or polyurethane catheter. It is
this catheter which lies directly into one of the central veins (Schwarz, Groeger and
Coit, 1997).
To administer treatment the skin overlying the
reservoir is punctured with a Huber needle and it is
through this needle that treatment is given
(Goodman, 2000).
Ports and Huber needles are available in many
different types and sizes, allowing device choice to
be tailored to each individual’s need (Dougherty,
2006).
(From Massachusetts General Hospital, America)
1.6.2 History
Totally implantable ports are accepted as a safe and effective method of facilitating
long-term intravenous therapy (Deerojanawong, Sawyer, Fink, Stokes and Robertson,
1998). These devices were first introduced in the early 1980’s and used as a form of
venous access in oncology patients (Dougherty, 2006). Ports are now also commonly
used in patients with cystic fibrosis requiring long-term intravenous antibiotics
because of their low complication rates (Deerojanawong et al. 1998).
1.6.3 Uses
Implantable ports are used for the same reasons as any other central venous access
device but are viewed as a long-term device for use in hospital and the community as
they are easy to maintain and have few associated complications (Dougherty, 2004).
Many recent studies have evaluated the suitability and safety of venous port
implantation and considered the advantages and disadvantages of using this device.
24
1.6.3 Advantages
The main advantage of ports over other venous access devices is that they are
implanted and therefore, not external to the body (Dougherty, 2006). Consequently,
there is less of an impact on patient’s body image as the port is not seen, less risk of
infection as the port is not exposed to life’s daily bacteria, the ability to swim and
bathe and allow more patient activity, an external dressing to the device is not
required and there is no risk of accidental pulling/cutting of the device (Dougherty,
2006; Lamont, McCarty, Stephens et al. 2003). The design of the device also means
that maintenance flushing is only required monthly (Eastridge and Lefor, 1995). The
other great advantage is that these devices are long lasting and can be punctured up to
2000 times before a device change is required. There has been some documented
evidence of ports remaining in situ for up to five years (Burdon, Conway, Murchan et
al. 1998).
1.6.4 Disadvantages
Initial and long-term complications and disadvantages of implantable ports have been
documented in many studies. As with any surgical procedure, pre, intra and post-
operative complications are always a risk (Ahmadi, Izadyar, Ashjaei, et al. 2006).
Biffi, de Braud, Orsi et al. (1998) recorded incidence of catheter/port malfunction,
catheter rupture and embolisation, venous thrombosis and infection. A further
recorded complication is extravasation (Ahmadi et al. 2006). Meanwhile,
disadvantages include mainly that of having to access the port with a Huber needle
which in itself leads to a further drawback of needle stick injury (Dougherty, 2006).
1.6.5 Insertion of Implanatable Ports
Insertion and removal of implantable ports is very similar to insertion and removal of
tunnelled central venous catheters (Dougherty, 2006). However, insertion and
removal of implantable ports should only be carried out by experienced and
competent professionals.
Implantable port insertion is a surgical technique which must be carried out within
strict aseptic guidelines. The port is placed through an incision into subcutaneous
25
tissue commonly in the forearm or upper chest wall (Goodman, 2000). Following
cannulation of the desired vein the catheter is attached to the port and tunnelled
subcutaneously. The catheter tip can then be threaded into the desired vein ensuring
that the tip is positioned within the SVC or right atrium (Baranowski, 1993). The port
can then be anchored to the deeper tissues using sutures and the subcutaneous incision
can then be sutured and dressed. The practitioner should ensure that the port is placed
below the intended suture line in order to prevent port cannulation through scar tissue
(Dougherty, 2006).
The patient should then have a check chest x-ray prior to use to ensure that the
catheter tip is in satisfactory position (Dougherty, 2006).
1.6.6 Care of Implantable Ports
Accessing implantable ports should also always be carried out using strict aseptic
techniques. Huber needles, once in situ, should be secured to prevent trauma and
dislodgement with the use of a transparent dressing (Dougherty, 2006). TIP’s sites
with no needle insitu require no dressing.
There is still some debate among researchers on how frequently these needles should
be changed. Vescia, Baumgärtner, Jacobs, et al. (2007) advice that Huber needles
should be changed after every 2000 punctures, while most other literature including
Dougherty (2006) and Masoorli and Angeles (2002) suggest Huber needles should be
changed weekly.
To maintain patency of the port research suggests that ports should be flushed every
four weeks with heparinised saline (McPhee, 1999).
1.6.7 Removal of Implantable Ports
Removal of implantable ports is also a surgical procedure which should be carried out
using strict aseptic technique. An incision should be made into the fibrous tissue
which forms around the port. The anchoring sutures should then be cut and the port
can be removed ensuring that the entire catheter length is pulled from the venous
system (Galloway and Bodenham, 2004). The subcutaneous incision can then be
sutured and dressings applied.
26
1.6.8 Recommendations for Practice
In conclusion, totally implantable ports are a safe, versatile and adequate method of
administering long-term intravenous therapy (Deerojanawong, Sawyer, Fink, Stokes
and Robertson, 1998).
∞ Implantable ports should be inserted, accessed and removed using strict
aseptic techniques and by practitioners who are competent and experienced in
doing so
∞ Huber needles should be changed after every 2000 punctures or weekly,
whichever is more frequently
∞ Implantable ports should be flushed every four weeks with heparinised saline
1.6.9 Conclusion
In conclusion, totally implantable ports are a safe, versatile and adequate method of
administering long-term intravenous therapy (Deerojanawong, Sawyer, Fink, et al.
1998). Research shows that they have a low incidence of complication rates, up to
85% of insertions have no associated complications related to implantation and
management of these devices (Ahmadi et al. 2006). Although the advantages and
disadvantages of implantable ports have been described, the implications of these i.e.
reduction in infection and service-life are the real advantages to both the patient and
health care organisation.
27
CHAPTER 2: SELECTION OF CATHETER INSERTION SITES
The selection of the best insertion site for the patient can minimise the risk of
infection (Pratt, 2007).
There are a number of factors that have to be assessed when determining the site of a
central venous access device (CVAD) including:
Patient - specific factors
∞ Pre - existing CVAD’s (Anatomic deformity, Bleeding diathesis, Some types
of positive pressure ventilation)
∞ Relative risk of mechanical complications (e.g., bleeding, pneumothorax,
thrombosis);
∞ The risk of infection.
CVAD’s are generally inserted in the subclavian, internal or external jugular, femoral
veins or peripherally inserted into the superior vena cava via the cephalic, or basilar
vein.
Following a systematic review, EPIC state that unless medically contraindicated, the
subclavian vein should be used in preference to the jugular or femoral sites for non -
tunnelled catheter placement. The femoral vein should be avoided.
EPIC further suggest the use of implantable access devices for patients who require
long - term, intermittent vascular access. For patients requiring regular or continuous
access, a tunnelled central venous access device is preferable.
CHAPTER 3: EDUCATION AND TRAINING
All Health Care Workers who deal with central venous catheters must have undergone
training, and deem themselves confident and competent. It is the responsibility of the
health care worker to ensure this prior to working with central venous catheters
(UKCC, 1992).
28
Training in care and maintenance of central venous catheters is available for
healthcare staff across NHSGG&C:
The Vascular Access Service / WOSCC run a ½ day workshop which can be booked
through the Training and Development Department, 34 Shelley Court, Gartnavel
General Hospital (Tel: 50148). This is run on a bimonthly basis.
3.1 Competency
Each health care worker should complete a competency pack when competency has
been obtained. This will be updated annually.
3.1.2 Link nurses for central venous catheter care
Training for link nurses is available at the training and development department 34
Shelley Court on a three monthly basis. The remit of these nurses is to act as mentors
to others within their department, and work with them through competencies thus
ensuring high standards of care within their department.
Contact: Training and Education department, Gartnavel General Hospital 50148
CHAPTER 4: DEVICE SELECTION
There is a range of catheters available for intravenous therapy. It is important to
ensure an optimal match between patient and catheter choice.
4.1 Peripheral and central venous vascular assessment
Consider the diagnosis and prognosis especially taking into account conditions that
may prevent vascular access e.g. radiotherapy skin reactions or previous multiple
peripheral cannulation. Finally consider patient lifestyle.
If peripheral cannulation is possible consider the treatment duration and the likelihood
of treatment extension or additional treatments, as prolonged and repeated intravenous
cannulation is time - consuming and unpleasant for the patient.
4.2 Consideration of the infusate
Peripheral cannualas should only be used for infusates that:
29
∞ Have a final osmolarity < 500mOsm/L
∞ PH between 5 & 8
∞ Not an irritant or vesicant for continuous infusion
Select the insertion site and catheter size that allows rapid dilution of the infusate to
reduce the risk of chemical phlebitis.
Select a single-lumen catheter unless multiple ports are essential for the management
of the patient. This will decrease the chance of catheter infection (Terotola, 2000,
Sansivero, 1998).
30
4.3 Length of treatment
The type of device will usually depend on the length of time the treatment will last.
Treatment required for: Device choice
Up to one week Cannula
One week to 6 months PiCC line / Tunneled catheter
One month to 2 years Tunneled catheter / Implantable port
(Vygon, 2001)
31
CHAPTER 5: INFECTION PREVENTION IN CENTRAL VENOUS
CATHETERS
Infection is one of the greatest complications associated with a central venous catheter
(CVC). Although CVC’s provide necessary vascular access, their invasive nature puts
patients at risk for local and systemic infectious complications. CVC’s disrupt skin
integrity and this direct opening into the vascular system creates a portal for
pathogens to enter the blood steam (Earsing et al. 2005) During prolonged
catheterisation CVC’s can be manipulated multiple times per day and can also have
multiple lumina therefore increasing the risk of complications. For this reason it is
advised that the lumina diameter and number of lumina is kept to a minimum. (Bishop
et al .2007; Pratt et al. 2007).
Infective complications can occur in several ways, including contamination of the
CVC by: skin flora at the point of insertion, skin bacteria migration down the tunnel
tract, bacteria transfer during manipulation and seeding from another site of
infection.(Rosenthal, 2006) Infective complications include: local site infection,
catheter-related bloodstream infection (CRBSI), septic thrombophelbitis and other
systemic infections.
5.1 Catheter-Related Bloodstream Infection
Defined by the following:
BSI is considered to be associated with a central line if the line was in use during the
48 hour period before the development of the BSI. If the time interval between onset
of infection and device use is greater than 48 hours, there should be compelling
evidence that the infection is related to the central line.
Or: At least two positive blood cultures with the same organism, obtained from at
least two separate sites at different times, in association with evidence of colonisation
of the catheter with the same organism. The later can only be strictly be fulfilled by
removing the catheter.
5.2 Clinical Sepsis
Should meet the following criteria:
32
Criteria 1: Patient has at least one of the following clinical signs with no other
recognised cause: Fever (>38 degrees centigrade), hypotension (systolic pressure
<90mm Hg), or oliguria (<20mL/hr), and blood culture not done or no organism or
antigen detected in blood and no apparent infection at another site, and physician
institutes treatment for sepsis.
Secondary BSI: A culture-confirmed BSI associated with nosocomial infection at
another site. Secondary BSI must yield culture of the same organism and exhibit same
antibiogram as the primary nosocomial infection site.
(Taken from NHS Scotland HAI prevalence survey protocol)
5.3.3 Prophylactic Antibiotics
Prophylactic administration of systemic antibiotics has previously been used to reduce
the incidence of catheter related infection. McKee et al (1985) stated that
contamination of the catheter might occur at the time of insertion despite the use of
aseptic techniques. They set out to determine whether the administration of a single
dose of prophylactic vancomycin at the time of insertion would decrease the incidence
of catheter- related sepsis. However, they failed to demonstrate a reduction in the
incidence of clinical or bacteriological proven catheter-related sepsis in patients
receiving vancomycin, which suggests that colonization of the catheter at the time of
insertion is not the predominant cause of catheter-related sepsis. They also suggested
that bacteria are more likely to be introduced during manipulation of a system, such as
changing the hubs or giving sets, thus further reason why single dose vancomycin at
the time of catheter insertion does not affect rates of catheter sepsis. Department of
Health, Epic Project (2001) and recently updated in February 2007, have developed
guidelines for preventing health care associated infection. Pratt et al, from the Epic
Project, advise not administering prophylactic antibiotics routinely for central venous
access, as many of the scientific studies examined were not conclusive.
Edmond et al. (1995) confirmed this thought and caused many to rethink the use of
vancomycin due to the spread of vancomycin resistant enreococci. The Centre for
Disease Control and Prevention (2002) have issued guidelines for limiting
vancomycin use, stating that the agent should not be used for routine prophylaxis.
33
The management of catheter infections remains controversial. Various studies have
produced conflicting results as to the benefits of antibiotic prophylaxis. Because of
the spread of vancomycin-resistant enterococci, as highlighted by Edmond et al
(1995), we need to rethink the use of routine antibiotic administration, especially in
non-neutropenic patients.
5.3.4 Definitions
Exit site infection: Local infection of the skin and soft tissue around the exit site.
Erythema and purulent discharge with tenderness are typically present. Usually the
subcutaneous tissue is not involved, although in some cases it may be affected. (Oncu
and Sakarya, 1992).
Tunnel Infection: Invasive soft tissue infection that extends along the subcutaneous
tunnel towards the vein. The cuff is typically involved. Tenderness and erythema
along the catheter tract is [present with copious purulent discharge from the exit site.
Tunnel infections require immediate line removal. (Ward et al.1999).
Catheter-related Bacteraemia: This presents with signs and symptoms of systemic
infection ranging in severity from minimal to life-threatening. Fever, shakes, nausea
and vomiting, back pain and changes in mental state. In any patient with a central
venous catheter, symptoms and signs of infection without another confirmed source
should raise the concern that the catheter may be the source of the infection. (Oncu
and Sakarya, 1992).
5.3.6 If site infection suspected
∞ Send swab to microbiology for culture and sensitivity.
∞ Start patient on broad spectrum antibiotics.
∞ Continue using the catheter.
5.3.7 If line infection is suspected
∞ Stop using the catheter.
∞ Take cultures from the line and peripherally.
∞ Check – does the temperature drop (after 3 -4 hours) when the catheter is not
in use. If yes, remove the catheter or discuss with the microbiologist. If no,
34
await the culture results and is positive, remove the line or discuss with the
microbiologist. If negative, continue use of the catheter.
5.3.8 Recommendations for Practice.
It is believed that the overall balance of care can prevent most catheter related
infections, rather than the administration of single dose antibiotics. We must be aware
of the following to reduce the risk of catheter infections.
∞ Selection of catheter type
∞ Selection of catheter site
∞ Optimum aseptic technique during catheter insertion
∞ Skin antisepsis with 2% Chlorhexadine solution
∞ Catheter and catheter site care
5.3.9 Catheter replacement
∞ Do not routinely replace catheters as a method of infection prevention
∞ If there is no evidence of infection at the catheter site or CRBSI guidewire can
be used to replace malfunctioning catheter.
∞ If CRI is suspected but no evidence of infection at site, new catheter can be
inserted at a different site (do not use guidewire exchange).
(Pratt, 2007)
35
Hand washing Cross-transmission, the transfer of micro organisms between humans, which occurs
directly via an environmental source, occurs at all time in hospitals. It is the
antecedent factor to cross infection that can result in negative clinical outcomes.
Overviews of epidemiological evidence conclude that hand cross contamination is a
major contributing factor in the current infection episodes in hospital in – patients
(Pratt et al. 2001) Therefore all health care workers must be aware of their
responsibility in prevention of infection. An effective hand washing technique is
essential and is demonstrated below
HAND HYGIENE Six stages of hand washing
36
CHAPTER 6: CUTANEOUS ANTISEPSIS
The cause of most catheter-related blood stream infections are those micro organisms
that colonise catheter hubs and the skin surrounding the catheter insertion site.
(Mermal, 2000). Skin antisepsis is regarded as one of the most important measures for
preventing catheter-related infection and appropriate preparation of the insertion site
will reduce this risk.
Maki et al. (1991) conducted a trial to compare the effectiveness of 2% chlorhexidine
compared to either 10% povidone iodine or 70% alcohol. They found that 2%
chlorhexidine was superior and an additional study by Mimoz et al (1996) has since
confirmed the superior efficacy of chlorhexidine 2%.
The Centre for Disease Control and Infection (O’Grady et al, 2002) have stated in
their guidelines for prevention of intra-vascular catheter-related infection that
although povidone iodine has been the most widely used antiseptic for cleaning
central venous catheter sites, that following these studies chlorhexidine is the optimal
cleaning solution.
6.1 Recommendations for Practice
Most central venous access devices and other catheter materials are generally alcohol
resistant. However, it is recommended that manufacturers’ guidance is adhered to
before using a solution of chlorhexidine containing alcohol.
Cloroprep stick
The following recommendations are taken from the Epic Guidelines updated in
February 2007.
37
∞ An alcoholic chlorhexidine gluconate solution (preferably 2% chlorhexidine
gluconate in 70% isopropyl alcohol) should be used to clean the catheter
insertion site and allowed to air dry. An aqueous solution of chlorhexidine
gluconate should be used if the manufacturer’s recommendations prohibit the
use of alcohol with their product.
∞ Individual single use sachets of antiseptic solution or individual packages of
single use antiseptic impregnated swabs or wipes should be used to disinfect
the insertion site.
∞ Do not apply antimicrobial ointment to catheter insertion site as part of routine
care
∞ Health care workers should ensure that the catheter site care is compatible
with catheter materials i.e. tubing, hubs, injection ports, leur connectors and
extensions. They should also check compatibility with the manufacturers’
recommendations.
Chlorhexidine impregnated disc (eg. Biopatch)
With the break in the patient’s skin being a common pathway for microbes to enter
the bloodstream (Mermel, 2000), it can be deemed beneficial to protect this site
further. Several studies have shown that the use of a chlorhexidine 2% impregnated
disc e.g. bio patch can reduce the incidence of catheter related bloodstream infection
when placed around the catheter at the point it exits the patient’s skin (Mann et al.
2001, Garland et al. 2001, Maki et al. 2000). This type of dressing has resulted in a
60% reduction in catheter related bloodstream infections and a 44% reduction in the
incidence of local infection. (Maki et al. 2000)
38
CHAPTER 7: CATHETER OBSTRUCTION
Central venous catheter occlusions are a common problem, especially with small –
gauge catheters.
7.1 Types of occlusion
7.1.1 Mechanical Occlusions
Mechanical occlusions are caused by improper function of some part of the
administration set up, the dressing, or the catheter that prevents flow. Some
occlusions are easy to identify, such as kinks or closed clamps, others are less obvious
and are caused internally through positioning of the catheter.
7.1.2 Blood occlusions
A blood occlusion occurs when a clot completely occludes the lumen of the catheter.
Blood occlusions can occur suddenly, as when the IV solution runs dry and the blood
backs up into the tubing, or over time as blood residue builds up in the catheter lumen,
causing a sluggish flow. Failure to correctly flush is a common cause of blood
occlusions.
7.1.3Fibrin sheath formation
The human body reacts to any irritant in the vascular system by depositing fibrin
around the irritant. In central lines, the body sees the catheter as a foreign object, and
deposits fibrin and thrombus around it (Santilli, 2002) Fibrin sheath formation has
been reported as early as 24 hours after insertion. According to Xiang (1998) after
catheterisation, 42% to 100% of central venous catheters are surrounded by a fibrin
sheath
The first sign of a fibrin sheath is the inability to withdraw blood. The vacuum created
by negative pressure of withdrawal pulls back a flap, which is formed by the fibrin
sheath, against the catheter opening and prevents blood from entering the lumen. IV
fluids may flow between the outside of the catheter and the sheath and leak out into
the insertion site causing extravasation if the fibrin continues to form along the length
of the catheter (Andris, 2000). It has been suggested that fibrin sheath may influence
catheter related sepsis (Lloyd, 1993, Mehall, 2002)
Central venous catheters that will not flush or allow flow, are considered to be
occluded. Occlusions can be caused by mechanical, drug, or blood obstructions.
39
Mechanical obstruction can be ruled out by checking the following:
∞ IV tubing not clamped or kinked
∞ All connections are tight and there are no air leaks
∞ Sutures are not too tight at the exit site
∞ The catheter is not kinked, twisted or misplaced
∞ Ask patient to change position, cough, deep breathe, stand up or lie down with
the foot of the bed tipped up
∞ If aspiration is possible following position change, consider chest x-ray to
check catheter position or possible kinking of catheter.
∞ If aspiration is still not possible following the above, consider thrombolytic
treatment.
7.2 Thrombolytic treatment
Savader et al. (2001) and Svoboda et al. (2004) have both demonstrated that catheter
occlusions can be treated with thrombolytic agents such as urokinase and alteplase.
These have both been shown to be effective in re - establishing patency in catheters.
Urokinase is a direct plasminogen activator and was first introduced in 1978. It has
been used therapeutically in millions of patients for a variety of indications. In low
doses, it is highly effective in re-establishing patency to occluded lumens of
indwelling CVC’s (Svoboda et al. 2004). Urokinase has traditionally been used as
thrombolytic agent for catheter de clotting, and success rates have been between 55%
to 85% (Haire et al. 1994 and Meers 1998). In December 1998, however, the United
States Food and Drug administration released a warning regarding potential infectious
disease risks from current supplies of urokinase (UK Food and Drug Adminstration,
1999). Since this time other thrombolytic agents have been used for catheter
clearance. One of these drugs was alteplase. Recombinant tissue plasminogen
activator (alteplase) has a low adverse reaction rate but is expensive and only stable
for 8 hours after reconstruction. Wiernikowski et al. (1999), however, provides
evidence that alteplase can safely be frozen at –30oC for up to 22 weeks.
7.3 Evidence to support the use of alteplase
40
There have been many clinical trials to assess the effectiveness of alteplase for
catheter clearance. In one trial by Genetech, inc. (2001) 2mg/2ml alteplase dose
restored the function to 150 patients with catheter occlusion up to 24 hours in
duration. Patients were randomised to receive either alteplase or a placebo instilled
into the lumen of the catheter; catheter function was assessed at 120 minutes.
Restoration of function was assessed by successfully withdrawing 3mls of blood and
infusion of 5mls of saline through the catheter. All patients whose catheters did not
meet these criteria where then re administered alteplase, until function was restored or
each patient had received up to two active doses. After the initial dose of study agent,
51 (67%) of 76 patients randomised to alteplase and 12 (16%) of 74 patients
randomised to placebo had catheter function restored. A total of 88% of alteplase –
treated patients had restored function after up to two doses.
The 2nd study was an open-label single arm trial in 995 patients with catheter
dysfunction. Patients were treated with up to two doses of alteplase 2mg / 2mls
instilled into the lumen of the catheter. Assessment for restoration was made at 30
minutes post instillation. 30 minutes after the first dose, 516 (52%) of 995 patients
had restored catheter function. If function was not restored after the first dose, a
second does was administered. 209 patients received a second dose. Thirty minutes
after instillation of the second dose, 70 (33%) of 209 patients had restored catheter
function. 120 minutes after the instillation of the second does, 97 (46%) of 209
patients had restored catheter function. A total of 844 (85%) of 995 patients had
function restored after up to 2 doses. Across both trials, 796 (68%) of 1043 patients
with occlusions present for less than 14 days had function restored after one dose, and
902 (88%) had function restored after up to two doses. Of 53 patients with occlusions
present for longer than 14 days, 30 (57%) of patients had function restored after a
single dose, and a total of 38 patients (72%) had restored function after up to two
doses.
346 patients who had successful treatment outcome were evaluated at 30 days after
treatment. The incidence of recurrent catheter dysfunction within this period was
26%). Although this study was carried out by the company supplying the product the
numbers were large, and the results very impressive.
41
A smaller study was carried out in the radiology department of the Royal Preston
Hospital (Donnelly et al. 2004). 21 patients presented with clinical features of fibrin
sheath formation. 1.5mgs / 2mls of alteplase was instilled into each catheter lumen,
and a repeat alteplase lock was instilled, if required. After one lock of 24 hours the
patency rate was 47.6%. A second dose was administered if necessary. The overall
patency rate was 100%. The result of this very small study is conclusive and proves
that alteplase could be considered as an alternative to urokinase.
There have been studies performed to evaluate the efficacy of urokinase versus
alteplase for the treatment of catheter occlusion. In a study by Aitkinson et al. (1990)
occlusions were initially treated with urokinase. Six out of 25 occlusions failed to
clear after a dose of urokinase. These six occlusions were treated with a 2 mg dose of
alteplase. Alteplase restored catheter function in five out of the six catheters. This
success was echoed in a double – blind, randomised clinical trial conducted by Haire
et al (1994) comparing urokinase and alteplase. A total of 50 occluded catheters were
treated with urokinase or alteplase, and a second dose instilled if catheter function was
not restored after the initial dose. The result of this study demonstrated that catheters
treated with alteplase had restored function for 89% compared with 59% of those
treated with urokinase. As well as this only 18% of catheters treated with urokinase
had restored function after one dose compared with those treated with alteplase,
which was 46%. Both of these studies suggest that alteplase has a more successful
rate of success than urokinase. There remain concerns however over using alteplase,
as the most common adverse event associated with its use is bleeding. If alteplase is
installed properly into the lumen of the catheter, this should result in minimal
systemic drug exposure (ResouceNurse.Com). Evidence from studies by Deitcher et
al (2002), Aitkinson et al (1990) and Shea et al (2001) all suggest that alteplase was
safe during use in trials, and produced no changes in prothombin time, and no adverse
effects were seen.
7.4 Urokinase administration (Hickman type catheters)
∞ After discussion with the medical staff, obtain a prescription for the
42
medication
∞ 2mls (5000ui/ml) urokinase should be administered into each catheter
lumen.
∞ If the catheter is completely blocked the use of a three way tap to suction
the medication through the catheter is advised
∞ The urokinase should remain in situ for up to one hour.
∞ Aspiration and flushing should be then attempted.
∞ Repeat administration if required.
∞ If unsuccessful a chest x-ray should be requested to check the tip position
of the catheter if this has not already been performed.
∞ If aspiration is still not possible consider catheter removal and re insertion.
43
7.5 FLUSHING / LOCKING
At the time a CVC is inserted in the vascular system, fibrin deposition
begins on the exterior and intraluminal catheter surfaces. Other proteins
associated with both maturation of the fibrin clot and extracellular matrix
formation (fibronectin) also accumulate. As these deposits continue to
develop they can rapidly result in several different types of thrombolic
events. (Bagnall-Reeb et al.1992). One such thrombolic event is intraluminal
thrombosis, which occurs when blood remaining in the catheter forms a clot
after inadequate flushing or from retrograde blood flow. Obstruction of a
CVC presents as the inability to either flush fluids through or withdraw
blood from the catheter. (Baranowski,1993). Heparin has historically been
used to routinely flush CVC’s to prevent the formation of thrombosis.
(Hickman et al. 1979). However the volume and concentration of heparin as
well as frequency of flushing required maintaining patency, continuing to be
areas of controversy and inconsistent practice. The RCN (2006) guidelines
suggest that CVC’s should be flushed and locked weekly. The flushing
solution (normal saline 0.9%) should be at least twice the volume of length
of catheter lumen.
When flushing a catheter a push pause technique should be used, as this
creates turbulence within the catheter which removes any debris from the
internal catheter wall. The clamp should be closed in the last second when
flushing to ensure positive pressure which prevents a backflow of blood into
the line (Todd, 1998; INS, 2000; EPIC, 2007)
44
7.5.1 Heparin locks
There is very little up to date research on flushing protocols for CVC’s. The
most recent article was by Weatherhill (1999), in which the author discussed
the development of a local policy for maintaining or increasing the patency
of CVC’s. In the article Weatherhill (1999) notes that the problems of using
heparin may depend on the concentration of heparin solution. Hanson (1976)
found that heparin solutions containing 10 units per ml did not affect clotting
time, prothombin time or activated partial thromboplastin time and this
solution prevented the formation of clots within the catheter. This strength of
heparin solution is also advocated by Weber (1991) who states, “The lowest
effective concentration of heparin should be used” 10 units/ml has been
shown to be effective. The RCN (2003) and INS (2000) also recommend
that the concentration of heparin should be the lowest possible that will
maintain patency – usually 10units of heparin in 1ml of 0.9% sodium
chloride.
The literature on the volume of heparin which should be used is also
variable, in a quasi-experimental/descriptive study conducted by Brown-
Smith, et al. (1990) comparing the incidence of thrombus in two cohorts of
patients using different flushing regimes, results indicated that 5mls of a
1:10 solution of heparin is a sufficient volume and concentration to flush
CVC. The RCN (2003) recommend the volume of the flush solution should
be equal to at least twice the volume of the catheter and add on devices –
usually 5-10 mls. Vygon manufactures state that the priming volume for a
6.6fr single lumen catheter is 1.10ml and for a 9.5fr double lumen catheter is
1.65ml and they recommend a lock of 2-3 mls of 500units of heparin
solution. However they also state that the CVC should be flushed with saline
after each injection, perfusion or blood sampling and finally flushed with 2-3
mls of 500units/ml of heparin. Barabowski (1993) also states that when
heparin is used to assess patency of the catheter and to eliminate potential
incompatibilities with medications being administered, the catheter should
be flushed with 0.9% sodium chloride before and after intermittent
medication administration. After blood withdrawal the catheter should also
45
be flushed with 0.9% sodium chloride to remove residual red blood cells and
thus prevent possible occlusion before flushing with the heparinized saline
solution.
Within NHSGG&C the recommendation is a 2ml lock of heparin 10units as
this extends the catheter lumen length.
7.5.2 Frequency of flushing
The RCN (2006) recommend frequency of flushing should be weekly unless
occlusive problems indicate otherwise. A study carried out by Kelly et al.
(1992) support the use of weekly flushing protocols, concluding that
flushing a CVC with 2mls of heparin 10units /ml was a safe and effective
method of cvc management. This study found that weekly flushing did not
increase incidents of dysfunction and the infection rate remained acceptable
when compared with the literature.
7.5.3 Flushing techniques
Todd (1998) advocates that the patency of the catheter should be maintained
by using a pulsated push-pause and positive pressure flush thus creating
turbulence within the catheter lumen – removing debris from the internal
catheter wall. Positive pressure with the lumen of the catheter should be
maintained to prevent reflux of blood (INS 2000). Consideration must be
given to syringe size used for flushing since the smaller the syringe size, the
greater the pressure generated. Catheters are designed to withstand venous
infusion pressures, but typically infusion pressures should never exceed 25-
40 pounds per square inch (PSI). Smaller sized syringes will generate
pressures in excess.
The flushing regimes and practices in maintaining CVC patency vary
widely. Recommendations for flushing catheters are abundant in the
literature but few are research based. It is therefore very clear that further
research is necessary focusing on the volume and concentration of heparin as
well as frequency of flush
46
Non –tunnelled central line
In between usage, flush with 10mls of 0.9% saline. Non tunnelled catheters
do not require heparin lock if used frequently. Consider line removal if line
not being used regularly.
Tunnelled central line (Hickman) and PICC lines
Non-valved catheters (catheters with clamps), require flushing with 10mls
0.9% saline per lumen, using push/pause technique. They require to be locked
with 2mls of 10 units/ml heparin per lumen. This requires to be done on a
weekly basis and following each use of the lumens of the catheter.
Valved catheters (catheters with no clamps), require flushing with 10mls 0.9%
saline, using push/pause technique but do not require a heparin lock.
Tunnelled Dialysis Lines
Dialysis catheters required to be flushed with 20mls 0.9% saline, using
push/pause technique and locked with heparin 5,000 units/ml, to lumen
volume. This requires to be done following dialysis and after each catheter
usage. Heparin must be aspirated from the catheter prior to use and prior to
catheter removal.
47
CHAPTER 8: DRESSING SELECTION
Consider before dressing Exit Site Sterility Stability Inspection Versatility Duration
The safe maintenance of a central venous catheter and relevant care of the catheter
site are essential components of a strategy for preventing catheter related (CR)
infections in patients. This includes good practice in all aspects of catheter care,
and the use of an appropriate catheter site dressing regimens.
The type of dressing used on the Vascular Access Device (VAD) has been
recognized as one of the variables which affect complication rates associated with
these devices (Larwood, 2000) In addition; dressings offer securement of the VAD.
Most studies support and recommend the use of dressings (Larwood, 2000)
however; the type of dressing remains controversial (CDC, 2002)
48
8.1 Review of the literature (Dressing choice)
A series of evidence based guidelines have been devised aimed at reducing
healthcare associated infections associated with vascular access devices (VAD’s).
As bloodstream infections associated with central venous catheters are a significant
cause of morbidity in 2001 the Department of Health commissioned the EPIC team
at Thames Valley University to produce a set of guidelines for the prevention of
health care associated infections (HCAI) in particular catheter related blood stream
infections (CR-BSI) It has been estimated that up to 6000 patients per year in
England acquire a CR-BSI and 1n 2000, the national Audit Office estimated the
additional cost of a bloodstream infection to be £6209 per patient. National
evidence - based guidelines for preventing healthcare - associated infections
(HCAI) in National Health Service (NHS) hospitals in England were updated in
2007 and provide comprehensive recommendations (Pratt et al. 2007) for
preventing HCAI. Following multiple systematic reviews of experimental and non
experimental research and expert opinion they recommend a sterile, transparent,
semi- permeable dressing to cover the catheter insertion site, they suggest that this
dressing should be changed every 7 days or sooner if they are no longer intact or
moisture collects under the dressing. If a patient has profuse perspiration or if the
insertion site is bleeding or oozing, a sterile gauze dressing is preferable to a
transparent, semi - permeable dressing. If a gauze dressing is used this will
required to be assessed daily and changed when inspection of the dressing becomes
damp, loose or soiled. A gauze dressing should be changed to a transparent
dressing as soon as possible. Dressings that are used on tunnelled or implanted
catheter insertion sites should be replaced every 7 days until the site has healed,
unless there is an indication to change them sooner. The ‘Winning Ways guidelines
also state that a dedicated occlusive dressing should be used to dress central venous
catheters.
Guidelines from both the ICNA (Infection Control Nurses Association), 2001 and
RCN (Royal College of Nursing, 2003) recommend a sterile, transparent, self –
adhesive, semi – permeable dressing and suggest the same dressing changes as
above.
49
A recent Cochrane review aimed to discover if different types of dressing
(transparent, polyurethane, gauze and tape) used to protect the VAD site reduced
the chance of developing a catheter related infection found that although the
dressings varied in their ease of use, ability to prevent infections and skin
reactions, no risk difference among the dressings reviewed was found and it was
recommended that dressings reflected patients preference (Gillies et al. 2003). A
recent by Mermel (2000) echoed these findings and drew the following conclusion
on the prevention of CR infections “on the basis of all available evidence, the
choice of central venous catheter dressings may be a matter of preference and cost”
The two main types of dressing used for CVC sites are transparent, semi -
permeable, polyurethane dressing and gauze and tape dressing.
8.2 Transparent dressings
These dressing prove popular as they reliably secure the device and permitted
continuous inspection of the catheter site, permit the patient to bathe and shower
and require less frequent changing than standard gauze and tape, thus saving time.
They allow prevent the entry of air into the vascular system following insertion and
removal of a VAD.
8.3 Colliod or Sterile gauze
Sterile gauze dressings are more appropriate than transparent dressings when
insertion sites are bleeding, oozing or if the patient is diaphoretic (CDC, 2002;
Hadaway, 2003b; Rosenthal, 2003)
The potential risk of infection associated with these dressings was controversial
and studies examined by Healthcare Infection Control Practices Advisory
Committee (HICPAC) were contradictory; some suggesting the use of transparent
dressing for peripheral and CVC’s increased both microbial colonization of the
catheter site and the risk of subsequent catheter related (CR) infections while
others including the largest controlled trial of peripheral venous catheter dressing
regimens available at the time (Maki, 1987) failed to demonstrate any difference in
infection risk between transparent and gauze dressings. In one meta - analysis of
catheter dressing regimes, CVC’s on which a transparent dressing was used had a
50
significantly higher incidence of catheter - tip colonization, but a non - significant
increase in the incidence of CR-BSI (Hoffman, 1992) HICPAC also noted
preliminary data that suggested that newer transparent dressing that permit the
escape of moisture from underneath the dressing could reduce the incidence of
colonization and CR infections (Maki et al. 1991)
The results of the meta - analysis are consistent with the favourable outcome of
previous studies addressing the issue of local flora overgrowth under transparent
dressings. A study with a 2 X 2 factorial design comparing transparent dressings
versus no dressing and chlorhexidine disinfectant versus no disinfectant on the
intact upper arm skin in 55 patients showed that transparent dressings significantly
reduced aerobic skin flora growth versus no dressing and that the reduction was
higher when the areas had been disinfected previously.
8.4 Functions of IV dressings
The functions of IV dressings are multiple and included:
∞ Providing a barrier impermeable to water and bacteria
∞ Protect the catheter site from extrinsic contamination
∞ Discourages bacterial production at the insertion site
∞ Secures the catheter thereby preventing dislodgement
VAD’s offers direct access to a patients’ vascular system and provides a potential
route of entry of micro organisms into the system. These organisms can cause
serious infection if they are allowed to enter and proliferate in the intravenous
cannula, insertion site or intravenous fluid.
51
8.5 Size and shape of dressing
There are a range of shapes and sizes of dressings and the chose is determined by
both the patient and the catheter type and location.
8.6 General guidelines
When choosing a dressing the factors that are essential are:
∞ Sterility on application
∞ Stability
∞ Allows continuous visual inspection of the catheter and insertion site
∞ Ability for the patient to shower and bathe with out the dressing becoming
saturated
∞ Limited dressing changes
8.7 Therefore a dressing should be
∞ Transparent (Allows visual inspection)
∞ Self - adhesive (Ensures stability therefore reducing the risk of trauma,
mechanical phlebitis and contamination)
∞ Semi - permeable (Protects the site from bacteria and liquid but allows the
skin to “breathe”)
Post line removal – Bioclusive dressing – helps prevent air entry.
52
CHAPTER 9: BLOOD SAMPLING
If a patient has a CVC in situ it should be used for blood sampling, therefore
minimizing undue stress to patients through multiple venepuncture.
Frequent unnecessary opening of the line has been shown to increase the risk of
contamination, therefore, blood sampling should only be taken on a “required” basis
and all samples should be taken at the one time if possible.
Using a strict aseptic technique, withdraw 5-10mls of blood and discard the syringe,
using a fresh syringe for the samples thus ensuring that samples are not including
“dead space” or contaminated with heparin (Cella and Watson, 1989). Only when
sampling for blood cultures must this initial 5-10mls be used for the sample to ensure
accurate diagnosis.
If the CVC is in use when blood sampling is required be aware that the infusate may
affect the laboratory results, therefore, infusion should be stopped prior to blood
sampling and lines should be flushed (RCN, 2003).
53
CHAPTER 10: REPLACEMENT OF INTRAVENOUS ADMINISTRATION
SETS AND HUB CARE
10.1 Administration Set Changes
The routine replacement of intravenous administration sets has been well researched.
Studies show that replacing intravenous administration sets and all attached tubing
should take place no more frequently than every 72 hours for clear fluid infusions to
ensure a cost-effective and safe practice, unless sets have been disconnected from the
central venous device (Pratt et al. 2007). With fluids, such as total parenteral nutrition
(TPN) and blood products, which enhance microbial growth, intravenous
administration sets should be changed more frequently. Research suggests that
administration sets which introduce blood products should be changed 12 hourly
(Effective Use of Blood Group Scottish National Blood Transfusion Service, 2004)
while those used for lipid based substances (i.e. TPN) should be changed 24 hourly
(Reiter, 2004). Further recent research shows that statistically central venous devices
with intravenous giving sets left in situ for up to 96 hours show no significant
increases in infection rates (Gillies, O’Riordan, Wallen, et al. 2004).
Intravenous administration sets (including any tubing from the catheter to the fluid
being administered) should be clearly labelled, indicating date and time of change,
with a specific lumen designated for the administration of TPN (LTHT Infection
Control Policies, 2003).
54
10.2 Hub Care
Hub care has also been hugely researched in recent years. The introduction of closed
needle-free sampling systems can reduce port and administration fluid contamination
(Leon et al. 2003), and the closed system ensures less risk of complications such as air
embolism and haemorrhage. The devices should be considered to have highly
contaminated external surfaces with some evidence suggesting that they may increase
the risk of infection. However, studies have shown that when these devices are used in
conjunction with manufacturer’s guidelines they do not significantly affect the
incidence of associated infection (Pratt et al. 2007). In particular these devices should
be cleaned with appropriate antiseptic cleaning solutions prior to and after every use
in order to minimise the risk of contamination (Pratt et al. 2007).
Care should be taken to ensure that closed sampling systems are changed in
accordance with manufacturer’s guidelines. These devices should be changed every 7
days.
55
CHAPTER 11: ASEPTIC TECHNIQUE
Aseptic technique is the methods taken to keep patients free from hospital-acquired
micro-organisms as much as possible by preventing contamination (Crow, 1989).
Procedure guidelines for aseptic technique include a full surgical scrub and the use of
sterile surgical clothing and protective devices, i.e sterile gloves and gowns
(Mangram, Horan, Pearson et al. 1999), or the use of the “no-touch” technique which
ensures that hands, even though they have not been washed using a full surgical scrub,
do not contaminate the sterile equipment or the patient by using sterile forceps, gloves
(Department of Health, 2001a) or swabs.
There is still a lot of controversy surrounding the handling of CVCs and aseptic
technique. The evidence is of a conflicting nature as there have been few statistically
significant findings showing that the “no touch” technique is adequate in preventing
infection when handling CVC’s (Larwood, Anstey and Dunn, 2000).
However, research does show that if a strict aseptic technique is not adhered during
all catheter manipulations, sites can easily become contaminated and act as a potential
source of infection due to contamination (Tebbs, Trend and Elliott, 1995).
Therefore, it would be our recommendation that a full aseptic technique is adhered to
when handling central venous access devices (CVAD’s) as research has not
statistically proven that the “no-touch” technique is satisfactory in the prevention of
contamination and thus, infection.
56
CHAPTER 12: POWER INJECTION OF CONTRAST MEDIA VIA CVC’S
CVAD’s are frequently placed for patients who receive chemotherapy or in patients in
whom long term IV therapy is necessary but do not have adequate venous access.
When bolus administration of contrast material is indicated for example during CT
examination there are few options for delivery of contrast media (Herts et al. 1996;
Reynolds and Grosvener, 2003)
∞ Peripheral catheter
∞ CVAD
The policy for delivery of contrast via CVAD varies among institutions. This may in
part due to local policy and that there are no concrete recommendations by
manufacturers of either CVAD’s or injectors.
Recently new catheters have been devised that, according to manufacturers’
guidelines, are suitable for power injection of contrast.
Recommendations for practice
∞ If not available local policies should be agreed.
∞ Radiologist should contact CVAD manufacturers for advice.
57
REFERENCE LIST
Adris D A, Zrzywde E A (1997) Central Venous Access: Clinical practice issues. Nurs In North America: 32, 719 – 740 Ahmadi J, Izadyar M, Ashjaei B, Klantari M, Nahvi H, Joodi M, Vali M and Mehrabi V (2006) Study of Advantages and Disadvantages of Totally Implantable Venous Access Devices. Tehran University of Medical Sciences, Acta Medica Iranica: 44(3), 199-202 Atkinson J, Bagnell H, Gomperts E (1990) Investigational use of tissue plasminogen activator (t-PA) for occluded central venous catheters. Journal of Parental and Enteral Nutrition: 14 (3) 310 – 311 Bagnall-Reeb H, Ryder M & Anglim M.A (1992) Venous access device occlusion. Abbott Laboratories, Illinois: Pharmaceutical Products Division.
Baranowski L (1993) Central Venous Access Devices – Current Technologies, Uses and Management Strategies. Journal of Intravenous Nursing: 16(3), 167-194
Bergenzer, T. (1998) ‘Is routine replacement necessary?’ In Arch. Intern. Med. 158, 151 - 156. (111)
Biffi R, de Braud F, Orsi F, Pozzi S, Mauri S, Goldhirsch A, Nole F and Andreoni B (1998) Totally Implantable Central Venous Access Ports for Long-Term Chemotherapy. Annals of Oncology: 9, 767-773 Bishop L, Dougherty L, Bodenham A, Mansi J, Crowe P, Kibbler C, Shannon M and Treleaven J (2007) Guidelines on the insertion and management of central venous access devices in adults. International Journal of Laboratory Haematology: 29(4), 261-278 British Committee for Standards in Haematology (2006) BCSH Guidelines on the Insertion and Management of Central Venous Access Devices. BCSH: London Brown-Smith J.K., Stenor M.H,.& Barley Z.K. (1990) Tunnelled catheter thrombosis : Factors related to incidence. Oncology Nursing Forum. 19(4) 599-605 Bunting, J. Slaughter, R.E. Masel, P.J (2000) Ultrasound placement of peripherally inserted central catheters (PICCs) in adults with cystic fibrosis. Thorax. (June) 55: 535
Burdon J, Conway SP, Murchan P, Lansdown M, Kester RCK (1998) Five Years’ Experience of PAS Port Intravenous Access System in Adult Cystic Fibrosis. European Respiratory Journal: 12, 212-216
Callaghan S, Copnell B, Johnston L (2002) Comparison of two methods of peripheral intravenous cannula securement in the paediatric setting. Journal of Infusion Nursing, 25 (4) 256 - 264
58
Carlson, K. Perdue, M.B. Hankins, J. (2001) ‘Infection Control’ In infusion therapy in clinical practice. 2nd ed. Pennsylvania: WB Saunders. Chapter 8, 126 - 140. Cella J and Watson J (1989) Nurses Manual of Laboratory Tests. FA Davis: Philadelphia
Centers for Disease Control and Prevention (2002) Guidelines for the Prevention of Intravascular Catheter – Related Infections. Department of Health and Human Services. Atlanta. USA Centers for Disease, Control and Prevention (2002) Guidelines for the Prevention of Intravascular Catheter-related Infections. Morbidity and Mortality Weekly Report. 51, RR-10 Cicalini S, Palmieri F, Petrossillo N (2004) Clinical review: new technologies for prevention of intravascular catheter related infections. Critical Care: 8 (3) 157 – 162 Crow S (1989) Asepsis: An indispensable Part of the Patient’s Care Plan. Critical Care Nurse Quarter: 11(4), 11-15.
Daeihagh P, Jordon J, Chen J, Rocco M (2000) Efficacy of Tissue Plasminogen Activator Administration on Patency of Haemodialysis Access Catheters: American Journal of Kidney Diseases: 36 (1) 75 - 79 Deerojanawong J, Sawyer SM, Fink AM, Stokes KB and Robertson CF (1998) Totally Implantable Venous Access Devices in Children with Cystic Fibrosis: Incidence and Type of Complications. Thorax: 53, 285-289
Department of Health (2001) Guidelines for preventing infections associations associated with the insertion and maintenance of central venous catheter. Journal of Hospital infection 47 (supplement) 47 – 67 Department of Health (2007) EPIC. National evidence – based guidelines for preventing hospital – acquired infections associated with the used of central venous catheters. Dolan M (1999) Intravenous flow control and infusion devices. In Dougherty, L and Lamb J. Intravenous therapy in nursing practice. Edinburgh: Churchill Livingstone. Dolan, S. Docherty, L. (2000) Vascular Access devices. In Mallet, J. Docerty, L. (Eds) Mannual of clinical nursing procedure - 5th edition. Oxford. Blackwood Science. Donnelly, M.E, Taylor, S, Thompson D, D’souza S.P. (2004) Radiology Department Royal Preston Hospital, England.
59
Dougherty L (2000) Vascular Access Device Mallett J and Dougherty L In: Manual of Clinical Nursing Procedures. Blackwell Scientific: Oxford
Dougherty L (2004) Vascular Access Devices. In: Dougherty L and Lister S (Eds) Manual of Clinical Nursing Procedures, 6th Ed. Blackwell Science: Oxford
Dougherty L (2006) Central Venous Access Devices: Care and Management. Blackwell Publishing: Oxford Eastridge BJ and Lefor AT (1995) Complications of Indwelling Venous Access Devices in Cancer Patients. Journal of Clinical Oncology: 13, 233-238 Earsling K, Hobson D, White K. (2005) Best practice protocols : prevention of central line infection. Nursing Management 36(10) 18-24 Edmond MB, Ober JF, Weinbaun DL, Pfallor MA, Hwang TZ, Sanford MD (1995) Vancomycin-resistent enterococcus faecium bacteraemia : risk factors for infection: Clinical Infectious Disease 20: 1126-1131.
Elliott T S J, Faroqui M H, Armstrong R F, et al (1994) Guidelines for good practice in central vascular catheterization. Journal of Hospital Infection. 28 (3) 163 - 176 Elliott TSJ, Tebbs SE (1998) Prevention of central venous catheter – related infection. Journal of Hospital Infection: 40(3) 193 –201
Freeman J, Epstein MF, Smith NE (1990) Extra hospital stay and antibiotic usage with nosocomial coagulase – negative staphyloccal bacteremia in two neonatal intensive care unit populations. American Journal of diseases in children144 ( ) 324 - 329 Fry, C. Anholt, D. (2001) Local anaesthesia prior to insertion of a PICC. Journal of Intravenous nursing. 24 (6) 404 - 408 Fuller A, Winn C (1999) Selecting equipment for peripheral cannulation. Professional Nurse. 14 (4) 233 – 236 Gabriel J Bravery K, Docherty L, Kayley J, Malster M, Scales K (2005) Vascular Access: indications and implications for patient care. Nursing Standard. 19 (26) 45 – 52 Gabriel J (2005) care and management of peripherally inserted central catheters. British journal of nursing vol 5 no10 Galloway S and Bodenham A (2004) Long-term Central Venous Access. British Journal of Anaesthesia: 92, 722-734
Garland JS, Buck R K, Maloney P, Durkin DM, Toth – Lloyd S, Duffy M (1995) Comparisons of 10% povidine – iodine and 0.5% chlorhexidine gluconate for the
60
prevention of peripheral intravenous catheter colonisation in neonates: a prospective trial. The paediatric Infectious Disease journal: 14(6) 510 – 516 Garland JS. (2001)A Randomised trial comparing povidone-iodine to a chlorhexidine gluconate-impregnated dressing for prevention of central venous catheter infections in neonates. Peadiatrics; 107(6): 1431-1436.1 Genentech Inc. (2001) Cathflo, ACTIVASE (ALTEPLASE) 2mg, information sheet.
Gillies D, O’Riordan L, Wallen M, Rankin K, Morrison A and Nagy S (2004) Timing of Intravenous Administration Set Changes: A Systematic Review. Infection Control and Hospital Epidemiology. 25(3), 240-250 Gillies D, O’Riodan L, Carr D, Frost J, Gunning R, O’Brien I. Gauze and tape and transparent polyurethane dressing for central venous catheters. Cochrane Database Systems Review 4: CD003827 Goodman M (2000) Chemotherapy: Principles of Administration. Cancer Nursing, Jones and Bartlett, Massachusetts: 385-443 Hadaway LC (2003) Skin flora and infection. Journal of Infusion Nursing, 26 (1) 44-48. Herts BR, Cohen MA, McInroy B, Davros, WJ Zepp C, Einstein DM Power injection of intravenous contrast material through central venous catheters for T: in vitro evaluation. 1996 200: 731 - 735
Hamilton. H, Fermo K (1998) Assessment of patients requiring IV therapy via a central venous route. British Journal of Nursing. 7 (8) 451 - 460 Hamilton H.C. (2000) ‘Selecting the correct IV device: Nursing assessment’. In British Journal of Nursing. 9 (15) 968 - 978. (111)
Hamilton, H. (2006) Complications associated with venous access devices. Journal of Infusion Nursing. 29 (3) 137 - 145 Hanazaki K, Shingu K, Adachi W, Miyazaki T, Amano J (1999) Chlorhexidine dressing for reduction in microbial colonisation of the skin with central venous catheters: A prospective randomised trial. Journal of Hospital Infections: 42, 166 – 168 Hanson RI et al (1976) Heparin lock maintenance with 10mls of sodium heparin in one ml of normal saline solution. Surgery, Gynaecology and obstetrics.142, 373-376. Haire W, Atkinson J, Stephens L, Kotulak G (1994) Urokinase versus recombinant tissue plasminogen activator in thrombosed central venous catheters: A double blinded, randomised trial, Thombosis Haemostasis: 72 (4) 543 – 547
61
Heaton DC, Han DY, Inder A : Minidose (1mg) warfarin as prophylaxis for central vein catheter thrombosis. Int Med J 2002, 32;84-88
Hickman RO., Buckner CD., Clift RA., Sanders JE., Stewart P & Thomas ED.
(1979) A modified right atrial catheter for access to the venous system in marrow transplant recipients. Surgery, Gynaecology & obstetrics 148(6) 871-875.
Hocking G (2000) Central Venous Access and Monitoring. Update in Anaesthesia. 12(13), 1-6
Hoffman K K, Weber D J, Samsa G P, Rutala W A (1992) Transparent polyurethane film as an intravenous catheter dressing. A meta analysis of the infection risks. JAMA 268, 2072 – 2076 Holmer, L.D. Holmes, K.R. (1998) Risks associated with 72 and 96 hour peripheral IV catheter dwell tims. Journal of Intravenous nursing. 21 (5) 301 - 305
Humar A, Ostromecki A, Marshall J C, Lazar N, Houston P C (2000) Prospective randomised trial of 10% povidone – iodine versus 0.5% tincture of chlorhexidine as cutaneous antisepsis for prevention of central venous catheter infection. Clinical Infectious Diseases: 31 ( ) 1001 - 1007
Infection Control Nurses Association (ICNA) 2002 Guidelines for Preventing Intravascular Catheter – related Infections. Fitwise. Edinburgh. INS (2000). Infusion nursing standards of practice. Journal of Intravenous Nursing. 23 (65) supplement (111). Kelly C., Dumenko L., McGregor SE., & McHutchon ME. (1993). A change in flushing protocols of central venous catheters. Oncology Nursing Forum 19(4) 599-605.
Kiernan M (1997) Know how IV insertion sites. Nursing Times. 93 (37) 72 – 73
62
Kinrirons B, Minoz O, Lafendi L, Naas T, Menunier J F, Nordmann P (2001) Chlorhexidine versus povidone iodine in preventing colonization of continuous epidural catheters in children: A randomised, controlled trial. Anesthesiology: 94 239 – 244 Lamont JP, McCarty TM, Stephens JS, Smith BA, Carlo J, Livingston S and Kuhn JA (2003) A Randomized Trial of Valved vs Nonvalved Implantable Ports for Vascular Access. Baylor University Medical Center Proceedings: 16(4), 384-387 Larwood K A, Anstey C M, Dunn S V (2000) Managing central venous catheters. A prospective randomized trial of two methods. Australian Critical Care, 13 (2) 44 - 50 Ledgerwood AM, Saxe,JM, Lucus CE. Venous access devices: a review. Surg Ann 1993,25:45-57 Leon C, Alvarez-Lerma F, Ruiz-Santana S, Gonzalez V, de la Torre MV, Sierra R, Leon M and Rodrigo J.J. (2003) Antiseptic Chamber–containing Hub Reduces Central Venous Catheter-related Infection: A Prospective, Randomised Study. Critical Care Medicine: 31(5), 1318-1324 Little K, Palmer D (1998) Central line exit sites: which dressing. Nursing Standard 12 (48) 42 – 44
Lloyd D A, Shanbhogue L K, Doherty P J, Sutherland D, Hart C A, W DF. (1993) Does the fibrin coat around a central venous catheter influence catheter-related sepsis? Journal of pediatric surgery, 28(3): 345-349. LTHT Infection Control Policies (2003) Guideline for the Prevention of Infection Associated with Central Venous Catheters (CVCs). LTHT Infection Control Policies: 137-142 Macklin D, Chernecky C (2004) Real world nursing survival guide series: IV therapy. Saunders Mann TJ, Orlikowski CE, Gurrin LC, Keil AD. The effect of the Biopatch, a chlorhexidine impregnated dressing, on bacterial coloniztion of epidural catheter exit sites. Anaesth Intensive Care 2001 ; 29(6): 600-603. Maki D G, Ringer M (1987) Evaluation of dressing regimens for prevention of infection with peripheral intravenous catheters. JAMA. 258 (17) 2396 - 2403
Maki DG, Ringer M, Alvarado CJ (1991) Propective randomised trial of povidone iodine, alcohol and chlorhexidine for the prevention of infection associated with central venous and arterial catheters. Lancet. 338: 339-343
63
Maki D G, Stolz, SM, Wheeler S. A (1991) prospective, randomized, three – way clinical comparison of a novel, highly – permeable polyurethane dressing with 206 Swan Ganz pulmonary artery catheters: Tegaderm vs gauze and Tape, 1: cutaneous colonization under the dressing, catheter – related infection. In Maki D G, ed. Improving Catheter Site Care. London, England: Royal Society of Medicine Services; 1991 Maki D G, Will L (1994) Colonisation and infection associated with transparent dressings for central venous, arterial and Hickman catheter. A comparative trial (Abstract) In program and abstracts of the 34th Interscience Conference on antimicrobial agents and chemotherapy (page 30) Washington DC: American Society for Microbiology. Maki DG, Mermel L, Kluger DM (2000). The efficacy of a chlorhexidine- impregnated sponge (Biopatch) for the prevention of intravascular catheter-related infection. A prospective randomised trial. (Abstract 1430). Program and abstracts of the 40th Interscience Conference on Antimicrobial Agents (Toronto). American Society for Microbiology, Washington, DC.
Mangram A, Horan T, Pearson M, Silver LC and Jarvis W (1999) Guidelines for Prevention of Surgical Site Infection. Infection Control and Hospital Epidemiology: 20, 247-278 Mann TJ, Orlikowski CE, Gurrin LC, Keil AD (2001) The effect of the Biopatch, a chlorhexidine impregnated dressing, on bacterial coloniztion of epidural catheter exit sites. Anaesth. Intensive Care. 29(6): 600-603. Markou Nikolaos, Apostolakos Haralampos, Koumoudiou Christiana, Athanasiou Maria, Koutsoukou Alexandra, Alamanos Ioannis and Leonidas Gregorakos Intravenous colistin in the treatment of sepsis from multiresistant Gram-negative bacilli in critically ill patients, Critical Care 2003, 7:R78-R83 Masci G, Magagnoli M, Zucali PA, et al: Minidose warfarin prophylaxis for catheter associated thombosis in cancer patient: can it be safely associated with fluorouracil-based chemotherapy. J Clin Oncol 2003, 21:736-739 Masoorli S and Angeles A (2002) Getting a Line on CVAD (Central Vascular Access Devices). www.findarticles.com/p/articles/mi_qa3869/is_200204/ai_n9044227/pg_1
McGee and Gould (2003) Preventing Complications of Central Venous Catheterization. New England Journal of Medicine. 348 (12) 1123 -1133 McKee R, Dunsmuir R, Whitby M, Garden OJ (1985) Does antibiotic prophylaxis at the time of catheter insertion reduce the incidence of catheter related sepsis in I.V. nutrition. Journal of Hospital Infection: 6: 419-425
McPhee A (1999) Handbook of infusion Therapy. Springhouse Corporation: Pennsylvania
64
Meers C (1998) Urokinase efficiency in the restoration of haemodialysis catheter formation: Journal of CANNT: 8 (2) 17 – 19 Medcomp www.medcompnet.com Instructions for use for long term access haemodialyis catheters 8 Mehall JR, Saltzman DA, Jackson RJ, Smith SD (2002) Fibrin Sheath enhances central venous catheter infection. Critical Care Medicine, 30(4): 908-912. Mermel L.A, McCormack R.D, Springman S.R, Maki D.G. (1991) The pathogensesis and epidemiology of catheter – related infection with pulmonary artery Swan – Ganz catheters: a prospective study utilizing molecular subtyping. American Journal of Medicine. Vol. 91 (suppl 3B) : S197 – S205 Mermel L.A. Prevention of intravascular catheter-related infection. Ann Intern Med 2000 March 7: 132(5) : 391-402
Minoz O, Pieroni L, Lawerence C, Edouard A, Costa Y, Samii K, Brun-Buisson C. (1996) Prospective randomised trial of two antiseptic solutions for prevrntion of central venous or arterial catheter colonization and infection in intensive care units patients. Critical Care Medical: 24 : 1818-1823.
Moureau N (2004) Drawing Blood through a Central Venous Catheter. www.findarticles.com/p/articles/mi_qa3689/is_200402/ai_n9385672 Murray et al very low doses of warfarin can prevent thrombosis in central venous catheters. A randomised prospective trial Ann Intern Med. 1990,112:423-428 National Institute for Clinical Excellence (2003) Clinical Guideline 2, Infection Control: Prevention of healthcare associated infection in primary and community care. Surrey. UK Occupational Safety and Health administration. Securing medical devices. OSHA Fact sheet. 2004. Publication no. 7.
O’Grady N P (2002) Applying the science to the prevention of catheter – related infections. Journal of Critical: 17 (2) 114 – 121 Ohmagari.N, Raad I et al.(2004);, Cancer 101:2300- 2302 Oldham P (1991) A sticky situation. A microbiological study of adhesive tape used to secure IV cannula. Professional Nurse. 6 (5) 265 – 269
Olson K, Rennie RP, Hanson J, Ryan M, Gilpin J, Falsetti J, Heffne (2004) Evaluation of a no – dressing intervention for tunnelled central catheter exit sites. Journal of Infusion Nursing: 27 (1) 37 - 44 Oncu S, Salarya S (2003) Central venous catheter – related infections: an overview with special emphasis on diagnosis, prevention and management. The Internet Journal of Anaesthesiology. 7 ,1
65
Polderman, Girbes (2002) Central Venous Catheter use. Part 1; mechanical complications. Intensive care medicine. 28 (1) 2002
Pratt RJ, Pellowe C, Loveday HP, Robertson N, Smith GW and the epic development tea: Barrett S, Davey P, Harper P, Loveday C, McDougall C, Mulhall A, Privett S, Smales C, Taylor L, Weller B, Wilcox M (2001) The Epic Project: Developing National Evidence-based Guidelines for Preventing Hospital associated infections. Phase 1: Guidelines for Preventing Hospital-acquired Infections. Journal of Hospital Infection: 47 (supplement): S1-S82. Pratt RJ, Pellowe C, Loveday HP, Robinson N, Smith GW (2001) The Epic Project: Guidelines for preventing hospital-acquired infections:Phase 1. Journal of Hospital Infection. 47(supplement): S3-S4
Pratt R J, Pellowe C, Wilson J A, Loveday H P, Harper P J, Jones S R L J, McDougall C, Wilcox M H (2007) Epic 2: National Evidence – Based Guidelines for Preventing Healthcare – Associated Infections in NHS Hospitals in England (WWW.sciencedirect.com) Raad II, Hanna H A (2002) Intravascular Catheter – Related Infections. New Horizons and Recent Advances. Archives of Internal Medicine: 162, 871 – 878
Removal of central venous line www.hericineau/net.ac/.clinical/icu/procedures cycrem.html.Resourcentre.com/RN/refcenter/declot_ctrl (assessed March 2004) Reynolds NJ, Grosvenor LJ, Anaesthesia (2003) 58 (9) 923-924.
Reynolds M G, Ringer M, Alvarado C J (1997) Do Dressings with Increased Permeability Reduce the Incidence of Central Venous Catheter Related Sepsis? Intensive and Critical Care Nursing 13, 26 – 29 Rosenthal K (2003) Pinpointing intravascular device infections. Nursing Management. 3 (6) 35 – 43 Rosenthal K. (2006) Guarding against vascular site infection: arm yourself with the latest knowledge on equipment and technique to prevent patients from catheter related bloodsteam infection. Nursing Management. April 2006: 55-65.
Rothschild, J. M. (2001) Ultrasound guidance of central vein catheterisation. Evidence Report ? Technology Assessment, No 43. Chapter 21. Making Healthcare Safer. A Critical Analysis of Patient Safety Practices. Agency for Healthcare Research and Quality Publication, No 01-E058. 2001; 245 - 253.
RCN IV Therapy Forum (2003) Standards for Infusion Therapy. RCN: London.
RCN IV Therapy Forum (2006) Standards of Infusion Therapy. RCN: London
66
Saint S, Veenstra D L, Lipsky B A (2000) The clinical and economic consequences of nosocmial central venous catheter – related infection: are antimicrobial catheters useful? Infection Control Hospital Epidemiol 21 (6) 375 – 380
Sansivero G E (1998) Venous anatomy and physiology. Considerations for
vascular access device placement and function, Journal of intravenous nursing 21 (5 supplement) S107 – 14
Santilli J (2002) Fibrin Sheath and Central Venous Catheter Occlusions: Diagnosis and Management. Techniques in Vascular and Interventional Radiology: 5 (2) 89 – 94 Savader S, Ehrman K, Porter D, Haikal L Oteham (2001) Treatment of haemodialysis catheter – associated fibrin sheaths PA infusion: critical analysis of 124 procedures. Journal of Vascular Interventional Radiology: 12 (6) 711 – 715 Scales K (1999) Vascular Access in the Acute Care Setting. In: Dougherty L and Lamb J (Eds) Intravenous Therapy in Nursing Practice. Churchill Livingstone: Edinburgh
Schwarz RE, Groeger RS and Coit G (1997) Subcutaneously Implanted Central Venous Access Devices in Cancer Patients. Cancer: 79, 1635-1640
Scottish Intercollegate Guidelines Network Antithrombotic therapy. Edinburgh: 1999. Shea M, Hmiel S, Beck A (2001) Use of tissue plasminogen activator for thrombolysis in occluded peritoneal catheters in children. Perit Dialysis: 17, 249 - 252 Sheppard K, LeDesma M, O’Connor K (1999) A prospective study of two intravenous catheter securement techniques in a skilled nursing facility. Journal of Intravenous Nursing : 22, 151 – 156 Slama, M. (1996) Improvement of internal jugular vein cannulation using an ultrasound guided technique. Intensive Care Medicine. 23: 692 - 697 Svoboda P, Barton R, Barbarash O, Butylin A, Jacobs B, Lata J, Haire W, Jaff M, Firszt C, Mouginis T, Schuerr D, Schulz G, Schwartz L, El-Shahawy M. (2004) Recombinant urokinase is safe and effective in restoring patency to occluded central venous access devices: A multi – center, international trial? Critical Care Medicine: 32 (10) 1990 - 1996 Tebbs SE, Trend V and Elliott TSJ (1995) The Potential reduction of Microbial Contamination of Central Venous Catheters. Journal of Hospital Infection: 30, 107-113
Todd (1998). “Peripherally inserted central catheters”. Professional Nurse. 13(5)
297-302 (111).
67
Trerotola SO, Kuhn-Fulton J, Johnson MS, Shah H, Ambrosious WT, Kneebone
PH (2000) Tunnelled infusion catheters: increased incidence of symptomatic venous thrombosis after subclavian versus internal jugular venous access. Radiology 217: 89 – 93
UKCC(1992) Code of Professional Conduct for the nurse, midwife and health visitor. UKCC. London
UKCC (1992) The scope of professional Practice. UKCC. London US Food and Drug Administration, Center for Biologics Evaluation and
Research. Alert for prescribers, urokinase (Abbott Laboratories), January 25, 1999. Bathesda, Food and Drug Administration, 1999
Vygon (2001) Mid to long term vascular access from Vygon (Brochure)
Waghorn D J (1994) Intravascular device – associated systemic infection: a 2 year analysis of cases in a DGH. Journal of Hospital Infection: 28 (2) 91 - 101
Ward M S, Lam K V, Cannell PK, Harrmann P R (1999) Mycobacterial central venous catheter tunnel infection: a difficult problem. Bone Marrow Transplant: 24 (3) 325 - 329
Weatherhill K (1999). Keeping the lines open. Nursing Standard. Vol 13(52) 15-21 Sept.
Weber DR (1991). Is heparin really necessary in the lock and so, how much?
Drug Intelligence & Clinical Pharamacy. 25, 309-407.
Wiernikowski J, Crowther M, Clase C, Ingram A, Chan A. (1999) Stability and sterility of recombinant tissue plasminogen activator at – 30oC. Research letter. Wood D (1997) A comparative study of two securement techniques for short peripheral intravenous catheters. Journal of Intravenous Nursing, 20 , 280 – 285
Woodrow p (2002) Central Venous Catheters and central venous pressure. Nursing Standard 2002: 16 (26) 45-51
Xiang D, Verbeken E, Van Lommel A, Stas M, De Wever I (1998) Composition of the sleeve enveloping a central venous catheter. Journal of Vascular Surgery: 28 (2) 260 – 271 Yamamoto AJ, Solomon JA, Soulen M C et al (2002) Sutureless securement devices reduces complications of PICC’s. Journal of Interventional Radiology: 13: 77 – 81